Abstract
Objective.
To describe the behavior of breast cancer (BC) during the 1962-2012 period from information provided by the Cali Cancer Registry and the Municipal Health Secretariat of Cali.
Materials and methods.
The incidence trend (1962-2007) and mortality trend (1984-2012) for breast cancer was studied and relative survival (RS)(1995-2004) was estimated. Age-standardized incidence and mortality rates to the world population (ASIR(w)/ASMR(w)) were expressed per 100 000 persons-year. Their temporal trend was examined with the annual percent of change (APC), and the Cox model was used to analyze the variables that influenced the survival of women with breast cancer.
Results.
The risk of breast cancer significantly increased in Cali through the 1962-2007 period, with an APC =1.7(95%CI:1.4-2.0). The ASIR(w) of BC increased from 27.1 in 1962 to 48.0 in 2007 and currently there are more than 500 cases reported annually. The mortality for BC has remained stable since 1984; in the 2009-2012 period, the ASMR(w) was 14.2. The 5-year RS was 69% (95%CI:66-71) from 2000-2004 and 62% (95%CI:59-65) from 1995-1999. The risk of death (HR) from BC was greater in persons from lower socioeconomic strata (SES) than from higher SES, HR=1.9(95%CI:1.3-2.9) and in those older than 70 years vs. <50, HR= 1,6(95%CI; 1.1-2.2).
Conclusion.
Mortality remained stable while incidence increased and survival improved, which may be associated with better detection and advances in treatment.
Keywords: diseases registries, breast cancer, survival analysis, trend studies, incidence rate, mortality, Colombia
Abstract
Objetivo.
Describir el comportamiento del cáncer de mama (CaMa) entre 1962 y 2012 con la información del Registro Poblacional de Cáncer de Cali y de la Secretarýa de Salud Municipal de Cali, Colombia.
Material y métodos.
Se estudió la tendencia de la incidencia (1962-2007) y mortalidad (1984-2012) por CaMa y se estimó la supervivencia relativa (SR) (1995-2004). Las tasas de incidencia y mortalidad estandarizadas por edad con población estándar mundial (TIEE(m)/TMEE(m)) se expresan por 100 000 personas/año. Su tendencia temporal fue estudiada con el porcentaje de cambio anual (APC, por su sigla en inglés) y el modelo de Cox fue utilizado para analizar las variables que influyen en la supervivencia.
Resultados.
La TIEE(m) de CaMa aumentó de 27.1 en 1962 a 48.0 en 2007 y actualmente más de 500 casos son registrados anualmente, con un APC de 1.7(IC95%: 1.4-2.0). La mortalidad por CaMa ha permanecido estable desde 1984; en el periodo 2009-2012 la TMEE(m) fue 14.2. La SR a cinco años fue 69% (IC95%:66-71) durante el periodo 2000-2004 y 62% (IC95%: 59-65) entre 1995 y 1999. El riesgo de morir (HR, por su sigla en inglés) por CaMa fue mayor en las personas de estratos socioeconómicos (ESE) bajos vs ESE altos, HR= 1.9(IC5%: 1.3-2.9) y en los mayores de 70 años vs los menores de 50, HR=1.6(95%CI: 1.1-2.2).
Conclusión.
La mortalidad estable, con aumento de la incidencia y mejor supervivencia, puede estar asociada con una mejor detección y avances en el tratamiento.
Keywords: registros de enfermedades, cáncer de mama, análisis de supervivencia, estudios de tendencia, incidencia, mortalidad, Colombia
Breast cancer (BC) is the most common cancer in women worldwide, comprising 16% of all female cancers and it is the leading cause of cancer-related death. Around half a million women die from BC each year, and although it is thought to be a disease of the developed world, a majority (69%) of all BC deaths occur in developing countries.1
The Globocan database for 2008 indicates that the age-standardized rate (ASR) of BC incidence is 66.4 per 100 000 in more developed regions (Europe, Australia, New Zealand, North America and Japan) compared with 27.1 per 100 000 in less developed regions (Africa, Central America, South America, all regions of Asia except Japan, the Caribbean, Melanesia, Micronesia and Polynesia). The highest incidence (ASR) occurs in Western Europe (89.7 per 100 000) and the lowest in Asia (26) and Eastern Africa (19.3).1
An estimated 1.7 million women will be diagnosed with breast cancer in 2020, a 26% increase from current levels.2 These rising cancer rates will be greatest in developing countries, and are projected to reach a 55% increased incidence and 58% increased mortality in fewer than 20 years.3 In the region of the Americas, the incidence rate of breast cancer increased from 18 to 35% between 1980 and 2008, and the mortality rate increased 18% from 2002 to 2008, with large regional variability (higher rates in the Southern Cone countries, such as Uruguay and Argentina).2 Unfortunately, the case-fatality rate within these nations tends to be higher than in developed countries, largely due to patients presenting at more advanced stages.4 The high probability of dying from breast cancer across the developing world further reflects the inequities in early detection and access to treatment.5 There is strong evidence that lower educational levels and lesser income status contribute to diagnosis delay.4
There are many known risk factors for breast cancer and most of them are related to the woman’s reproductive history, e.g. early menarche, late first childbirth, low parity and late menopause. Women who take oral contraceptive pills and hormonal replacement therapy (HRT) have an increased risk. Obesity and reduced physical activity have also been linked to increased risk. Women who drink more are more likely to have breast cancer but the link between cigarette smoking and breast cancer is debatable. Over the last two decades of the twentieth century, widespread implementation of screening mammography led to a steady increase in BC diagnoses in most developed countries. After a steady increase in BC incidence throughout the 1990s, an unprecedented decrease in incidence of 6.7% occurred from 2002 to 2003 in the USA. Implicated in this decline was the dramatic decrease in the use of postmenopausal hormone therapy (HT). Several ecological studies reported temporal correlations between HT discontinuation and decreased BC incidence.6–9 However, this decreased incidence has not been observed among women of Latin America.10
The purpose of this study was to describe the relative survival, incidence and mortality rates found between 1962 and 2012 using information from the Cancer Registry in Cali, Colombia (RPCC in Spanish) and the mortality databases from the Cali Secretariat of Municipal Public Health.
