Abstract
Previous research has identified a relationship between climate and occurrence of SARS‐CoV and MERS‐CoV cases, information that can be used to reduce the risk of infection. Using COVID‐19 notification and postcode data from New South Wales, Australia during the exponential phase of the epidemic in 2020, we used time series analysis to investigate the relationship between 749 cases of locally acquired COVID‐19 and daily rainfall, 9 a.m. and 3 p.m. temperature, and 9 a.m. and 3 p.m. relative humidity. Lower 9 a.m. relative humidity (but not rainfall or temperature) was associated with increased case occurrence; a reduction in relative humidity of 1% was predicted to be associated with an increase of COVID‐19 cases by 6.11%. During periods of low relative humidity, the public health system should anticipate an increased number of COVID‐19 cases.
Keywords: Australia, COVID‐19, humidity, meteorological factors, rainfall, temperature, time series analysis
1. INTRODUCTION
The first cases of severe acute respiratory coronavirus‐2 (SARS‐CoV‐2) were reported in Wuhan, China in December 2019 (Wu, Leung, & Leung, 2020). Since that time, the disease caused by SARS‐CoV‐2—novel coronavirus disease (COVID‐19)—has been reported throughout the world and the resulting pandemic of more than 5 million infections and more than 300,000 deaths has caused a dramatic impact on the global economy and social structure.
The first case of COVID‐19 was reported in Australia (Sydney, New South Wales [NSW]) on 21 January 2020 (NSW Government, 2020a). Preventing transmission is based on the practice of good hygiene, social distancing, limiting public gatherings and for those infected or a close contact of those infected, self‐isolation (Australian Government Department of Health, 2020a). The Australian Government's response to COVID‐19 is staged—initial action, targeted action, stand‐down and preparedness (Australian Government Department of Health, 2020a). In the initial stage, public awareness and health system capacity was increased; entry was refused to direct flights from Hubei Province, and health checks were initiated on people arriving from countries considered to be high risk. On 15 March, the response moved to targeted action and between 23 and 29 March restrictions were applied on non‐essential gatherings and travel (Australian Government Department of Health, 2020b), an effective ‘shutdown’. As of the end of April, the number of notified cases was restricted to 6,753 and 91 deaths, with 563,641 tests conducted (Australian Government Department of Health, 2020c).
Although still an area of active research, the spread of SARS‐CoV‐2 between people appears to be predominantly via respiratory droplets and aerosols and fomites (Cai et al., 2020), with possibly faecal–oral spread being a route of transmission (Yeo, Kaushal, & Yeo, 2020). Due to the nature of the virus and likely mechanism of spread, environmental factors—especially temperature and relative humidity—likely influence coronavirus transmission (Casanova, Jeon, Rutala, Weber, & Sobsey, 2010) via the relationship between virus survival in the environment and these factors. An inverse relationship between relative humidity and SARS cases (Cai et al., 2007; Tan et al., 2005), and a positive correlation with temperature (Tan et al., 2005), in China have previously been identified. Similarly in a study of Middle East respiratory syndrome coronavirus (MERS‐CoV) (Gardner et al., 2019)—in which a case‐crossover design was used to identify statistically significant temporal associations between 446 cases reported from Saudi Arabia, 2015–2017 (likely to be spillover transmission from camels) and climatic variables—lower humidity and lower temperature were associated with increased cases 8–10 days later. In another study based on MERS‐CoV case occurrence between 2012 and 2018, high temperature and low relative humidity were identified as contributors to increased MERS‐CoV cases (Altamimi & Ahmed, 2020). Thus, for both SARS and MERS‐CoV, lower relative humidity appears to be associated with case occurrence, however the nature of the relationship between temperature and case occurrence is less clear. In one of the first studies of its type, based on the daily count of COVID‐19 cases in 30 Chinese provinces Qi et al. (2020) found significant negative associations between cases and average temperature and relative humidity. In addition, an interaction between temperature and humidity in Hubei province was identified. Every 1% increase in average relative humidity was predicted to decrease daily confirmed cases by 11%–22%, when average temperature was in the range of 5–8°C. It was suggested that in China in the spring, there should be a focus on monitoring and prevention of COVID‐19 in northern regions with low temperature and low relative humidity, because of the presence of suitable climatic conditions for SARS‐CoV‐2 transmission.
