Abstract
Background: Malnutrition is associated with poor outcomes in patients with cancer, heart failure and chronic kidney disease. This study aimed to investigate the predictive value of the Controlling Nutritional Status (CONUT) score in coronary artery disease (CAD) patients. Methods: We recruited a cohort of 3118 patients with CAD undergoing percutaneous coronary intervention (PCI) from 2005 to 2015. Nutritional status was evaluated using the CONUT score, with higher scores reflecting worse nutritional status. Results: After adjustment for comorbidities and medication, an increased CONUT score was independently associated with a higher risk of acute myocardial infarction (AMI) (HR: 1.13; 95% CI: 1.03–1.24), cardiovascular (CV) death (HR: 1.18; 95% CI: 1.07–1.30), congestive heart failure (CHF) (HR: 1.11; 95% CI: 1.04–1.18), a major adverse cardiovascular event (MACE) (HR: 1.14; 95% CI: 1.07–1.22), and total CV events (HR: 1.11; 95% CI: 1.07–1.15). The subgroup analyses demonstrated that the association of the CONUT score existed independently of other established cardiovascular risk factors. In addition, CONUT significantly improved risk stratification for myocardial infarction (MI), cardiac death, CHF, MACEs and total CV events compared to conventional risk factors in CAD patients by the significant increase in the C-index (p < 0.05) and reclassification risk categories in cardiac death and MACEs. Conclusions: The CONUT score improved the risk prediction of adverse events compared to traditional risk factors in CAD patients after percutaneous coronary intervention (PCI).
Keywords: coronary artery disease, percutaneous coronary intervention, nutrition, risk stratification, Controlling Nutritional Status (CONUT) score
1. Introduction
Cardiovascular disease remains one of the leading causes of death worldwide despite improvements in evidence-based management [1,2]. Cardiovascular disease not only impairs quality of life but also imposes a heavy economic burden in many countries [3]. Apart from conventional risk factor modification, a multidisciplinary approach is necessary to achieve improved clinical outcomes and cost-effectiveness.
Malnutrition is known to be associated with worse clinical outcomes in patients with heart failure, ischemic stroke, cancer and chronic kidney disease [3,4,5,6,7]. Albumin, body weight, body mass index, cholesterol, etc. are commonly used indices to determine nutritional status but are often inaccurate. Various tools have been developed to evaluate nutritional status including the Geriatric Nutritional Risk Index (GNRI), Prognostic Nutritional Index (PNI), Controlling Nutritional Status (CONUT) score and Mini Nutritional Assessment (MNA). These nutritional assessment tools showed prognostic value in patients with malignancy, heart failure, peripheral arterial disease and coronary artery disease [8,9,10,11]. Various studies have shown PNI to be a promising means of risk stratification for stable coronary artery disease (CAD) and acute ST-elevation myocardial infarction (STEMI) patients [11,12]. However, research was lacking in the utility of the CONUT score for the purposes of assessing clinical outcomes in CAD patients. Therefore, we aim to evaluate the prognostic value of the CONUT score in patients with coronary artery disease undergoing percutaneous coronary intervention (PCI).
2. Materials and Methods
2.1. Study Population
A total of 3118 patients with symptomatic CAD who received coronary intervention at the Taipei Veterans General Hospital between 2005 and 2015 were enrolled in this study. CAD was diagnosed by at least one of the following modalities: (1) a history of myocardial infarction as evidenced by ischemic change in a 12-lead electrocardiography (ECG) and elevated cardiac enzymes; or (2) a history of angina with ischemic ECG changes, a positive response to a stress test, or the presence of a significant stenotic lesion on a coronary computed tomography angiography (CCTA). CAD patients who fulfilled the above criteria and received a coronary intervention (percutaneous coronary intervention (PCI)) with either coronary stenting or balloon angioplasty were enrolled. This work was a retrospective observational study that complied with the Declaration of Helsinki and was approved by the appropriate Health Authorities, Independent Ethics Committees, and Independent Review Boards in Taipei Veterans General Hospital (2016-03-014CC).