Materials and methods
The RPCC has operated continuously since 1962 in Cali, the third largest city of Colombia. The area of registry is 119 km2 and corresponds to the city’s urban zone. Most of the inhabitants are mestizos (ancestral admixture of Amerindians and Caucasian). More than half are immigrants, mostly from other parts of Colombia. According to the 2005 census, Cali had a population of 2 030 000 inhabitants. An ecological time series analysis was used on the incidence rate trends for 1962-2007, the mortality rates from 1984-2012, and the relative survival analysis from cases of breast cancer in Cali from 1995 to 2004.
The data analyzed was obtained from the Cancer Registry in Cali, Colombia (RPCC) and from the mortality database containing individual death records at the Secretariat of Municipal Public Health in Cali (SSPM in Spanish). We included new cases of breast cancer diagnosed in women of all ages living in Cali between 1962 and 2007. Mortality rates were estimated for the period 1984-2012. There was no mortality information for periods prior to 1984.
The RPCC uses quality assurance procedures advocated by the IARC to validate the quality and completeness of cancer registration.11 The details with respect to the history, objectives, logistics and coverage of RPCC have been previously described. Similarly, incidence data and data quality indices for these data have been previously published in all nine volumes of Cancer Incidence in Five Continents.12 For the last period (2003-2007), the percentage of BC cases morphologically verified was 95.6%; the mortality to incidence ratio (M:I) was 30.8% and the percentage of records abstracted from death certificates only (DCO) was 0.7%. A high quality index was observed for cancer death registration with 92.8% of the cancer deaths properly certified. The percentage of omissions of age at time of death was 0.2%. The percentage of an unknown and non-specific primary site of the cancer (C76-C80) was 6.7%. Death certificates were signed by physicians in nearly all cases (99.7%).
The prevailing International Classification of Diseases (ICD) was used for cancer classification. Three ICD versions have been used over the length of time that registration has been conducted. According to a WHO ICD translator, ICD-8 and ICD-9 breast cancer codes (174.0-174.9) map only to ICD-10 breast cancer codes (C50.0-C50.9), and vice versa. To define multiple tumors the guidelines of IARC were followed.13 Age was categorized into three groups: “less than 50”, “50-69”, and “70 and over”. The socioeconomic stratum (SES) was assigned according to the guidelines of the Municipal Planning Department of Cali, that classifies residential property into six strata. The lower-lower economic stratum and the lower stratum were grouped together as low, the medium-low and medium were grouped as medium, and the medium-high and high-high strata were grouped as high. Of the 3 798 cases for survival analysis, 83.0% had at least one residential address and they were zoned on the digital map. Information was available for 966 women about the stage of the tumor, and it was classified according to the American Joint Committee on Cancer.14
For the survival analysis from BC, 3 798 cases recorded during the period 1995-2004 were considered. Women between the ages 16 to 80 year’s at the time of diagnosis were eligible for the study. The survival analysis excluded from the study: tumors identified as in situ, benign or uncertain-acting tumors, multiple tumors or those detected only at necropsy, or that were only evident from the death certificate, women with cancer diagnosed before 1995 and any subsequent malignancy occurring with the same individual after 1995. To compare the survival trends from BC, the total period was divided into two periods: a first period from 01/01/95 to 12/31/99; and a second from 01/01/2000 to 12/31/2004. The latter dates mark the implementation of health care reform in Colombia.15
To update vital status and the date of last contact, cross-matching was made between the RPCC information system and the following databases: a) death certificates from SSPM, 1984-2010, b) hospital discharges mainly from hospitals of levels II-III, c) identification and classification system of the potential beneficiaries of social programs (SISBEN 2008),15 d) and public and private insurers from Valle de Cauca.15 Cases lacking individual updating were searched for in the information system of the Solidarity Fund and the Warranty Security System in Health (FOSYGA).15 The residual list of unmatched cases was sent to the National Office of Identification, and the public telephone company in Cali. Telephone contact was made by a professional psychology member of the research group.
Statistical analysis:
The population structure by age was obtained from the National Bureau of Statistics of Colombia (DANE).16 Age-standardized incidence/mortality rates (ASIR(w)/ASMR (w)) were calculated by the direct method, using the world standard population as reference. Age-specific incidence/mortality rates (ASIR/ASMR) and (ASIR(w)/ASMR(w)) are expressed per 100 000 persons/year. Rate trends were evaluated by Joinpoint analysis* and by the Annual Percent of Change (APC), using the weighted least squares method embedded in the U.S. National Cancer Institute’s SEER*Stat software that is publicly accessible.‡
The Annual Percent of Change (APC) represents the average percent increase or decrease in cancer rates per year over a specified period of time. In describing the change, the terms “increase” or “decrease” were used when the APC was significantly different from zero (two-tailed p values <0.05); otherwise the term “stable or flat” was used.
The cumulative observed survival was estimated using the Kaplan-Meier method.* Survival time was calculated from the date of first diagnosis to the event of death from any cause. Follow-up was conducted until December 31, 2006.The following censorship criteria were established: a) loss during follow-up, and b) all those who remained alive at the end of the study period. The estimates are presented in tables that were stratified according to age, sex, socioeconomic strata and period of diagnosis. The log-rank test was used to compare survival proportions between groups.
