Abstract
The pandemic outbreak of the novel coronavirus epidemic disease (COVID-19) is spreading like a diffusion-reaction in the world and almost 208 countries and territories are being affected around the globe. It became a sever health and socio-economic problem, while the world has no vaccine to combat this virus. This research aims to analyze the connection between the fast spread of COVID-19 and regional climate parameters over a global scale. In this research, we collected the data of COVID-19 cases from the time of 1st reported case to the 5th June 2020 in different affected countries and regional climatic parameters data from January 2020 to 5th June 2020. It was found that most of the countries located in the relatively lower temperature region show a rapid increase in the COVID-19 cases than the countries locating in the warmer climatic regions despite their better socio-economic conditions. A correlation between metrological parameters and COVID-19 cases was observed. Average daylight hours are correlated to total the COVID-19 cases with a coefficient of determination of 0.42, while average high-temperature shows a correlation of 0.59 and 0.42 with total COVID-19 cases and death cases respectively. The finding of the study will help international health organizations and local administrations to combat and well manage the spread of COVID-19.
Keywords: COVID-19, Regional climate, Average high temperature, Average low temperature, Daylight hours
Graphical abstract
Highlights
-
•
The study explores the effect of regional climatic conditions on the spread of COVID-19.
-
•
The regional climate parameters are important factors that may trigger the spread of the COVID-19.
-
•
The fast-spreading of COVID-19 has an association with average high and low temperatures.
-
•
The average daylight hours have a connotation with the spreading rate of pandemic disease.
1. Introduction
The pandemic diseases have been some of the most distressing happenings in the history of mankind. The Black Death sponged about one-third of the total European population and the Spanish Flu in 1918 affected more human beings than the entire victims of the 1st World War (Davis et al., 2018; Decaro and Lorusso, 2020; Djalante et al., 2020; Gould, 2009; Hussain et al., 2020; Kandel et al., 2020; Keilman, 2019; Liu et al., 2020d; Malik et al., 2020; Molineri et al., 2017; Salam et al., 2020). The epidemic outbreak of Swine Flu, Zika, and Ebola Virus had caused worldwide panic, while the outbreak of novel coronavirus (nCoV) and Middle East Respiratory Syndrome (MERS) caused severe loss of human life and economic value (Altamimi and Ahmed, 2019; Bhowmick et al., 2020; Chan et al., 2011; Decaro and Lorusso, 2020; Hoogeveen, 2020; Lin et al., 2018; Liu et al., 2020d; Paz and Semenza, 2016; Zhang et al., 2020).
Human beings already facing significant global challenges of water scarcity, food security, and climate change (Iqbal et al., 2018a; Iqbal et al., 2019; Iqbal et al., 2018b; Yokomatsu et al., 2020), came under a swear attack of epidemic COVID-19 in December 2019, in Wuhan, a city of China (Burki, 2020; Chinazzi et al., 2020; World Health Organization, 2020a). Initially, the virus was acknowledged by the Chinese health care administration as of January 07, 2020 (Millán-Oñate et al., 2020). The COVID-19 also entitled as novel coronavirus causes severe respirational problems in effected patients (Burki, 2020; Chinazzi et al., 2020; World Health Organization, 2020b).
The virus spread from Wuhan city of China and affected more than 210 countries and territories of the world (World Health Organization, 2020a; Zu et al., 2020). Although, most of the novel COVID-19 cases indicate mild symptoms and recover from this disease due to early precautionary measures and self-immunization systems (Lai et al., 2020). Yet many cases are reported with severe symptoms which caused a high number of deceases in many parts of the world i.e. Italy (15,887), Spain (13,055), USA (9624), France (8078), UK (4934), Iran (3739), China (3331), Malaysia (62), India (118) Hong Kong (4), Thailand (26), and Pakistan (50) with a varying number of closed cases outcomes ranging from 0.4 to 50% (Ji et al., 2020; Surveillances, 2020).
COVID-19 spreading continuously and created one of the biggest panics of the 21st century with a lockdown of more than 6 billion people of the planet. The virus is considered as one of the most lethal invisible enemies known to the human being, where its fast transmission mechanism remains inadequately understood (Altamimi and Ahmed, 2019). Many contagious epidemics occur and wane away with a change in the weather. Flu and other seasonal diseases such as norovirus vomiting bug, pneumonia come in winter. Other diseases, such as typhoid and summer fever, be likely to peak for the period of the summer season. The infection of Measles cases declines in the temperate climatic regions during the summer seasons, while the infection spread peaks in the tropical regions especially in the dry period (Altamimi and Ahmed, 2019; Chan et al., 2011; Darniot et al., 2018; Davis et al., 2018; Gould, 2009; Jones, 2016; Keilman, 2019; Lee and Chowell, 2017; Merle et al., 2018; Molineri et al., 2017; Morin et al., 2018; Paz and Semenza, 2016).
The thrilling weather condition and influence of temperature variation also triggered the spread of the West Nile virus in the European world (Bhowmick et al., 2020; Liu et al., 2020d; Zhang et al., 2020). Researchers are interested in knowing whether there will be any similarity with the fast spread of COVID-19 or otherwise. Ever since it was first identified in mainland China in the mid of December 2019, the virus has spread very abruptly, with the number of cases increasing more severely in cooler regions such as European and North American countries. Many weather condition can be well-thought-out as the top forecasters of respiratory syndromes such as SARS. Hydro-meteorological variables can also have a direct association between coronaviruses and humans being via biological interaction. Climate parameters may have a link with the fast transmission rate of COVID-19 (Armitage and Nellums, 2020; Auler et al., 2020; Méndez-Arriaga, 2020; O'Reilly et al., 2020). Optimum climatic parameters such as temperature, wind speed, relative humidity, and precipitation can be considered as leading variable activating the existence and diffusion of the viruses. Furthermore, weather changes and regional climate are also verily associated with the pneumonia fatalities (Bhowmick et al., 2020; Hoogeveen, 2020; Liu et al., 2020a; Liu et al., 2020b; Ma et al., 2020; Qi et al., 2020; Schwartz, 2020; Tobías and Molina, 2020; Wang et al., 2020; Zambrano-Monserrate et al., 2020; Zhang et al., 2020).
