Abstract
Background:
Outcomes and complications at mid- or long-term follow-up after medial open-wedge high tibial osteotomy (MOWHTO) with the TomoFix locking plate have not been fully evaluated.
Purpose:
To evaluate the complications and midterm clinical outcomes after MOWHTO using a TomoFix.
Study Design:
Case series; Level of evidence, 4.
Methods:
Enrolled in this study were 80 patients (85 knees) who underwent MOWHTO with the TomoFix locking plate between 2009 and 2013. There were 66 women and 14 men, with a mean age of 61.5 years at the time of surgery. The diagnosis was medial osteoarthritis in 76 knees and spontaneous osteonecrosis of the knee in 9 knees. Metal removal and second-look arthroscopy were performed in all cases. Clinical and radiological examinations were performed at final follow-up after surgery (mean, 4.5 years).
Results:
The mean Japanese Orthopaedic Association score and Knee injury and Osteoarthritis Outcome Score improved significantly from pre- to postoperatively (P < .0001). The weightbearing line percentage shifted to pass through a point 67.7% lateral from the medial edge of the tibial plateau. The Caton-Deschamps index changed significantly from 0.88 to 0.66 at final follow-up (P < .0001). The mean posterior tibial slope changed significantly from 8.9° to 11.9° at final follow-up (P < .0001). Limb length was significantly increased after MOWHTO (10.3 mm; P < .0001). During plate removal, 14 locking screws were found to be broken in 9 knees (10.6%). The articular cartilage grade of the patellofemoral joint was significantly higher in the second arthroscopy than in the first arthroscopy (P < .0001). The cumulative rate of all complications was 41.2%, with major complications (ie, those requiring additional or extended treatment) in 24.7%.
Conclusion:
Postoperative outcome scores indicated significant improvement after MOWHTO, although the cumulative rate of all complications was 41.2% and the rate of major complications was 24.7%. These results indicate that MOWHTO with the TomoFix is a technically demanding procedure. Careful preoperative planning and meticulous surgical technique are needed to decrease the incidence of complications associated with MOWHTO.
Keywords: complications, high tibial osteotomy, knee osteoarthritis, medial open-wedge
In 2003, Staubli et al41 modified the conventional medial open-wedge high tibial osteotomy (MOWHTO) procedure by developing a biplanar osteotomy and applying stable fixation with the TomoFix locking plate (Depuy Synthes). This MOWHTO procedure now provides surgeons many advantages in comparison with lateral closed-wedge high tibial osteotomy (HTO). The most notable advantages of the MOWHTO are that correction of the limb alignment is not difficult and that the risk of peroneal nerve palsy is minimized because fibular osteotomy is not needed.39,41,43 In addition, recent studies have reported that the improved MOWHTO can allow patients early weightbearing after surgery.43 However, mid- or long-term clinical outcomes after MOWHTO with the TomoFix remain unclear, although many studies have reported that the short-term results after the MOWHTO are good.8,17,33,34,37,41
Several recent studies have pointed out that MOWHTO with the TomoFix is frequently associated with various types of complications during or after surgery.6,21,27,44–46 For example, Marti et al27 reported that MOWHTO created an adverse deformity of the tibia, such as an increase in the posterior tibial slope (PTS) and elongation of tibial length. Brouwer et al6 showed that patellar height was significantly decreased after MOWHTO, and Takeuchi et al44 reported that lateral hinge fractures occurred in 25% of MOWHTO cases.
The purpose of this study was to clarify the midterm (3-7 year) follow-up results after MOWHTO using the TomoFix as well as major and minor complications found throughout the follow-up period. Drawing on previous studies,32,35,44 we made the following hypotheses: (1) clinical outcomes of MOWHTO may be significantly improved and (2) various degrees of complications may occur during or after MOWHTO.
Methods
Study Design
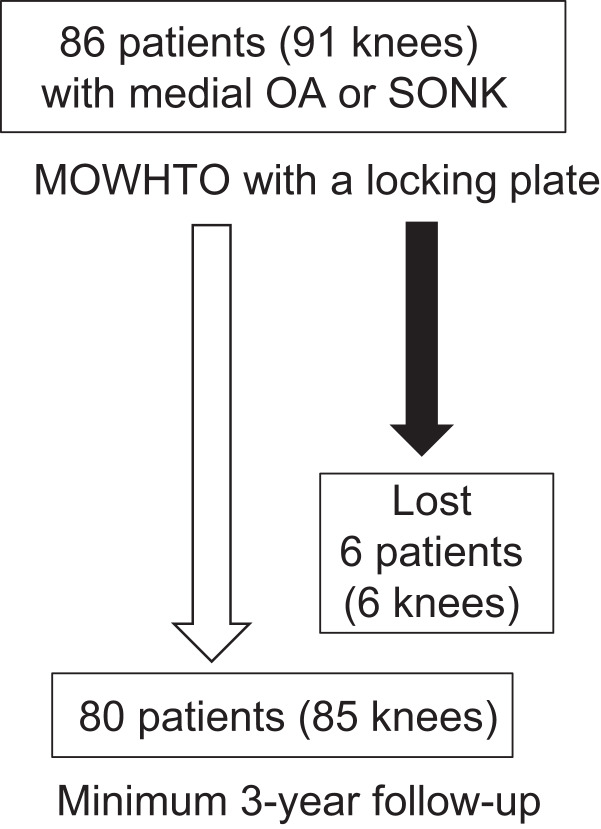
A prospective case series was conducted between January 2009 and July 2013 involving patients who underwent MOWHTO with a locking plate. All operations were performed by 1 of 2 senior orthopaedic surgeons (T.Y. and E.K.) who were sufficiently trained in knee surgery. The study inclusion criteria were persistent pain due to medial osteoarthritis (OA) or spontaneous osteonecrosis of the knee in the medial femoral condyle after nonoperative treatment for at least 3 months. Exclusion criteria included (1) lateral femorotibial angle (FTA) greater than 185°; (2) a loss of knee extension greater than 15°; (3) range of knee motion less than 130°; (4) history of knee infection; (5) severe patellofemoral joint OA; (6) anterior cruciate ligament insufficiency or varus/valgus instability greater than 10°; and (7) smokers.44 The study design was approved by the institutional review board of the Hokkaido University Hospital, and informed consent was obtained from all individual participants. A total of 86 patients (91 knees) were enrolled in this study. We followed up with the patients in our outpatient clinic for 3 years or more after surgery; 6 patients were lost to follow-up. Thus, a total of 80 patients (85 knees) participated in this study and underwent clinical and radiological evaluations (Figure 1). The diagnosis was medial osteoarthritis in 76 knees and spontaneous osteonecrosis of the knee in 9 knees.
Figure 1.
Study design and follow-up examinations. MOWHTO, medial open-wedge high tibial osteotomy; OA, osteoarthritis; SONK, spontaneous osteonecrosis of the knee.