Relative survival was calculated as the ratio of observed to expected survival which was calculated by the Ederer II method using life tables for the general population of Cali. Statistical analysis was performed with Hakulinen approach embedded in the SEER*Stat software.§ Differences in 5-year relative survival by sex were modeled using a multiple regression method based on Cox’s model that adopted Poisson’s assumptions for the observed number of deaths. The Hazard Ratios (HR) for death derived from these models quantify the degree to which the risk of death in each given group would differ from the reference category after considering the baseline risk of death in the general population. A probability value of <0.05 (two-tailed) was considered statistically significant. Data management and statistical analyses were performed using STATA.§
Results
There were 9 804 new BC cases from 1962 to 2007. Breast cancer was the most common cancer among women in Cali. It accounted for 12% of all diagnosed cancers between 1962-66 and nearly a quarter (23.7%) of all cancers diagnosed for the last study period (2003-2007).The number of women diagnosed with BC in Cali increased from 250 for the first five-year period to 2 691 during the last.
The age distribution of women with BC in Cali has changed over the last 50 years. In 1962, the mean age at diagnosis (MAD) was 51.6 +/− 1.51 years. The MAD increased steadily through the period of observation (APC=0.17 EE) and for 2007 the MAD was 57.2 +/− 0.55 year’s. From 1962 to 1966 almost half of BC cases (45.2%) were in women under 50 years of age and only 17.8% were older than 70. Currently (2003-2007), 33.3% of new BC cases occurred in women younger than 50 and 30.1% occurred in women aged 70 and over.
Breast cancer incidence rates:
Evidence of a significant increase in breast cancer risk for women in Cali from 1962 to 2007 was found. The ASIR(w) per 100 000 women/year for BC in Cali increased from 27.1 in 1962-1966 to 48.0 in 2003-2007, APC=1.7 [95%CI:1.4-2.0] (figure 1A). This increase was observed in all age groups and was more accentuated in women over 70 years of age, APC=1.9 [95%CI:1.4-2.4] (table I).
Figure 1A.
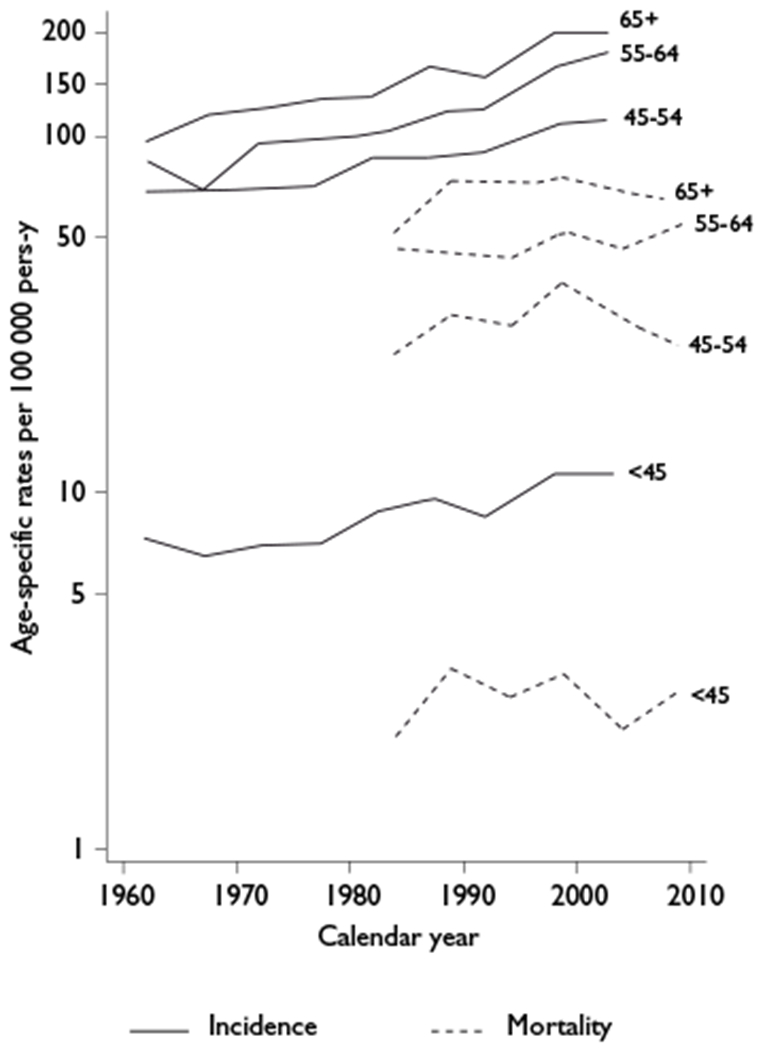
Trends for age-specific breast cancer incidence rates from 1962 to 2007 and mortality rates through 1984-2011. Cali, Colombia.
Table I.