2.2. Baseline Characteristics and Biochemical Data
Baseline characteristics and risk factors, including a history of hypertension, diabetes and smoking, as well as medication history, were collected. In addition, biochemical profiles including albumin, blood profiles, lipid profiles, renal function parameters and parameters related to coronary intervention were collected.
2.3. Nutrition Status Evaluation
Nutritional status was evaluated using the CONUT score, which takes into account serum values of albumin (g/dL), total cholesterol level (mg/dl), and total lymphocyte count (/mL), with a score ranging from 0 to 12 [6,13]. Higher scores reflect a worse nutritional status and have been used for nutrition status evaluation [13]. Subjects were classified as normal (0–1) or mildly (2–4), moderately (5–8) or severely (9–12) malnourished based on the CONUT score. A similar classification of nutritional status has been reported in other studies [6,7].
2.4. Clinical Follow-Up for Future Adverse Cardiovascular Events
The study patients resumed outpatient clinic visits within two to four weeks of discharge. After their first return visit, they were regularly followed up at one- to three-month intervals. Data for follow-up were retrospectively obtained from hospital records and chart reviews. The primary endpoint was major cardiovascular events including cardiovascular death, non-fatal myocardial infarction, non-fatal stroke and revascularization procedures including coronary intervention and bypass surgery. Myocardial infarction was confirmed in patients presenting with ischemic symptoms with elevated serum cardiac enzyme levels and/or characteristic ECG changes. Coronary revascularization procedures with either coronary intervention or coronary artery bypass grafting surgery were confirmed by medical record review. Stroke was confirmed if there was a new neurologic deficit lasting for at least 24 h with definite imaging evidence of cerebrovascular accident by either MRI or CT scan. Major adverse cardiovascular events (MACEs) included cardiac death, non-fatal myocardial infarction (MI) and ischemic stroke. The protocol for cardiovascular (CV) event follow-up was similar to that previously reported [14,15].
2.5. Statistical Analyses
The baseline characteristics of patients according to baseline CONUT score categories were compared. The occurrence of future adverse outcomes including non-fatal stroke, non-fatal myocardial infarction, repeat revascularization, and total CV events during the follow-up period was compared between groups. Quantitative variables were expressed as the mean and standard deviation in the presence of a normal distribution, or as the median and interquartile range in the presence of an asymmetric distribution. Qualitative variables were presented as both absolute frequencies (number of patients) and relative frequencies (percentage). Comparisons of continuous variables between groups were performed by an ANOVA test, while subgroup comparisons of categorical variables were assessed by a χ2 or Fisher’s exact test. The primary and secondary outcomes were described as overall percentages and expressed as means of proportions with a 95% confidence interval (CI). The event-free survival rate was calculated using the Kaplan–Meier method, with the significance evaluation using log rank tests. The primary analysis used an unstratified log-rank test to compare the overall survival between variable CONUT groups. Multiple regression analysis was carried out using Cox proportional hazard regression analysis adjusted for age, gender, BMI, history of hypertension, diabetes, medications including statins, LDL and HDL to evaluate whether the CONUT score was an independent factor in determining the occurrence of acute myocardial infarction, congestive heart failure (CHF), CV death, major cardiovascular events, and total CV events. Subsequent subgroup analysis was performed to investigate the effects of the CONUT score among other risk factors for cardiovascular events, such as age, gender, history of diabetes mellitus, hypertension, LDL and HDL. To assess whether the accuracy of predicting adverse cardiac events would improve after the addition of CONUT to a baseline model with established risk factors (i.e., age, gender, hypertension, diabetes, BMI and medications), the C-index, net reclassification improvement (NRI), and integrated discrimination improvement (IDI) were calculated. A similar analysis has been used in our previous work [16]. Statistical analysis was performed utilizing the SPSS software (Version 15.0, IBM Corporation, Armonk, NY, USA) and R version 3.2.3 (http://www.R-project.org/; R Foundation for Statistical Computing, Vienna, Austria). In all of the tests, the two-tailed alpha significance level was 0.05.
