Abstract
PIM-1 is an oncogene involved in cell cycle progression, cell growth, cell survival and therapy resistance, activated in many types of cancer, and is now considered as a very promising target for cancer therapy. We report for the first time that PIM-1 is overexpressed in circulating tumor cells (CTCs) from metastatic castration-resistant prostate cancer patients (mCRPC). We first developed and validated a highly sensitive RT-qPCR assay for quantification of PIM-1 transcripts. We further applied this assay to study PIM-1 expression in EpCAM(+) CTC fraction isolated from 64 peripheral blood samples of 50 mCRPC patients. CTC enumeration in all samples was performed using the FDA-cleared CellSearch® system. PIM-1 overexpression was detected in 24/64 (37.5%) cases, while in 20/24 (83.3%) cases that were positive for PIM-1 expression, at least one CTC/7.5 mL PB was detected in the CellSearch®. Our data indicate that PIM-1 overexpression is observed at high frequency in CTCs from mCRPC patients and this finding, in combination with androgen receptor splice variant 7 (AR-V7) expression in CTCs, suggest its potential role as a very promising target for cancer therapy. We strongly believe that PIM-1 overexpression in EpCAM(+) CTC fraction merits to be further evaluated and validated as a non-invasive circulating tumor biomarker in a large and well-defined patient cohort with mCRPC.
Keywords: liquid biopsy, CTCs, mCRPC, PIM-1, AR-V7, RT-qPCR
1. Introduction
Prostate cancer (PCa) is the second most common cancer in men worldwide, with an estimated global incidence of 1.3 million cases in 2018 [1]. Therapeutic options exist for patients with clinically localized disease, and the 10-year survival rate is over 90% [2]. However, a significant minority of patients present de novo metastatic disease after initiation of primary treatment with androgen deprivation therapy (ADT). In most cases, the progression is inevitable leading to increasing values of serum prostate-specific antigen (PSA) despite the castrated levels of serum testosterone (<50 ng/dL), termed the disease state as castration-resistant prostate cancer (CRPC) [3,4]. In recent years, the therapeutic management of advanced disease has been rapidly improved, including mainly taxanes as chemotherapy regimens such as docetaxel and cabazitaxel and androgen receptor (AR) inhibitors such as abiraterone acetate and enzalutamide, significantly increasing the life expectancy of metastatic castration-resistant prostate cancer (mCRPC) patients [5]. The diagnosis and monitoring of PCa are currently based on the combination of PSA testing, abnormal digital rectal examination and histopathologic evaluation of prostate biopsy [6]. Although PSA became widely adopted for cancer screening by the early 1990s, its main drawback is the lack of specificity and its limited value for predicting responses to therapy [7]. Since classical biopsy is highly invasive, it cannot be used to monitor tumor genomic changes in real time.
Liquid biopsy, based on serial blood testing, covers this gap by enabling the prospective and sequential evaluation of the disease dynamics, and this is feasible for the detection of minimal residual disease and early prediction of relapse [8,9]. Liquid biopsy is based on the analysis of circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), circulating miRNAs and tumor-derived extracellular vesicles (EVs) that are shed from primary tumors or metastatic sites into peripheral blood [9,10,11]. The test for CTC enumeration in metastatic prostate cancer is FDA-cleared for prognosis since 2008 [12,13]. In addition to CTC enumeration, the molecular characterization of CTC in mCRPC has important therapeutic implications; androgen receptor splice variant 7 (AR-V7) expression in CTCs from patients with mCRPC predicts a lack of response to anti-androgen therapy with enzalutamide or abiraterone [14], while AR-V7 expression status does not affect responsiveness to taxanes [15]. We have recently developed and validated a multiplex RT-qPCR assay for AR splice variants and have shown that the AR-V7 splice variant is highly overexpressed in CTCs of patients with mCRPC [16].
However, new surrogate biomarkers that could be easily measurable and could predict the treatment outcomes for prostate cancer management are still highly needed. Basic research has shown that the proviral integration site for the Moloney murine leukemia virus-1 (PIM-1) is an oncogene that encodes a serine/threonine kinase, involved in cell cycle progression, cell growth, cell survival and therapy resistance [17,18]. PIM-1 is activated in many types of cancer including prostate, providing a common target for therapy [19,20,21]. Recent data have shown that PIM activation is induced by tumor microenvironment changes, such as hypoxia, and causes resistance to angiogenesis inhibitors [21]. PIM-1 is a component of the small 40S ribosomal subunit and could regulate the expression of ribosomal small subunit protein-7, RPS7, demonstrating that ribosome-targeting drugs may be effective against diverse CRPC subtypes including AR-null disease [22,23]. Moreover, PIM-1 is thought to promote the carcinogenesis by cooperating with myc as transgenic mouse study has demonstrated that PIM1 enhanced c-Myc-induced tumorigenesis in PCa [24]. PIM-1 has been shown to be overexpressed in approximately 50% of human prostate cancer specimens using tissue microarrays [25]. Moreover, PIM-1 overexpression was observed in high-grade prostate intraepithelial neoplasia and in prostate cancer compared to normal prostatic tissue and benign prostate hyperplasia [26,27]. Increased levels of PIM-1 have been shown to be the direct result of oncogenic fusion proteins and active signal transduction pathways, while its elevated levels can lead to genomic instability and promote the neoplastic process [28]. PIM-1 kinase can also phosphorylate AR, regulating its degradation and function, indicating its involvement in mCRPC. Furthermore, PIM-1 expression has been shown to be increased in prostate tissue demonstrating partial response to docetaxel, suggesting the predictive role of PIM-1 to this type of treatment [28]. Initial efforts to inhibit PIM with monotherapies have been hampered by compensatory upregulation of other pathways and drug toxicity, and as such, it has been suggested that co-targeting PIM with other treatment approaches may permit lower doses and be a more viable option in the clinic [29].
In this study, we first developed and validated a highly sensitive RT-qPCR assay for quantification of PIM-1 transcripts and reported for the first time that PIM-1 is overexpressed in EpCAM(+) CTC fraction isolated from mCRPC patients. We further evaluated whether PIM-1 overexpression in EpCAM(+) CTC fraction is correlated with ARV7 expression in the same samples. Our data indicate that PIM-1 overexpression in CTCs should be prospectively evaluated as a potential biomarker for prostate cancer management in a large and well-defined patient cohort.