All patients underwent follow-up at an average of 4.5 years (range, 3-7 years). The patients were first evaluated in our outpatient clinic at 3 months after surgery. After 1 year, we evaluated the patients annually. Radiological examinations were carried out to detect adverse deformities of the tibia, via computed digital radiograph (Fujifilm), before and immediately after surgery and at the final follow-up. The patients had digital radiographs in our outpatient clinic at 1, 2, 3, 4, 5, 6, 9, and 12 months after surgery, then annually thereafter. To evaluate bone union, we divided the osteotomized gap area of the coronal plane into 5 zones according to Brosset et al.5 Bone union was defined as mature trabecular continuity in zone 3, the lateral hinge point, and the ascending osteotomy site of the tibial tuberosity, as observed through use of anteroposterior (AP) and lateral digital radiographs.35 Delayed union and nonunion were defined as lack of mature trabecular continuity in these areas more than 4 and 6 months after surgery, respectively. Radiological measurements were performed by 2 observers (K.Y. and J.O.).
Each patient underwent an additional procedure approximately 1 year (mean, 13 months; range, 7-30 months) after the initial surgery to remove the implanted TomoFix, because patients wanted the metal plate removed for religious reasons.15,24 Arthroscopic examinations were performed twice, immediately before surgery and during plate removal, to evaluate morphological changes of the articular cartilage in the knee joint.
Patient Demographics
There were 66 women and 14 men enrolled in the study, with a mean age of 61.5 years at the time of surgery. Their background characteristics are shown in Table 1.
Table 1.
Background Characteristics of the Patientsa
| Age, y | 61.5 (40-78) |
| Sex, male/female, n | 14/66 |
| Body mass index, kg/m2 | 27.0 (18.8-43.4) |
| Young adult mean, % | 89.8 (57-112) |
aData except for patient sex are reported as mean (range). The young adult mean is a ratio (percentage) of the bone density in patients to the normal bone density in a young adult.
Preoperative Planning
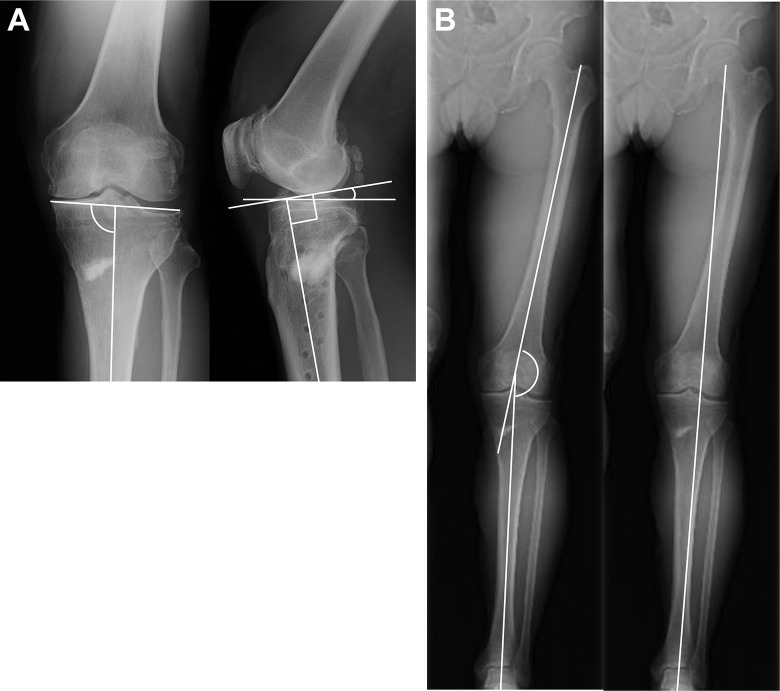
Preoperative planning with an appropriate correction angle of the tibia was performed through use of a standing full-length lower limb AP radiograph.30 The surgical planning method is shown in Figure 2.
Figure 2.
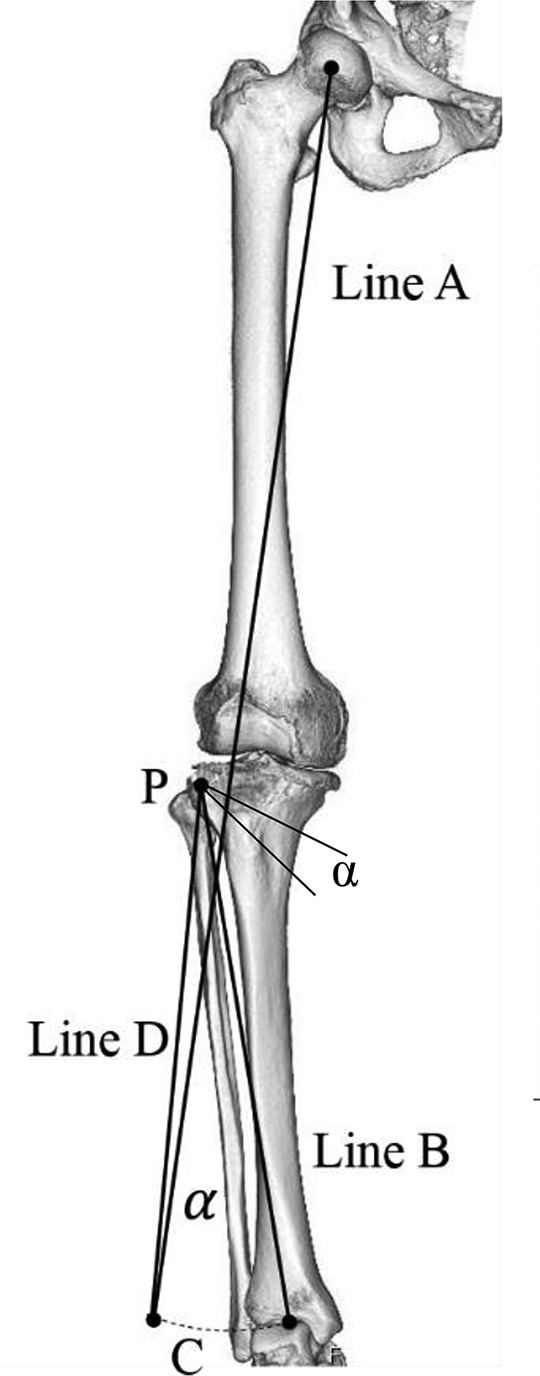
Preoperative planning. An appropriate correction angle of the tibia is determined by use of a standing, full-length, lower limb anteroposterior radiograph. Open-wedge osteotomy lines are drawn on the full-length lower limb radiograph so that the hinge point (P) is located at approximately 5 mm medial from the tibiofibular joint on the lateral tibial condyle. To calculate an appropriate angle of the medial opening wedge, a long line (line A) is drawn from the center of the femoral head through the point 62.5% lateral from the medial edge of the tibial plateau on the lateral tibial plateau. Then, another line (line B) is drawn from hinge point P to the center of the talar dome, and the length of line B is measured. Then an arc (C), the center and the radius of which are the hinge point P and line B, respectively, is drawn so that the arc is across line A. Next, a line (line D) is drawn from hinge point P to the crossing point between line A and arc C. The angle (α) formed between line B and line D provides the medial opening angle, which is identical to the correction angle of the lower limb alignment. A medial opening line is drawn using this angle.