Trends in incidence rates and mortality rates for invasive breast cancer in women, from 1962 to 2012 Cali, Colombia
| Data | Period | Age-specific incidence rates | Incidence rates | |||||
|---|---|---|---|---|---|---|---|---|
| <50 | 50-69 | 70+ | n | Crude | ASR | |||
| Incidence | 1962-1966 | 11.4 | 86.1 | 94.5 | 257 | 15.7 | 27.1 | |
| 1967-1971 | 11.0 | 83.7 | 98.1 | 325 | 16.0 | 27.3 | ||
| 1972-1976 | 11.3 | 95.6 | 117.4 | 492 | 20.1 | 33.2 | ||
| 1977-1981 | 11.4 | 95.5 | 135.8 | 614 | 20.5 | 34.8 | ||
| 1982-1986 | 14.0 | 105.7 | 126.4 | 853 | 24.3 | 34.8 | ||
| 1987-1991 | 15.0 | 113.0 | 167.5 | 1151 | 29.4 | 38.8 | ||
| 1992-1996 | 15.0 | 109.5 | 162.3 | 1306 | 29.6 | 37.3 | ||
| 1998-2002 | 17.6 | 149.2 | 207.9 | 2139 | 44.0 | 47.5 | ||
| 2003-2007 | 18.1 | 159.4 | 202.9 | 2667 | 49.6 | 48.0 | ||
| Trends over | APC | 1.4 | 1.7 | 1.9 | 1.7 | |||
| Period | 95%CI | [1.1-1.7] | [1.4-2.1] | [1.4-2.4] | [1.4-2.0] | |||
| Data | Period | Age-specific mortality rates | Mortality rates | |||||
| <50 | 50-69 | 70+ | n | Crude | ASR | |||
| Mortality | 1984-1988 | 3.4 | 41.1 | 65.1 | 298 | 8.30 | 11.9 | |
| 1989-1993 | 4.7 | 47.1 | 84.0 | 460 | 11.30 | 14.7 | ||
| 1994-1998 | 4.3 | 45.2 | 81.4 | 529 | 11.70 | 14.0 | ||
| 1999-2003 | 5.4 | 51.8 | 87.1 | 763 | 15.40 | 16.2 | ||
| 2004-2008 | 3.9 | 45.2 | 80.4 | 813 | 14.80 | 13.6 | ||
| 2009-2012 | 4.0 | 48.9 | 79.2 | 774 | 13.30 | 14.2 | ||
| Trends over | APC | −0.1 | 0.4 | 0.2 | 0.3 | |||
| Period | 95%CI | [−1.2-1.1] | [−0.3-1.1] | [−0.9-1.2] | [−0.3-0.9] | |||
Age-specific-rate per 100 000 per-year
Mortality data not available before 1984.
ASR: Age-standardised rate per 100 000 per year. ASR derived by the direct method using the ‘world population’
Figure 2A shows a clear increase in incidence rates for BC in all age groups during each successive period. The shape of the curves has changed over time. For the period 2003-2007 the age-specific incidence rate curve for breast carcinoma rapidly increased overall until the age of 50, where it then continued to increase at a slower rate for older women. This accelerated growth in young people with a plateau in the older age brackets suggests a cohort effect. Figure 2B and 2C show the plot of age-specific incidence rates for separate birth cohorts in Cali, Colombia over the period 1962-2007. The risk of BC within each cohort rises consistently over a lifetime. The shifting of the birth cohort curves to the left, as seen in figure 2B, implies that there are consistent incidence increases for each successive cohort.
Figure 2A.

Age-specific incidence rates of breast cancer for three time periods. Cali, Colombia.
Figure 2B.
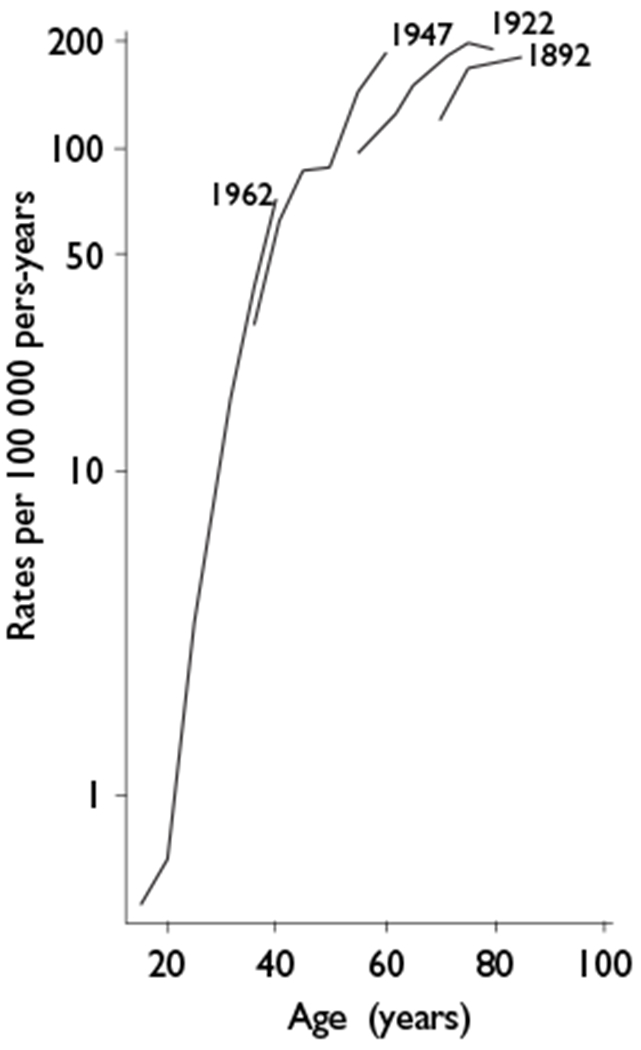
Age-specific incidence rates of breast cancer for three birth cohorts. Cali, Colombia.
Figure 2C.
