Abstract
Study Design
Case-control study.
Purpose
To investigate the independent associations of back pain with sarcopenia and with back muscle degeneration, and to introduce a new risk index for back muscle degeneration.
Overview of Literature
The Asian Working Group for Sarcopenia recommends diagnosis using handgrip strength, gait speed, and skeletal muscle mass. However, these criteria do not strongly reflect back muscle degeneration.
Methods
Patients who completed a questionnaire on back-pain between October 2016 and October 2017 were enrolled in this study. Appendicular skeletal muscle index (ASMI), cross-sectional area (CSA) index, fatty infiltration (FI) rate of the paraspinal muscles, and lumbar extensor strength index (LESI) were measured and compared between no back-pain and back-pain group. Correlations between LESI and ASMI, CSA index, and FI rate were analyzed. The back-pain group was further divided according to ASMI into sarcopenia and non-sarcopenia subgroups and by our newly developed back muscle degeneration risk index based on correlation coefficients between LESI and CSA index, FI rate. Differences in ASMI, CSA index, FI rate, LESI, and Visual Analog Scale (VAS) score between subgroups were analyzed.
Results
The ASMI, CSA index, FI rate, and LESI differed significantly between back-pain and pain-free groups. The LESI demonstrated the strongest correlation with FI rate. There were no significant differences in VAS score and back muscle degeneration index in the back-pain group when divided according to the presence of sarcopenia. However, there was a significant difference in VAS score between back-pain patients when classified according to high and low back muscle degeneration risk index.
Conclusions
We suggest that the degree of back pain is more strongly associated with back muscle degeneration than with sarcopenia. This back muscle degeneration risk index, reflecting both back muscle morphology and function, could be a useful parameter for evaluation of back pain and muscle degeneration.
Keywords: Back pain, Sarcopenia, Back muscle degeneration, Cross-sectional area, Fatty infiltration Copyright
Introduction
Interest in the pathogenesis and clinical manifestations of sarcopenia has grown rapidly since the first description by Rosenberg [1]. Sarcopenia decreases muscle mass and function, thereby limiting patient activity, physical performance, and quality of life [2]. The recent upsurge in research and interest in sarcopenia is attributed to its recognition as an independent condition by the International Classification of Diseases, 10th revision, clinical modification [3]. Age-related sarcopenia is a common health problem, so evaluation and measurement of sarcopenia are important for clinical research and treatment strategies [2,4]. Back pain is one of the most common musculoskeletal symptoms of many diseases, including sarcopenia [5]. Potential causes of back pain include degeneration of the intervertebral disk, hypertrophy of the facet joint, and segmental instability [6]. Studies have explored the relationship between sarcopenia and degenerative spinal disease, including back pain [7,8], and some suggest that back muscle degeneration is another cause of back pain [9,10]. However, these studies focused only on muscle atrophy and fatty infiltration (FI), and excluded functional measures. Back muscle degeneration can be classified according to morphological change or functional decrease [2], the former using cross-sectional area (CSA) and FI rate, and the latter by lumbar extensor strength testing [11]. Lumbar extensor strength, measured using a lumbar extension dynamometer, is an important parameter in patients with back pain and functional disability [11-13]. Furthermore, muscle strength and function are better predictors of adverse outcomes than muscle mass [14].
The recently proposed diagnostic criteria of the Asian Working Group for Sarcopenia (AWGS) include calculating handgrip strength, gait speed, and skeletal muscle mass as indices of muscle strength, physical activity, and performance level [15]. However, sarcopenia according to these criteria does not necessarily reflect back muscle degeneration, so sarcopenia and back muscle degeneration may be independent factors that can induce back pain.
To the best of our knowledge, no studies have focused on indicators that reflect both morphological change and functional decrease due to back muscle degeneration. Studies evaluating factors relevant to back pain in patients with sarcopenia and (or) back muscle degeneration are also rare. Therefore, this study aimed to analyze the association between sarcopenia and back muscle degeneration and to verify the effects of sarcopenia and back muscle degeneration on back-pain severity. Additionally, we aimed to establish a risk index of back muscle degeneration using the quantified data.
