To rapidly communicate short reports of innovative responses to Covid-19 around the world, along with a range of current thinking on policy and strategy relevant to the pandemic, the Journal has initiated the Covid-19 Notes series.
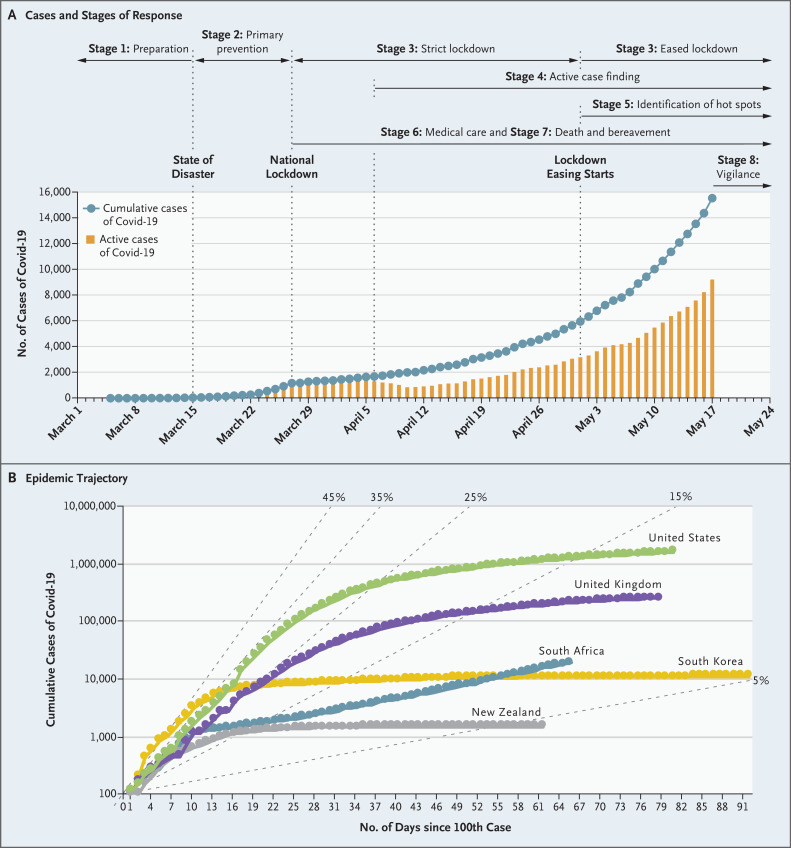
The first person with confirmed Covid-19 in South Africa was a traveler who had returned from Italy and was diagnosed on March 5, 2020. When 402 cases had been identified after 18 days, the government announced a national lockdown, which was implemented 4 days later when the doubling time was 2 days and there were 1170 identified cases (Figure 1A). During 35 days of strict lockdown, the doubling time slowed to 15 days, and there were 5647 cases (including 103 deaths) by April 30. As of May 19, when a less strict lockdown was in place, South Africa had recorded 17,200 cases and 312 deaths and had conducted 488,609 tests (www.gov.za/Coronavirus).
Figure 1. Covid-19 in South Africa.
Panel A shows the number of cumulative and active cases of Covid-19 and the stages of South Africa’s response. Panel B shows the trajectory of the Covid-19 epidemic in South Africa and in selected other countries. Diagonal lines indicate hypothetical trajectories for daily increases in cases. Data for Panel B are from Tulio de Oliveira, Maria Schuld, and the University of KwaZulu-Natal CoV Big Data Consortium.
South Africa’s national Covid-19 response has comprised eight overlapping stages. The first stage was focused on preparing for Covid-19, including establishing testing capacity. Stage 2 started when there were 51 cases, 10 days after the first South African patient was diagnosed. The government declared a national state of disaster, banning international travel, closing schools, restricting gatherings, and promoting social distancing and hand hygiene. A high-level advisory committee with 51 clinicians, virologists, epidemiologists, mathematical modelers, public health practitioners, and other experts is providing strategic advice to the minister of health and establishing evidence-based policy guidance.
Stage 3 consisted of the national lockdown, which is now being eased slowly. The lockdown has caused substantial economic hardship, especially among poor and vulnerable people. The contraction of the economy could have important long-term consequences. Restrictions on movement and the risk of contracting Covid-19 in health care facilities has brought major reductions in the use of health services, thereby compromising continuity of care for people with HIV, tuberculosis (TB), and chronic noncommunicable diseases.
During Stage 4, which was initiated on day 33, the government has deployed more than 28,000 community health workers to the highest-risk communities to undertake active house-to-house case finding. South Africa’s community contact-tracing teams, established for TB control, have been used for Covid-19 contact tracing and monitoring of compliance with quarantine. With the highest HIV burden in the world, the country has a network of providers, including tens of thousands of trained community health workers experienced in conducting door-to-door visits in socially vulnerable communities. This community-based response has been used to screen 11,114,600 people (almost 20% of the population) for Covid-19. A mobile-phone application is used to administer a symptom checklist, and data for each household are uploaded, along with mobile-phone location coordinates, to a central database to map screening coverage. People with Covid-19 symptoms are referred to mobile testing stations or nearby health facilities.
Stage 5 involves identification of hot spots and implementation of prevention measures in areas with localized outbreaks. Stage 6 is focused on providing medical care, including constructing field hospitals — some in convention centers. Stage 7 involves preparing for deaths, burials, and the mental health challenges associated with bereavement. The final stage focuses on staying vigilant by engaging in case-finding activities and monitoring population immunity levels using serosurveys in preparation for subsequent epidemic waves.
Several challenges may hinder epidemic control. The country is trying to further scale up testing from the current cumulative rate of 9.6 tests per 1000 people. Initially restrictive criteria made it difficult for people to get tested in public clinics and hospitals, with private-sector providers conducting about 80% of tests. The criteria were changed after about 1 month, and most testing now occurs in the public sector. Securing sufficient testing supplies and personal protective equipment for health care personnel has been challenging.
Poverty and unemployment mean many people live in informal settlements where implementing preventive interventions such as hand washing and social distancing is difficult. These vulnerable communities utilize public health care services; more than 80% of South Africans don’t have medical insurance. There were 7.9 million people living with HIV and about a quarter million incident cases of TB in South Africa in 2018. Covid-19 could add severe strain to the already overburdened health care system, particularly if people with HIV or TB are at higher risk of developing severe Covid-19 illness. The potential for a double whammy looms as South Africa prepares to enter its annual influenza season.
South Africa’s early interventions have delayed the Covid-19 peak (Figure 1B). Its response is being implemented in the face of constrained resources and other challenges. The national commitment to responding to the epidemic provides hope that the country won’t experience the devastation seen elsewhere. As South Africa braces for an expected surge of cases over the coming weeks, I describe the national Covid-19 response as “sailing a ship while building it.”
Disclosure Forms
This note was published on May 29, 2020, at NEJM.org.
Dr. Abdool Karim is chair of the South African Ministerial Advisory Committee for Covid-19.
Footnotes
Disclosure forms provided by the author are available with the full text of this note at NEJM.org.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.