MOWHTO Procedure
This MOWHTO procedure has been reported in detail previously.35 The proximal tibia was exposed through a 7-cm medial longitudinal incision. After the complete release of the distal attachment of the superficial medial collateral ligament, 3 pairs of Kirschner wires (K-wires) were inserted into the tibia so that each inserted K-wire precisely reached the proximal tibiofibular joint using the parallel guide. Next, a biplanar osteotomy of the tibia, which consisted of an oblique HTO and a frontal plane osteotomy behind the tibial tubercle,2 was performed with an oscillating saw and chisel. The oblique osteotomy site was then gradually opened by use of a protractor-installed specially designed spreader (Olympus Terumo Biomaterials) under fluoroscopic control based on preoperative planning. Under fluoroscopic control, and using a long, straight metal rod, the surgeon confirmed that the mechanical axis of the corrected lower limb passed through the Fujisawa point (62.5%) on the tibial plateau.12 Then, 2 wedge-shaped β-tricalcium phosphate spacers (Osferion 60; Olympus Terumo Biomaterials) were implanted into the anterior and posterior parts of the opening space.35 Finally, the tibia was fixed with a locking plate (TomoFix) by insertion of 8 locking screws. All screws were tightened through use of a torque driver. All screw holes were used as suggested by the manufacturer. The TomoFix Medial High Tibia Plate (model 440.834) and the small TomoFix Medial High Tibia Plate (Asian version, model 440.831) were used in this study. The small plate is indicated for all tibial open-wedge osteotomies in patients less than 65 kg in weight.
As additional treatments for the intra-articular lesions, partial meniscectomy of the medial meniscus was performed in 68 knees. Osteochondral autograft transfer was carried out in 12 knees by use of the Osteochondral Autograft Transfer System (OATS; Arthrex); the mean size of the articular defects was 3.2 cm2 (range, 2-4 cm2). A donor graft was harvested from the lateral femoral trochlea.
Postoperative Rehabilitation
After surgery, all patients underwent postoperative management using the same rehabilitation protocol reported previously.35 Straight-leg raising and quadriceps sitting exercises, as well as active and passive knee motion exercises, were encouraged on the day after surgery.35 Partial weightbearing was permitted with crutches 2 weeks after surgery. Full weightbearing was allowed 4 weeks after surgery.
Clinical Evaluation
The patients were evaluated by use of the Japanese Orthopaedic Association (JOA) score2,47 and Knee injury and Osteoarthritis Outcome Score (KOOS)36 at preoperative and final follow-up periods in our outpatient clinic. The JOA score was the primary outcome measure, as it is the standard knee function scale in Japan. Based on previous studies,2,47 the results were graded as good for scores of 85 to 100 points, fair for 70 to 84, and poor for 69 or less.
Radiological Evaluation
AP view radiographs of the knee and the whole lower limb were taken with the patient in the single-leg standing position. Lateral and skyline view radiographs at 30° of flexion were taken in the nonloading condition. On the AP radiograph of the knee, the radiological stage of OA was assessed according to the Kellgren-Lawrence grading system.20 Using the AP view of the whole limb radiograph, we measured the FTA, the medial-proximal tibial angle (MPTA), the point at which the weightbearing line passed across the joint line (WBL point), the length of the tibia, and the length of the lower limb. Using the lateral radiograph of the knee, we determined the patellar height ratios and the PTS (Figure 3). The PTS was defined as the angle between the line perpendicular to the middiaphysis of the tibia and the posterior inclination of the medial tibial plateau.
Figure 3.
Postoperative radiographs 7 years after surgery. (A) The medioproximal tibial angle was defined as the angle between the proximal tibial joint line and the mechanical axis of the tibial shaft. The posterior tibial slope was defined as the angle between the line perpendicular to the middiaphysis of the tibia and the posterior inclination of the medial tibial plateau. (B) The lateral femorotibial angle was defined as the angle between the longitudinal axes of the femur and the tibia. The point at which the weightbearing line passed across the joint line (WBL point) was drawn from the center of the femoral head to the middle point of the ankle joint surface, and the WBL point was shown as a ratio (%) of the length between the point and the medial edge of the tibial plateau, which was divided by the width of the whole tibial plateau.
Arthroscopic Examination
Arthroscopic examinations were performed before MOWHTO and at the plate removal surgery to evaluate the degree of cartilage degeneration in the medial tibiofemoral joints and the patellofemoral joint, through use of the International Cartilage Repair Society (ICRS) classification.4 All arthroscopic examinations were performed by 2 senior orthopaedic surgeons (T.Y. and E.K.) who were sufficiently trained in arthroscopic surgery. Under arthroscopic evaluation, the articular surface was evaluated as the most progressive grade at the femur or the tibia in the medial femorotibial joint and at the femoral trochlea or the patella in the patellofemoral joint.
Complications
When a complication was clinically or radiologically detected during surgery or follow-up, it was recorded in the electronic medical record system. Intraoperative lateral hinge fractures were classified by location according to Takeuchi et al44 as type I (just proximal to or within the tibiofibular joint), type II (distal portion of the proximal tibiofibular joint), or type III (lateral plateau). Martin et al28 reported classifications for adverse events as follows: class 1 events were considered those that required no additional treatment or very minor alterations in postoperative care; class 2 events required additional or extended nonoperative treatment for a limited period of time; and class 3 events required either long-term medical treatment or additional surgery. Using their system, we categorized complications as minor (class 1) or major (classes 2 and 3).
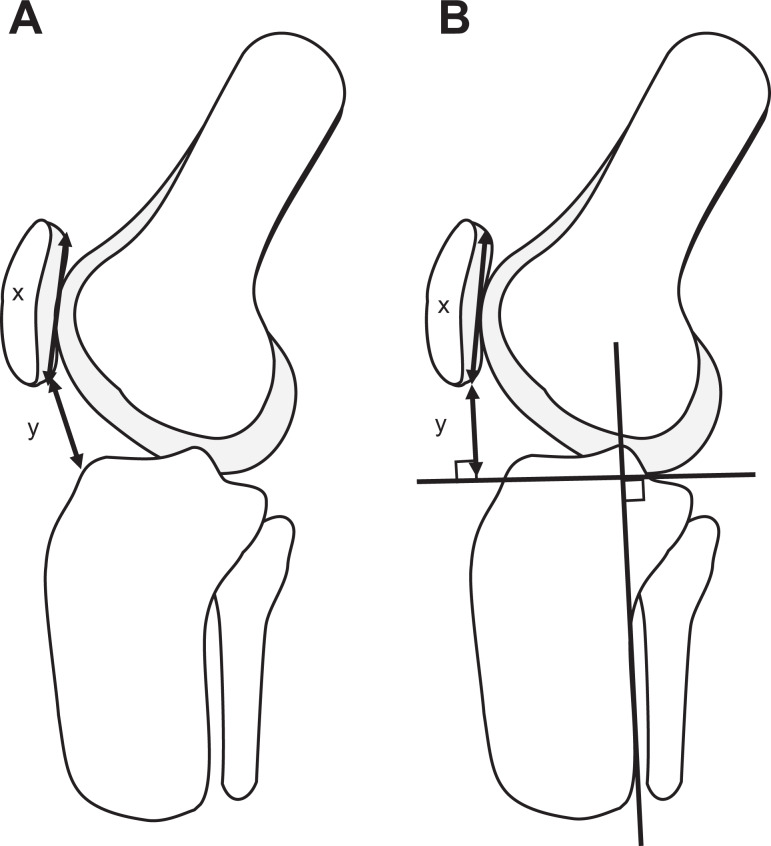
To quantify the postoperative deformity of the patellar height as a complication after MOWHTO, we measured the Insall-Salvati ratio,19 which was defined as the length of the patellar tendon (the distance between the inferior pole of the patella and the tibial tubercle) divided by the patellar length. Additionally, the Caton-Deschamps (C-D) index7 and the Miura-Kawamura (M-K) index31 were measured at 30° of knee flexion (Figure 4).