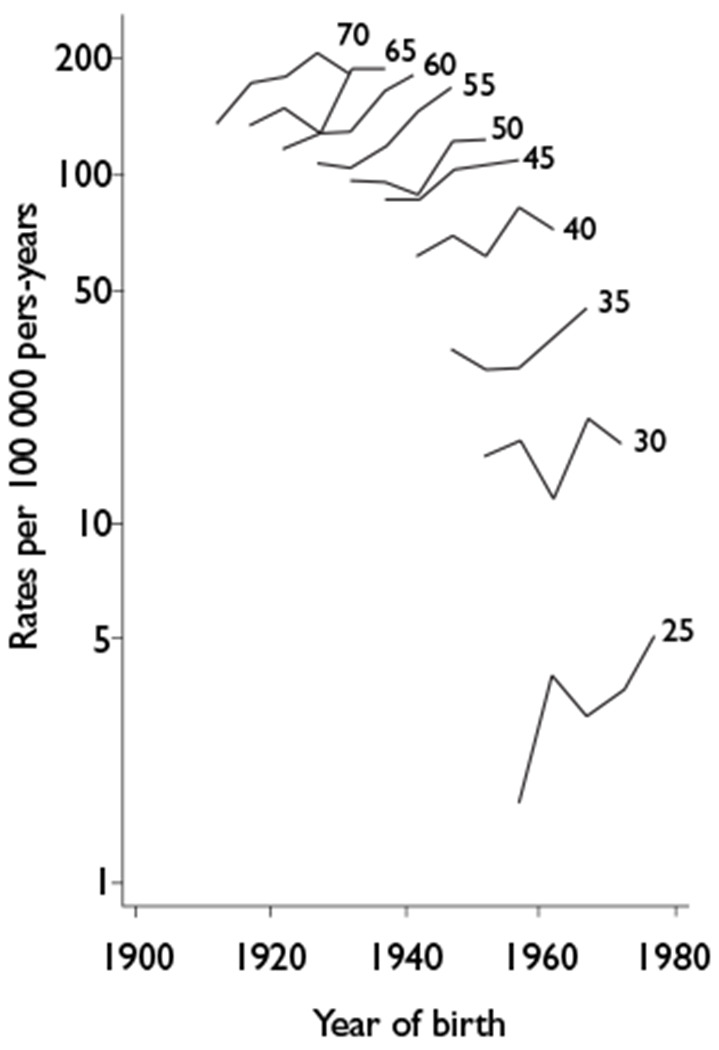
Incidence rates per 100 000 For breast cancer in Cali during 1962 through 2007 by birth cohorts and age groups. Colombia
Breast cancer mortality rates:
There were 3 445 female deaths from BC through the period of 1984 to 2012 and BC was the leading cause of cancer-related death in Cali women. Table I shows mortality data of BC for five quinquennial periods, 1984-2008, and for one quadrennial period (2009-2012). The ASMR and ASMR(w) per 100 000 females per year with BC increased until 1999-2003; however, the APC was not significantly different from zero (p<0.05): APC=0.5% (95%CI:−0.3-1.3). Since 2008, the ASMR(w) and the ASMR tended to decrease in all age groups. This change warrants follow-up over time (figure 1A). Joinpoint analysis does not show the existence of statistically significant points of change in breast cancer incidence rates (ASIR(w)/ ASIR) or mortality rates (ASMR(w)/ ASMR).
Relative survival for breast cancer:
Table II shows the relative survival estimated at 1, 3 and 5 years for women with breast cancer from 1995 to 2004, with follow-up to December 2006. The 5-year relative survival rate was 69% (95%CI:66-71) for the period of 2000-2004. The probability of dying from BC among women of the lowest SES was 1.9 times greater, when compared to higher income patients, p <0.001. A direct relationship was observed between cancer stage, age and the risk of dying from breast cancer. Women 70 and over with BC had a 58% greater risk of dying when compared with those less than 50 years of age (table III). Women with advanced BC had elevated risks of mortality compared to women with a localized disease, HR: 19.1 (SE:8.7) (table III and figure 1B). The interval-specific relative survival rate (IS-RSR) was lower than 1 throughout the five years of follow-up. The fifth year IS-RSR was 95.6% +/− 0.94%. A significant excessive mortality remains for women with BC after five years from first diagnosis.
Table 2.
Relative survival estimates at 1, 3 and 5 years for breast cancer from 1995 to 2004, with follow-up to 2006. Cali, Colombia
| Period | Characteristic |
1 year |
Survival (%),
[CI95%] 3 years |
5 years |
|||||
|---|---|---|---|---|---|---|---|---|---|
| n | Observed | Relative | Observed | Relative | Observed | Relative | |||
| 1995-1999 | |||||||||
| SES | |||||||||
| Low | 362 | 83 [78-86] | 83 [79-87] | 59 [53-64] | 61 [55-66] | 45 [39-50] | 47 [41-53] | ||
| Medium | 733 | 85 [82-88] | 86 [83-89] | 67 [64-71] | 71 [67-74] | 57 [53-60] | 62 [57-66] | ||
| High | 246 | 90 [85-93] | 91 [86-95] | 76 [70-81] | 80 [73-85] | 69 [63-75] | 76 [68-81] | ||
| Age (years) | |||||||||
| <50 | 574 | 91 [88-93] | 91 [88-93] | 68 [63-72] | 68 [64-72] | 56 [52-61] | 57 [52-62] | ||
| 50-69 | 672 | 84 [81-87] | 85 [82-88] | 71 [67-75] | 73 [69-77] | 61 [57-65] | 65 [60-69] | ||
| 70+ | 284 | 82 [76-86] | 86 [80-90] | 63 [57-69] | 74 [66-81] | 53 [46-59] | 69 [60-77] | ||
| All | 1 530 | 86 [84-88] | 88 [86-89] | 68 [66-71] | 71 [69-74] | 58 [55-60] | 62 [59-65] | ||
| 2000-2004 | |||||||||
| SES | |||||||||
| Low | 633 | 87 [84-89] | 88 [85-90] | 66 [62-69] | 68 [64-72] | 52 [48-57] | 55 [50-60] | ||
| Medium | 978 | 86 [84-88] | 88 [85-90] | 72 [69-75] | 76 [72-78] | 64 [60-67] | 69 [65-72] | ||
| High | 319 | 93 [90-96] | 95 [91-97] | 87 [82-90] | 91 [86-94] | 76 [70-81] | 83 [76-88] | ||
| Age (years) | |||||||||
| <50 | 809 | 92 [90-94] | 93 [90-94] | 77 [74-80] | 77 [74-80] | 64 [60-68] | 65 [61-69] | ||
| 50-69 | 1 052 | 88 [86-90] | 89 [87-91] | 75 [72-78] | 77 [74-80] | 68 [64-71] | 71 [67-74] | ||
| 70+ | 407 | 81 [76-84] | 84 [80-88] | 66 [61-71] | 76 [70-81] | 55 [49-60] | 70 [62-77] | ||
| All | 2 268 | 88 [87-90] | 89 [88-91] | 74 [72-76] | 77 [75-79] | 64 [62-67] | 69 [66-71] | ||
SES: Socioeconomic status
Table III.