Numerous major pandemic outbreaks have occurred in the regions where the weather intensity is extremes, leading to rumor that the pandemic might begin to decline with the influx of change in weather. Generally, the largest contiguous syndromes outbreak in the regions of cooler weather, leading to the theories that high temperatures might begin to the tail of in the summer season. It remains uncertain whether or not high temperatures of certain degrees would successfully eradicate the COVID-19, according to experts. In the meantime, COVID-19 is a new virus and no research to prove these theories so far from validation. Research on regional weather parameters and COVID-19 is also quite limited. The following study opens new ways to understand and prevent the spread of COVID-19 with its relation to climatic conditions and related parameters.
2. Materials and methods
2.1. Study area
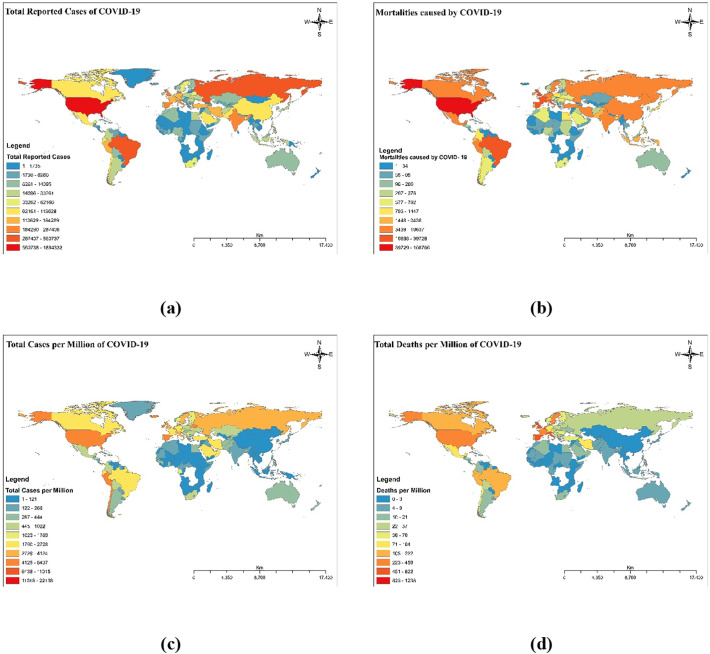
The study is accompanied by the countries and territories of the entire world. Computerized data of the COVID-19 cases until 5th June 2020 was obtained from the official health department sources of all countries as well as from the world info meter of COVID-19 (https://www.worldometers.info/coronavirus/). Fig. 1 shows the heat maps of confirmed cases, death cases, cases per million population, and death per million population as of 5th June 2020 over 210 countries and territories of the world. Furthermore, data of death cases, closed outcomes cases, cases per million population were also obtained from similar sources. Regional daily and monthly average climatological parameters of each country were obtained from the concerned meteorological stations and different international organizations to include World Meteorological Organization (https://www.wmo.int/datastat/wmodata_en.html), NASA Earth Observatory (https://earthobservatory.nasa.gov/), NASA Earth Observations (NEOs) (https://neo.sci.gsfc.nasa.gov/), Climate data guide (https://climatedataguide.ucar.edu/climate-data), Climate data online (https://www.ncdc.noaa.gov/cdo-web/), Global climate change (https://climate.nasa.gov/), and Monthly climate reports (NOVA). Monthly average temperature and daylight hours were calculated by averaging the daily based value. Furthermore, an overall average from January 2020 to May 2020 was calculated to find the correlation between climate parameters and COVID-19 spread. A simple linear association of the reported cases of COVID-19 and metrological parameters was drawn.
Fig. 1.
The pandemic of COVID-19 over the entire world as of 5th June 2020, (a) total reported cases worldwide, (b) reported death cases worldwise, (c) reported cases per million population, and (d) reported death cases per million population.
2.2. Statistical analysis
The coefficient of determination (R2) was applied to analyze the association among regional climatological parameters with average data of high temperature, low temperature and day light hours with total and death cases of COVD-19 reported until 5th June 2020. R2 is an estimator used for the analyzing the mutual association among two different data sets. It indicates that how one set of data set is well associate the flow of other data sets. It shows the level of variability among data sets.