2. Results
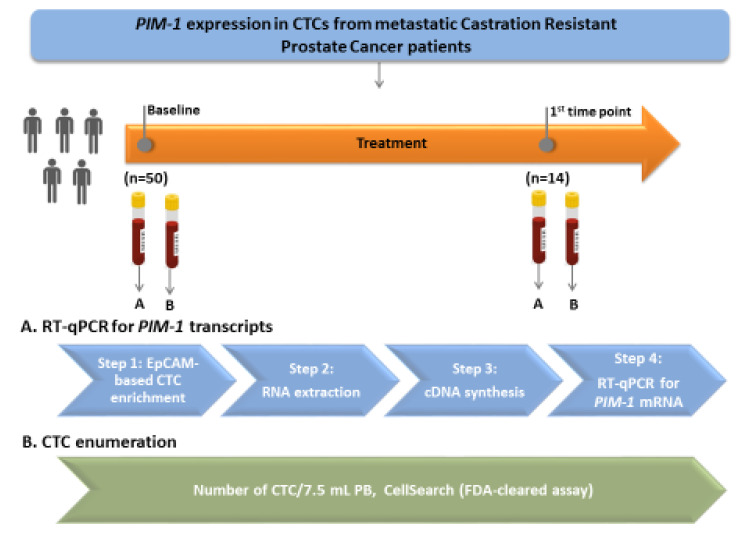
The outline of the study is shown in Figure 1.
Figure 1.
Outline of the experimental procedure.
2.1. TCGA Analysis
In The Cancer Genome Atlas (TCGA), the PanCancer Atlas for the prostate cohort contains data from 492 prostate adenocarcinoma patients (PRAD). Bioinformatic analyses of the TCGA datasets demonstrated that PIM-1 is elevated in 28/492 (6%) cases. To verify PIM-1 mRNA expression, the GEPIA (http://gepia.cancer-pku.cn/index.html) web server was used to plot a gene expression level between prostate adenocarcinoma and normal tissues in the TCGA database (Figure S1). The patient data were grouped according to the transcripts per million (TPM) value. Log2 (TPM + 1) was used for log-scale, and four-way analysis of variance (ANOVA) was applied.
2.2. PIM-1 Overexpression in EpCAM(+) CTC Fraction
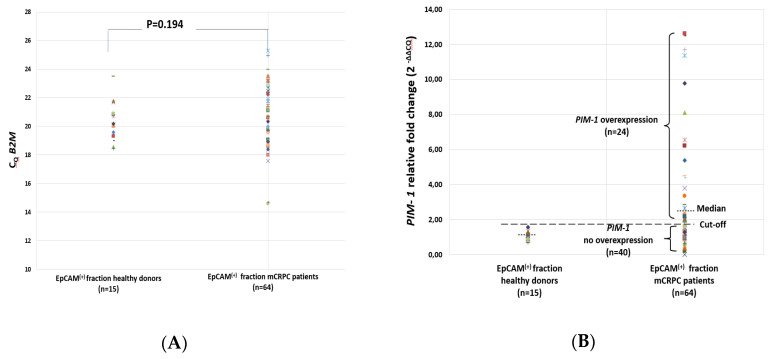
A total of 64 peripheral blood samples from 50 mCRPC patients collected at two different time points were used to isolate EpCAM(+) fractions, isolate total RNA and synthesize cDNAs. All these cDNAs were first checked for their quality by RT-qPCR for B2M. All these cDNA samples were positive for B2M expression. B2M expression levels did not differ between EpCAM(+) fractions in the mCRPC patients group and the healthy donors (HD) group, as expected (Figure 2A). In these cDNAs, we performed RT-qPCR to quantify PIM-1 expression in the EpCAM(+) fractions.
Figure 2.
(A) Cq values for B2M and (B) relative fold change for PIM-1 in the EpCAM(+) fraction in healthy donors (HD) (n = 15) and metastatic castration-resistant prostate cancer (mCRPC) patients samples (n = 64).
A novel method based on RT-qPCR for PIM-1 assay was developed and the experimental conditions were first optimized in detail. Under optimized conditions, the specificity of the assay was tested using peripheral blood samples from 15 healthy donors (HD) that were analyzed exactly as patient samples [16]. Median fold change of PIM-1 expression in the HD group was used to define the cut-off (1.03, range: 0.7–1.58). Based on the defined cut-off, 40/64 (62.5%) patient samples were found negative for PIM-1 overexpression (median fold change: 0.98, range: 0.04–1.51, p = 0.034) and 24/64 (37.5%) samples were found positive for PIM-1 overexpression (median fold change: 5.13, range: 1.53–12.64, p < 0.001) (Figure 2B). PIM-1 overexpression was detected in 21/50 (42%) samples at baseline (before) and in 3/14 (21.4%) samples at the first time point of treatment (after).
2.3. PIM-1 Overexpression in the EpCAM(+) CTC Fraction before and after Treatment
For a subgroup of these mCRPC patients (n = 14), PB samples were available both at baseline and at the first time point of treatment. In this group, PIM-1 overexpression was observed in total of 7/28 (25%) EpCAM(+) CTC fraction samples; in 25/28 (89.3%) of these cases CTCs were detected by the CellSearch®, and more than 5CTCs/7.5 mL were identified in 22/25 (88%) of CTC-positive samples (Table 1). There was only one case (P#38) where the EpCAM(+) CTC fraction was found to be positive for PIM-1 overexpression, whereas CellSearch® didn’t identify CTCs. There were two cases (P#2, P#34) where both CellSearch® and PIM-1 expression analyses were negative (Table 1). It is important to note that 5/14 (35.7%) patient samples (P#2, P#27, P#33, P#38, P#39) were positive for PIM-1 overexpression, in at least one time point of treatment, and that 4/5 (80%) of these patients where PIM-1 was overexpressed in CTCs have died (Table 1). There was only one case (P#2) where the patient was identified as positive for PIM-1 overexpression at baseline and was still alive at the time of our results evaluation (Table 1, Figure 3).
Table 1.