3. Results
3.1. Baseline Characteristics
A total of 3118 patients who underwent percutaneous coronary intervention were enrolled in this study. The baseline characteristics of the participants according to CONUT score categories are shown in Table 1. The mean age of our patients was 71.5 ± 12.1 years, of whom 81.5% were male, and the mean CONUT score was 2.6. Patients with higher CONUT score were older, had lower body weights, lower BMIs, lower LDL-C values and worse renal function (p for trend < 0.05). In addition, patients with worse nutrition had more underlying comorbidities including congestive heart failure, chronic kidney disease and more extensive coronary artery disease.
Table 1.
Baseline characteristics of patients in different categorical groups of nutritional status.
| Baseline Characteristics | Overall (n = 3118) | Nutritional Status as Classified by CONUT | ||||
|---|---|---|---|---|---|---|
| Normal (n = 1181) | Mild (n = 1366) | Moderate (n = 505) | Severe (n = 66) | p Value | ||
| Age, years | 71.50 ± 12.12 | 68.17 ± 12.67 | 73.01 ± 11.31 | 74.71 ± 11.49 | 75.11 ± 8.83 | <0.001 |
| Male, n (%) | 2542 (81.5) | 947 (80.2) | 1153 (84.4) | 390 (77.2) | 52 (78.8) | 0.001 |
| SBP, mm Hg | 128.47 ± 19.54 | 128.75 ± 19.09 | 128.98 ± 19.43 | 126.54 ± 20.72 | 127.45 ± 20.46 | 0.117 |
| DBP, mm Hg | 70.52 ± 11.43 | 72.37 ± 11.32 | 70.06 ± 11.29 | 67.90 ± 11.30 | 66.57 ± 11.79 | <0.001 |
| Height, cm | 163.66 ± 8.13 | 164.30 ± 8.36 | 163.81 ± 7.76 | 162.53 ± 8.22 | 161.44 ± 9.51 | 0.001 |
| Weight, kg | 66.69 ± 12.07 | 70.35 ± 12.10 | 66.27 ± 11.39 | 62.34 ± 11.29 | 59.14 ± 13.01 | <0.001 |
| BMI, kg/m2 | 24.78 ± 3.68 | 25.94 ± 3.57 | 24.57 ± 3.44 | 23.53 ± 3.76 | 22.56 ± 3.86 | <0.001 |
| Smoking, n (%) | 1272 (40.8) | 473 (40.1) | 551 (40.3) | 217 (43) | 31 (47) | 0.490 |
| Medical history | ||||||
| Acute coronary syndrome, n (%) | 1323 (42.4) | 408 (34.5) | 559 (40.9) | 305 (60.4) | 51 (71.33) | <0.001 |
| Hypertension, n (%) | 1980 (63.5) | 768 (65) | 908 (66.5) | 273 (54.1) | 31 (47) | <0.001 |
| Diabetes mellitus, n (%) | 1133 (36.3) | 440 (37.3) | 497 (36.4) | 171 (33.9) | 25 (37.9) | 0.607 |
| Dyslipidemia, n (%) | 375 (12) | 105 (8.9) | 178 (13) | 87 (17.2) | 5 (7.6) | <0.001 |
| Chronic kidney disease, n (%) | 264 (8.5) | 41 (3.5) | 115 (8.4) | 89 (17.6) | 19 (28.8) | <0.001 |
| Congestive heart failure, n (%) | 549 (17.6) | 148 (12.5) | 251 (18.4) | 136 (26.9) | 14 (21.2) | <0.001 |
| Stroke, n (%) | 233 (7.5) | 73 (6.2) | 116 (8.5) | 38 (7.5) | 6 (9.1) | 0.161 |
| Peripheral artery disease, n (%) | 212 (6.8) | 60 (5.1) | 102 (7.5) | 45 (8.9) | 5 (7.6) | 0.018 |
| Malignancy, n (%) | 130 (4.2) | 42 (3.6) | 56 (4.1) | 27 (5.3) | 5 (7.6) | 0.187 |
| Medication | ||||||
| Aspirin, n (%) | 2287 (73.3) | 883 (74.8) | 1012 (74.1) | 356 (70.5) | 36 (54.5) | 0.001 |
| P2Y12 inhibitor, n (%) | 795 (25.5) | 295 (25) | 341 (25) | 131 (25.9) | 28 (42.4) | 0.001 |