Materials and Methods
1. Subjects
We conducted a prospective data-based case–control study of patients receiving bioimpedance analysis (BIA) using the Inbody720 (Inbody720; InBody Corp., Seoul, Korea), abdominopelvic computed tomography (CT, SOMATOM Definition AS+; Siemens, Munich, Germany), and lumbar extensor strength measurement using a lumbar extension dynamometer (SYSTEM 3 PRO; Biodex Medical Systems, Shirley, NY, USA) during regular health checkups at Eulji University Hospital from October 2016 to October 2017. All participants provided written informed consent, and the Institutional Review Board of Eulji University Hospital approved this study (EUH IRB file no., 2016-03-003). Subjects examined for lumbar extensor strength were requested to answer the question “Have you felt back pain enough in your daily life to take pain medications in the last 12 months?” from the modified Nordic questionnaire for musculoskeletal symptoms [16]. Those who answered “Yes” were included as back-pain subjects. All participants who complained of back pain were also asked to rate pain on a 100-mm horizontal Visual Analog Scale (VAS). Patients were excluded in cases of recent trauma (within the past 1 month), tumors, and infections. Patients answering “No” were enrolled as the control group. A total of 212 subjects (100 controls and 112 with back pain) were included in this study. Neither mean age nor sex ratio (male/female) differed between control and back-pain groups (mean age, 56.6±15.2 years [range, 28–74 years] versus 57.8±17.6 years [range, 18–77 years]; p=0.63; sex ratio, 58:42 versus 50:62; p=0.12).
2. Measurement of appendicular skeletal muscle mass
Appendicular skeletal muscle mass index (ASMI) was determined as the sum of arm and leg lean mass (kg) using the InBody720 BIA method and divided by the square of height (m2) for normalization across subjects (Fig. 1). Male subjects were classified into the sarcopenia group according to ASMI <7.0 kg/m2 (sarcopenia) and females according to ASMI <5.7 kg/m2 based on AWGS recommendations, while participants with higher values were classified into corresponding non-sarcopenia groups [15].
Fig. 1.
Appendicular skeletal muscle mass measurement using InBody 720 (InBody Corp., Seoul, Korea) bioelectrical impedance analysis.
3. Measurement of cross-sectional area and fatty infiltration of paraspinal muscles
Abdominopelvic CT was used to measure the CSA (cm2) and FI rate (%) of the paraspinal muscles (multifidus and erector spinae) at intervertebral disk levels L2–3, L3–4, and L4–5, the levels where the paraspinal muscles have highest stretching force and thus where exact muscle size can be measured [17,18]. All measurements were averaged and standardized. Images were acquired using a 120 kV CARE Dose 4D CT device with axial section thickness of 0.6 mm, and reconstructed to 0.3 mm thickness by the measured values of muscle and fat selected in the ‘Standard Algorithm 131 medium Smooth.’ The CSA was measured using the Marosis PACS system (Marotech Inc., Seoul, Korea) region of interest function by tracing the fascial boundary of the multifidus and erector spinae (Fig. 2). The measured value was normalized across subjects by dividing by the square of subject height to obtain the CSA index (cm2/m2). FI rate was measured by muscle attenuation in Hounsfield units (HUs), where FI rate equals the area with fat-specific HU divided by the whole back muscle area with variable HU. Intra- and inter-observer correlation coefficients were also calculated for CSA and FI rate of the paraspinal muscles [19] and results revealed high reliabilities for measurements of both multifidus and erector spinae muscles (0.84–0.92 and 0.81–0.93, respectively).
Fig. 2.
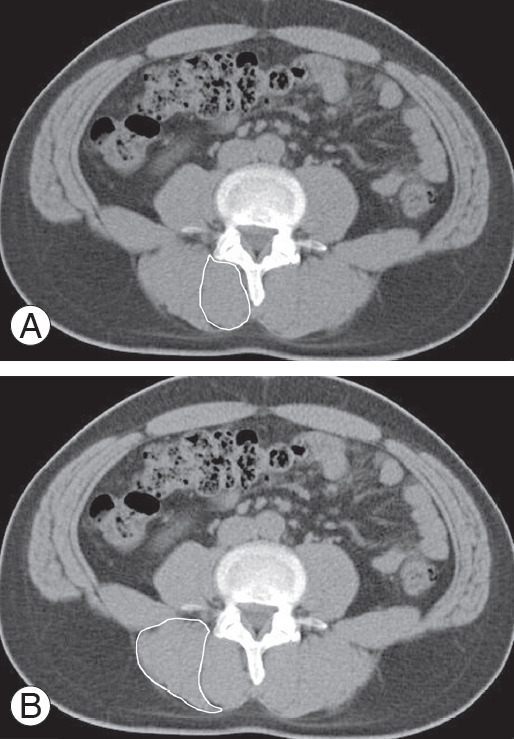
Cross-sectional area and fatty infiltration rate measurements of multifidus (A) and erector spinae (B) muscles using axial images from abdominopelvic computed tomography at the L2–3, L3–4, and L4–5 intervertebral disk levels.