PIM-1 overexpression in relation to circulating tumor cell (CTC) enumeration in the CellSearch® system, Androgen Receptor splice variant 7 (AR-V7) expression and clinical outcome before and after treatment (n = 14).
| Patient’s ID |
CTCs/7.5 mL PB (CellSearch® Analysis) |
PIM-1 in CTCs | AR-V7 in CTCs | Therapy | Clinical Outcome | Death | |||
|---|---|---|---|---|---|---|---|---|---|
| Before Therapy |
After Therapy |
Before Treatment |
After Treatment |
Before Treatment |
After Treatment |
||||
| P#2 | 5 | 0 | + | - | + | - | Enzalutamide | SD | No |
| P#11 | 1 | 2 | - | - | - | - | Enzalutamide | CR | No |
| P#12 | 15 | 20 | - | - | - | + | Docetaxel | PR | No |
| P#17 | 24 | 37 | - | - | + | - | Docetaxel | PR | Yes |
| P#27 | 8 | 141 | + | + | - | + | Docetaxel | PR | Yes |
| P#29 | 5 | 9 | - | - | - | - | Abiraterone | CR | No |
| P#32 | 15 | 44 | - | - | + | - | Docetaxel | PR | Yes |
| P#33 | 1 | 6 | - | + | - | - | Abiraterone | PR | Yes |
| P#34 | 18 | 0 | - | - | - | + | Abiraterone | PD | Yes |
| P#35 | 25 | 74 | - | - | - | + | Docetaxel | PR | Yes |
| P#36 | 6 | 196 | - | - | - | + | Docetaxel | PR | Yes |
| P#38 | 0 | 26 | + | - | + | + | Docetaxel | PR | Yes |
| P#39 | 87 | 145 | + | + | + | - | Docetaxel | PD | Yes |
| P#44 | 121 | 189 | - | - | + | + | Abiraterone | PD | Yes |
SD: Stable Disease, CR: Complete Response, PR: Partial Response, PD: Progression of Disease.
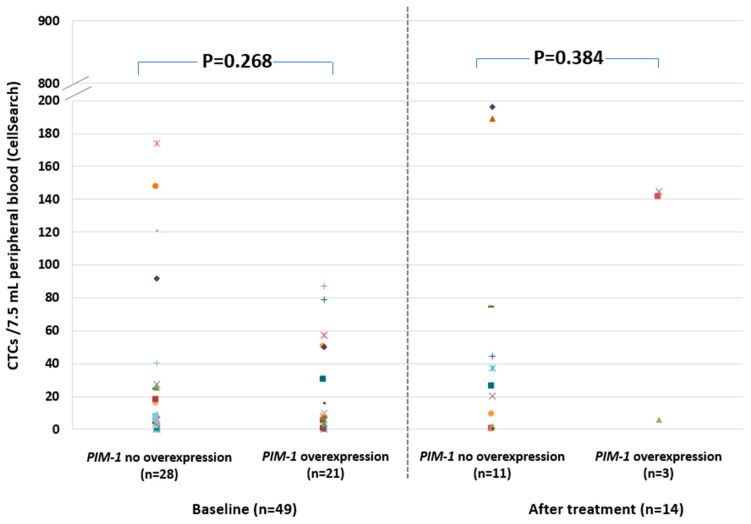
Figure 3.
CTC enumeration (CTCs/7.5 mL PB, CellSearch®) in 14 pairs of mCRPC patient samples before and after treatment and PIM-1 overexpression in EpCAM(+) CTC fraction.
2.4. PIM-1 Overexpression in Relation to CTC Enumeration in the CellSearch® System
CTC enumeration was performed in parallel, in identical peripheral blood draws in 63 patient samples using the FDA-cleared CellSearch® system (Menarini, Silicon Biosystems), 49 at baseline, and 14 after the first time point of treatment. CTCs were detected by the CellSearch® in 53/63 (84.1%) cases, while in 44/63 (69.8%) cases at least 5CTCs/7.5mL PB were enumerated. PIM-1 was overexpressed in 21/49 (42.8%) of these samples before and in 3/14 (21.4%) samples after the first time point of treatment (Figure 4). In 20/53 (37.7%) cases where the CellSearch® analysis detected at least one CTC/7.5mL PB, PIM-1 was found to be overexpressed. However, there were four cases where EpCAM(+) CTC fractions were found positive for PIM-1 overexpression, while in the CellSearch® no CTCs were detected. According to our results PIM-1 overexpression in CTC was not associated with CTC counts both before and after treatment (Figure 4). PIM-1 overexpression was detected in 24/63 (38.1%) cases; 21/49 (42.8%) were positive for PIM-1 overexpression before treatment and 3/14 (21.4%) were positive for PIM-1 overexpression after the first time point of treatment. It is important to mention that in the majority 20/24 (83.3%) of these samples that were positive for PIM-1 overexpression, at least one CTC/7.5 mL PB was detected in the CellSearch® (Figure 4).
Figure 4.
Relative fold change (2−ΔΔCq) of PIM-1 transcripts in EpCAM(+) CTC fraction before and after treatment, in relation to CTC enumeration (CTCs/7.5 mL PB, CellSearch®), in identical blood draws.
2.5. PIM-1 Overexpression in Relation to AR-V7 Expression
We further evaluated for the first time whether PIM-1 overexpression in EpCAM(+) CTC fraction is correlated with AR-V7 expression in the same samples. For 44/50 (88%) of these patients, the status of AR-V7 expression in EpCAM(+) CTCs before treatment was known to us through our previous study [16]. Our comparison indicated that 5/44 (11.4%) samples were positive for both PIM-1 overexpression and AR-V7 expression; 4/5 (80%) of these patients died (Table S1). There were 13/44 (29.5%) samples positive for PIM-1 overexpression and negative for AR-V7 expression, and 10/44 (22.7%) samples positive for AR-V7 expression and negative for PIM-1 overexpression (Table S1). Thus, in total, in 28/44 (63.6%) patient samples either PIM-1 was overexpressed or/and AR-V7 was positive in EpCAM(+) CTC fraction, and a high percentage (20/28, 71.4%) of these patients died. On the contrary, 10/16 (62.5%) patients, where in the EpCAM(+) CTC fraction PIM-1 was not overexpressed and AR-V7 was also negative, were still alive (Table 2). According to these findings, although there was no association between PIM-1 overexpression in EpCAM(+) fraction and the outcome of the patients (p = 0.296), there was a statistically significant association between PIM-1 overexpression and/or expression of AR-V7 in EpCAM(+) fraction before treatment and the outcome of the same patients (chi-square p = 0.030).
Table 2.