| ACE inhibitors, n (%) | 586 (18.8) | 212 (18) | 269 (19.7) | 96 (19) | 9 (13.6) | 0.487 |
| ARBs, n (%) | 1146 (36.8) | 445 (37.7) | 521 (38.1) | 163 (32.3) | 17 (25.8) | 0.025 |
| Beta blockers, n (%) | 1368 (43.9) | 525 (44.5) | 607 (44.4) | 212 (42) | 24 (36.4) | 0.460 |
| Calcium channel blockers, n (%) | 1045 (33.5) | 408 (34.5) | 475 (34.8) | 150 (29.7) | 12 (18.2) | 0.008 |
| Statins, n (%) | 1580 (50.7) | 649 (55) | 678 (49.6) | 232 (45.9) | 21 (31.8) | <0.001 |
| Lab | ||||||
| Creatinine, mg/dl | 1.80 ± 1.96 | 1.38 ± 1.32 | 1.89 ± 2.03 | 2.41 ± 2.60 | 2.71 ± 2.72 | <0.001 |
| eGFR, ml/min/1.73 m2 | 57.32 ± 27.03 | 64.63 ± 24.73 | 55.38 ± 26.58 | 47.19 ± 28.38 | 43.95 ± 28.46 | <0.001 |
| Glucose, mg/dL | 122.49 ± 43.90 | 122.79 ± 42.97 | 120.94 ± 42.28 | 127.09 ± 51.67 | 117.93 ± 33.71 | 0.138 |
| HbA1c, % | 7.05 ± 1.39 | 7.12 ± 1.42 | 6.96 ± 1.35 | 7.09 ± 1.41 | 7.02 ± 1.29 | 0.122 |
| Uric acid, mg/dl | 6.55 ± 2.01 | 6.48 ± 1.79 | 6.57 ± 2.02 | 6.69 ± 2.37 | 6.36 ± 2.54 | 0.208 |
| Total bilirubin, mg/dl | 0.72 ± 0.63 | 0.72 ± 0.67 | 0.72 ± 0.61 | 0.70 ± 0.60 | 0.71 ± 0.56 | 0.960 |
| Cholesterol, mg/dl | 170.11 ± 40.64 | 191.97 ± 34.32 | 161.98 ± 37.62 | 146.45 ± 37.68 | 128.33 ± 29.93 | <0.001 |
| Triglyceride, mg/dl | 132.32 ± 86.16 | 159.27 ± 98.53 | 121.21 ± 76.40 | 103.82 ± 62.65 | 95.35 ± 54.98 | <0.001 |
| HDL-C, mg/dl | 42.49 ± 12.25 | 43.39 ± 11.83 | 42.99 ± 12.59 | 39.56 ± 11.77 | 37.32 ± 11.83 | <0.001 |
| LDL-C, mg/dl | 105.05 ± 33.97 | 119.66 ± 32.33 | 99.53 ± 31.80 | 88.78 ± 29.69 | 76.03 ± 29.49 | <0.001 |
| Chol/HDL Ratio | 4.28 ± 1.50 | 4.72 ± 1.49 | 4.02 ± 1.36 | 3.99 ± 1.65 | 3.70 ± 1.34 | <0.001 |
| Non-HDL, mg/dl | 127.80 ± 39.94 | 148.54 ± 35.16 | 118.88 ± 36.79 | 107.16 ± 37.02 | 89.58 ± 28.52 | <0.001 |
| Stent | ||||||
| Stent number, n | 1.83 ± 1.06 | 1.78 ± 1.03 | 1.82 ± 1.03 | 1.97 ± 1.12 | 2.07 ± 1.45 | 0.005 |
| Stent diameter, mm | 3.08 ± 0.44 | 3.09 ± 0.43 | 3.08 ± 0.47 | 3.04 ± 0.42 | 3.13 ± 0.47 | 0.232 |
| Total stent length, mm | 23.36 ± 6.33 | 23.36 ± 5.99 | 23.17 ± 6.66 | 23.88 ± 6.36 | 23.48 ± 5.08 | 0.275 |
| Number of culprit vessel | ||||||
| SVD, n (%) | 791 (25.4) | 361 (30.6) | 333 (24.4) | 84 (16.6) | 13 (19.7) | |
| DVD, n (%) | 995 (31.9) | 386 (32.7) | 435 (318) | 159 (31.5) | 15 (22.7) | <0.001 |
| TVD, n (%) | 1329 (42.6) | 433 (36.7) | 596 (43.6) | 262 (51.9) | 38 (57.6) | |
SBP, systolic blood pressure; DBP, diastolic blood pressure; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker; CONUT, Controlling Nutritional Status; DPP-4, dipeptidyl peptidase-4; eGFR, estimated glomerular filtration rate; HbA1C, hemoglobin A1c; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; WBC, white blood cells; DES, drug-eluting stent; BMS, bare metal stent; SVD, single vessel disease; DVD, double vessel disease; TVD, triple vessel disease.