3. Results and discussion
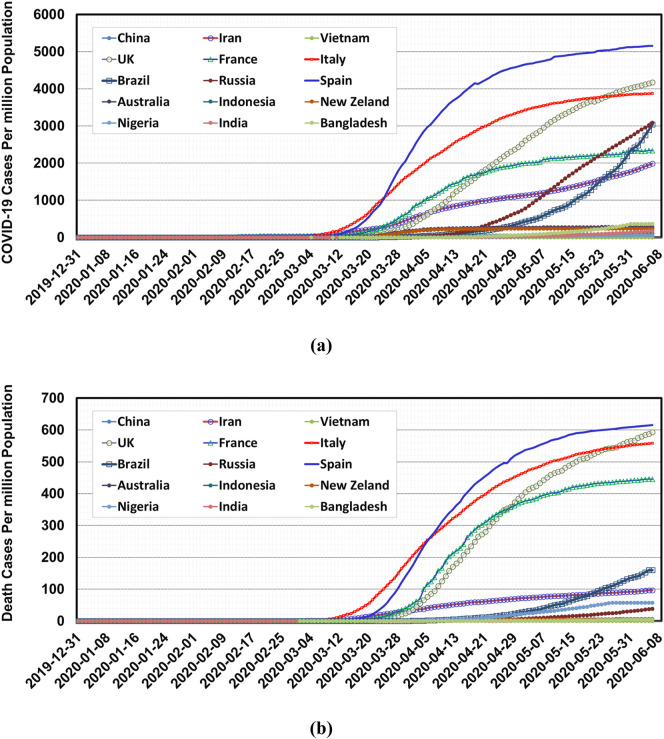
The occurrence of total cases and death cases, on the timeline, reported in the different countries of the world is shown in Fig. 2 . The number of COVID-19 cases increases at an exponential rate from the 1st case identification to the selected study period i.e., 5th June 2020. Some countries show a very rapid increase in the COVID-19 transformation despite their better socioeconomic condition and value of life. Most of the cooler regions especially European and North American countries show a rapid increase in the COVID spread. USA, Italy, Spain, France, Germany, UK have a fast spread of COVID cases than India, Pakistan, Bangladesh, Indonesia, and Malaysia despite their better quality of life. Countries like Pakistan, India, Bangladesh, Indonesia are relatively warm and humid countries (together they account for 25% of the world population) but have slow growth of COVID-19 cases. The virus does not multiply outside the living bodies but the contagious virus may retain on different surfaces where the duration of retention of the virus is influenced prominently by local weather conditions. Unclean surfaces, weather conditions, and human mass gatherings are notorious to be momentous vectors in the profligate contagions in the community and regions. The COVID associated to human beings with the seasonal flu and common cold was testified to remain workable only for a short duration of 3 h on the different surfaces in an arid environment, though it remains workable for more duration in humid environment Influenza and RSV viruses reported viable for 2 and 6 h respectively after drying on surfaces (Artika et al., 2020; Beeler and Eichelberger, 2013; Crisci et al., 2013; Liu et al., 2020d; Zhang et al., 2020). Human coronavirus (229E) on aerosolized shape is mostly less stable in high humidity and temperature (Altamimi and Ahmed, 2019; Brugger and Rubel, 2009; Chan et al., 2011; Gould, 2009; Hoogeveen, 2020; Li et al., 2018; Liu et al., 2020a; Liu et al., 2020c; Lyth and Holbrook, 2015; Ma et al., 2020; Mas-Coma et al., 2020; Morin et al., 2018; Nicholson and Munoz, 2018; Otter et al., 2016; Schwartz, 2020; Sirisena and Noordeen, 2014).
Fig. 2.
Total coronavirus cases in different countries of the world (a) Total confirmed cases per million population and (b) total death cases per million population by COVID-19.
In the present study, the authors suggested that the COVID-19 virus can stay alive after drying at a daily high temperature and in humid condition for at least two weeks. In a liquid substance, SAR-COV-2 can be stable up to 3 weeks at room temperature but can be killed easily at the high temperature of 56 °C up to 15 min (Abduljalil and Abduljalil, 2020; Chow et al., 2003; Clark, 1993; Lee and Qureshi, 2013). Therefore, results revealed that coronavirus is a more stable pandemic that can transmit by indirect contact or fomites. Moreover, this situation revealed that tainted surfaces can show a vital role in the fast diffusion of infection in the local community, isolation centers, and hospitals. The present study revealed that unswerving droplet transmission is a more dangerous and important route of virus broadcast from the infected carrier. Moreover, fomites and environmental contaminated aerosols may perhaps play a foremost role in the fast-spreading of the virus. In nutshell, fomites may be a strong source of fast transmission of the virus. Besides, to avoid from droplet transmission, frequent hand washing for at least 20 s is recommended by WHO (Abduljalil and Abduljalil, 2020; Akkina et al., 2019; Darniot et al., 2018; Hoogeveen, 2020; Kandel et al., 2020; Lee and Qureshi, 2013; Lee and Chowell, 2017; Lin et al., 2018; Merle et al., 2018; Nicholson and Munoz, 2018; Nicola et al., 2020; Segars et al., 2020; Wang et al., 2020; Zambrano-Monserrate et al., 2020).
A present study, revealed that climate parameters i.e. high temperature, as well as higher relative humidity, have a significant effect on in-activation of COVID-19 transmission while low relative humidity and low temperature support the prolong survival of COVID-19 virus on infected surfaces (i.e. wood, metal, and glass) (Brugger and Rubel, 2009; Chan et al., 2011; Darniot et al., 2018; Davis et al., 2018; Gould, 2009; Jones, 2016; Li et al., 2018; Lyth and Holbrook, 2015; Morin et al., 2018; Paz and Semenza, 2016; Sirisena and Noordeen, 2014).
Furthermore, another study has shown that during the pandemic outbreak, the daily infected cases of COVID-19 were 18.18 fold higher in days with a lower air temperature versus higher temperature days i.e. Hong Kong and another part of the world. Collectively, this observation may be described that why some Asian countries in the tropical region (at high temperatures with higher relative humidity) i.e. Malaysia, Thailand, and Indonesia are less affected by a coronavirus. COVID-19 virus can stay alive for two (2) weeks in low humidity and low-temperature conditions which maybe guide the fast virus diffusion in the respective country as in Hong Kong which track down in subtropical zone (Ahmadi et al., 2020; Altamimi and Ahmed, 2019; Bhandari et al., 2020; Bhowmick et al., 2020; Liu et al., 2020c; Robert et al., 2019; Schwartz, 2020; Smith, 2019).
Moreover, other ecological aspects i.e. day sunlight, average maximum temperature, and the average minimum temperature had shown association with coronavirus pandemic disease outbreak transmission rate. The dynamic nature of this pandemic disease also involves multiple other factors i.e. out-door and indoor environment, physical properties of virus (i.e. shape, size), space, hygiene and genetic changes in different regions. Some authors find changes in shape in the size of the virus in a different region of the world (Hansen et al., 2015; Kone et al., 2017; Otter et al., 2016; Sprygin et al., 2019; Turnage and Gibson, 2017).