Association between PIM-1 overexpression and/or AR-V7 expression in EpCAM(+) CTC fraction and patient status in mCRPC patients (n = 44).
|
PIM-1 Overexpression and/or AR-V7 Expression |
Patient Status | Total | |
|---|---|---|---|
| Alive | Dead | ||
| NO | 10 (62.5%) | 6 (37.5%) | 16 |
| YES | 8 (28.6%) | 20 (71.4%) | 28 |
| Total | 18 (40.9%) | 26 (59.1%) | 44 |
| Chi-square p = 0.030 | |||
3. Discussion
The application of liquid biopsy in metastatic prostate cancer has been the most rapidly evolving paradigm of translational research in recent years. In metastatic prostate cancer, CTC-enumeration is an established and FDA-cleared prognostic test that allows the estimation of overall metastatic burden in cancer patients. Beyond enumeration, the molecular characterization of CTCs hold great promise to improve our knowledge of the metastatic process and to identify new treatment predictive markers. At present, two commercial AR-V7 detection systems are available for clinical use in order to guide which patients will benefit from enzalutamide or abiraterone treatment. CTC molecular analysis based on AR-V7 transcript in mCRPC patients was first described by RT-qPCR performed on EpCAM immuno-magnetically captured cells using the AdnaTest platform (Qiagen, Hilden, Germany). The Oncotype DX AR-V7 Nucleus Detect Test, which is the second platform, was developed by Epic Sciences (Epic Science, San Diego, California), and is based on immunofluorescent CTC staining [30,31]. Detection of AR-V7 at the protein level by this test led to the first approval of CTCs as a predictive biomarker to guide the choice of therapy [9,29]. It is also important to note that a more recent comparison study between these two assays, performed under the PROPHECY trial, has demonstrated a very good agreement (82%) [32].
It is now clear in many cancer types, that as CTCs constitute a dynamic heterogenic population of cancer cells from several primary or metastatic lesions, changes at the gene expression [16,33,34], DNA methylation [35,36,37,38], and DNA mutation levels [39,40,41,42] do occur during treatment. These molecular changes can be evaluated for their potential as novel biomarkers in prostate cancer. Recently, after developing highly sensitive multiplex RT-qPCR assays for the expression of 14 genes, we have shown that the combination of in vivo CTC isolation with downstream RNA analysis is highly promising as a high-throughput, specific, and ultrasensitive approach for multiplex liquid biopsy-based molecular diagnostics in prostate cancer [33].
In the present study, we evaluated for the first time PIM-1 overexpression in the EpCAM(+) fraction of mCRPC patients using a highly sensitive and specific RT-qPCR assay. We have chosen to study PIM-1, since very recent data have shown that PIM-1 kinase plays a critical role in tumorigenesis, and overexpression of PIM-1 protein has been suggested as a potential biomarker for many malignancies including prostate cancer [43]. In preclinical studies, PIM-1 overexpression may lead to cancer development in the following major ways; by inhibiting apoptosis, by promoting cell proliferation and also through promoting genomic instability [44].
Our results indicate that PIM-1 is overexpressed at a high frequency in EpCAM(+) CTC fraction in mCRPC (37.5%), when compared to the TCGA data in prostate adenocarcinoma primary tumors (6%). In the present study, we report for the first time that PIM-1 is overexpressed in CTCs. This positivity rate (37.5%) is not only detected for the first time in CTCs, but in comparison to other genes tested for their expression in EpCAM(+), CTCs’ expression in similar samples [16] is really very high. When we compared PIM-1 overexpression in CTCs with the corresponding CTC counts as estimated by CellSearch®, we found that it was not associated with CTC counts both before and after treatment. We found that in a substantial number of cases where CellSearch® detected CTCs, these CTCs were positive for PIM-1 overexpression. However, there were four cases where CTCs were not detected by the CellSearch®, but the corresponding EpCAM(+) fractions were positive for PIM-1 overexpression by RT-qPCR. These results could be possibly explained by the fact that some EpCAM-positive cells can be negative for CKs (CK-8, CK-18, CK-19) due to epithelial–mesenchymal transition (EMT) process, so they are reported as negative for CTC by the CellSearch®. These findings are in accordance with our previous studies where we detected a lot of molecular alterations in EpCAM(+) CTC fraction, in samples that were “officially” negative for CTCs when using the CellSearch® system [33,41,42].
In recent years, PIM kinase has become one of the important therapeutic targets for the development of novel cancer therapeutics and many inhibitors are under different phases of clinical trials [43,45,46]. Several different derivatives have been synthesized and evaluated for their PIM inhibitory activity, including pyrrole [47,48], pyrimidine [49,50], thiazolidine [51], indole [52], triazole [53], oxadiazole [54], and quinolone [55]. All these derivatives have a specific ring or functional groups which are associated with the PIM kinase inhibitory activity. It is highly important to note that according to our results, in most cases PIM-1 overexpression in EpCAM(+) CTCs at least in one time point during treatment, was associated with the death of patients. This finding indicates that therapy targeted towards PIM-1 would inhibit the activation of this molecule, and could possibly lead to a better clinical outcome for these patients [29].
It is well known that androgen receptor plays a crucial role in the regulation of the normal prostate as well as in the promotion and progression of prostate cancer. However, many studies have investigated whether the regulation of AR transcriptional activity by post-translational modifications, such as phosphorylation, is affected by multiple kinases. PIM1 is a kinase that is overexpressed in prostate cancer, while the two isoforms, PIM-1S and PIM-1L, are the major mediators of AR serine 213 (Ser-213) and threonine 850 (Thr-850) phosphorylation. Based on our previous published study regarding the evaluation of AR-V7 molecular profile in CTCs, we proceed further to co-evaluate for the first time the pattern status of PIM-1 overexpression and/or AR-V7 in the same samples [16]. We noticed that the majority (74.1%) of patients where PIM-1 was overexpressed or/and AR-V7 was positive in the EpCAM(+) CTC fractions have died. On the contrary, the majority (62.5%) of patients where PIM-1 was not overexpressed and AR-V7 was negative in the EpCAM(+) CTCs fractions were still alive at the time of analysis of our data. Our findings are in accordance with the very recent study of Luszczak et al., who demonstrated that AR levels do not appear to affect PIM-1, suggesting that the combination of PIM inhibitors and androgen deprivation therapy are needed in order to assess whether the inhibition of PIM-1 could overcome resistance to androgen deprivation therapy [29].