Figure 4.
Measurement of the patellar height ratios. (A) The Caton-Deschamps index was defined as a ratio of the distance (y) between the inferior pole of the patella and the anteroproximal edge of the tibial plateau divided by the patellar length (x). (B) To calculate the Miura-Kawamura index, a line perpendicular to the axis of the tibia was drawn at the distal end of the femur. The distance (y) between the lower end of the articular surface of the patella and the distal femoral line was divided by the length (x) of the articular surface of the patella.
Statistical Analysis
An a priori power analysis was performed. In our previous study,35 the difference between the pre- and postoperative clinical outcome was 28.0%. Based on this result, a sample size of 80 patients (85 knees) was calculated to have greater than 80% power to test the hypothesis. All data are shown as means with range. For each preoperative and postoperative parameter, the paired Student t test and the chi-square test were used to test for significance. JMP Pro10.0 for Windows (SAS Institute Japan) was used for statistical analyses. The significance level was set at P = .05.
The inter- and intrarater reliabilities for the radiological measurements were 0.91 (range, 0.85-0.96) and 0.93 (range, 0.86-0.98), respectively. The inter- and intrarater reliabilities for the arthroscopic evaluations were satisfactory (mean inter- and intraclass correlation coefficients, 0.81 [range, 0.72-0.88] and 0.85 [range, 0.80-0.92], respectively).
Results
Clinical Results
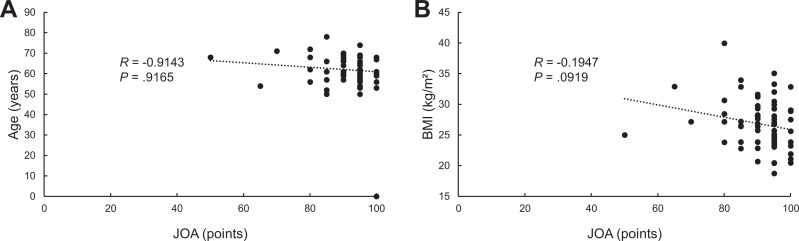
Regarding knee pain and function, the mean JOA score significantly (P < .0001) improved, from 65.6 to 90.8 at the final follow-up evaluation (Table 2). The final follow-up results were graded as good in 72 knees (84.7%), fair in 10 knees (11.8%), and poor in 3 knees (3.5%). The total KOOS and each of the KOOS subscale scores also significantly improved (P < .0001) (Table 2). The mean loss of knee extension was slightly but significantly improved, from –5.1° to –2.3° (P < .0001) (Table 2). The 3 knees graded as poor underwent total knee arthroplasty (TKA) at 8, 11, and 23 months after MOWHTO because of residual knee pain in 1 knee and unexpected deformity of the proximal tibia in 2 knees. In addition, we compared clinical scores among MOWHTO, MOWHTO with meniscectomy, and MOWHTO with OATS, finding no significant differences among the 3 groups. We analyzed the effect of age and body mass index (BMI) on the JOA scores and found no significant correlations (Figure 5).
Table 2.
Clinical Evaluationa
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| Extension angle, deg | –5.1 (–20 to 0) | –2.3 (–15 to 0) | <.0001 |
| Flexion angle, deg | 138.9 (125 to 155) | 140.3 (115 to 155) | .6520 |
| JOA score | 65.6 (50 to 80) | 90.8 (50 to 100) | <.0001 |
| Knee function, n (%) | |||
| Good: 85-100 points | 1 (1.2) | 72 (84.7) | |
| Fair: 70-85 points | 26 (30.6) | 10 (11.8) | |
| Poor: ≤69 points | 58 (68.2) | 3 (3.5) | |
| KOOS | |||
| Pain | 46.8 (0 to 69) | 81.4 (57 to 100) | <.0001 |
| Symptoms | 54.5 (7 to 82) | 82.5 (50 to 100) | <.0001 |
| Activities of Daily Living | 59.2 (10 to 84) | 87.2 (57 to 100) | <.0001 |
| Sports/Recreation | 25.8 (0 to 65) | 57.9 (0 to 100) | <.0001 |
| Quality of Life | 26.6 (6 to 56) | 64.2 (25 to 100) | <.0001 |
aData are reported as mean (range) unless otherwise noted. JOA, Japanese Orthopaedic Association; KOOS, Knee injury and Osteoarthritis Outcome Score.
Figure 5.
Correlation between Japanese Orthopaedic Association (JOA) score and (A) age and (B) body mass index (BMI).
Radiological Evaluation
During surgery, an average wedge opening of 11.7° (mean opening distance, 12.2 mm) was made in the tibia by means of the protractor-installed specially designed spreader and caliper. Under fluoroscopic control, and using a long, straight metal rod, the surgeon confirmed that the mechanical axis of the corrected lower limb passed through at least the Fujisawa point (62.5%) on the tibial plateau. Our previous studies demonstrated that an FTA of 164° to 168° should be attained to ensure favorable long-term results in HTO.2,47 Therefore, our correction tended to overcorrect. At the final follow-up, the mean WBL point was significantly (P < .0001) corrected, from 26.9% to 67.7%, and the mean FTA was significantly (P < .0001) corrected, from 179.6° to 169.8° (Table 3). No significant difference was seen between the pre- and postoperative radiographic OA grades (Table 3).
Table 3.
Radiographic Evaluationa
| Preoperative | Immediately After Surgery | Final Follow-up | P Value | |
|---|---|---|---|---|
| Open wedge angle, deg | NA | 11.7 (8.0-16.7) | NA | NA |
| Maximum open distance, mm | NA | 12.2 (8.0-18.3) | NA | NA |
| WBL point, % | 26.9 (–14.4 to 46.9) | 68.3 (56.0 to 82.4) | 67.7 (50.7 to 86.6) | <.0001b
.2006c |
| FTA, deg | 179.6 (176.5 to 186.0) | 169.7 (165.5 to 175.5) | 169.8 (163.5 to 177.9) | <.0001b
.9455c |
| Radiographic OA grade, n of kneesd | .5976 | |||
| Grade 1 | 0 | 0 | ||
| Grade 2 | 0 | 0 | ||
| Grade 3 | 21 | 17 | ||
| Grade 4 | 58 | 59 | ||
| Grade 5 | 6 | 9 |
aData are reported as mean (range) unless otherwise noted. FTA, lateral femorotibial angle; NA, not applicable; OA, osteoarthritis; WBL, weightbearing line.
bPreoperative vs final follow-up data.
cImmediately after surgery vs final follow-up data.
dDetermined via the Kellgren-Lawrence grading system.