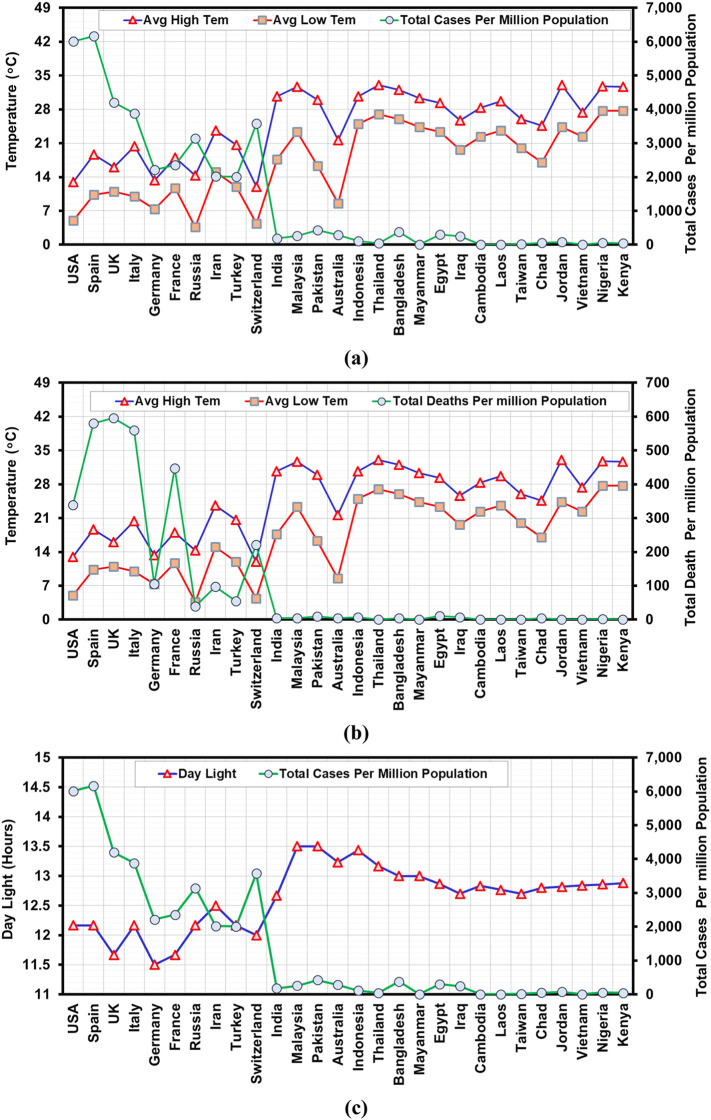
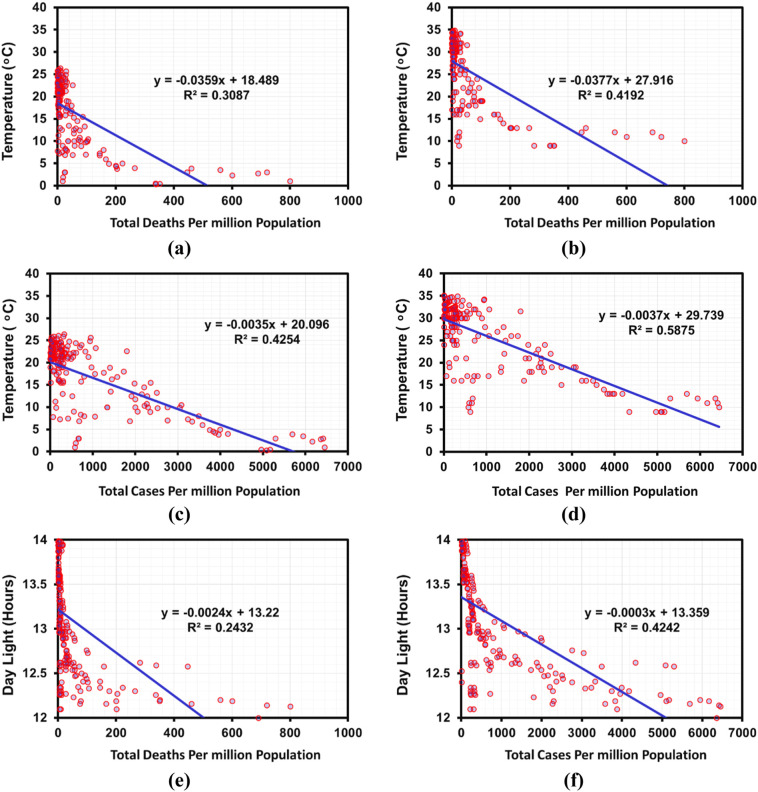
Fig. 3, Fig. 4 show the association of meteorological parameter and COVID-19 total and death cases. Average low temperature, average high temperature and daylight hours show a stronger relationship with the total number of reported cases than death cases in different countries of the world. The study provides a picture of COVID-19 cases against meteorological conditions globally. The study observed a positive linear correlation among total COVID-19 cases and average high and low temperatures with a coefficient of determination of 0.4016 and 0.4668, respectively, while a linear correlation among total COVID-19 death cases and average high and low temperatures with a coefficient of determination of 0.1987 and 0.3008, respectively. Furthermore, a positive linear correlation was also observed among average daylight hours and total COVID reported cases with a coefficient of determination of 0.3698 and death cases with a coefficient of determination of 0.4834. This association is supported by the previous studies which show the relationship between regional meteorological conditions and transmissions of different contagious diseases such as common cold flu and human coronaviruses (Coverstone et al., 2019; Keilman, 2019; Li et al., 2018; Liu et al., 2020b; Ma et al., 2020; Otter et al., 2016; Pattison, 2020; Paz and Semenza, 2016; Yang and Sarfaty, 2016). Conversely, to our study of COVID-19 which outbreak in winter season in Wuhan City, China, Altamimi and Ahmed (2019) reported that the fast spread of novel coronavirus, MERS-CoV which outbreak in summer season in Riyadh is increased with high temperature, low wind speed, as well as the high ultraviolet index, and low relative humidity.
Fig. 3.
Total COVID-19 cases per million population and climatic factors, (a) Total cases per million population and average high temperature, (b) Total death cases per million population and average low temperature, and (c) Total cases per million population and average daylight hours.
Fig. 4.
Shows relationship between COVID-19 cases per million population in the different countries of the world until 5th June and climatic parameters (a) average low-temperature vs a total number of death cases per million population, (b) average high temperature vs death cases per million population, (c) average low-temperature vs total number of reported cases per million population (d) average high-temperature vs total number of reported cases per million population (e) average daylight hours vs total number of death cases per million population, and (f) average daylight (hours) vs total number of reported cases per million population.