4. Measurement of lumbar extensor strength
Lumbar extensor strength was measured using a lumbar extension dynamometer in the sitting position with stable pelvis. Warm-up trials and stretching exercises were conducted for 5 minutes before measurements. The testing device was set to an angular velocity of 60° per second, and lumbar extensor strength was measured 5 times and recorded as peak torque (Nm) (Fig. 3). The lumbar extensor strength index (LESI, Nm/kg) was obtained by dividing the measured peak torque value by body weight (kg).
Fig. 3.
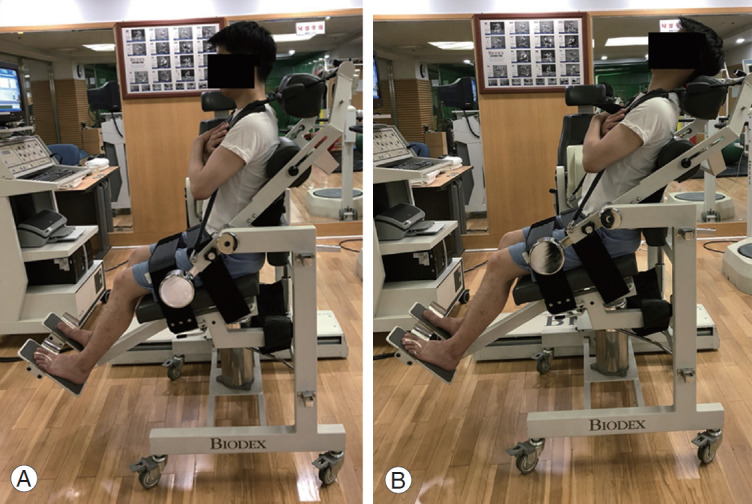
(A, B) Lumbar extensor strength measurement using the SYSTEM 3 PRO (Biodex Medical Systems, Shirley, NY, USA) lumbar extension restraint system dynamometer.
5. Relationship between sarcopenia and back muscle degeneration
The relationship between sarcopenia and back muscle degeneration was assessed by dividing all subjects into sarcopenia and non-sarcopenia groups based on ASMI (above). These groups then compared for differences in CSA index, FI rate, and LESI by independent samples Student t-test.
6. Back muscle degeneration risk index
To develop a single risk index reflecting both functional and morphological aspects of back muscle degeneration, we conducted Pearson correlation analysis of the association between LESI and CSA index and between LESI and FI rate. The correlation coefficient between LESI, reflecting back muscle function, and CSA index, reflecting back muscle morphological degeneration, was multiplied by the CSA index. Similarly, the correlation coefficient between LESI and FI rate was multiplied by the FI rate. The sum of these two products was defined as the back muscle degeneration risk index (risk index=coefficient of LESI and CSA index×CSA index+coefficient of LESI and FI rate×FI rate). The FI rate was expressed as a percentage to prevent the absolute value from becoming too small.
7. Comparison of back-pain severity between sarcopenia/non-sarcopenia and high/low back muscle degeneration groups
The back-pain group was classified into ASMI-based sarcopenia and non-sarcopenia groups, and CSA index, FI rate, LESI, and VAS scores compared. Back-pain patients were subsequently divided into high-risk and low-risk back muscle degeneration groups using the median cutoff risk index as a threshold, and ASMI, CSA index, FI rate, LESI, and VAS scores compared by Student t-test or Mann-Whitney U-test. Through these comparisons, the effects of sarcopenia and back muscle degeneration on back-pain severity were revealed.