4. Materials and Methods
4.1. Clinical Samples
We analyzed 64 peripheral blood samples (20 mL in EDTA) from 50 patients with mCRPC; 50 samples at baseline, before treatment, and for 14 patients a sample at the first time point of treatment was available, and 15 peripheral blood samples from healthy male donors. In 63/64 of these cases, using the same blood draw, PB (7.5 mL) was isolated in CellSave tubes for CTC enumeration in the FDA-cleared CellSearch® system (Menarini, Silicon Biosystems, Italy) [56]. The first 5 mL were not used, to avoid contamination from skin epithelial cells. For 14 patients, peripheral blood samples were also available at the first time point of treatment with abiraterone or enzalutamide. All patients gave a written informed consent to participate in the study, which was approved by the Ethics and Scientific Committee of Aretaieio University Hospital.
4.2. CTC Enumeration in the CellSearch®
For CellSearch®, 7.5 mL of venous blood was collected into CellSave tubes (Menarini, Silicon Biosystems) and processed using the CellSearch® Circulating Tumor Cell Kit (Menarini, Silicon Biosystems) according to the manufacturer’s instructions.
4.3. CTC Immunomagnetic Enrichment and RNA-Based Analysis
EpCAM(+) CTCs were enriched from 20mL peripheral blood in EDTA, using immune-magnetic capture beads coated with Ber-EP4 (Dynabeads® Epithelial Enrich, Invitrogen) as previously described [56]. RNA and cDNA synthesis was performed as previously described [16,56].
4.4. RT-qPCR Assay for PIM-1 Expression
We first designed in-silico the primers and one hydrolysis probe (TaqMan) for PIM-1 mRNA using Primer Premier 5.0 software (Premier Biosoft, San Francisco, CA, USA). Our primers and probe were carefully designed to completely avoid primer–dimer formation, false priming sites, formation of hairpin structures, and hybridization to genomic DNA, while amplifying specifically only PIM-1 isoform according to our search in the BLAST Sequence Similarity Search tool (NCBI, NIH) (sequences available upon request). The hydrolysis probe included a 5′-fluorescein (FAM) as a fluorophore covalently attached to the 5’-end of the oligonucleotide probe and a Black Hole Quencher as a quencher at the 3’-end. B2M (Beta-2 microglobulin) was used as a reference gene. RT-qPCR was performed in the LightCycler® 480 instrument (Roche, Germany). Detailed optimization experiments were carried out. The amplification reaction mixture for PIM-1 contained 2 μL of the PCR synthesis buffer (5×), 1 μL MgCl2 (25 mM), 0.2 μL dNTPs (10 mM), 0.15 μL BSA (10 μg/μL), 0.1 μL Hot-Start DNA polymerase (Promega), 0.3 μL of forward and reverse primer (10 μΜ), 1 μL hydrolysis probe (3 μM) and H2O to a final volume of 10 μL, while the amplification reaction mixture for B2M contained 1 μL of PCR synthesis buffer (5×), 1.2 μL MgCl2 (25 mM), 0.15 μL dNTPs (10 mM), 0.3 μL BSA (10 μg/μL), 0.1 μL Hot Start DNA polymerase (Promega), 0.25 μL of forward and reverse primer (10 μΜ), 0.83 μL hydrolysis probe (3 μM) and H2O to a final volume of 10 μL.
4.5. RT-qPCR Assay for AR-V7 Expression
AR-V7 expression in exactly the same cDNAs derived from EpCAM(+) CTC fraction before therapy was evaluated in 44 of these 50 patients as previously described [16].
4.6. Quality Control
Each experimental procedure included one positive and one negative control. cDNA from PC3 cell line was used as a positive control. In order to ensure that amplification of gDNA was completely avoided, four genomic DNAs at high concentrations were used as templates. None of these DNA samples were amplified. B2M was used as a reference gene for RT-qPCR.
4.7. Statistical Analysis
RT-qPCR data for PIM-1 expression were normalized in respect to B2M expression in the same cDNAs, using the 2−ΔΔCt approach [57]. CTCs isolated through positive immune-magnetic enrichment are not 100% pure; since the presence of co-isolated PBMC in the EpCAM(+) fraction could affect the specificity of the PIM-1 assay, we evaluated this ‘background noise’ by analyzing peripheral blood samples from 15 healthy male individuals in exactly the same way as patients. We estimated a cut-off based on PIM-1 normalized expression in respect to B2M expression in this control group (cut-off ΔΔCq = 1.51). Using this approach we defined a sample as positive PIM-1 for overexpression (PIM-1 positive) based on the fold change of PIM-1 expression in the EpCAM(+) fraction in respect to the corresponding EpCAM(+) fraction in the group of these 15 healthy individuals.
5. Conclusions
We conclude that PIM-1 overexpression is observed at high frequency in CTCs from mCRPC patients and this finding, in combination with AR-V7 expression in CTCs, suggests its potential role as a very promising target for cancer therapy. Our data point towards the direction of prospective further evaluation of PIM-1 mRNA overexpression in CTCs as a potential liquid biopsy-based biomarker in a large and well-defined cohort of mCRPC patients.
Acknowledgments
This research has been co-financed by the European Union and Greek national funds through the Operational Program Competitiveness, Entrepreneurship and Innovation, under the call RESEARCH–CREATE–INNOVATE (project code: T1RCI-02935).
Abbreviations
| ADT | Androgen Deprivation Therapy |
| AR | Androgen Receptor |
| AR-V7 | Androgen Receptor splice variant 7 |
| CTCs | Circulating Tumor Cells |
| CtDNA | Circulating tumor DNA |
| EMT | Epithelial Mesenchymal Transition |
| EVs | Extracellular Vesicles |
| HD | Healthy Donors |
| CRPC | Castration-Resistant Prostate Cancer |
| PB | Peripheral Blood |
| PCa | Prostate Cancer |
| PRAD | Prostate Adenocarcinoma |
| TPM | Transcripts Per Million |
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/12/5/1188/s1, Figure S1: PIM-1 expression in Prostate Adenocarcinoma Tumors (n = 492) and normal prostate tissues (n = 52) according to the TCGA, Table S1: Association between PIM-1 overexpression and AR-V7 expression levels in EpCAM(+) CTCs before treatment and clinical outcome of mCRPC patients (n = 44).