Furthermore, we have explored the linear correlation between ambient temperature and infected total confirmed COVID-19 cases with the help of the coefficient of determination model. The average daily temperature and daylight hours for the study period from 1st COVID case detection to the 5th June shows the positive linear relationship in the different countries of the world, indicating that as the local weather conditions altered the transmission of the virus may be declined. Previous studies have shown that local weather condition such as temperature, humidity, and precipitation is also a vital aspect in the existence and broadcast of other coronaviruses, like influenza viruses, retroviruses, MERS, poxviruses, Severe acute respiratory syndrome (SARS), and paramyxoviruses (Altamimi and Ahmed, 2019; Beeler and Eichelberger, 2013; Hansen et al., 2015; Jones, 2016; Kone et al., 2017; Lee and Qureshi, 2013; Lee and Chowell, 2017; Li et al., 2018; Lin et al., 2018; Morin et al., 2018; Otter et al., 2016; Paz and Semenza, 2016; Salehuddin et al., 2017; Yang and Sarfaty, 2016). Previous studies were only confined to a single country and smaller region, but the following study analyzed the most countries of the world.
Some studies conducted in Hong Kong, Beijing, Guangzhou and Taiyuan on SARS cased and conclude that 16–28 °C temperature is optimum. While, other studies found the negative relationship of temperature and SARS transmission in both countries Beijing and Hong Kong during 2003 (Abduljalil and Abduljalil, 2020; Chan et al., 2011; Chow et al., 2003; Decaro and Lorusso, 2020; Lin et al., 2018; Otter et al., 2016). Casanova et al. (2010) found that viruses were inactive more rapidly at 20 °C than 4 °C.
Furthermore, de Sousa et al. (2014) perform the test in the laboratory for coronavirus laboratory testing on coronavirus and revealed that virus was stable for 5 days on a smooth surface in between −25 °C to 22 °C but its visibility swiftly vanished at high temperature e.g. 38 °C and above. van Doremalen et al. (2020) also revealed that virus MERS-CoV was also not as active at high temperatures. Moreover, many other studies revealed that moderate temperature range is optimum and feasible for coronavirus growth and expansion but in high temperature, was harmful to it viability and also help in the reduction of its spreading (Loeffelholz and Tang, 2020). Therefore, further laboratory testing and experiments are also dire need to be done further strengthen of this myth (Corman et al., 2012; de Sousa et al., 2014; Shahkarami et al., 2015). In Pakistan and many other countries are having long and hot summer so it might be a chance of less effected by COVID-19.
In nutshell, minimum temperature or below 3 °C in the winter season leads to high risk for its fast transmission in those countries, which are having long and cold winter. This provides very remarkable information for policymakers, may be COVID-19 exist for a long time until the development of a proper and effective vaccine (Liu et al., 2020c; Ma et al., 2020; Robert et al., 2019; Schwartz, 2020; Smith, 2019; Tobías and Molina, 2020). There are some limitations, i.e. we did not analyze the results in subgroup bases, i.e. gender, different age ranges, due to maximum missing information worldwide.
Without a proper vaccine, social distancing is the only new norm adopted to reduce the transmission effect of COVID-19. When a few cases of COVID-19 have been reported than every country announces the lockdown and SOP of social distancing. Yezli and Khan (2020) reported that the implementation of social distancing rules and regulations is a challenge due to its various norms of society, i.e. social and religious activities, annual hosting of various festivals, national and international festivals, and religious mass gatherings.
Moreover, it has been confirmed that the COVID-19 can spread through droplets created by infected human coughing or sneezing or touching. To overcome the droplet infection rate, 1.83 m distance for social distancing is recommended, which is based on assumptions. However, no study was conducted yet on droplet transmission in the air (wind) and relative humidity (RH). Feng et al. (2020) validated computational fluid-particle dynamics (CFPD) model to simulate the transient transport, condensation/evaporation, and deposition of SARS-CoV-2 laden droplets (2–2000 μm) emitted by coughs, with different environmental wind velocities (0–16 km) and RHs (40% and 99.5%). The social distances were maintained at 1.83 and 3.05 m (6 and 10 ft). The facial covering effect is also under investigation. Numerical results revealed that micro-droplets can travel in the air more than 3.05 m distance. RH also helped in increasing the droplet size. Moreover, it is concluded that, within complex environmental wind and RH conditions, social distancing policy of 1.83 m (6 ft) is not sufficient to protect the person. Coughing or sneezing droplets of an infected person can infect the other human in less than 5 s. Therefore, a social distancing longer than 1.83 m (6 ft) needs to be considered.
Some countries i.e. Australia, USA, Italy, France, the UK, and Europe having a high literacy rate and quality of life as compared to other under developing countries i.e. Pakistan and India. Without proper social distancing and wearing masks, per million effected cases and per a million deaths are less in Pakistan and India because both countries have a high temperature in March–June as compare to other countries. Australia is having a high population density at its habitat area because in the mid of Australia, there is a desert and very less population density is there. On the other hand, populated areas are under moderate climate conditions, which cause a high/less number of COVID-19 cases.
4. Conclusion
This study explored the effect of native weather disorders on the fast spread of COVD-19 worldwide. The novel coronavirus is convincingly influenced by the local weather conditions in the different parts of the world from their 1st case identification to the 5th June 2020. The spread of the COVID-19 appears to be faster in cooler regions. The average temperature and daylight hours have shown a positive association towards the spread rate of COVID-19. Hence, regional meteorological parameters (aerosols, maximum and minimum temperature, day length, etc.) are among the contributors to the fast spread of coronavirus over most countries of the world. This study gives evidence that the fast spread of cases of COVID-19 could diminish when the local weather conditions become warmer. Most of the Asian countries have a high temperature in May–June, they have shown less number of affected cases per million population i.e. Vietnam, Laos, Pakistan, India, etc. This study suggest that along with proper management such as social distancing and hand washing, long summer may also slow down the spread of pandemic disease. This study provides useful inferences for health departments and decision-makers in defeating and understanding the fast spread of COVID-19.