Arthroscopic Evaluation
The findings from the preoperative and postoperative (at plate removal) arthroscopic evaluations are shown in Table 4. No significant differences were found in the medial femorotibial joint between the first and second evaluations. However, the articular cartilage grade of the patellofemoral joint was significantly higher in the second arthroscopy than in the first arthroscopy (P < .0001).
Table 4.
Arthroscopic Evaluations of the Articular Cartilagea
| ICRS Classification | First Arthroscopy | Second Arthroscopy | P Value |
|---|---|---|---|
| Medial femoral joint | .9840 | ||
| Grade 0 | 0 | 0 | |
| Grade 1 | 0 | 0 | |
| Grade 2 | 22 | 22 | |
| Grade 3 | 28 | 27 | |
| Grade 4 | 35 | 36 | |
| Patellofemoral joint | <.0001 | ||
| Grade 0 | 36 | 14 | |
| Grade 1 | 30 | 27 | |
| Grade 2 | 12 | 32 | |
| Grade 3 | 5 | 9 | |
| Grade 4 | 2 | 3 |
aData are reported as number of knees. ICRS, International Cartilage Repair Society.
Complications
Intraoperatively, lateral hinge fractures occurred in 25 knees (29.4%) (Table 5). After surgery, 2 knees (2.3%) had superficial infections around the skin incision for 3 months postoperatively, although no patients had deep infections. Within 1 year postoperatively, unacceptable overcorrection, the FTA of which was 162°, occurred in 1 knee, correction loss greater than 5° occurred in 2 knees, and nonunion occurred in 1 knee. In the patient with unacceptable overcorrection, we performed revision open-wedge HTO at 1 week after the first surgery. In the 2 patients with correction loss and increased PTS (>10°), TKA was performed 8 and 11 months after surgery. In the patient with nonunion, after 6 months a revision open-wedge HTO and iliac bone graft was performed by use of bilateral plate fixation. No cases of popliteal vascular injury, peroneal nerve injury, tibial tubercle fracture, or compartment syndrome were noted. The rate of major complications was 24.7%. Of these, 9.4% were class 3 and 15.3% were class 2 according to the classification by Martin et al28 (Table 5). Our analysis revealed no significant differences between age or BMI and the occurrence of complications.
Table 5.
Complications in Medial Open-Wedge High Tibial Osteotomy
| No. of Knees (%) | |
|---|---|
| Minor (class 1a): no additional treatment required | 14 (16.5) |
| Intraoperative lateral hinge fracture type Ib | 14 (16.5) |
| Major (class 2): adverse events requiring additional or extended nonoperative management | 13 (15.3) |
| Intraoperative lateral hinge fracture types II and III | 5 (5.9); 1 type II, 4 type III |
| Superficial infection | 1 (1.2) |
| Implant failure | 7 (8.2) |
| Proximal locking screw breakage | 3 (3.5) |
| Distal locking screw breakage | 4 (4.7) |
| Major (class 3): additional surgery or long-term nonoperative treatment required | 8 (9.4) |
| Overcorrection (with type I fracture) | 1 (1.2) |
| Nonunion (with type II fracture, implant failure) | 1 (1.2) |
| Loss of correction >5° (with type III fracture) | 2 (2.3) |
| Increased posterior tibial slope >10° (with type I fracture) | 2 (2.3) |
| Superficial infection requiring surgery | 1 (1.2) |
| Implant failure: distal locking screw breakage (with tibial fracture) | 1 (1.2) |
| Other complications | |
| Difficulty with inserted screws during hardware removal | 9 (10.6) |
| Increased tibial length >10 mm | 23 (27.1) |
| Patella baja (Caton-Deschamps index <0.6) | 32 (37.6) |
The postoperative adverse deformities of the tibia on radiological evaluation are shown in Table 6. Patellar height was significantly reduced as a result of the surgery. Namely, the preoperative C-D index (mean, 0.88) was significantly (P < .0001) decreased to 0.71 immediately after surgery and 0.66 at final follow-up (Table 6), and 32 of the 85 knees (37.6%) showed a patella baja: a C-D index less than 0.6. The M-K index showed similar results. The mean PTS increased significantly from 8.9° to 11.9° at final follow-up (P < .0001). We think that an incomplete cutting of the posterior cortex of the proximal tibia caused an increase of PTS of more than 10° in 2 knees. Tibial length and whole lower limb length were both significantly (P < .0001) increased after surgery (Table 6), although the patients did not desire lengthening of the limb.
Table 6.
Adverse Deformity of the Tibiaa
| Preoperative | Immediately After Surgery | Final Follow-up | P Value | |
|---|---|---|---|---|
| Caton-Deschamps index | 0.88 (0.67 to 1.33) | 0.71 (0.48 to 1.15) | 0.66 (0.38 to 1.10) | <.0001b
.1731c |
| Miura-Kawamura index | 0.81 (0.52 to 1.22) | 0.73 (0.43 to 1.16) | 0.70 (0.46 to 1.14) | <.0001b
.0585c |
| Insall-Salvati ratio | 0.91 (0.67 to 1.31) | 0.91 (0.64 to 1.31) | 0.94 (0.64 to 1.48) | .1342b
.1907c |
| Posterior tibial slope, deg | 8.9 (4.0 to 16.0) | 11.6 (3.0 to 19.6) | 11.9 (4.1 to 21.7) | <.0001b
.0563c |
| Tibial length, mm | 321.3 (276.5 to 382.2) | 328.8 (280.0 to 389.9) | 329.1 (277.9 to 389.9) | <.0001b
.2249c |
| ▵Tibial length, mm | NA | 8.9 (0.2 to 17.7) | 8.6 (–1.9 to 15.5) | |
| Whole lower limb length, mm | 730.2 (630.4 to 852.8) | 739.1 (636.3 to 854.7) | 740.5 (636.1 to 855.0) | <.0001b
.9757c |
| ▵Whole lower limb length, mm | NA | 10.3 (–6.5 to 21.0) | 10.3 (–7.2 to 20.0) |
aData are reported as mean (range). NA, not applicable.
bPreoperative vs final follow-up.
cImmediate after surgery vs final follow-up.