8. Statistical analyses
All data are expressed as mean±standard deviation. Differences in demographic characteristics, sarcopenia prevalence, back muscle degeneration indices, and VAS scores were examined using Student t-test or MannWhitney U-test. Pearson correlation coefficients for LESI versus ASMI, LESI versus CSA index, and LESI versus FI rate were also calculated. A p<0.05 (two-tailed) was considered significant for all tests. Statistical analyzes were performed using IBM SPSS ver. 22.0 software (IBM Corp., Armonk, NY, USA).
Results
1. Comparison of sarcopenia prevalence and back muscle degeneration characteristics between patients with and without back pain
Body mass index did not differ between the back painfree group (group A) and the back-pain group (group B; mean VAS score, 6.32±1.88; 24.23±5.14 kg/m2 versus 25.63±4.70 kg/m2, p=0.07), while sarcopenia prevalence was significantly higher in group B than group A (26.8% [n=30] versus 8.0% [n=8], p<0.01) (Table 1).
Table 1.
Comparison of sarcopenia and back muscle degeneration characteristics between group A and B
| Characteristic | Group A (n=100) | Group B (n=112) | p-value |
|---|---|---|---|
| Age (yr) | 56.6±15.2 | 57.8±17.6 | 0.63 |
| Sex | 0.12 | ||
| Male | 58 | 50 | |
| Female | 42 | 62 | |
| Body mass index (kg/m2) | 24.23±5.14 | 25.63±4.70 | 0.07 |
| Prevalence of sarcopenia | 8 (8.0) | 30 (26.8) | <0.01* |
| Appendicular skeletal muscle index (kg/m2) | 7.35±1.01 | 6.75±1.18 | <0.01* |
| Cross-sectional area index (cm2/m2) | 10.13±1.95 | 6.40±1.25 | <0.01* |
| Fatty infiltration rate (%) | 8.10±1.74 | 18.33±3.40 | <0.01* |
| Lumbar extensor strength index (Nm/kg) | 1.64±0.21 | 0.76±0.12 | <0.01* |
Values are presented as mean±standard deviation, number, or number (%).
p <0.05 was defined as statistically significant.
There were no significant differences in demographic variables between pain-free and back-pain groups; however, there were significant group differences in indicators of both sarcopenia and back muscle degeneration. Average ASMI, which was used as an indicator for sarcopenia, was significantly lower in the back-pain group. In addition, CSA index and FI rate differed significantly between groups, and we found that back muscle degeneration tended to progress further in the back-pain group (Table 1).
2. Relationship between sarcopenia and back muscle degeneration
Average age did not differ between the total sarcopenia and non-sarcopenia groups (57.6±13.3 years versus 55.5±13.5 years, p=0.45). Similarly, there were no significant differences in the indicators of back muscle degeneration CSA index, FI rate, and LESI between sarcopenia groups (Table 2), indicating that the presence of sarcopenia alone does not predict progression of back muscle degeneration.
Table 2.
Comparison between sarcopenia and non-sarcopenia group in all subjects
| Variable | Sarcopenia group (n=38) | Non-sarcopenia group (n=174) | p-value |
|---|---|---|---|
| Age (yr) | 57.6±13.3 | 55.5±13.5 | 0.45 |
| Sex | 0.21 | ||
| Male | 18 | 90 | |
| Female | 20 | 84 | |
| Appendicular skeletal muscle index (kg/m2) | 6.11±0.72 | 7.47±1.03 | <0.001* |
| Cross-sectional area index (cm2/m2) | 8.99±2.11 | 8.65±1.81 | 0.63 |
| Fatty infiltration rate (%) | 12.21±2.92 | 13.32±2.73 | 0.90 |
| Lumbar extensor strength index (Nm/kg) | 1.12±0.64 | 1.35±0.63 | 0.14 |
Values are presented as mean±standard deviation or number.
p <0.05 was defined as statistically significant.
3. Pearson correlation coefficients used to develop a back muscle degeneration risk index
Pearson correlation coefficient for the associations between LESI and ASMI, LESI and CSA index, and LESI and FI rate were all signifi cant within group B (LESI versus ASMI, r=0.493; LESI versus CSA index, r=0.557; LESI versus FI rate, r=−0.741) (Table 3).
Table 3.