CRediT authorship contribution statement
Muhammad Mazhar Iqbal:Conceptualization, Formal analysis, Investigation, Writing - original draft, Writing - review & editing.Irfan Abid:Conceptualization, Formal analysis, Investigation.Saddam Hussain:Conceptualization, Formal analysis, Investigation.Naeem Shahzad:Conceptualization.Muhammad Sohail Waqas:Conceptualization.Muhammad Jawed Iqbal:Conceptualization.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
This research work was supported by the National University of Science and Technology. The authors are grateful to Mr. Asif Ali, School of Civil Engineering, National University of Science and Technology, Islamabad, for helping in GIS based heat mapping the COVID case. Furthermore, authors also thankful for providing free data sources by worldometer and different climatic data portals of NASA, JAXA, and ESA.
Editor: Jianmin Chen
References
- Abduljalil J.M., Abduljalil B.M. Epidemiology, genome, and clinical features of the pandemic SARS-CoV-2: a recent view. New Microbes New Infect. 2020;35 doi: 10.1016/j.nmni.2020.100672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akkina R., Garry R., Bréchot C., Ellerbrok H., Hasegawa H., Menéndez-Arias L. 2019 meeting of the global virus network. Antivir. Res. 2019;172 doi: 10.1016/j.antiviral.2019.104645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. J. Infect. Public Health. 2019;13:704–708. doi: 10.1016/j.jiph.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage R., Nellums L.B. Water, climate change, and COVID-19: prioritising those in water-stressed settings. Lancet Planet. Health. 2020;4:e175. doi: 10.1016/S2542-5196(20)30084-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artika I.M., Wiyatno A., Ma’roef C.N. Pathogenic viruses: molecular detection and characterization. Infect. Genet. Evol. 2020;81 doi: 10.1016/j.meegid.2020.104215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auler A.C., Cássaro F.A.M., da Silva V.O., Pires L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeler J.A., Eichelberger M.C. Influenza and respiratory syncytial virus (RSV) vaccines for infants: safety, immunogenicity, and efficacy. Microb. Pathog. 2013;55:9–15. doi: 10.1016/j.micpath.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari D., Bi P., Sherchand J.B., Dhimal M., Hanson-Easey S. Climate change and infectious disease research in Nepal: are the available prerequisites supportive enough to researchers? Acta Trop. 2020;204 doi: 10.1016/j.actatropica.2020.105337. [DOI] [PubMed] [Google Scholar]
- Bhowmick S., Gethmann J., Conraths F.J., Sokolov I.M., Lentz H.H.K. Locally temperature-driven mathematical model of West Nile virus spread in Germany. J. Theor. Biol. 2020;488 doi: 10.1016/j.jtbi.2019.110117. [DOI] [PubMed] [Google Scholar]
- Brugger K., Rubel F. Simulation of climate-change scenarios to explain Usutu-virus dynamics in Austria. Prev. Vet. Med. 2009;88:24–31. doi: 10.1016/j.prevetmed.2008.06.023. [DOI] [PubMed] [Google Scholar]
- Burki T. Outbreak of coronavirus disease 2019. Lancet Infect. Dis. 2020;20:292–293. doi: 10.1016/S1473-3099(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S., Lam S.Y., Poon L.L., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011:734690. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow K.Y.C., Hon C.C., Hui R.K.H., Wong R.T.Y., Yip C.W., Zeng F. Molecular advances in severe acute respiratory syndrome-associated coronavirus (SARS-CoV) Genomics Proteomics Bioinforms. 2003;1:247–262. doi: 10.1016/S1672-0229(03)01031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark M.A. Bovine coronavirus. Br. Vet. J. 1993;149:51–70. doi: 10.1016/S0007-1935(05)80210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman V., Müller M., Costabel U., Timm J., Binger T., Meyer B. Assays for laboratory confirmation of novel human coronavirus (hCoV-EMC) infections. Eurosurveillance. 2012;17 doi: 10.2807/ese.17.49.20334-en. [DOI] [PubMed] [Google Scholar]
- Coverstone A.M., Wang L., Sumino K. Beyond respiratory syncytial virus and rhinovirus in the pathogenesis and exacerbation of asthma: the role of metapneumovirus, bocavirus and influenza virus. Immunol. Allergy Clin. N. Am. 2019;39:391–401. doi: 10.1016/j.iac.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crisci E., Mussá T., Fraile L., Montoya M. Review: influenza virus in pigs. Mol. Immunol. 2013;55:200–211. doi: 10.1016/j.molimm.2013.02.008. [DOI] [PubMed] [Google Scholar]
- Darniot M., Pitoiset C., Millière L., Aho-Glélé L.S., Florentin E., Bour J.-B. Different meteorological parameters influence metapneumovirus and respiratory syncytial virus activity. J. Clin. Virol. 2018;104:77–82. doi: 10.1016/j.jcv.2018.05.002. [DOI] [PubMed] [Google Scholar]
- Davis J.K., Vincent G.P., Hildreth M.B., Kightlinger L., Carlson C., Wimberly M.C. Improving the prediction of arbovirus outbreaks: a comparison of climate-driven models for West Nile virus in an endemic region of the United States. Acta Trop. 2018;185:242–250. doi: 10.1016/j.actatropica.2018.04.028. [DOI] [PubMed] [Google Scholar]
- Decaro N., Lorusso A. Novel human coronavirus (SARS-CoV-2): a lesson from animal coronaviruses. Vet. Microbiol. 2020;244 doi: 10.1016/j.vetmic.2020.108693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djalante R., Lassa J., Setiamarga D., Sudjatma A., Indrawan M., Haryanto B. Review and analysis of current responses to COVID-19 in Indonesia: period of January to March 2020. Prog. Disaster Sci. 2020;6 doi: 10.1016/j.pdisas.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Marchal T., Sperry T., Yi H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J. Aerosol Sci. 2020;147 doi: 10.1016/j.jaerosci.2020.105585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould E. Emerging viruses and the significance of climate change. Clin. Microbiol. Infect. 2009;15:503. doi: 10.1111/j.1469-0691.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- Hansen L.J.J., Daoussi R., Vervaet C., Remon J.P., De Beer T.R.M. Freeze-drying of live virus vaccines: a review. Vaccine. 2015;33:5507–5519. doi: 10.1016/j.vaccine.2015.08.085. [DOI] [PubMed] [Google Scholar]