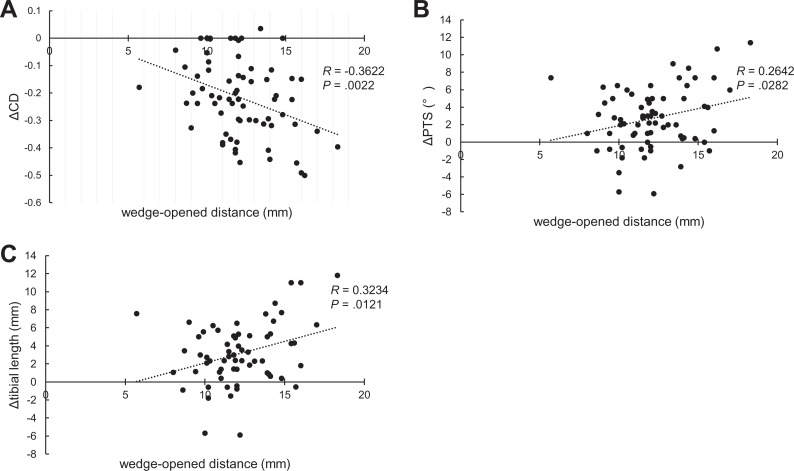
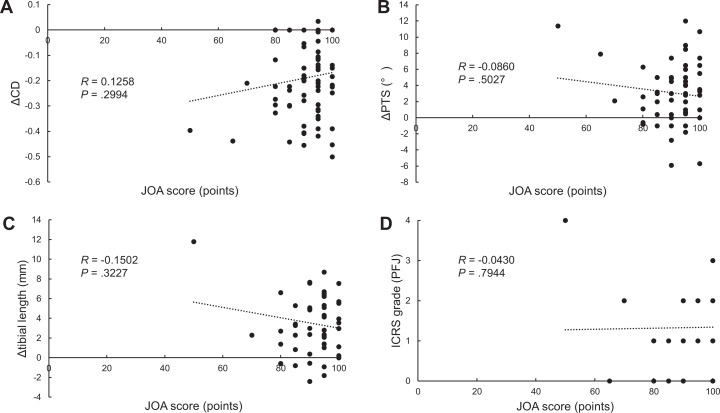
Pearson correlation coefficient showed significant correlations between the wedge-opened distance and the degree of patellar height (P = .0022 for C-D index; P = .0173 for M-K index), the degree of PTS (P = .0282), and the length of the tibia (P = .0121) (Figure 6). No significant correlations were found between the JOA score and the degree of patellar height (P = .2994 for C-D index; P = .6424 for M-K index), the degree of PTS (P = .5027), the length of the tibia (P = .3227), or ICRS grade (patellofemoral joint; P = .7944) (Figure 7).
Figure 6.
Correlation between the wedge-opened distance and (A) change in Caton-Deschamps index (▵CD), (B) change in posterior tibial slope (▵PTS), and (C) ▵tibial length.
Figure 7.
Correlation between Japanese Orthopaedic Association (JOA) score and (A) change in Caton-Deschamps index (▵CD), (B) change in posterior tibial slope (▵PTS), (C) ▵tibial length, and (D) International Cartilage Repair Society (ICRS) grade (patellofemoral joint [PFJ]).
Each patient underwent an additional procedure approximately 1 year (mean, 13 months; range, 7-30 months) after the initial surgery to remove the implanted TomoFix. During the plate removal surgery, complications were found or occurred in a total of 9 knees (10.6%) in 85 operations (Table 5). We confirmed that 14 locking screws were broken. Of these cases, 1 knee had nonunion, in which 3 of the proximal locking screws had broken. An additional 3 knees had 1 or 2 broken locking screws at the time of plate removal; the proximal screw breakages were found on postoperative radiograph at approximately 6 months after surgery. In these cases, we removed the inserted screw by hollowing out the bone tissue with a core reamer. In 5 knees, 7 screws inserted into the distal tibia were so tightly locked to the plate that we could not turn the screw head. In these cases, after we destroyed the screw head with a carbide-alloy drill, we detached the plate from the screws and then removed the inserted screw by hollowing out the bone tissue. In 1 of the 7 knees, a crack occurred in the tibial cortex during the hollowing procedure.
Discussion
The present study showed that the 3- to 7-year follow-up clinical results after MOWHTO using the TomoFix were good for 84.7% of patients. Saito et al37 also reported good results in a series of 64 patients who underwent MOWHTO with the TomoFix. In the current study, various degrees of complications occurred during or after MOWHTO, even though the clinical results were good. Intraoperatively, lateral hinge fractures occurred in 29.4% of patients. Within 1 year postoperatively, a case of unacceptable overcorrection, a case of nonunion, and 2 cases of correction loss were identified.
The radiological evaluation showed that MOWHTO resulted in adverse deformities of the tibia. First, although decreasing the C-D index did not cause symptoms or problems, it was significantly reduced from 0.88 preoperatively to 0.66 at final follow-up. In the second arthroscopy, progression of the ICRS grade was seen in the patellofemoral joint, and although the result was statistically significant, the deterioration was not clinically significant. Second, the mean PTS was significantly increased from 8.9° to 11.9° but, again, this result carried no clinical implications. Third, the length of the entire lower limb was significantly increased after surgery, due to lengthening of the tibia and correction of the varus deformity of functional limb shortening. Additionally, during the plate removal surgery at approximately 1 year after surgery, complications related to breakage of the inserted screws were found in 10.6% of 85 knees.
Complications associated with MOWHTO have been reported to occur in 0% to 55% of cases.¶ For example, Hernigou and Ma18 reported a complication rate of 5.3% in a series of 245 patients who underwent MOWHTO with plaster cast. Niemeyer et al33 noted an 8.6% complication rate among the cases involving the TomoFix plate. Miller et al29 reported a 37% overall complication rate using Puddu plate and VS Osteotomy Plate (EBI). Spahn et al40 reported complications with 34% of the cases using a Puddu-plate (Arthrex) or C-plate (Königsee-Implantate; Aschau). Martin et al28 reported that the rate of class 2 and class 3 complications was 36.7%. The cumulative rate of all complications detected in the present study was 41.2%. However, the rate of major complications was 24.7%. These results indicate that the MOWHTO procedure with the TomoFix is a technically demanding procedure, although the overall clinical results were good.
Among the complications found in the present study, there was 1 knee with nonunion. In this knee, a type II lateral hinge fracture had occurred during the MOWHTO surgery. There were 2 knees with alignment correction loss greater than 5°. In these knees, type III lateral hinge fracture had occurred during the surgery. We did not perform additional fixation to type III lateral hinge fracture. In these patients, rehabilitation protocol was changed. Takeuchi et al44 reported that the type II and type III lateral hinge fractures were unstable and frequently caused delayed union and nonunion, alignment correction loss, and increasing PTS. Several authors reported that disruption of the lateral hinge in MOWHTO was observed in 2.6% to 35% of cases.# Takeuchi et al44 reported that lateral cortex fractures were observed in 26 knees (25%). Nakamura et al32 reported that 20% of cases sustained lateral hinge fractures after MOWHTO. In addition, Lee et al25 reported that 27.5% of cases had lateral hinge fractures as identified on computed tomography scans. In the current study, the lateral hinge fracture rate was 29.4%. Han et al16 recommended that to lessen the chance of a fracture, the first oblique osteotomy should be started from the upper margin of the pes anserinus and end 5 mm from the lateral cortical margin, just above the proximal tibiofibular joint, to establish a “safe zone.” Therefore, meticulous care should be taken during the MOWHTO procedure to decrease the incidence of lateral hinge fractures.