Results of correlation analysis between LESI and ASMI, CSA index, FI rate in group B
| Factor | Correlation with LESI (n=112) |
p-value |
|---|---|---|
| Coefficient | ||
| ASMI (kg/m2) | 0.493 | <0.01* |
| CSA index (cm2/m2) | 0.557 | <0.01* |
| FI rate (%) | -0.741 | <0.01* |
LESI, lumbar extensor strength index; ASMI, appendicular skeletal muscle index; CSA, cross-sectional area; FI, fatty infiltration.
p <0.05 was defined as statistically significant.
4. The back muscle degeneration risk index but not sarcopenia presence alone predicted more severe back pain
There were no significant differences in CSA index, FI rate, and LESI between the sarcopenia and non-sarcopenia patients of group B. The degree of back pain as measured by VAS score also did not differ significantly between sarcopenia and non-sarcopenia groups (p=0.067) (Fig. 4). However, LESI was significantly lower in the high-risk muscle degeneration subgroup of group B, defined as those patients with back muscle degeneration index value above the median, compared to the low-risk group (below the median value) (p=0.015). Similarly, VAS score was significantly greater in the high-risk group (p<0.05) (Fig. 5). The specific cutoff values for the high-risk group were ASMI <5.87 kg/m2, CSA index <6.78 cm2/m2, FI rate >24.89%, and LESI <0.58 Nm/kg (Table 4).
Fig. 4.
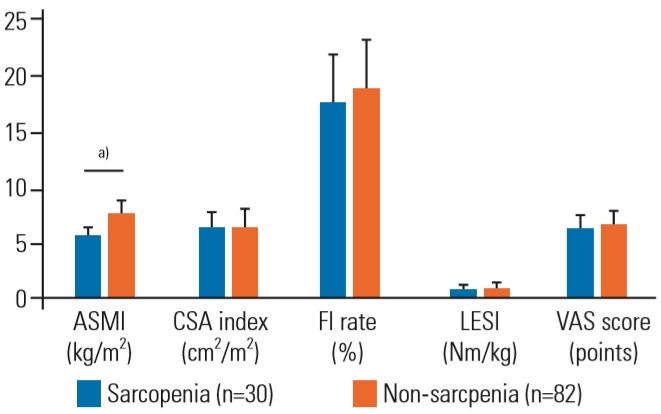
Comparisons of ASMI, CSA index, FI rate, and VAS scores between sarcopenia and non-sarcopenia groups of back-pain patients (group B) stratified by ASMI score (group B). ASMI, appendicular skeletal muscle index; CSA, cross-sectional area; FI, fatty infiltration; VAS, Visual Analog Scale. a)Means difference with statistical significance.
Fig. 5.
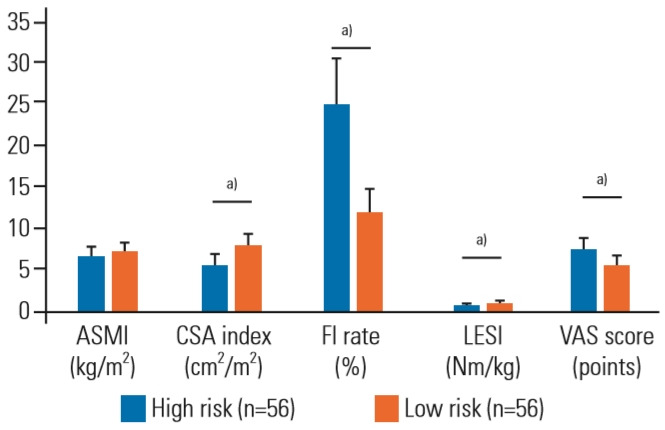
Comparisons of ASMI, CSA index, FI rate, LESI, and VAS scores between high-risk and low-risk muscle degeneration groups of back-pain patients stratified by the median value of the back muscle degeneration risk index. ASMI, appendicular skeletal muscle index; CSA, cross-sectional area; FI, fatty infiltration; LESI, lumbar extensor strength index; VAS, Visual Analog Scale. a)Means difference with statistical significance.
Table 4.
