Abstract
Background
Percutaneous tracheostomy (PT) in patients with coronavirus disease (COVID‐19) included several critical steps associated with increased risk of aerosol generation. We reported a modified PT technique aiming to minimize the risk of aerosol generation and to increase the staff safety in COVID‐19 patients.
Methods
PT was performed with a modified technique including the use of a smaller endotracheal tube (ETT) cuffed at the carina during the procedure.
Results
The modified technique we proposed was successfully performed in three critically ill patients with COVID‐19.
Conclusions
In COVID‐19 critically ill patients, a modified PT technique, including the use of a smaller ETT cuffed at the carina and fiber‐optic bronchoscope inserted between the tube and the inner surface of the trachea, may ensure a better airway management, respiratory function, patient comfort, and great safety for the staff.
Keywords: airway management, COVID‐19, critically ill patients, intensive care unit, percutaneous tracheostomy
1. INTRODUCTION
As the novel coronavirus (2019‐nCov) globally spreads, the coronavirus disease (COVID‐19) pandemic is straining health care workers worldwide. 1 In hospitalized patients with severe COVID‐19, endotracheal intubation is one of the most common and indispensable life‐saving interventions. In a recent report from the city of New York, 12% of COVID‐19 patients required invasive mechanical ventilation. 2 Since difficult weaning and prolonged mechanical ventilation represent the two most common indications for tracheostomy in intensive care unit (ICU), it may play a central role in COVID‐19 management. 3 During the 2019‐nCov pandemic, the aerosol generating procedures, such as tracheostomy, expose physicians at high risk to contract the infection. 4 Accordingly, special consideration may be done to protect otolaryngologists, general surgeons, and critical care physicians from the risk of infection while performing a tracheostomy in COVID‐19 patients. 5 Percutaneous tracheostomy (PT) is routinely performed at the bedside in ICU; unfortunately, a modified protocol to perform PT in COVID‐19 patients included several critical steps associated with increased risk of aerosol generation, such as changing the catheter mount, repositioning the endotracheal tube (ETT) cuff to the level of the vocal cords, and removal of large dilator. 6 So far, there has been no prior description in the literature of how to minimize the aerosol generation during PT. We reported a modified PT technique aiming to minimize the risk of aerosol generation and to increase the staff safety in COVID‐19 patients.
2. PROCEDURAL STEPS
We performed three PTs at ICU bedside because of three COVID‐19 patients were difficult to wean from mechanical ventilation. Patients were aged 47, 67, and 71 years old (one woman and two men) and all reported positive after nasopharyngeal swabs. Since the COVID‐19 outbreak in Italy, from the 10th of March, our ICU was completely dedicated to COVID‐19 patients. The rooms had no negative pressure inside. As follow we reported the procedural steps of PT performed with a guidewire forceps technique. The readers are encouraged to watch the supplementary video (Video S1) for a more comprehensive understanding of the procedure.
The tracheostomy team was formed by two expert ICU physicians in airway procedures and a nurse.
All personnel were equipped with the proper personal protective equipment, including an N99 mask, eye goggles, transparent full‐face shield, gown, and double gloves.
Before the procedure, patients were anesthetized with midazolam 0.3 to 0.35 mg/kg, fentanyl 0.1 mg, and cisatracurium 0.2 mg/kg.
Before the beginning of the procedures, volume control ventilation was set at a respiratory rate of 15 breaths/min with an FiO2 of 1.0, tidal volume of 500 mL, and positive end‐expiratory pressure of 5 cm H2O.
After 5 minutes of preoxygenation with the previous ventilation settings, the ventilator was switched off by the nurse. The ICU physician replaced the ETT in place with a smaller ETT with an internal diameter of 6 mm by using a videolaryngoscope.
The ETT was cuffed at the level of the carina (Figure 1). Then the ventilator was connected with the ETT and switched on.
By using the videolaryngosocpe to visualize the glottis, the fiber‐optic bronchoscope with an external diameter of 5 mm was passed through the vocal cords.
The fiber‐optic bronchoscope was kept just under the level of vocal cords outside the ETT to control the different PT steps.
PT was performed with the guidewire forceps technique.
The puncture of the anterior tracheal wall, Seldinger insertion, dilatation, and cannula positioning were all performed with the smaller ETT cuffed and positioned at the carina (Figure 2).
When the cannula was correctly positioned, the ventilator was switched off and the smaller ETT was removed. The cannula was cuffed and the ventilator was connected with it and switched on.
The fiber‐optic bronchoscope was removed after the removal of the ETT.
FIGURE 1.