The most frequent radiographic change seen after this MOWHTO procedure with ascending tibial tuberosity osteotomy was patella baja as a deformity of the tibia. Namely, the C-D index was less than 0.6 in 37.6% of the patients. Patella baja is known as an adverse deformity of the knee. Recently, Goshima et al14 reported that cartilage degeneration was frequently found in the patellofemoral joint in patients after MOWHTO surgery. In the present study, a similar finding was observed at the time of the hardware removal surgery. Although Goshima et al14 reported that the patella baja induced by the MOWHTO surgery did not result in a significant reduction of functional results in the short-term evaluation, there is a risk that the functional results may be significantly reduced in the long-term follow-up evaluation. The present study clearly showed a significant correlation between the wedge-opened distance and the degree of patella baja (Figure 6). This finding indicates that this complication is unavoidable in MOWHTO when the tibial alignment requires large correction.
Recently, several authors reported descending tibial tuberosity osteotomy in MOWHTO.1,10,11,13 Erquicia et al10 reported that MOWHTO with a dihedral L-cut distal and posterior to the tibial tubercle accurately corrected axial malalignment without any change at the patellofemoral joint or any modification to the posterior tibial slope while providing improved knee function at short-term follow-up. They concluded that the radiographic as well as the clinical results support the use of this technique to treat medial compartment knee OA and varus malalignment in young and middle-aged patients with a normal to low patellar height. Floerkemeier et al11 reported that a descending tuberosity cut was recommended to prevent anterior knee pain as well as patella baja in large open-wedge corrections. Another group using a proximal ascending tuberosity osteotomy reported that the patellar height and the angle of correction were related: the larger the correction angle, the lower the postoperative patellar height and the higher the patellofemoral contact stress.42 It should be kept in mind that a painful retropatellar OA should be an exclusion criterion for MOWHTO because of the risk of increased retropatellar pressure and pain impairment postoperatively.
An increase in the PTS by 10° or more was not frequent (2.3%) in the present study, but we found a significant correlation between the wedge-opened distance and the degree of the PTS. El-Azab et al9 reported that the PTS showed a significant increase of 2.1° after MOWHTO. In our previous study,35 we recommended that the tibia be osteotomized with the TomoFix in a hyperextended position of the knee. We believe that this fixation technique is useful to prevent a large increase of the PTS. In addition, the surgeon can open the posterior aspect of the osteotomy more than the anterior aspect to avoid increasing the PTS.
However, the deformity of the tibia after this MOWHTO procedure included a significant increase of lower limb length, an average of 10.3 mm. We noted a significant correlation between the wedge-opened distance and the length of the tibia (Figure 6). Bae et al3 reported that the mean change in limb length was 7.8 mm after MOWHTO. Commonly, a lower limb length discrepancy of less than 20 mm does not cause significant disability in walking. In our clinical experience, however, some patients have complained of an uncomfortable sensation in walking or running. Thus, we do not recommend MOWHTO for knees that need large alignment correction. However, the length gain may be a desired outcome, as the limb is usually shortened from the varus deformity and medial wear, and patients complain if a single knee is addressed where there is bilateral disease.
Each patient underwent an additional procedure approximately 1 year after the initial surgery to remove the implanted plate, because Japanese patients desire to remove the metal materials after surgery due to religious reasons and cultural factors, which include sitting on tatami flooring.15,24 We believe that the case of tibial fracture might not have occurred if the plate had not been removed. In addition, patients wished to confirm the knee condition at the time of plate removal. Arthroscopic examinations were performed twice, immediately before surgery and during plate removal to evaluate morphological changes of the articular cartilage in the knee joint. In the present study, proximal locking screws were broken in 4 knees (4.7% of the cases), and distal locking screws were broken in 5 knees (5.9% of the cases). This suggests that changes could be made to improve the fixation system or to slow down the rehabilitation program to avoid screw breakage. Maehara et al26 suggested that surgeons should be concerned about plate removal, and patients should be well-informed about the possibility of difficulty removing locking screws.
There are some limitations in this study. First, it was a case series. Second, the follow-up period averaged only 4.5 years, and long-term follow-up is needed. Third, we did not assess articular cartilage using magnetic resonance imaging (MRI). In the future, we should conduct an MRI study concerning the alteration of articular cartilage.
Conclusion
Postoperative outcome scores indicated significant improvement after the MOWHTO procedure, although the cumulative rate of all complications was 41.2% and the rate of major complications was 24.7%. These results indicate that MOWHTO with the TomoFix is a technically demanding procedure. Careful preoperative planning and meticulous surgical technique are needed to decrease the incidence of complications associated with MOWHTO.
Acknowledgment
Many thanks go to Mr Mitsuya Urata and Olympus Terumo Biomaterials Corporation, Tokyo, Japan, for development of the surgical instruments used in this study.
Footnotes
Final revision submitted February 4, 2020; accepted February 13, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Hokkaido University Hospital.
References
- 1. Akiyama T, Osano K, Mizu-Uchi H, et al. Distal tibial tuberosity arc osteotomy in open-wedge proximal tibial osteotomy to prevent patella infra. Arthrosc Tech. 2019;8(6):e655–e662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aoki Y, Yasuda K, Mikami S, Ohmoto H, Majima T, Minami A. Inverted V-shaped high tibial osteotomy compared with closing-wedge high tibial osteotomy for osteoarthritis of the knee: ten-year follow-up result. J Bone Joint Surg Br. 2006;88(10):1336–1340. [DOI] [PubMed] [Google Scholar]
- 3. Bae DK, Song SJ, Kim HJ, Seo JW. Change in limb length after high tibial osteotomy using computer-assisted surgery: a comparative study of closed- and open-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):120–126. [DOI] [PubMed] [Google Scholar]
- 4. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85(suppl 2):58–69. [DOI] [PubMed] [Google Scholar]
- 5. Brosset T, Pasquier G, Migaud H, Gougeon F. Opening wedge high tibial osteotomy performed without filling the defect but with locking plate fixation (TomoFixTM) and early weight bearing: prospective evaluation of bone union, precision and maintenance of correction in 51 cases. Orthop Traumatol Surg Res. 2011;97:705–711. [DOI] [PubMed] [Google Scholar]
- 6. Brouwer RW, Bierma-Zeinstra SMA, van Raaij TM, Verhaar JAN. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. J Bone Joint Surg Br. 2006;88(B):1454–1459. [DOI] [PubMed] [Google Scholar]