In the current study, our aim was to further investigate the relationship between reports of COVID‐19 cases during the early epidemic phase in NSW, Australia and temperature and relative humidity. Understanding this relationship in different parts of the world enables the development of better pandemic response plans and surveillance systems, and potentially highlights regions where additional public health inventions might be needed to control COVID‐19.
2. METHODS
Case reports in NSW, Australia from the beginning of the epidemic in January 2020 to the peak of the epidemic at the end of March 2020 were accessed (NSW Government, 2020a). Case reports in which the source of infection was determined to be locally acquired, and in which a date of notification and postcode of residence was reported, were selected for inclusion into the study. A time series of case reports was then created. Based on the reported postcode, for all reported cases in the time series the closest weather observation station reporting rainfall, temperature and humidity for the period January to March 2020 was identified (NSW Government, 2020b). Daily observations of the following meteorological recordings were downloaded: rainfall (mm), and temperature (°C) and relative humidity (%) recorded at 9 a.m. and at 3 p.m. (Australian Government Bureau of Meteorology, 2020). The median values for each day for all selected weather observation stations were estimated, and time series of median rainfall, and 9 a.m. and 3 p.m. temperature and relative humidity were created. Two additional time series were then created by determining the daily difference between 9 a.m. and 3 p.m. temperature, and between 9 a.m. and 3 p.m. relative humidity. Thus, 7 predictor time series were available for modelling.
A correlation matrix was used to select meteorological variables to avoid multicollinearity in the analysis. Variables with a correlation coefficient <0.6 were retained. Each remaining variable was included in a univariate generalized additive model (GAM) with daily number of reported cases as the dependent variable. Variables with p value < 0.1 in univariate analyses were then included in a multivariate GAM, and the best‐fitting model based on Akaike information criterion (AIC) was selected using a backward algorithm. COVID‐19 cases were assumed to follow a negative binomial distribution given that the variances of the daily cases reported were greater than their means. Meteorological variables were analysed using a 14‐day exponential moving average (EMA), based on the assumed incubation period of SARS‐CoV‐2. Natural splines of two degrees of freedom were also included to account for additional short‐term trend. A sensitivity analysis was performed by modifying the EMA from 14 days to 10 and 21 days, respectively. R software (version 3.5.3, http://cran.r‐project.org; R Foundation for Statistical Computing, Vienna, Austria) was used to perform all the statistical analyses and visualization.
3. RESULTS
The first case was reported in NSW on 22 January 2020. For this case and the subsequent 5 cases, infections were determined to have been acquired overseas. The first case in which infection was determined to have been acquired locally was notified on 26 February (NSW Government, 2020b). Between 26 February and 31 March, a total of 749 cases were notified in which infection was determined to have been acquired locally and which reported a residence postcode. The median (interquartile range [IQR]) day of reporting was 24 March (19 March, 27 March). Cases were notified from 58 different local government areas, and 74% were from the Greater Sydney area. The daily counts gradually increased until reaching a peak around 27 March (Figure 1a) and then gradually decreased. Climatic data were acquired from 52 weather observation stations (Australian Government Bureau of Meteorology, 2020). During the period 14 days prior to the first case with local transmission (12 February) to 31 March (49 days), 9 a.m. and 3 p.m. relative humidity and 3 p.m. temperature remained approximately constant (median [IQR]: 82.0% [75.5, 88], 60.0% [52.5, 69] and 24.1°C [21.9, 25.5], respectively); however, the 9 a.m. temperature time series (median [IQR]: 19.9°C [18.4, 21.6]) showed a decreasing trend (−0.106/day; r 2 .5109). During this period, there were 27 days (55%) with recorded rainfall (median [IQR]: 1.5 mm [0.2, 4.7]). Substantial rainfall (28–71 mm daily medians) was reported between 7 and 10 February. The difference in 9 a.m. and 3 p.m. relative humidity difference varied over a wide range, whereas 9 a.m. and 3 p.m. temperature difference remained relatively constant about a median value of 3.95°C (Figure 1b).
FIGURE 1.