3.2. Association of Nutritional Status and Clinical Outcomes of Patients After Percutaneous Coronary Intervention
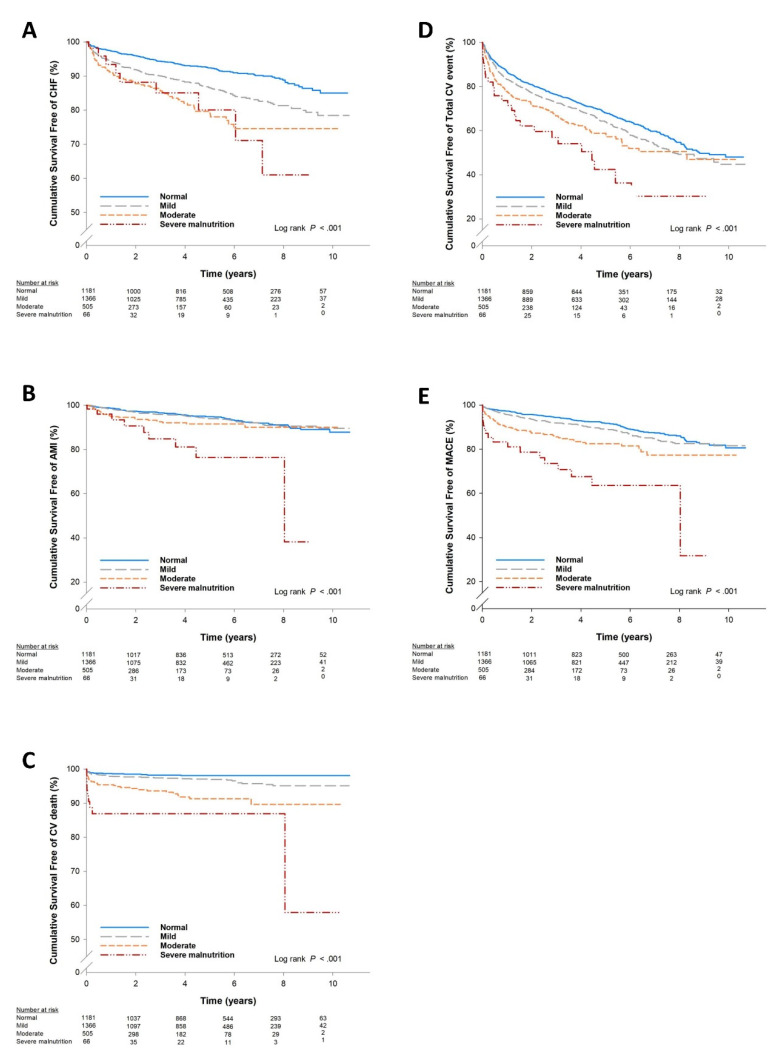
Table 2 shows the clinical outcomes according to baseline CONUT score categories. During a follow-up of 58.5 ± 35.8 months in the entire cohort, there were 197 acute myocardial infarctions (6.3%), 109 cardiac deaths (3.5%), 366 congestive heart failures (11.7%), 583 revascularizations (18.7%), 370 MACEs (11.9%) and 1098 total CV events (35.2%). Poor nutrition with increased baseline CONUT categories was correlated with a higher incidence of acute myocardial infarction, cardiac death, congestive heart failure, revascularization, MACEs and total CV events (Table 2). Figure 1 shows the relationship between baseline CONUT categories and the future risk of an event according to Kaplan–Meier survival analysis. The Kaplan–Meier analysis showed that patients with a high CONUT score were significantly associated with higher rates of major events including MACEs (log-rank p < 0.001), AMI (log-rank p < 0.001), cardiovascular death (log-rank p < 0.001), CHF (log-rank p < 0.001) and total CV events (log-rank p < 0.001). This suggests that a higher CONUT category (poor nutrition status) was associated with an increased risk of future adverse events in CAD patients after coronary intervention.