Author Contributions
A.M.: investigation, methodology, writing—original draft preparation, E.T.: investigation, methodology, writing—original draft preparation, A.S.: investigation, M.Z.: investigation, S.M.: investigation, E.B.: resources, and E.L.: supervision, writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the European Union and Greek national funds through the Operational Program Competitiveness, Entrepreneurship and Innovation, under the call RESEARCH–CREATE–INNOVATE, grant number: T1RCI-02935).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2018. CA Cancer J. Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.PDQ Adult Treatment Editorial Board . PDQ Cancer Information Summaries. National Cancer Institute (US); Bethesda, MD, USA: 2002. Prostate Cancer Treatment (PDQ®): Patient Version. 30 April 2018. [Google Scholar]
- 3.Scher H.I., Morris M.J., Stadler W.M., Higano C., Basch E., Fizazi K., Antonarakis E.S., Beer T.M., Carducci M.A., Chi K.N., et al. Trial Design and Objectives for Castration-Resistant Prostate Cancer: Updated Recommendations from the Prostate Cancer Clinical Trials Working Group 3. J. Clin. Oncol. 2016;34:1402–1418. doi: 10.1200/JCO.2015.64.2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pantel K., Hille C., Scher H.I. Circulating Tumor Cells in Prostate Cancer: From Discovery to Clinical Utility. Clin. Chem. 2019;65:87–99. doi: 10.1373/clinchem.2018.287102. [DOI] [PubMed] [Google Scholar]
- 5.Sumanasuriya S., De Bono J. Treatment of Advanced Prostate Cancer-A Review of Current Therapies and Future Promise. Cold Spring Harb. Perspect Med. 2018;8:a030635. doi: 10.1101/cshperspect.a030635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hendriks R.J., Van Oort I.M., Schalken J.A. Blood-based and urinary prostate cancer biomarkers: A review and comparison of novel biomarkers for detection and treatment decisions. Prostate Cancer Prostatic Dis. 2017;20:12–19. doi: 10.1038/pcan.2016.59. [DOI] [PubMed] [Google Scholar]
- 7.Filella X., Albaladejo M.D., Allué J.A., Castaño M.A., Morell-Garcia D., Ruiz M.À., Santamaría M., Torrejón M.J., Giménez N. Prostate cancer screening: Guidelines review and laboratory issues. Clin. Chem. Lab. Med. 2019;57:1474–1487. doi: 10.1515/cclm-2018-1252. [DOI] [PubMed] [Google Scholar]
- 8.Lianidou E., Hoon D. Circulating Tumor Cells and circulating Tumor DNA. In: Rifai N., Horvath A.-R., Wittwer C., editors. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 6th ed. Elsevier B.V.; Amsterdam, The Netherlands: 2017. pp. 1111–1144. [Google Scholar]
- 9.Pantel K., Alix-Panabières C. Liquid biopsy and minimal residual disease-latest advances and implications for cure. Nat. Rev. Clin. Oncol. 2019;16:409–424. doi: 10.1038/s41571-019-0187-3. [DOI] [PubMed] [Google Scholar]
- 10.Castro-Giner F., Aceto N. Tracking cancer progression: From circulating tumor cells to metastasis. Genome Med. 2020;12:31. doi: 10.1186/s13073-020-00728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alix-Panabières C. “Circulating Tumor Cells: Finding Rare Events for a Huge Knowledge of Cancer Dissemination”. Cells. 2020;3:661. doi: 10.3390/cells9030661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Bono J., Scher H.I., Montgomery R.B., Parker C., Miller M.C., Tissing H., Doyle G., Terstappen L.W., Pienta K.J., Raghavan D. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 2008;14:6302–6309. doi: 10.1158/1078-0432.CCR-08-0872. [DOI] [PubMed] [Google Scholar]
- 13.Scher H.I., Jia X., De Bono J.S., Fleisher M., Pienta K.J., Raghavan D., Heller G. Circulating tumour cells as prognostic markers in progressive, castration-resistant prostate cancer: A reanalysis of IMMC38 trial data. Lancet Oncol. 2009;10:233–239. doi: 10.1016/S1470-2045(08)70340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antonarakis E.S., Lu C., Wang H., Luber B., Nakazawa M., Roeser J.C., Chen Y., Mohammad T.A., Chen Y., Fedor H.L., et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl. J. Med. 2014;371:1028–1038. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antonarakis E.S., Lu C., Luber B., Wang H., Chen Y., Nakazawa M., Nadal R., Paller C.J., Denmeade S.R., Carducci M.A., et al. Androgen receptor splice variant 7 and efficacy of taxane chemotherapy in patients with metastatic castration-resistant prostate cancer. JAMA Oncol. 2015;1:582–591. doi: 10.1001/jamaoncol.2015.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strati A., Zavridou M., Bournakis E., Mastoraki S., Lianidou E. Expression pattern of androgen receptors, AR-V7 and AR-567es, in circulating tumor cells and paired plasma-derived extracellular vesicles in metastatic castration resistant prostate cancer. Analyst. 2019;144:6671–6680. doi: 10.1039/C9AN00999J. [DOI] [PubMed] [Google Scholar]
- 17.Narlik-Grassow M., Blanco-Aparicio C., Carnero A. The PIM family of serine/threonine kinases in cancer. Med. Res. Rev. 2014;34:136–159. doi: 10.1002/med.21284. [DOI] [PubMed] [Google Scholar]