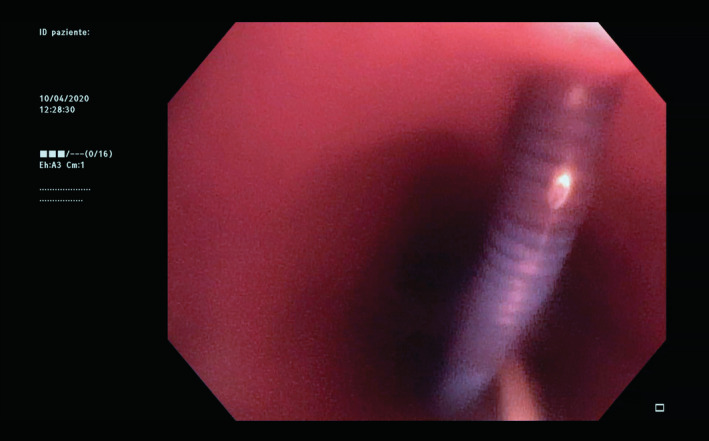
Seldinger passed through the anterior tracheal wall with the smaller endotracheal tube inside the trachea [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
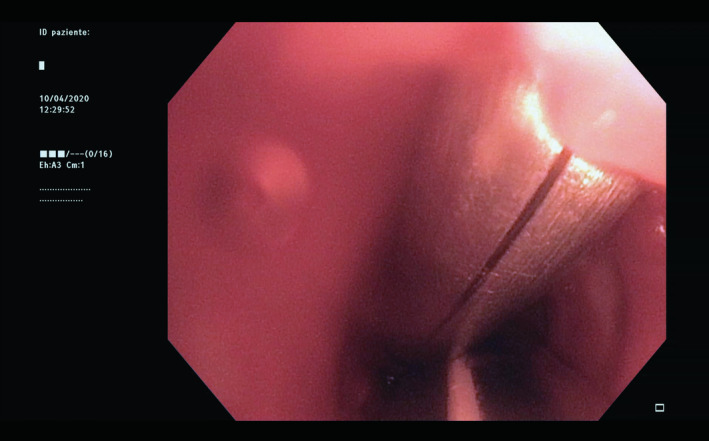
Positioning of the guidewire dilating forceps with the endotracheal tube inside the trachea [Color figure can be viewed at wileyonlinelibrary.com]
3. DISCUSSION
To our knowledge, our was the first report describing a modified PT procedure targeted to COVID‐19 critically ill patients. Ensuring minimal exposure and risk to the staff that perform the procedures was of paramount importance. 7 Takhar et al proposed a modified PT technique in COVID‐19 6 : this technique differed from the standard one for (a) the clamping of the ETT and pausing the ventilator while positioning the cuff at the level of the vocal cords, (b) pausing the ventilator again while removing the dilator from the trachea, and 3) for covering the tracheal puncture site with gauze. 6 In our opinion, changing catheter mount for bronchoscopy, repositioning ETT cuff to the level of the vocal cords, and removal of large rhino dilator were three steps associated with an increased risk of aerosol generation. 6 In the modified procedure proposed by our team, only the exchanging of the ETT with a smaller one might increase the risk of aerosol generation. However, our expertise in airway management allowed us to perform this step by using the videolaryngoscope as recommended by a recent guideline. 8 Indeed, using a videolaryngoscope with a separate screen enables the operator to stay further away from the airway; this technique is recommended only for those physicians trained in their use. 8 Having the cannula, the ETT and fiber‐optic bronchoscope inside the trachea while removing the smaller ETT at the end of the procedure may limit the aerosol spread at this step. Our previous experience demonstrated that the ETT, the tracheal cannula, and the fiber‐optic bronchoscope can be simultaneously inserted inside the trachea. 9 Our modified PT technique was performed with ETT cuffed at the level of the carina and the fiber‐optic bronchoscope outside it; this allowed a stable gas exchange, airway pressure, ventilation, and no spread of aerosol during the procedure. 8
4. CONCLUSIONS
In COVID‐19 critically ill patients, a modified PT technique, including the use of a smaller ETT cuffed at the carina and fiber‐optic bronchoscope inserted between the tube and the inner surface of the trachea, just below the vocal cords, may ensure a better airway management, respiratory function, patient comfort, and great safety for the staff.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Supporting information
Video S1
Vargas M, Russo G, Iacovazzo C, Servillo G. Modified percutaneous tracheostomy in COVID‐19 critically ill patients. Head & Neck. 2020;42:1363–1366. 10.1002/hed.26276
REFERENCES
- 1. Zhong Y, Xiao H, Varvares MA. How to avoid nosocomial spread during tracheostomy for COVID‐19 patients. Head Neck. 2020. 10.1002/hed.26167; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City Area. JAMA. 2020. 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vargas M, Sutherasan Y, Antonelli M, et al. Tracheostomy procedures in the intensive care unit: an international survey. Crit Care. 2015;19:291‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan YJK, Wong EWY, Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemican experience in Hong Kong. JAMA Otolaryngol Head Neck Surg. 2020. 10.1001/jamaoto.2020.0488. [DOI] [PubMed] [Google Scholar]
- 5. Heyd CP, Desiato VM, Nguyen SA, et al. Tracheostomy protocols during COVID‐19 pandemic. Head Neck. 2020. 10.1002/hed.26192; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Takhar A, Walker A, Tricklebank S, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID‐19 pandemic. Eur Arch Otorhinolaryngol. 2020. 10.1007/s00405-020-05993-x; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vargas M, Servillo G. Improving staff safety during tracheostomy in COVID‐19 patients. Head Neck. 2020. 10.1002/hed.26163; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cook TM, El‐Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID‐19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020. 10.1111/anae.15054; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vargas M, Pelosi P, Tessitore G, et al. Percutaneous dilatational tracheostomy with a double‐lumen endotracheal tube: a comparison of feasibility, gas exchange, and airway pressures. Chest. 2015;147(5):1267‐1274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1