Comparison and value ratio of high risk group to group A
| Variable | High risk group (n=56) | Group A (n=100) | Value ratio of high risk group to group A (%) | p-value |
|---|---|---|---|---|
| Appendicular skeletal muscle index (kg/m2) | 5.87±1.00 | 7.35±1.01 | 79.9 | <0.01 |
| Cross-sectional area index (cm2/m2) | 6.78±1.56 | 10.13±1.95 | 66.9 | <0.01 |
| Fatty infiltration rate (%) | 24.89±5.52 | 8.10±1.74 | 307.3 | <0.01 |
| Lumbar extensor strength index (Nm/kg) | 0.58±0.34 | 1.64±0.21 | 35.4 | <0.01 |
Values are presented as mean±standard deviation, unless otherwise stated.
Discussion
The central findings of this study are that back-pain severity is more strongly related to back muscle degeneration than to sarcopenia, and that back muscle degeneration is only weakly related to sarcopenia. Thus, sarcopenia and back muscle degeneration are mainly independent factors influencing back pain. Here ASMI was assessed as an index of sarcopenia, and CSA, FI rate, and LESI as indices of back muscle degeneration. As sarcopenia indicates the co-occurrence of skeletal muscle mass and strength loss [4], we used CSA index and FI rate to reflect back muscle morphology (quantity and quality) and LESI to indicate back muscle function (strength). The prevalence of sarcopenia as well as ASMI, CSA index, FI rate, and LESI scores differed significantly between control pain-free and backpain groups, suggesting that both sarcopenia and back muscle degeneration contribute to back pain. Sarcopenia prevalence varies from 5%–13% in people >60 years, and is as high as 50% in those >80 years old [20]. In this study, sarcopenia prevalence was approximately 18%, which is unexpectedly high considering the participants’ average age (<60 years). Moreover, 53% of all participants had back pain that interfered with daily activity, suggesting reduced muscle mass and strength, which may have elevated sarcopenia prevalence. The CSA index, FI rate, and LESI did not differ between sarcopenia and non-sarcopenia groups stratified by ASMI score, suggesting that sarcopenia is not directly related to back muscle degeneration. Thus, sarcopenia and back muscle degeneration should be considered separate factors influencing back pain.
Lumbar extensor muscles are important for controlling gait in patients with back pain [21], and lumbar extensor strengthening exercises can substantially improve clinical outcome in patients with chronic back pain plus deconditioning [22]. Additionally, lumbar extensor muscles are critical for the dynamic control of spinal segments [23]. The clinical significance of lumbar extensor strength has been widely reported. Moreover, the isokinetic lumbar extensor dynamometer is widely used and its reliability well established [11,24]. Here, we also confirmed high reliability in a retest of 30 subjects (intraclass correlation coefficient=0.862).
Among ASMI, CSA index, and FI rate, the latter was most strongly correlated with LESI, suggesting a close relation between back muscle function and FI rate. This may be because the back muscle is replaced by fat concomitant with aging and degeneration, while the CSA itself may not change [9]. Thus, FI rate and lumbar extensor strength are important factors reflecting back muscle degeneration.
There was no significant difference in CSA index or FI rate between the general sarcopenia and non-sarcopenia groups or the sarcopenia and non-sarcopenia subgroups of back-pain patients. Among back-pain patients, in fact, FI rate was even higher in the non-sarcopenia group, although the difference did not reach statistical significance. This result further supports the independent influences of sarcopenia and back muscle degeneration on back pain, and validates our initial purpose of analyzing the relationship between sarcopenia and back muscle degeneration. Moreover, no significant difference in VAS score was found between the sarcopenia and non-sarcopenia groups, suggesting that sarcopenia is only weakly associated with the severity of back pain (Fig. 4).
We analyzed the correlations between LESI and CSA index and between LESI and FI rate to establish a risk index that can quantify both morphological and functional aspects of back muscle degeneration. The correlation coefficients were multiplied by the CSA index and FI rate, respectively, and added to obtain the risk index, which was then used to classify patients into high-risk and low-risk back muscle degeneration groups. There was a significant difference in VAS score between these groups, but not between sarcopenia groups, indicating a close association between back muscle degeneration and back-pain severity. Average index values of 79.9% of ASMI, 66.9% of CSA index, 307.3% of FI rate, and 35.4% of LESI define the high-risk group and so may be used as clinical references to assess back muscle degeneration (Table 4). Collectively, these findings suggest that patients at high-risk of back muscle degeneration according to this index should be carefully managed in clinical practice.