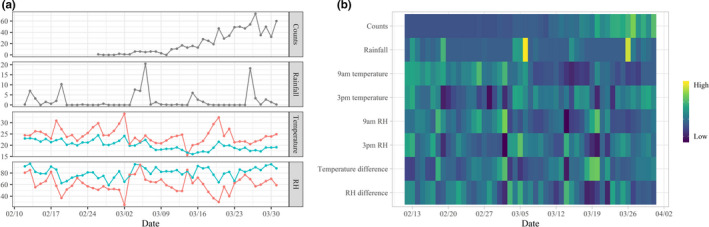
Time series (a) of 749 notified cases of COVID‐19 in New South Wales, Australia (counts) in which infection was determined to be locally acquired and for which postcode of residence was reported, during the period 12 February (day 43) to 31 March (day 91); and median rainfall and 9 a.m. (green) and 3 p.m. (red) temperature and relative humidity (RH) and (b) heatmap of standardized notified cases (counts), rainfall, temperature and relative humidity, 9 a.m.–3 p.m. temperature difference and 9 a.m.–3 p.m. relative humidity difference recorded at weather observation stations closest to reported case postcode of residence. Two periods of high rainfall were observed, and 9 a.m. temperatures tended to decrease throughout the period, but 9 a.m.–3 p.m. temperature differences tended to be less variable than 9 a.m.–3 p.m. humidity differences
Collinearity was identified between some of the predictor variables, so univariate GAMs were fit to cases and rainfall, 9 a.m. temperature, 9 a.m. relative humidity, and the difference between 9 a.m. and 3 p.m. relative humidity. A negative relationship between cases and 9 a.m. relative humidity was found, and a positive relationship between cases and 9a.m. temperature (Table 1). In multivariate analysis, only 9 a.m. relative humidity was found to be significantly (p = .0304) associated with cases (AIC 211.8; Table 2). The interaction between 9 a.m. temperature and 9 a.m. relative humidity was not statistically significant. Using either a 10‐day or 21‐day exponential moving average, the best‐fitting model (AIC 212.2 and 211.4, respectively) remained 9 a.m. relative humidity only (p = .0408 and .0254, respectively). Including 9 a.m. temperature in either of these three models did not improve the model fit.
TABLE 1.
Association between 749 notified cases of COVID‐19 in New South Wales, Australia in which infection was determined to be locally acquired and for which postcode of residence was reported, during the period 12 February (day 43) to 31 March (day 91), and climate recorded at the weather observation station closest to reported case postcode of residence
| Parameter | Estimate | SE | Z | p |
|---|---|---|---|---|
| Temperature, 9 a.m. | 0.27 | 0.18 | 1.48 | .14 |
| Relative humidity, 9 a.m. | −0.06 | 0.03 | −2.17 | .03 |
| Rainfall | −0.03 | 0.08 | −0.44 | .66 |
| Relative humidity difference a | −0.02 | 0.03 | −0.66 | .51 |
Relative humidity, 9 a.m.—relative humidity, 3 p.m.
TABLE 2.
Multivariate generalized additive model of the association between 749 notified cases of COVID‐19 in New South Wales, Australia in which infection was determined to be locally acquired and for which postcode of residence was reported, during the period 12 February (day 43) to 31 March (day 91), and 9 a.m. relative humidity (10‐, 14‐ and 21‐day exponential moving average) recorded at the weather observation station closest to reported case postcode of residence. Natural splines were included to control short term trend.
| Parameter | Exponential moving average | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 10‐day | 14‐day | 21‐day | |||||||
| Estimate (SE) | Z | p | Estimate (SE) | Z | p | Estimate (SE) | Z | p | |
| Intercept | 2.69 (1.74) | 1.54 | .12 | 4.06 (2.27) | 1.78 | .07 | 6.55 (3.31) | 1.98 | .05 |
| Relative humidity, 9 a.m. | −0.04 (0.02) | −2.05 | .04 | −0.06 (0.03) | −2.17 | .03 | −0.09 (0.04) | −2.24 | .03 |
| Natural spline (1) | 7.62 (0.71) | 10.70 | <.01 | 7.81 (0.73) | 10.70 | <.01 | 8.03 (0.76) | 10.60 | <.01 |
| Natural spline (2) | 3.16 (0.21) | 14.90 | <.01 | 3.22 (0.22) | 14.60 | <.01 | 3.31 (0.24) | 13.80 | <.01 |
4. DISCUSSION
There have been few published investigations on the relationship between climate and COVID‐19, and to our knowledge none in the Southern Hemisphere or specifically Australia. We found a negative relationship between the evolving COVID‐19 epidemic in NSW, Australia and relative humidity, but not rainfall nor temperature; a 1% decrease in 9 a.m. relative humidity could increase the number of COVID‐19 cases by 6.11%.