- 18.Warfel N.A., Kraft A.S. PIM kinase (and Akt) biology and signaling in tumors. Pharmacol. Ther. 2015;151:41–49. doi: 10.1016/j.pharmthera.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cen B., Mahajan S., Wang W., Kraft A.S. Elevation of receptor tyrosine kinases by small molecule AKT inhibitors in prostate cancer is mediated by Pim-1. Cancer Res. 2013;73:3402–3411. doi: 10.1158/0008-5472.CAN-12-4619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tursynbay Y., Zhang J., Li Z., Tokay T., Zhumadilov Z., Wu D., Xie Y. Pim-1 kinase as cancer drug target: An update. Biomed. Rep. 2016;4:140–146. doi: 10.3892/br.2015.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Casillas A.L., Toth R.K., Sainz A.G., Singh N., Desai A.A. Hypoxia-Inducible PIM kinase expression promotes resistance to antiangiogenic agents. Clin. Cancer Res. 2018;24:169–180. doi: 10.1158/1078-0432.CCR-17-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawrence M.G., Obinata D., Sandhu S., Selth L.A., Wong S.Q., Porter L.H., Lister N., Pook D., Pezaro C.J., Goode D.L., et al. Patient-derived Models of Abiraterone- and Enzalutamide-resistant Prostate Cancer Reveal Sensitivity to Ribosome-directed Therapy. Eur. Urol. 2018;74:562–572. doi: 10.1016/j.eururo.2018.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang C., Qie Y., Yang T., Wang L., Du E., Liu Y., Xu Y., Qiao B., Zhang Z. Kinase PIM1 promotes prostate cancer cell growth via c-Myc-RPS7-driven ribosomal stress. Carcinogenesis. 2019;40:52–60. doi: 10.1093/carcin/bgy126. [DOI] [PubMed] [Google Scholar]
- 24.Wang J., Kim J., Roh M., Franco O.E., Hayward S.W., Wills M.L., Abdulkadir S.A. Pim1 kinase synergizes with c-MYC to induce advanced prostate carcinoma. Oncogene. 2010;29:2477–2487. doi: 10.1038/onc.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhanasekaran S.M., Barrette T.R., Ghosh D., Shah R., Varambally S., Kurachi K., Pienta K.J., Rubin M.A., Chinnaiyan A.M. Delineation of prognostic biomarkers in prostate cancer. Nature. 2001;412:822–826. doi: 10.1038/35090585. [DOI] [PubMed] [Google Scholar]
- 26.Valdman A., Fang X., Pang S.T., Ekman P., Egevad L. Pim-1 expression in prostatic intraepithelial neoplasia and human prostate cancer. Prostate. 2004;60:367–371. doi: 10.1002/pros.20064. [DOI] [PubMed] [Google Scholar]
- 27.Cibull T.L., Jones T.D., Li L., Eble J.N., Ann Baldridge L., Malott S.R., Luo Y., Cheng L. Overexpression of Pim-1 during progression of prostatic adenocarcinoma. J. Clin. Pathol. 2006;59:285–288. doi: 10.1136/jcp.2005.027672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holder S.L., Abdulkadir S.A. PIM1 kinase as a target in prostate cancer: Roles in tumorigenesis, castration resistance, and docetaxel resistance. Curr. Cancer Drug Targets. 2014;14:105–114. doi: 10.2174/1568009613666131126113854. [DOI] [PubMed] [Google Scholar]
- 29.Luszczak S., Kumar C., Sathyadevan V.K., Simpson B.S., Gately K.A., Whitaker H.C., Heavey S. PIM kinase inhibition: Co-targeted therapeutic approaches in prostate cancer. Signal. Transduct. Target Ther. 2020;5:7. doi: 10.1038/s41392-020-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moreno J.G., Gomella L.G. Evolution of the Liquid Biopsy in Metastatic Prostate Cancer. Urology. 2019;132 doi: 10.1016/j.urology.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Scher H.I., Graf R.P., Schreiber N.A., Jayaram A., Winquist E., McLaughlin B., Lu D., Fleisher M., Orr S., Lowes L., et al. Assessment of the validity of nuclear-localized androgen receptor splice variant 7 in circulating tumor cells as a predictive biomarker for castration-resistant prostate cancer. JAMA Oncol. 2018;4:1179–1186. doi: 10.1001/jamaoncol.2018.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Armstrong A.J., Halabi S., Luo J., Nanus D.M., Giannakakou P., Szmulewitz R.Z., Danila D.C., Healy P., Anand M., Rothwell C.J., et al. Prospective multicenter validation of androgen receptor splice variant 7 and hormone therapy resistance in high-risk castration-resistant prostate cancer: The PROPHECY study. J. Clin. Oncol. 2019;37:1120–1129. doi: 10.1200/JCO.18.01731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Markou A., Lazaridou M., Paraskevopoulos P., Chen S., Świerczewska M., Budna J., Kuske A., Gorges T.M., Joosse S.A., Kroneis T., et al. Multiplex Gene Expression Profiling of in Vivo Isolated Circulating Tumor Cells in High-Risk Prostate Cancer Patients. Clin. Chem. 2018;64:297–306. doi: 10.1373/clinchem.2017.275503. [DOI] [PubMed] [Google Scholar]
- 34.Josefsson A., Larsson K., Freyhult E., Damber J.E., Welén K. Gene Expression Alterations during Development of Castration-Resistant Prostate Cancer Are Detected in Circulating Tumor Cells. Cancers. 2019;12:39. doi: 10.3390/cancers12010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chimonidou M., Strati A., Malamos N., Georgoulias V., Lianidou E.S. SOX17 promoter methylation in circulating tumor cells and matched cell-free DNA isolated from plasma of patients with BrCa. Clin. Chem. 2013;59:270–279. doi: 10.1373/clinchem.2012.191551. [DOI] [PubMed] [Google Scholar]
- 36.Mastoraki S., Strati A., Tzanikou E., Chimonidou M., Politaki E., Voutsina A., Psyrri A., Georgoulias V., Lianidou E. ESR1 Methylation: A Liquid Biopsy–Based Epigenetic Assay for the Follow-up of Patients with Metastatic Breast Cancer Receiving Endocrine Treatment. Clin. Cancer Res. 2018;24:1500–1510. doi: 10.1158/1078-0432.CCR-17-1181. [DOI] [PubMed] [Google Scholar]
- 37.Friedlander T.W., Ngo V.T., Dong H., Premasekharan G., Weinberg V., Doty S., Zhao Q., Gilbert E.G., Ryan C.J., Chen W.T., et al. Detection and characterization of invasive circulating tumor cells derived from men with metastatic castration-resistant prostate cancer. Int. J. Cancer. 2014;134:2284–2293. doi: 10.1002/ijc.28561. [DOI] [PubMed] [Google Scholar]
- 38.Pixberg C.F., Raba K., Müller F., Behrens B., Honisch E., Niederacher D., Neubauer H., Fehm T., Goering W., Schulz W., et al. Analysis of DNA methylation in single circulating tumor cells. Oncogene. 2017;36:3223–3231. doi: 10.1038/onc.2016.480. [DOI] [PubMed] [Google Scholar]