- Hoogeveen M.J. Pollen likely seasonal factor in inhibiting flu-like epidemics. A Dutch study into the inverse relation between pollen counts, hay fever and flu-like incidence 2016–2019. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain S., Malikb S., Cheemac M.J.M., Ashrafd M.U., Waqase M.S., Iqbalf M.M. An overview on emerging water scarcity challenge in Pakistan, its consumption, causes, impacts and remedial measures. Big Data in Water Resources Engineering (BDWRE) 2020;1:22–31. [Google Scholar]
- Iqbal M.M., Shoaib M., Agwanda P., Lee J.L. Modeling approach for water-quality management to control pollution concentration: a case study of Ravi River, Punjab, Pakistan. Water. 2018;10:1068. [Google Scholar]
- Iqbal M.M., Shoaib M., Farid H.U., Lee J.L. Assessment of water quality profile using numerical modeling approach in major climate classes of Asia. Int. J. Environ. Res. Public Health. 2018;15:2258. doi: 10.3390/ijerph15102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal M.M., Shoaib M., Agwanda P.O. The response of pollution load from coastal river waterfront on red tides in South Sea. J. Coast. Res. 2019;91:231–235. [Google Scholar]
- Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob. Health. 2020;8(4) doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.A.C. Chapter three — future scenarios for plant virus pathogens as climate change progresses. In: Kielian M., Maramorosch K., Mettenleiter T.C., editors. Advances in Virus Research. Vol. 95. Academic Press; 2016. pp. 87–147. [DOI] [PubMed] [Google Scholar]
- Kandel N., Chungong S., Omaar A., Xing J. Health security capacities in the context of COVID-19 outbreak: an analysis of international health regulations annual report data from 182 countries. Lancet. 2020;395:1047–1053. doi: 10.1016/S0140-6736(20)30553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilman L.J. Seasonal influenza (flu) Nurs. Clin. N. Am. 2019;54:227–243. doi: 10.1016/j.cnur.2019.02.009. [DOI] [PubMed] [Google Scholar]
- Kone N., Asare-Bediako E., Koita O., Kone D., Winter S. Seasonal and spatial variation in the prevalence of viral diseases and associated aphid-borne viruses in cucurbits in Cote d’Ivoire. Ann. Agric. Sci. 2017;62:227–234. [Google Scholar]
- Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Chowell G. Exploring optimal control strategies in seasonally varying flu-like epidemics. J. Theor. Biol. 2017;412:36–47. doi: 10.1016/j.jtbi.2016.09.023. [DOI] [PubMed] [Google Scholar]
- Lee N., Qureshi S.T. Other viral pneumonias: coronavirus, respiratory syncytial virus, adenovirus, hantavirus. Crit. Care Clin. 2013;29:1045–1068. doi: 10.1016/j.ccc.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Lu Y., Liu J., Wu X. Climate change and dengue fever transmission in China: evidences and challenges. Sci. Total Environ. 2018;622–623:493–501. doi: 10.1016/j.scitotenv.2017.11.326. [DOI] [PubMed] [Google Scholar]
- Lin M.-H., Moses D.C., Hsieh C.-H., Cheng S.-C., Chen Y.-H., Sun C.-Y. Disulfiram can inhibit MERS and SARS coronavirus papain-like proteases via different modes. Antivir. Res. 2018;150:155–163. doi: 10.1016/j.antiviral.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Zhang Y., Tian Y., Zheng Y., Gou F., Yang X. Epidemic features of seasonal influenza transmission among eight different climate zones in Gansu, China. Environ. Res. 2020;183 doi: 10.1016/j.envres.2020.109189. [DOI] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Hou X., Ren Z., Lowe R., Wang Y., Li R. Climate factors and the East Asian summer monsoon may drive large outbreaks of dengue in China. Environ. Res. 2020;183 doi: 10.1016/j.envres.2020.109190. [DOI] [PubMed] [Google Scholar]
- Liu Y., Lillepold K., Semenza J.C., Tozan Y., Quam M.B.M., Rocklöv J. Reviewing estimates of the basic reproduction number for dengue, Zika and chikungunya across global climate zones. Environ. Res. 2020;182 doi: 10.1016/j.envres.2020.109114. [DOI] [PubMed] [Google Scholar]
- Loeffelholz M.J., Tang Y.-W. Laboratory diagnosis of emerging human coronavirus infections—the state of the art. Emerg. Microbes Infect. 2020:1–26. doi: 10.1080/22221751.2020.1745095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyth A., Holbrook N.J. Assessing an indirect health implication of a changing climate: Ross River virus in a temperate island state. Clim. Risk Manag. 2015;10:77–94. [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik S., Hussain S., Waqas M.S. Effect of water quality and different meals on growth of Catla catla and Labeo rohita. Big Data In Water Resources Engineering (BDWRE) 2020;1:4–8. [Google Scholar]
- Mas-Coma S., Jones M.K., Marty A.M. One Health; 2020. COVID-19 and Globalization; p. 100132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735 doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merle H., Donnio A., Jean-Charles A., Guyomarch J., Hage R., Najioullah F. Ocular manifestations of emerging arboviruses: dengue fever, chikungunya, Zika virus, West Nile virus, and yellow fever. J. Fr. Ophtalmol. 2018;41:e235–e243. doi: 10.1016/j.jfo.2018.05.002. [DOI] [PubMed] [Google Scholar]
- Millán-Oñate J., Rodriguez-Morales A.J., Camacho-Moreno G., Mendoza-Ramírez H., Rodríguez-Sabogal I.A., Álvarez-Moreno C. A new emerging zoonotic virus of concern: the 2019 novel coronavirus (COVID-19) Infectio. 2020;24 [Google Scholar]