- 7. Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera: apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 8. Darees M, Putman S, Brosset T, Roumazeille T, Pasquier G, Migaud H. Opening-wedge high tibial osteotomy performed with locking plate fixation (TomoFix) and early weight-bearing but without filling the defect: a concise follow-up note of 48 cases at 10 years’ follow-up. Orthop Traumatol Surg Res. 2018;104(4):477–480. [DOI] [PubMed] [Google Scholar]
- 9. El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90:1193–1197. [DOI] [PubMed] [Google Scholar]
- 10. Erquicia J, Gelber PE, Perelli S, et al. Biplane opening wedge high tibial osteotomy with a distal tuberosity osteotomy, radiological and clinical analysis with minimum follow-up of 2 years. J Exp Orthop. 2019;6(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):170–180. [DOI] [PubMed] [Google Scholar]
- 12. Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee: an arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 13. Gaasbeek RD, Sonneveld H, van Heerwaarden RJ, Jacobs WC, Wymenga AB. Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee. 2004;11(6):457–461. [DOI] [PubMed] [Google Scholar]
- 14. Goshima K, Sawaguchi T, Shigemoto K, et al. Large opening gaps, unstable hinge fractures, and osteotomy line below the safe zone cause delayed bone healing after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1291–1298. [DOI] [PubMed] [Google Scholar]
- 15. Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Nakanishi A, Ueoka K. Patellofemoral osteoarthritis progression and alignment changes after open-wedge high tibial osteotomy do not affect clinical outcomes at mid-term follow-up. Arthroscopy. 2017;33(10):1832–1839. [DOI] [PubMed] [Google Scholar]
- 16. Han SB, Lee DH, Shetty GM, Chae DJ, Song JG, Nha KW. A “safe zone” in medial open-wedge high tibia osteotomy to prevent lateral cortex fracture. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):90–95. [DOI] [PubMed] [Google Scholar]
- 17. Hantes ME, Natsaridis P, Koutalos AA, Ono Y, Doxariotis N, Malizos KN. Satisfactory functional and radiological outcomes can be expected in young patients under 45 years old after open wedge high tibial osteotomy in a long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3199–3205. [DOI] [PubMed] [Google Scholar]
- 18. Hernigou P, Ma W. Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee. 2001;8(2):103–110. [DOI] [PubMed] [Google Scholar]
- 19. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. [DOI] [PubMed] [Google Scholar]
- 20. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim GB, Kim KI, Song SJ, Lee SH. Increased posterior tibial slope after medial open-wedge high tibial osteotomy may result in degenerative changes in anterior cruciate ligament. J Arthroplasty. 2019;34(9):1922–1928. [DOI] [PubMed] [Google Scholar]
- 22. Kim KI, Kim DK, Song SJ, Lee SH, Bae DK. Medial open-wedge high tibial osteotomy may adversely affect the patellofemoral joint. Arthroscopy. 2017;33(4):811–816. [DOI] [PubMed] [Google Scholar]
- 23. Kim KI, Kim GB, Kim HJ, Lee SH, Yoon WK. Extra-articular lateral hinge fracture does not affect the outcomes in medial open-wedge high tibial osteotomy using a locked plate system. Arthroscopy. 2018;34(12):3246–3255. [DOI] [PubMed] [Google Scholar]
- 24. Kondo E, Yasuda K. Second-look arthroscopic evaluations of anatomic double-bundle anterior cruciate ligament reconstruction: relation with postoperative knee stability. Arthroscopy. 2007;23:1198–1209. [DOI] [PubMed] [Google Scholar]
- 25. Lee BS, Jo BK, Bin SI, Kim JM, Lee CR, Kwon YH. Hinge fractures are underestimated on plain radiographs after open wedge proximal tibial osteotomy: evaluation by computed tomography. Am J Sports Med. 2019;47(6):1370–1375. [DOI] [PubMed] [Google Scholar]
- 26. Maehara T, Moritani S, Ikuma H, Shinohara K, Yokoyama Y. Difficulties in removal of the titanium locking plate in Japan. Injury. 2013;44(8):1122–1126. [DOI] [PubMed] [Google Scholar]
- 27. Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20(4):366–372. [DOI] [PubMed] [Google Scholar]
- 28. Martin R, Birmingham TB, Willits K, Litchfield R, Lebel ME, Giffin JR. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med. 2014;42(5):1118–1126. [DOI] [PubMed] [Google Scholar]
- 29. Miller BS, Downie B, McDonough EB, Wojtys EM. Complications after medial opening wedge high tibial osteotomy. Arthroscopy. 2009;25(6):639–646. [DOI] [PubMed] [Google Scholar]
- 30. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy: a new fixation device. Clin Orthop Relat Res. 1989;246:250–259. [PubMed] [Google Scholar]
- 31. Miura H, Kawamura H, Nagamine R. Is patellar height really lower after high tibial osteotomy? Fukuoka Igaku Zassi. 1997;88:261–266. [PubMed] [Google Scholar]
- 32. Nakamura R, Komatsu N, Fujita K, et al. Appropriate hinge position for prevention of unstable lateral hinge fracture in open wedge high tibial osteotomy. Bone Joint J. 2017;99(10):1313–1318. [DOI] [PubMed] [Google Scholar]
- 33. Niemeyer P, Koestler W, Kaehny C, Kreuz PC, Brooks CJ, Strohm PC. Two-year results of open-wedge high tibial osteotomy with fixation by medial plate fixator for medial compartment arthritis with varus malalignment of the knee. Arthroscopy. 2008;24(7):796–804. [DOI] [PubMed] [Google Scholar]
- 34. Niemeyer P, Schmal H, Haushild O, von Heyden J, Sudkamp NP, Kostler W. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy. 2010;26:1607–1616. [DOI] [PubMed] [Google Scholar]
- 35. Onodera J, Kondo E, Omizu N, Ueda D, Yagi T, Yasuda K. Beta-tricalcium phosphate shows superior absorption rate and osteoconductivity compared to hydroxyapatite in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;22(11):2763–2770. [DOI] [PubMed] [Google Scholar]
- 36. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 37. Saito T, Kumagai K, Akamatsu Y, Kobayashi H, Kusayama Y. Five- to ten-year outcome following medial opening-wedge high tibial osteotomy with rigid plate fixation in combination with an artificial bone substitute. Bone Joint J. 2014;96(3):339–344. [DOI] [PubMed] [Google Scholar]
- 38. Song EK, Seon JK, Park SJ, Jeong MS. The complications of high tibial osteotomy: closing-versus opening-wedge methods. J Bone Joint Surg Br. 2010;92(B):1245–1252. [DOI] [PubMed] [Google Scholar]
- 39. Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg. 2004;124(10):649–653. [DOI] [PubMed] [Google Scholar]
- 40. Spahn G, Kirschbaum S, Kahl E. Factors that influence high tibial osteotomy results in patients with medial gonarthritis: a score to predict the results. Osteoarthritis Cartilage. 2006;14(2):190–195. [DOI] [PubMed] [Google Scholar]
- 41. Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34(suppl 2):B55–B62. [DOI] [PubMed] [Google Scholar]
- 42. Stoffel K, Willers C, Korshid O, Kuster M. Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1094–1100. [DOI] [PubMed] [Google Scholar]
- 43. Takeuchi R, Ishikawa H, Aratake M, et al. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009;25(1):46–53. [DOI] [PubMed] [Google Scholar]
- 44. Takeuchi R, Ishikawa H, Kumagai K, et al. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy. 2012;28(1):85–94. [DOI] [PubMed] [Google Scholar]
- 45. Tanaka T, Matsushita T, Miyaji N, et al. Deterioration of patellofemoral cartilage status after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1347–1354. [DOI] [PubMed] [Google Scholar]
- 46. Woodacre T, Ricketts M, Evans JT, et al. Complications associated with opening wedge high tibial osteotomy. Knee. 2016;23:276–282. [DOI] [PubMed] [Google Scholar]
- 47. Yasuda K, Majima T, Tsuchida T, Kaneda K. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res. 1992;282:186–195. [PubMed] [Google Scholar]