Crude and adjusted hazard ratios* (HR) and standard error (SE) for factors associated with the risk of breast cancer death. Cali, Colombia
| Characteristic |
Crude |
Adjusted |
Test of proportional
hazards assumptions |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | SE | p | HR | SE | p | χ2 | p | ||
| Age (years) | |||||||||
| <50 | 1 | 1.00 | |||||||
| 50-69 | 0.96 | 0.06 | 0.470 | 1.11 | 0.14 | 0.402 | 0.38 | 0.54 | |
| 70+ | 1.52 | 0.11 | 0.000 | 1.58 | 0.27 | 0.008 | 0.00 | 0.98 | |
| Stage | |||||||||
| I | 1 | 1.00 | |||||||
| II | 3.31 | 1.54 | 0.010 | 3.10 | 1.45 | 0.016 | 0.83 | 0.36 | |
| III | 10.94 | 4.97 | 0.000 | 9.33 | 4.26 | 0.000 | 0.04 | 0.84 | |
| IV | 20.62 | 9.46 | 0.000 | 19.07 | 8.79 | 0.000 | 0.00 | 0.97 | |
| SES | |||||||||
| Upper | 1 | 1.00 | |||||||
| Middle | 1.60 | 0.11 | 0.000 | 1.34 | 0.27 | 0.133 | 0.15 | 0.70 | |
| Lower | 1.99 | 0.23 | 0.000 | 1.93 | 0.39 | 0.001 | 0.02 | 0.89 | |
| Period | |||||||||
| 2000-2004 | 1 | 1.00 | |||||||
| 1995-1999 | 1.24 | 0.07 | 0.000 | 1.11 | 0.11 | 0.364 | 0.71 | 0.40 | |
| Global test | 9.40 | 0.31 | |||||||
Obtained from Cox proportional hazards regression
SES: Socioeconomic status
Figure 1B.

Plots of estimated cumulative relative survival for females diagnosed with breast cancer from 1995 to 2004 and followed up to the end of 2006 by tumor stage. Cali, Colombia
5-year relative survival (%) by breast cancer stage
Discussion
During the half century under review, 9 804 cases of BC were registered in Cali. Currently, BC accounts for almost one quarter (24%) of the cancer burden for women in Cali, Colombia. Breast cancer incidence rates in Cali have increased by 1.7 percent annually over the past 45 years and more than 500 cases are now registered annually. Trend analysis showed no significant change in breast cancer mortality rates through 1984-2012. However, mortality rates appeared to decrease in all age groups after 2004 (figure 1B). The analysis showed a significant improvement (p=0.001) in the 5-year relative survival rate through 2000-2004, when compared with the 1995-1999 period. This is a first approach to BC survival in Colombia.
Between 1960 and 2010, the age index for women in Colombia changed from 7.6 to 30.8%16 and the average life expectancy at birth rose from 57 to 74 years.17 In the 1960’s, the MAD for women with BC in Cali was ten years younger than in the United States and Europe. In the early twenty-first century, the mean age at diagnosis for cancer of the breast among women in Cali was 57 years of age. The narrowing gap among countries with a MAD for BC reflects changes in the age structure of the population.
The multi-step carcinogenesis of breast cancer is a time-consuming process where the final product of cancer is more likely to occur in persons of advanced age, depending on the cumulative doses of environmental carcinogens.18,19 The exposure to known risk factors for breast cancer has changed in Cali during the last 50 years. As there is very limited information on risk factor trends for BC in Cali, we can only speculate on an explanation for the rising incidence trends in Cali suggested by our analysis. However, trend information was available on fertility rates among Colombian states, which is an aggregate measure of reproductive BC risk factors. As part of a demographic transition, the total fertility rate shows an important reduction over nearly 40 years, from an average of almost six children per woman to an average of a little over two.20 This is thought to be the result of a birth control program that included oral contraception, intra-uterine devices and surgery. The use of these methods in Colombia grew by 13% between 1990 (66%) and 2010 (79%).20 While 74.3% of Colombians live in municipalities, only 53.5% are meeting the recommendation of doing at least 150 minutes of physical activity during the week, and only 20% of Colombians follow through with the recommendations during their free time. The prevalence of excess weight shows an upward trend, increasing from 46% in 2005 to 51.2% in 2010. This condition is more prevalent in women and in the 50 to 64 year old age group.17,21
Figures 2B and 2C plot the age-specific incidence rates for separate birth cohorts in Cali. There were consistent increases in incidence for each successive cohort and these cohort effects were most noticeable for women born from 1920 to 1940 where the distance between the curves is greatest. Many of the risk factors that were previously described, especially those related to women’s reproductive history, are affecting the women in Cali due to social and environmental changes that occurred over the last fifty years. This may be affecting the incidence rates for breast cancer in a cohort-related way.