This study has several limitations. First, although the data was collected prospectively, the study design was cross-sectional. Further longitudinal studies with followup assessments of sarcopenia and back muscle degeneration over time should be conducted. Recent studies have shown that the multifidus muscle affects back pain more strongly than the erector spinae muscle, whereas the erector spinae muscle shows wider and earlier fatty degeneration than the multifidus [25,26]. This indicates a relationship between stress loading and back muscle degeneration, and suggests that the multifidus and erector spinae muscles may contribute differently to back muscle degeneration. In our study, however, paraspinal muscle was considered the sum of the multifidus and erector spinae muscles. In addition, only ASMI was used to evaluate sarcopenia based on AWGS guidelines [15]. However, the complete AWGS algorithm using grip strength and gait speed was not employed for two reasons. First, measurements using BIA are equally objective and valid under the same conditions [27] and second, the grip strength may vary depending on patient cooperation, as patients with back pain demonstrate deteriorated physical performance not just from muscle weakness or wasting but from pain. We also did not investigate the causes of back pain in patients without sarcopenia or back muscle degeneration, such as disk degeneration, hypertrophy of facet joints, instability between the segments [28], or myofasciitis, a systemic acquired inflammatory muscle disease with perifascicular cellular infiltration [29]. Myofasciitis patients often complain of diffuse myalgia and various types of pain, such as aching and cramps. The lower extremities are mainly involved, but there are also reported cases with back muscle involvement [30]. The etiology of back pain is so variable that it is difficult to know exactly whether a given condition such as myofasciitis alone contributes to back pain. It is critical therefore to validate this muscle degeneration index on patients with known back-pain etiology. However, the effect of sarcopenia and back muscle degeneration on back pain was compared at the same time, and the back muscle degeneration risk index was set to reflect both CSA and FI rate of the back muscle. This index may therefore facilitate future studies on back pain, sarcopenia, and back muscle degeneration.
Conclusions
Back muscle degeneration is more strongly associated with back pain than with sarcopenia. Lumbar extensor strength in particular was closely related to back muscle degeneration and so may be an important indicator of back muscle function and the root cause of back pain. We also developed and validated a risk index reflecting both muscle morphology and function for assessing back muscle degeneration. This value may be a useful clinical reference for determining the degree of back muscle degeneration and a helpful treatment guide.
Acknowledgments
This research was supported by EMBRI Grants 2016-EMBRI-DJ0003 from the Eulji University
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 Suppl):990S–1S. doi: 10.1093/jn/127.5.990S. [DOI] [PubMed] [Google Scholar]
- 2.Takayama K, Kita T, Nakamura H, et al. New predictive index for lumbar paraspinal muscle degeneration associated with aging. Spine (Phila Pa 1976) 2016;41:E84–90. doi: 10.1097/BRS.0000000000001154. [DOI] [PubMed] [Google Scholar]
- 3.Cao L, Morley JE. Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J Am Med Dir Assoc. 2016;17:675–7. doi: 10.1016/j.jamda.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Cruz-Jentoft AJ, Landi F. Sarcopenia. Clin Med (Lond) 2014;14:183–6. doi: 10.7861/clinmedicine.14-2-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968–74. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 6.White AA, 3rd, Gordon SL. Synopsis: workshop on idiopathic low-back pain. Spine (Phila Pa 1976) 1982;7:141–9. doi: 10.1097/00007632-198203000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Park S, Kim HJ, Ko BG, et al. The prevalence and impact of sarcopenia on degenerative lumbar spinal stenosis. Bone Joint J. 2016;98-B:1093–8. doi: 10.1302/0301-620X.98B8.37623. [DOI] [PubMed] [Google Scholar]