Table 2.
Clinical outcomes of patients with different nutritional status after percutaneous coronary intervention.
| Overall (n = 3118) | Nutritional Status as Classified by CONUT | |||||
|---|---|---|---|---|---|---|
| Normal (n = 1181) | Mild (n = 1366) | Moderate (n = 505) | Severe (n = 66) | p Value | ||
| Acute myocardial infarction | 197 (6.3) | 77 (6.5) | 80 (5.9) | 31 (6.1) | 9 (13.6) | 0.087 |
| Cardiovascular death | 109 (3.5) | 21 (1.8) | 45 (3.3) | 34 (6.7) | 9 (13.6) | <0.001 |
| Congestive heart failure | 366 (11.7) | 104 (8.8) | 181 (13.3) | 72 (14.3) | 9 (13.6) | 0.001 |
| MACEs | 370 (11.9) | 126 (10.7) | 155 (11.3) | 71 (14.1) | 18 (27.3) | <0.001 |
| Total CV events | 1098 (35.2) | 414 (35.1) | 493 (36.1) | 163 (32.3) | 28 (42.4) | 0.274 |
MACEs, major adverse cardiovascular events; CV, cardiovascular.
Figure 1.
Cumulative survival free of events stratified by different nutritional categories based on Kaplan–Meier analysis: (A) congestive heart failure (CHF); (B) acute myocardial infarction (AMI); (C) cardiovascular death; (D) total cardiovascular events; (E) major adverse cardiovascular events (MACEs).
Cox regression analysis further confirmed the independent predictive role of the CONUT score in the future risk of an adverse cardiovascular event after adjustment for age, gender, BMI, lipid profile, renal function and medication (Table 3). An increasing CONUT score was independently associated with a higher risk of acute myocardial infarction (AMI) (HR: 1.13; 95% CI: 1.03–1.24; p = 0.008), CV death (HR: 1.18; 95% CI: 1.07–1.30; p = 0.001), CHF (HR: 1.11; 95% CI: 1.04–1.18; p = 0.002), MACEs (HR: 1.14; 95% CI: 1.07–1.22; p < 0.001) and total CV events (HR: 1.11; 95% CI: 1.07–1.15; p < 0.001). The trends toward increased risks of AMI, CV death, CHF, MACEs and total CV events were significant across worse CONUT categories (Table 3). Both showed that higher CONUT scores are associated with worse outcomes in patients after coronary intervention. The subgroup analyses further demonstrated that the association of CONUT score existed independently of other established cardiovascular risk factors including gender group, age, history of hypertension, diabetes, smoking status, the presence of myocardial infarction, BMI, lipid profile, baseline renal function, heart function and statin use. This indicates that the CONUT score is a useful independent marker for risk stratification in patients with CAD undergoing PCI (Supplementary Figures S1–S5).
Table 3.