Temperature and relative humidity are known to be important factors in the spread of respiratory diseases. Several epidemiological and laboratory studies have found that temperature and relative humidity affect the spread of coronavirus‐related diseases, with both low temperature and relative humidity being suitable for the survival and transmission of coronavirus (Casanova et al., 2010; Chan et al., 2011; Guionie et al., 2013). Some statistical modelling studies have found that higher relative humidity could lead to a reduction in COVID‐19 cases (Qi et al., 2020; Ma et al., 2020), which is consistent with our study findings. However, we did not find an association between temperature and COVID‐19 cases. Despite some studies suggesting that lower temperature could increase the incidence of COVID‐19 (Qi et al., 2020), other studies have not identified such a relationship (Yao et al., 2020; Zhu & Xie, 2020). These inconsistencies might suggest that the impact of temperature on SARS‐CoV‐2 transmission is more complex and heterogeneous across the landscape and in different countries—or even hemispheres. Temperature ranged from 16 to 24°C (9 a.m.) and 16 to 34°C (3 p.m.) in our study area during the epidemic period, which is very different from most of the recent studies from China and elsewhere in the Northern Hemisphere winter. The timing of the COVID‐19 pandemic—beginning in January—and the differences between climate (especially temperature) between the Northern and Southern Hemispheres could explain a lack of association in our study with temperature and might also partially explain the relatively limited transmission of SARS‐CoV‐2 in Australia to date (265 cases per million). However, despite the temperatures experienced in the Southern Hemisphere summer, SARS‐CoV‐2 can be transmitted. Our study suggests that even with higher temperature, COVID‐19 could persist through the coming northern summer and ongoing surveillance and prevention will be needed. In addition, our finding that lower relative humidity is associated with cases together with other published studies suggests that any area—regardless of season or location—can be at risk of SARS‐CoV‐2 transmission and that this risk increases at lower humidity.
In conclusion, under the conditions of high temperature in the Southern Hemisphere summer, our study provides evidence that lower relative humidity is associated with COVID‐19 cases. It also suggests that all countries need to maintain vigilance for COVID‐19, even during the summer months.
CONFLICT OF INTEREST
No conflict of interest is declared.
ETHICAL APPROVAL
The authors confirm that the ethical policies of the journal, as noted on the journal’s author guidelines page, have been adhered to. No ethical approval was required as the case notification data was accessed from the public (NSW Government) domain.
ACKNOWLEDGEMENTS
NSW Ministry of Health is thanked for freely making available COVID‐19 case notification data.
Ward MP, Xiao S, Zhang Z. The role of climate during the COVID‐19 epidemic in New South Wales, Australia. Transbound Emerg Dis. 2020;67:2313–2317. 10.1111/tbed.13631
Michael P. Ward and Zhijie Zhang contributed equally.
Contributor Information
Michael P. Ward, Email: michael.ward@sydney.edu.au.
Zhijie Zhang, Email: zhj_zhang@fudan.edu.cn.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from NSW.Data and the Australian Bureau of Meteorology. These data were derived from the following resources available in the public domain: https://data.nsw.gov.au/dataset/nsw‐covid‐19‐tests‐by‐location‐and‐result and http://www.bom.gov.au/nsw/observations/map.shtml.