- 8.Tanishima S, Hagino H, Matsumoto H, Tanimura C, Nagashima H. Association between sarcopenia and low back pain in local residents prospective cohort study from the GAINA study. BMC Musculoskelet Disord. 2017;18:452. doi: 10.1186/s12891-017-1807-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teichtahl AJ, Urquhart DM, Wang Y, et al. Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J. 2015;15:1593–601. doi: 10.1016/j.spinee.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 10.Wan Q, Lin C, Li X, Zeng W, Ma C. MRI assessment of paraspinal muscles in patients with acute and chronic unilateral low back pain. Br J Radiol. 2015;88:20140546. doi: 10.1259/bjr.20140546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drouin JM, Valovich-mcLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91:22–9. doi: 10.1007/s00421-003-0933-0. [DOI] [PubMed] [Google Scholar]
- 12.Hirsch G, Beach G, Cooke C, Menard M, Locke S. Relationship between performance on lumbar dynamometry and Waddell score in a population with low-back pain. Spine (Phila Pa 1976) 1991;16:1039–43. doi: 10.1097/00007632-199109000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Keller A, Hellesnes J, Brox JI. Reliability of the isokinetic trunk extensor test, Biering-Sorensen test, and Astrand bicycle test: assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine (Phila Pa 1976) 2001;26:771–7. doi: 10.1097/00007632-200104010-00017. [DOI] [PubMed] [Google Scholar]
- 14.Kim YH, Kim KI, Paik NJ, Kim KW, Jang HC, Lim JY. Muscle strength: a better index of low physical performance than muscle mass in older adults. Geriatr Gerontol Int. 2016;16:577–85. doi: 10.1111/ggi.12514. [DOI] [PubMed] [Google Scholar]
- 15.Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- 16.Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–7. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 17.Han JS, Ahn JY, Goel VK, Takeuchi R, McGowan D. CT-based geometric data of human spine musculature: part I. Japanese patients with chronic low back pain. J Spinal Disord. 1992;5:448–58. doi: 10.1097/00002517-199212000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Keller A, Johansen JG, Hellesnes J, Brox JI. Predictors of isokinetic back muscle strength in patients with low back pain. Spine (Phila Pa 1976) 1999;24:275–80. doi: 10.1097/00007632-199902010-00016. [DOI] [PubMed] [Google Scholar]
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 20.Morley JE, Anker SD, von Haehling S. Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology-update 2014. J Cachexia Sarcopenia Muscle. 2014;5:253–9. doi: 10.1007/s13539-014-0161-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steele J, Bruce-Low S, Smith D, Jessop D, Osborne N. Lumbar kinematic variability during gait in chronic low back pain and associations with pain, disability and isolated lumbar extension strength. Clin Biomech (Bristol, Avon) 2014;29:1131–8. doi: 10.1016/j.clinbiomech.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 22.Steele J, Fisher J, Perrin C, Conway R, Bruce-Low S, Smith D. Does change in isolated lumbar extensor muscle function correlate with good clinical outcome?: a secondary analysis of data on change in isolated lumbar extension strength, pain, and disability in chronic low back pain. Disabil Rehabil. 2019;41:1287–95. doi: 10.1080/09638288.2018.1424952. [DOI] [PubMed] [Google Scholar]
- 23.Kamaz M, Kiresi D, Oguz H, Emlik D, Levendoglu F. CT measurement of trunk muscle areas in patients with chronic low back pain. Diagn Interv Radiol. 2007;13:144–8. [PubMed] [Google Scholar]
- 24.Nordez A, Casari P, Cornu C. Accuracy of Biodex system 3 pro computerized dynamometer in passive mode. Med Eng Phys. 2008;30:880–7. doi: 10.1016/j.medengphy.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Lee SH, Park SW, Kim YB, Nam TK, Lee YS. The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J. 2017;17:81–7. doi: 10.1016/j.spinee.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Ohtori S, Orita S, Yamauchi K, et al. Classification of chronic back muscle degeneration after spinal surgery and its relationship with low back pain. Asian Spine J. 2016;10:516–21. doi: 10.4184/asj.2016.10.3.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mijnarends DM, Meijers JM, Halfens RJ, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc. 2013;14:170–8. doi: 10.1016/j.jamda.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Hodges PW. The role of the motor system in spinal pain: implications for rehabilitation of the athlete following lower back pain. J Sci Med Sport. 2000;3:243–53. doi: 10.1016/s1440-2440(00)80033-x. [DOI] [PubMed] [Google Scholar]
- 29.Greenberg SA, Amato AA. Myofasciitis: imaging and pathology. Arch Neurol. 2012;69:406. doi: 10.1001/archneurol.2011.1159. [DOI] [PubMed] [Google Scholar]
- 30.Papo T. Macrophagic myofasciitis: focal or systemic? Joint Bone Spine. 2003;70:242–5. doi: 10.1016/s1297-319x(03)00093-9. [DOI] [PubMed] [Google Scholar]