The joinpoint regression did not show change points during the rising rates of breast cancer incidence that occurred in Cali between 1962 and 2007. However, the percent change (PC) of the ASIR(w) for the periods evaluated had significant variations. The ASIR(w) of BC per 100 000 women/year increased from 33.2 to 37.3 between 1972 and 1996 (PC = 12.3%); it grew from 37.3 to 47.5 between 1996 and 2002, (PC = 27.3%). This increased incidence rate has been sustained through 2007. It coincides with the implementation of health reform,15 and the implementation of mammography screening programs in Colombia since 2000. The latter strategy has been used for the purpose of early detection of BC in asymptomatic women over 50 years of age who sought medical consultation for various reasons.
The ASMR(w) for breast cancer decreased by 12% in Cali from its peak in 1999-2003 (at 16.2 per 100 000 women) to the lower rate (i.e. 14.2 per 100 000 women) in 2009-2013. Since 2008 the ASMR(w) tended to decrease in all age groups. These changes in mortality warrant follow-up over time as it is too early to attribute them exclusively to the screening practices. The sudden increased incidence of breast cancer during 1996-2007, in the absence of a similar trend in mortality rates, may reflect improvements in surveillance and early diagnostic techniques that led to diagnoses in the earlier stages where breast cancer is more curable. Breast cancer mortality can be diminished in any population with the appropriate diagnosis and treatment programs.22
There is a currently a paucity of sufficiently long-term, high-quality time series analyses for cancer data in many developing areas. Nonetheless, where data is available, increases in breast cancer incidence and mortality rates are seen. This observation is often more apparent with recent birth cohort groups, and it is probably a consequence of the adoption of western lifestyles. Most countries in Latin America have an intermediate level incidence rate for breast cancer.23 Incidence and mortality rates have been observed as increasing in most countries. In Uruguay, Argentina and Chile, women are at high or intermediate risk, and mortality rates for younger women have been reported as more or less constant over time.23
For the period of 2000-2004, the five-year relative survival rate estimated for BC patients in Cali was 69% (95%CI:66-71). This is comparable to rates found in Costa Rica, Brazil and Eastern European countries and it is significantly lower than those described in North America, Sweden, Japan, Finland, Australia and 24 European countries in the Concord study. The level of development of health services and their efficiency in providing early diagnosis, treatment, and clinical follow-up care have a profound effect on cancer survival. The observed differences in survival between countries seem to be largely a result of differences in the availability and accessibility of early diagnosis and treatment.24,25
Chances for survival have varied by cancer stage. In a multivariate adjusted model, Cali women diagnosed with advanced BC had elevated risks of mortality compared to women with a localized disease, HR: 19.1 (SE: 8.7). Colombia lacks an organized program for BC screening and early detection based on opportunity and education of the population, as well as one for preparing public health professionals to identify the warning signs and symptoms that would allow for an early diagnosis.26 There is also evidence of an inadequate distribution in the response to the health care needs of cancer patients. The probability of dying from BC in Cali women from the lower SES group was 1.9 greater when compared to upper SES levels, p <0.001. The diagnosis and treatment of BC is more rapidly provided to women with higher educational levels, to women affiliated to private health insurance plans, to those from higher socioeconomic strata, and to those who had screening. Those with a private insurance plan affiliation were eight times more likely to have timely access to mammography screening than were users of the state-subsidized health service.27
Strengths and limitations:
This population study included all BC cases diagnosed in Cali, Colombia from 1962 to 2007. However, the RPCC was not actively tracking participants, and the city lacked reliable statistics on the migrant population. In Colombia, the identification number on the citizenship card (Cédula de ciudadanía) is not used for all medical records and passive monitoring may also be a limitation, especially in the less lethal malignant breast tumors.
Acknowledgments
Appreciation is extended to all staff at the collaborating healthcare institutions in Cali, and to the Population-based Cancer Registry of Cali. Acknowledgment is given to the National Science, Technology and Health Innovation Program (Programa Nacional de Ciencia, Tecnología e Innovatión en Salud) of the National Program for Scientific Research and Innovation (Departamento Administrativo de Ciencia, Tecnología e Innovatión – Colciencias). This work is supported in part by: Grant RC.302-2007-11-06-4082-0552, Universidad del Valle-Colciencias. Grant Prime Award No. 2 P01 CA028842-24, Subaward No.VUMC32390. National Institutes of Health/National Cancer Institute (NIH/NCI) Vanderbilt University - Universidad del Valle. Authors are grateful to GlaxoSmithKline Oncology Ethnic Research Initiative (GSK ERI) for financial and institutional support.
Footnotes
Joinpoint Regression Program. 4.0.4 ed. Bethesda, MD: Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute; May 2013.
Seer*Stat software. Version: 7.0.9 ed. Bethesda, MD: Surveillance Research Program, National Cancer Institute. National Cancer Institute; 2012
Stata/IC 12.0. College Station, TX 77845. USA: StataCorp LP; 2011.