- Molineri A., Giacobino A., Pacini A., Bulacio Cagnolo N., Fondevila N., Ferrufino C. Risk factors for the presence of deformed wing virus and acute bee paralysis virus under temperate and subtropical climate in Argentinian bee colonies. Prev. Vet. Med. 2017;140:106–115. doi: 10.1016/j.prevetmed.2017.02.019. [DOI] [PubMed] [Google Scholar]
- Morin C.W., Stoner-Duncan B., Winker K., Scotch M., Hess J.J., Meschke J.S. Avian influenza virus ecology and evolution through a climatic lens. Environ. Int. 2018;119:241–249. doi: 10.1016/j.envint.2018.06.018. [DOI] [PubMed] [Google Scholar]
- Nicholson E.G., Munoz F.M. A review of therapeutics in clinical development for respiratory syncytial virus and influenza in children. Clin. Ther. 2018;40:1268–1281. doi: 10.1016/j.clinthera.2018.06.014. [DOI] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. Lancet Planet. Health. 2020;4:e172. doi: 10.1016/S2542-5196(20)30106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otter J.A., Donskey C., Yezli S., Douthwaite S., Goldenberg S.D., Weber D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J. Hosp. Infect. 2016;92:235–250. doi: 10.1016/j.jhin.2015.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattison N. End-of-life decisions and care in the midst of a global coronavirus (COVID-19) pandemic. Intensive Crit. Care Nurs. 2020;58 doi: 10.1016/j.iccn.2020.102862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz S., Semenza J.C. El Niño and climate change—contributing factors in the dispersal of Zika virus in the Americas? Lancet. 2016;387:745. doi: 10.1016/S0140-6736(16)00256-7. [DOI] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W. COVID-19 transmission in mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert M.A., Christofferson R.C., Weber P.D., Wearing H.J. Temperature impacts on dengue emergence in the United States: investigating the role of seasonality and climate change. Epidemics. 2019;28 doi: 10.1016/j.epidem.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salam M., Cheema M.J.M., Zhang W., Hussain S., Khan A., Bilal M. Groundwater storage change estimation using grace satellite data in Indus Basin. Big Data in Water Resources Engineering (BDWRE) 2020;1:13–18. [Google Scholar]
- Salehuddin A.R., Haslan H., Mamikutty N., Zaidun N.H., Azmi M.F., MMi Senin. Zika virus infection and its emerging trends in Southeast Asia. Asian Pac J Trop Med. 2017;10:211–219. doi: 10.1016/j.apjtm.2017.03.002. [DOI] [PubMed] [Google Scholar]
- Schwartz S.A. Climate change, Covid-19, preparedness, and consciousness. EXPLORE. 2020;16(3):141–144. doi: 10.1016/j.explore.2020.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segars J., Katler Q., McQueen D.B., Kotlyar A., Glenn T., Knight Z. Prior and novel coronaviruses, COVID-19, and human reproduction: what is known? Fertil. Steril. 2020;113(6):1140–1149. doi: 10.1016/j.fertnstert.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahkarami M., Yen C., Glaser C., Xia D., Watt J., Wadford D.A. Laboratory testing for Middle East respiratory syndrome coronavirus, California, USA, 2013–2014. Emerg. Infect. Dis. 2015;21:1664. doi: 10.3201/eid2109.150476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirisena P.D.N.N., Noordeen F. Evolution of dengue in Sri Lanka—changes in the virus, vector, and climate. Int. J. Infect. Dis. 2014;19:6–12. doi: 10.1016/j.ijid.2013.10.012. [DOI] [PubMed] [Google Scholar]
- Smith E. The effect of potential climate change on infectious disease presentation. J. Nurse Pract. 2019;15:405–409. [Google Scholar]
- de Sousa R., Reusken C., Koopmans M. MERS coronavirus: data gaps for laboratory preparedness. J. Clin. Virol. 2014;59:4–11. doi: 10.1016/j.jcv.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprygin A., Pestova Y., Wallace D.B., Tuppurainen E., Kononov A.V. Transmission of lumpy skin disease virus: a short review. Virus Res. 2019;269 doi: 10.1016/j.virusres.2019.05.015. [DOI] [PubMed] [Google Scholar]
- Surveillances V. China CDC Weekly 2020. Vol. 2. 2020. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China; pp. 113–122. [PMC free article] [PubMed] [Google Scholar]
- Tobías A., Molina T. Is temperature reducing the transmission of COVID-19? Environ. Res. 2020;186 doi: 10.1016/j.envres.2020.109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnage N.L., Gibson K.E. Sampling methods for recovery of human enteric viruses from environmental surfaces. J. Virol. Methods. 2017;248:31–38. doi: 10.1016/j.jviromet.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Chen K., Zhu S., Wang P., Zhang H. Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak. Resour. Conserv. Recycl. 2020;158 doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Vol. 51. 2020. Coronavirus Disease 2019 (COVID-19): Situation Report. [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease 2019 (COVID-19) Situation Report-43. 03 March 2020. [Google Scholar]
- Yang Y.T., Sarfaty M. Zika virus: a call to action for physicians in the era of climate change. Prev. Med. Rep. 2016;4:444–446. doi: 10.1016/j.pmedr.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yezli S., Khan A. COVID-19 social distancing in the Kingdom of Saudi Arabia: bold measures in the face of political, economic, social and religious challenges. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokomatsu M., Ishiwata H., Sawada Y., Suzuki Y., Koike T., Naseer A. A multi-sector multi-region economic growth model of drought and the value of water: a case study in Pakistan. Int. J. Disaster Risk Reduction. 2020;43 [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ye C., Yu J., Zhu W., Wang Y., Li Z. The complex associations of climate variability with seasonal influenza A and B virus transmission in subtropical Shanghai, China. Sci. Total Environ. 2020;701 doi: 10.1016/j.scitotenv.2019.134607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zu Z.Y., Jiang M.D., Xu P.P., Chen W., Ni Q.Q., Lu G.M. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]