- 39.El-Heliebi A., Hille C., Laxman N., Svedlund J., Haudum C., Ercan E., Kroneis T., Chen S., Smolle M., Rossmann C., et al. In Situ Detection and Quantification of AR-V7, AR-FL, PSA, and KRAS Point Mutations in Circulating Tumor Cells. Clin. Chem. 2018;64:536–546. doi: 10.1373/clinchem.2017.281295. [DOI] [PubMed] [Google Scholar]
- 40.Faugeroux V., Lefebvre C., Pailler E., Pierron V., Marcaillou C., Tourlet S., Billiot F., Dogan S., Oulhen M., Vielh P., et al. An Accessible and Unique Insight into Metastasis Mutational Content Through Whole-exome Sequencing of Circulating Tumor Cells in Metastatic Prostate Cancer. Eur. Urol. Oncol. 2019 doi: 10.1016/j.euo.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 41.Markou A., Farkona S., Schiza C., Efstathiou T., Kounelis S., Malamos N., Georgoulias V., Lianidou E. PIK3CA mutational status in circulating tumor cells can change during disease recurrence or progression in patients with breast cancer. Clin. Cancer Res. 2014;20:5823–5834. doi: 10.1158/1078-0432.CCR-14-0149. [DOI] [PubMed] [Google Scholar]
- 42.Tzanikou E., Markou A., Politaki E., Koutsopoulos A., Psyrri A., Mavroudis D., Georgoulias V., Lianidou E. PIK3CA hotspot mutations in circulating tumor cells and paired circulating tumor DNA in breast cancer: A direct comparison study. Mol. Oncol. 2019;13:2515–2530. doi: 10.1002/1878-0261.12540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arrouchi H., Lakhlili W., Ibrahimi A. A review on PIM kinases in tumors. Bioinformation. 2019;15:40–45. doi: 10.6026/97320630015040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Magnuson N.S., Wang Z., Ding G., Reeves R. Why target PIM-1 for cancer diagnosis and treatment? Future Oncol. 2010;9:1461–1478. doi: 10.2217/fon.10.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Asati V., Mahapatra D.K., Bharti S.K. PIM kinase inhibitors: Structural and pharmacological perspectives. Eur. J. Med. Chem. 2019;172:95–108. doi: 10.1016/j.ejmech.2019.03.050. [DOI] [PubMed] [Google Scholar]
- 46.Arrouchi H., Lakhlili W., Ibrahimi A. Re-positioning of known drugs for Pim-1 kinase target using molecular docking analysis. Bioinformation. 2019;15:116–120. doi: 10.6026/97320630015116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Casuscelli F., Ardini E., Avanzi N., Casale E., Cervi G., D’Anello M., Donati D., Faiardi D., Ferguson R.D., Fogliatto G., et al. Discovery and optimization of pyrrolo[1,2-a]pyrazinones leads to novel and selective inhibitors of PIM kinases. Bioorg. Med. Chem. 2013;21:7364–7380. doi: 10.1016/j.bmc.2013.09.054. [DOI] [PubMed] [Google Scholar]
- 48.Suchaud V., Gavara L., Giraud F., Nauton L., Thery V., Anizon F., Moreau P. Synthesis of pyrazolo[4,3-a]phenanthridines, a new scaffold for PIM kinase inhibition. Bioorg. Med. Chem. 2014;22:4704–4710. doi: 10.1016/j.bmc.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 49.El-Nassan H.B., Naguib B.H., Beshay E.A. Synthesis of new pyridothienopyrimidinone and pyridothienotriazolopyrimidine derivatives as pim-1 inhibitors. J. Enzym. Inhib. Med. Chem. 2018;33:58–66. doi: 10.1080/14756366.2017.1389921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abouzid K.A.M., Al-Ansary G.H., El-Naggar A.M. Eco-friendly synthesis of novel cyanopyridine derivatives and their anticancer and PIM-1 kinase inhibitory activities. Eur. J. Med. Chem. 2017;134:357–365. doi: 10.1016/j.ejmech.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 51.Bataille C.J.R., Brennan M.B., Byrne S., Davies S.G., Durbin M., Fedorov O., Huber K.V.M., Jones A.M., Knapp S., Liu G., et al. Thiazolidine derivatives as potent and selective inhibitors of the PIM kinase family. Bioorg. Med. Chem. 2017;25:2657–2665. doi: 10.1016/j.bmc.2017.02.056. [DOI] [PubMed] [Google Scholar]
- 52.Nishiguchi G.A., Atallah G., Bellamacina C., Burger M.T., Ding Y., Feucht P.H., Garcia P.D., Han W., Klivansky L., Lindvall M. Discovery of novel 3,5- disubstituted indole derivatives as potent inhibitors of PIM-1, PIM-2, and PIM-3 protein kinases. Bioorg. Med. Chem. Lett. 2011;21:6366–6369. doi: 10.1016/j.bmcl.2011.08.105. [DOI] [PubMed] [Google Scholar]
- 53.Fan Y.B., Li K., Huang M., Cao Y., Li Y., Jin S.Y., Liu W.B., Wen J.C., Liu D., Zhao L.X. Design and synthesis of substituted pyrido[3,2-d]-1,2,3-triazines as potential PIM-1 inhibitors. Bioorg. Med. Chem. Lett. 2016;26:1224–1228. doi: 10.1016/j.bmcl.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 54.Wurz R.P., Pettus L.H., Jackson C., Wu B., Wang H.L., Herberich B., Cee V., Lanman B.A., Reed A.B., Chavez F.J., et al. The discovery and optimization of aminooxadiazoles as potent PIM kinase inhibitors. Bioorg. Med. Chem. Lett. 2015;25:847–855. doi: 10.1016/j.bmcl.2014.12.067. [DOI] [PubMed] [Google Scholar]
- 55.Li K., Li Y., Zhou D., Fan Y., Guo H., Ma T., Wen J., Liu D., Zhao L. Synthesis and biological evaluation of quinoline derivatives as potential anti-prostate cancer agents and PIM-1 kinase inhibitors. Bioorg. Med. Chem. 2016;24:1889–1897. doi: 10.1016/j.bmc.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 56.Zavridou M., Mastoraki S., Strati A., Tzanikou E., Chimonidou M., Lianidou E. Evaluation of Preanalytical Conditions and Implementation of Quality Control Steps for Reliable Gene Expression and DNA Methylation Analyses in Liquid Biopsies. Clin. Chem. 2018;64:1522–1533. doi: 10.1373/clinchem.2018.292318. [DOI] [PubMed] [Google Scholar]
- 57.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta DeltaC(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.