INTRODUCTION
Impetigo is a contagious infectious dermatosis caused by Staphylococcus aureus or group A beta‐hemolytic Streptococcus pyogenes, or both. 1 , 2 Children 2 to 5 years of age, especially in both resource‐poor countries and underprivileged populations within high‐income countries, are often involved, but persons of any age can be affected. 3 , 4 Here, we describe a case of goggle‐mask‐related impetigo in a nurse at the time of coronavirus disease (COVID‐19) pandemic.
Case report
A 24‐year‐old female nurse of the intensive care unit developed three itchy, erythematous, exudative, and crusted plaques on her face in the past 4 weeks. The lesion was initially erythema with several yellow blisters limited to the right side of perioral skin. She sought medical care at the hospital where she works and was diagnosed with herpes simplex. She was treated with oral acyclovir and topical acyclovir cream. However, the lesion continued to progress and gradually extended to the left side of the perioral and periorbital skin. Then, the patient visited our clinic in February 2020. Before the lesions appeared, she engaged in clinical frontline work and wore goggles and a mask for at least 12 hours daily during the COVID‐19 pandemic.
She denied any prior medical history and was afebrile. Physical examination revealed the presence of red plaques covered with honey‐colored crusts, distributed in the perioral and periorbital skin (Figure 1a‐d). Some of the lesions had shallow erosions and exudations. Regional lymph nodes were not palpable. Secretion smear staining showed the presence of Gram‐positive cocci. Subsequently, bacterial culture and drug sensitivity test from perioral and periorbital skin lesions were performed, isolating Methicillin‐sensitive S. aureus. Necessary laboratory tests were conducted and were within normal limits.
FIGURE 1.
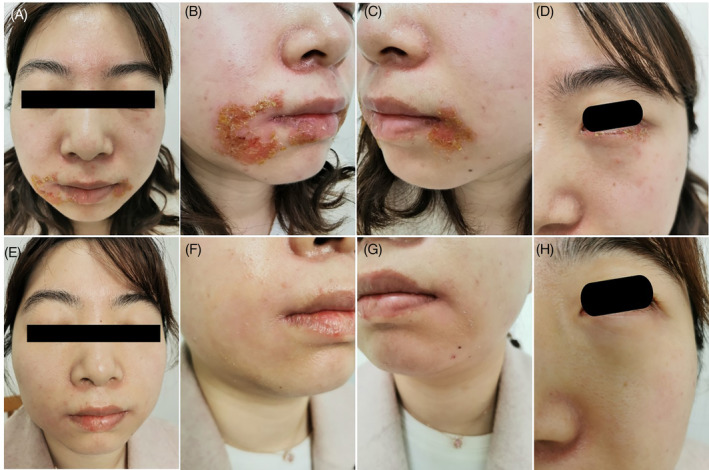
Clinical images. Skin lesions of the patient with goggle‐mask‐related impetigo at the initial visit, A‐D, and subsided skin lesions after 4 weeks of treatment, E‐H
With these results, a diagnosis of goggle‐mask‐related impetigo was made. The patient was instructed to rest at home, stop wearing goggles and masks, and apply topical 2% fusidic acid cream twice daily. The lesions were completely resolved after 7 days of treatment (Figure 1e‐h).
DISCUSSION
Impetigo is usually a self‐limiting infection, with some cases persisting for several weeks. 2 Therefore, antibiotic treatment is often initiated for a quicker cure and to prevent the spread to others. 5 , 6 The duration of this case was 4 weeks since it was initially misdiagnosed as herpes simplex, probably because the initial site of pathogenesis was perioral skin and the lesion presented as multiple vesicles with an erythematous base, characteristic of both impetigo and herpes simplex. Hence, these were differentiated by secretion smear staining and bacterial culture. The skin lesions promptly subsided with correct diagnosis and treatment.
Many bacteria inhabit healthy skin; some types, especially S. aureus, intermittently colonize the nasal, axillary, pharyngeal, or perineal areas and have varying risks of infecting other skin surfaces. 5 , 7 These bacteria can lead to the infection of susceptible skin and various predisposing factors, such as high humidity, skin trauma, malnutrition, increase the risk of infection and transmission. 7 In this case, the skin lesions are located in the perioral and periorbital areas, corresponding to the coverage areas of goggles and masks. Our patient wore goggles and a mask for lengthy periods daily, which led to a moist occlusive environment where S. aureus thrived and caused an infection. She had tiresome and lengthy clinical work every day, an irregular diet, and lack of rest during the pandemic, further predisposing her to disease progression. After the patient complied with the treatment, we acquired a favorable curative effect.
At the time of the COVID‐19 pandemic, health care workers actively take care of COVID‐19 sufferers; meanwhile, they should pay attention to self‐protection, especially from goggle‐mask‐related skin diseases. We surely can get through difficulties together and win the battle against the coronavirus disease.
CONFLICT OF INTEREST
All authors declare no conflicts of interest.
INFORMED CONSENT
Informed consent was obtained from the participant included in this study.
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current are available from the corresponding author.
ACKNOWLEDGMENT
We thank Hong Yang (Shanghai Dermatology Hospital) for her technical support in the bacterial identification.
Qian Yu and Wei Li contributed equally to this work.
Funding information Science and Technology Commission of Shanghai Municipality , Grant/Award Number: 18411969700; Shanghai Municipal Commission of Health and Family Planning, Grant/Award Number: 20194Y0337
REFERENCES
- 1. Koning S, van der Sande R, Verhagen AP, et al. Interventions for impetigo. Cochrane Database Syst Rev. 2012;1:CD003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hartman‐Adams H, Banvard C, Juckett G. Impetigo: diagnosis and treatment. Am Fam Physician. 2014;90:229‐235. [PubMed] [Google Scholar]
- 3. Cole C, Gazewood J. Diagnosis and treatment of impetigo. Am Fam Physician. 2007;75:859‐864. [PubMed] [Google Scholar]
- 4. Bowen AC, Mahé A, Hay RJ, et al. The global epidemiology of impetigo: a systematic review of the population prevalence of impetigo and pyoderma. PLoS One. 2015;10:e0136789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feaster T, Singer JI. Topical therapies for impetigo. Pediatr Emerg Care. 2010;26:222‐227. quiz 228–231. [DOI] [PubMed] [Google Scholar]
- 6. Loadsman MEN, Verheij TJM, van der Velden AW. Impetigo incidence and treatment: a retrospective study of Dutch routine primary care data. Fam Pract. 2019;36:410‐416. [DOI] [PubMed] [Google Scholar]
- 7. Bangert S, Levy M, Hebert AA. Bacterial resistance and impetigo treatment trends: a review. Pediatr Dermatol. 2012;29:243‐248. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current are available from the corresponding author.