REFERENCES
- Altamimi, A. , & Ahmed, A. E. (2020). Climate factors and incidence of Middle East respiratory syndrome coronavirus. Journal of Infection and Public Health, 13(5), 704–708. 10.1016/j.jiph.2019.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Government Bureau of Meteorology (2020). New South Wales weather observation stations. Retrieved from http://www.bom.gov.au/nsw/observations/map.shtml [Google Scholar]
- Australian Government Department of Health (2020a). Australian health sector emergency Response plan for novel coronavirus (COVID‐19). Retrieved from https://www.health.gov.au/sites/default/files/documents/2020/03/australian‐health‐sector‐emergency‐response‐plan‐for‐novel‐coronavirus‐covid‐19‐short‐form‐the‐australian‐health‐sector‐emergency‐response‐plan‐for‐novel‐coronavirus‐short‐form.pdf [Google Scholar]
- Australian Government Department of Health (2020b). How to protect yourself and others from coronavirus COVID‐19. Retrieved from https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/how‐to‐protect‐yourself‐and‐others‐from‐coronavirus‐covid‐19/limits‐on‐public‐gatherings‐for‐coronavirus‐covid‐19 [Google Scholar]
- Australian Government Department of Health (2020c). Coronavirus (COVID‐19) health alert. Current status. Retrieved from https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert [Google Scholar]
- Cai, J. , Sun, W. , Huang, J. , Gamber, M. , Wu, J. , & He, G. (2020). Indirect virus transmission in cluster of COVID‐19 cases, Wenzhou, China, 2020. Emerging Infectious Diseases, 26(6), 1343–1345. 10.3201/eid2606.200412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, Q. C. , Lu, J. , Xu, Q. F. , Guo, Q. , Xu, D. Z. , Sun, Q. W. , … Jiang, Q.‐W. (2007). Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Public Health, 121, 258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova, L. M. , Jeon, S. , Rutala, W. A. , Weber, D. J. , & Sobsey, M. D. (2010). Effects of air temperature and relative humidity on coronavirus survival on surfaces. Applied and Environmental Microbiology, 76, 2712–2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, K. H. , Peiris, J. S. , Lam, S. Y. , Poon, L. L. , Yuen, K. Y. , & Seto, W. H. (2011). The effects of temperature and relative humidity on the viability of the SARS coronavirus. Advances in Virology, 2011, 734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner, E. G. , Kelton, D. , Poljak, Z. , Van Kerkhove, M. , von Dobschuetz, S. , & Greer, A. L. (2019). A case‐crossover analysis of the impact of weather on primary cases of Middle East respiratory syndrome. BMC Infectious Diseases, 19, 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guionie, O. , Courtillon, C. , Allee, C. , Maurel, S. , Queguiner, M. , & Eterradossi, N. (2013). An experimental study of the survival of turkey coronavirus at room temperature and +4 degrees C. Avian Pathology, 42, 248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, Y. , Zhao, Y. , Liu, J. , He, X. , Wang, B. , Fu, S. , … Luo, B. (2020). Effects of temperature variation and humidity on the death of COVID‐19 in Wuhan, China. Science of the Total Environment, 724, 138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NSW Government (2020a). Data.NSW: NSW COVID‐19 data. Retrieved from https://data.nsw.gov.au/nsw‐covid‐19‐data [Google Scholar]
- NSW Government (2020b). Data.NSW: COVID‐19 cases by notification date, location. Retrieved from https://data.nsw.gov.au/dataset/nsw‐covid‐19‐tests‐by‐location‐and‐result [Google Scholar]
- Qi, H. , Xiao, S. , Shi, R. , Ward, M. P. , Chen, Y. , Tu, W. , … Zhang, Z. (2020). COVID‐19 transmission in Mainland China is associated with temperature and humidity: A time‐series analysis. Science of the Total Environment, 728, 138778. 10.1016/j.scitotenv.2020.138778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan, J. G. , Mu, L. N. , Huang, J. X. , Yu, S. Z. , Chen, B. H. , & Yin, J. (2005). An initial investigation of the association between the SARS outbreak and weather: With the view of the environmental temperature and its variation. Journal of Epidemiology and Community Health, 59, 186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, J. T. , Leung, K. , & Leung, G. M. (2020). Nowcasting and forecasting the potential domestic and international spread of the 2019‐nCoV outbreak originating in Wuhan, China: A modelling study. Lancet, 395, 689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao, Y. , Pan, J. , Liu, Z. , Meng, X. , Wang, W. , Kan, H. , & Wang, W. (2020). No association of COVID‐19 transmission with temperature or UV radiation in Chinese cities. European Respiratory Journal, 55(5), 2000517. 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo, C. , Kaushal, S. , & Yeo, D. (2020). Enteric involvement of coronaviruses: Is faecal–oral transmission of SARS‐CoV‐2 possible? Lancet Gastroenterology & Hepatology, 5, P335–337. 10.1016/S2468-1253(20)30048-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, Y. , & Xie, J. (2020). Association between ambient temperature and COVID‐19 infection in 122 cities from China. Science of the Total Environment, 724, 138201. 10.1016/j.scitotenv.2020.138201 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from NSW.Data and the Australian Bureau of Meteorology. These data were derived from the following resources available in the public domain: https://data.nsw.gov.au/dataset/nsw‐covid‐19‐tests‐by‐location‐and‐result and http://www.bom.gov.au/nsw/observations/map.shtml.