Declaration of conflict of interests. The authors declare that they have no conflicts of interest.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010. ; 127(12):2893–2917. eng. [DOI] [PubMed] [Google Scholar]
- 2.González-Robledo MC, González-Robledo LM, Nigenda G. Formulación de políticas públicas sobre el cáncer de mama en América Latina. Rev Panam Salud Publica 2013;33(3): 183–189. [DOI] [PubMed] [Google Scholar]
- 3.Anderson BO, Cazap E, El Saghir NS, Yip CH, Khaled HM, Otero IV, et al. Optimisation of breast cancer management in low-resource and middle-resource countries: executive summaíy of the Breast Health Global Initiative consensus, 2010. Lancet Oncol 2011. ; 12(4):387–398. eng. [DOI] [PubMed] [Google Scholar]
- 4.Sharma K, Costas A, Shulman LN, Meara JG. A systematic review of barriers to breast cancer care in developing countries resulting in delayed patient presentation. J Oncol 2012. [Published online 2012 August 22]. doi: 10.1155/2012/121873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shulman LN, Willett W, Sievers A, Knaul FM. Breast cancer in developing countries: opportunities for improved survival. J Oncol 2010;2010:595167 [Published online 2010 December 29]. doi: 10.1155/2010/595167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breast Cancer Incidence in Canada Declines as Hormone Therapy Drops. J Natl Cancer Inst 2010. September eng. [Google Scholar]
- 7.Clarke CA, Glaser SL, Uratsu CS, Selby JV, Kushi LH, Herrinton LJ. Recent declines in hormone therapy utilization and breast cancer incidence: clinical and population-based evidence. J Clin Oncol 2006;24(33):e49–e50. eng. [DOI] [PubMed] [Google Scholar]
- 8.Glass AG, Lacey JV, Carreon JD, Hoover RN. Breast cancer incidence, 1980-2006: combined roles of menopausal hormone therapy, screening mammography, and estrogen receptor status. J Natl Cancer Inst [Epub 2007 Jul 24]2007;99(15):1152–1161. eng. [DOI] [PubMed] [Google Scholar]
- 9.Krieger N Hormone therapy and the rise and perhaps fall of US breast cancer incidence rates: critical reflections. Int J Epidemiol [Epub 2008 Mar 28]. 2008;37(3):627–637. doi: 10.1093/ije/dyn055. [DOI] [PubMed] [Google Scholar]
- 10.Porter PL. Global trends in breast cancer incidence and mortality. Salud Publica Mex 2009;51 Suppl 2:s141–s146. eng. [DOI] [PubMed] [Google Scholar]
- 11.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer [Epub 2008 Dec 29]2009. ;45(5):747–755. doi: 10.1016/j.ejca.2008.11.032 [DOI] [PubMed] [Google Scholar]
- 12.Bravo LE, Collazos T, Collazos P, García LS, Correa P. Trends of Cancer Incidence and Mortality in Cali, Colombia. 50 years experience. Colomb Med 2012;43(4):246–255. [PMC free article] [PubMed] [Google Scholar]
- 13.Hotes JL, Ellison LF, Howe HL, Friesen I, Kohler B. Variation in breast cancer counts using SEER and IARC multiple primary coding rules. Cancer Causes Control 2004; 15(2): 185–191. eng. [DOI] [PubMed] [Google Scholar]
- 14.Fritz A, Ries L. SEER Program Code Manual. 3rd edition, ed. Bethesda: National Cancer Institute, 1998. [Google Scholar]
- 15.Rosa RM, Alberto IC. Universal health care for Colombians 10 years after Law 100: challenges and opportunities. Health Policy 2004;68(2):129–142. eng. [DOI] [PubMed] [Google Scholar]
- 16.Departamento Administrativo Nacional de Estadística Estimaciones y proyecciones de población periodo 1985-2020. Bogotá: Departamento Administrativo Nacional de Estadística, 2010. [Google Scholar]
- 17.Instituto Colombiano de Bienestar Familiar. Encuesta Nacional de la Situación Nutricional en Colombia 2010. ENSIN. Bogotá: Da Vinci, 2011. [Google Scholar]
- 18.Peto R, Roe FJ, Lee PN, Levy L, Clack J. Cancer and ageing in mice and men. Br J Cancer 1975;32(4):411–426. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anisimov VN. The relationship between aging and carcinogenesis: a critical appraisal. Crit Rev Oncol Hematol 2003;45(3):277–304. eng. [DOI] [PubMed] [Google Scholar]
- 20.Mesa-Salamanca CA, Junca-Rodríguez GA. Análisis de reducción de la fecundidad en Colombia. Modelo de determinantes próximos. Cuadernos de Economía 2011;30(54):127–150. [Google Scholar]
- 21.Instituto Colombiano de Bienestar Familiar. Encuesta Nacional de la Situación Nutricional en Colombia 2005 ENSIN. Bogotá: Panamericana Formas e Impresos, 2006. [Google Scholar]
- 22.Botha JL, Bray F, Sankila R, Parkin DM. Breast cancer incidence and mortality trends in 16 European countries. Eur J Cancer 2003;39(12):1718–1729. eng. [DOI] [PubMed] [Google Scholar]
- 23.Bray F, McCarron P, Parkin DM. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res [Published online 2004 August 26] 2004;6(6):229–239. doi: 10.1186/bcr932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman MP, Quaresma M, Berrino F, Lutz JM, De Angelis R, Capocaccia R, et al. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Onco. [Epub 2008 Jul 17]2008;9(8):730–56. doi: 10.1016/S1470-2045(08)70179-7 [DOI] [PubMed] [Google Scholar]
- 25.Sankaranarayanan R, Swaminathan R, Brenner H, Chen K, Chia KS, Chen JG, et al. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol [Epub 2009 Dec 10] 2010;11(2):165–73. doi: 10.1016/S1470-2045(09)70335-3 [DOI] [PubMed] [Google Scholar]
- 26.Anderson BO, Yip CH, Ramsey SD, Bengoa R, Braun S, Fitch M, et al. Breast cancer in limited-resource countries: health care systems and public policy. Breast J 2006; 12 Suppl 1:S54–S69. eng. [DOI] [PubMed] [Google Scholar]
- 27.Charry LC, Carrasquilla G, Roca S. [Equity regarding early breast cancer screening according to health insurance status in Colombia]. Rev Salud Publica (Bogota) 2008; 10(4):571–82. spa. [DOI] [PubMed] [Google Scholar]