Association of CONUT nutritional score and the clinical outcomes in different models.
| Crude | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Acute myocardial infarction | ||||||||
| CONUT as continuous variable | 1.14 (1.07–1.21) | <0.001 | 1.13 (1.07–1.21) | <0.001 | 1.13 (1.03–1.23) | 0.006 | 1.13 (1.03–1.24) | 0.008 |
| CONUT as categorical variable | ||||||||
| Normal | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Mild | 1.02 (0.75–1.40) | 0.896 | 0.99 (0.72–1.36) | 0.938 | 0.98 (0.60–1.59) | 0.924 | 1.02 (0.62–1.70) | 0.926 |
| Moderate | 1.61 (1.06–2.45) | 0.026 | 1.55 (1.01–2.38) | 0.044 | 1.33 (0.73–2.41) | 0.356 | 1.36 (0.73–2.56) | 0.336 |
| Severe malnutrition | 4.29 (2.14–8.57) | <0.001 | 4.14 (2.06–8.30) | <0.001 | 3.73 (1.52–9.15) | 0.004 | 3.64 (1.40–9.51) | 0.008 |
| Cardiovascular death | ||||||||
| CONUT as continuous variable | 1.30 (1.21–1.39) | <0.001 | 1.27 (1.19–1.36) | <0.001 | 1.16 (1.07–1.26) | <0.001 | 1.18 (1.07–1.30) | 0.001 |
| CONUT as categorical variable | ||||||||
| Normal | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Mild | 1.99 (1.18–3.34) | 0.009 | 1.80 (1.07–3.05) | 0.027 | 1.21 (0.67–2.19) | 0.536 | 1.10 (0.89–2.05) | 0.770 |
| Moderate | 4.94 (2.85–8.54) | <0.001 | 4.12 (2.36–7.19) | <0.001 | 2.49 (1.35–4.61) | 0.004 | 2.51 (1.29–4.90) | 0.007 |
| Severe malnutrition | 10.83 (4.95–23.69) | <0.001 | 9.18 (4.18–20.17) | <0.001 | 3.24 (1.18–8.90) | 0.022 | 3.79 (1.31–10.95) | 0.014 |
| Congestive heart failure | ||||||||
| CONUT as continuous variable | 1.16 (1.11–1.21) | <0.001 | 1.12 (1.07–1.17) | <0.001 | 1.11 (1.04–1.17) | 0.001 | 1.11 (1.04–1.18) | 0.002 |
| CONUT as categorical variable | ||||||||
| Normal | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Mild | 1.73 (1.36–2.20) | <0.001 | 1.48 (1.16–1.89) | 0.002 | 1.78 (1.24–2.54) | 0.002 | 1.74 (1.21–2.52) | 0.003 |
| Moderate | 2.69 (1.99–3.64) | <0.001 | 2.12 (1.55–2.88) | <0.001 | 2.24 (1.48–3.41) | <0.001 | 2.21 (1.42–3.45) | <0.001 |
| Severe malnutrition | 2.88 (1.46–5.70) | 0.002 | 2.38 (1.20–4.71) | 0.013 | 2.04 (0.80–5.18) | 0.136 | 2.10 (0.81–5.43) | 0.127 |
| MACE | ||||||||
| CONUT as continuous variable | 1.17 (1.12–1.22) | <0.001 | 1.16 (1.11–1.21) | <0.001 | 1.14 (1.07–1.20) | <0.001 | 1.14 (1.07–1.22) | <0.001 |
| CONUT as categorical variable | ||||||||
| Normal | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Mild | 1.20 (0.95–1.52) | 0.131 | 1.13 (0.89–1.43) | 0.320 | 1.05 (0.74–1.47) | 0.800 | 1.04 (0.72–1.48) | 0.849 |
| Moderate | 2.12 (1.58–2.85) | <0.001 | 1.96 (1.46–2.64) | <0.001 | 1.82 (1.24–2.67) | 0.002 | 1.83 (1.21–2.78) | 0.005 |
| Severe malnutrition | 4.80 (2.93–7.89) | <0.001 | 4.47 (2.72–7.35) | <0.001 | 3.14 (1.63–6.05) | 0.001 | 3.34 (1.67–6.67) | 0.001 |
| Total CV events | ||||||||
| CONUT as continuous variable | 1.09 (1.06–1.11) | <0.001 | 1.08 (1.05–1.11) | <0.001 | 1.10 (1.06–1.14) | <0.001 | 1.11 (1.07–1.15) | <0.001 |
| CONUT as categorical variable | ||||||||
| Normal | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Mild | 1.16 (1.02–1.32) | 0.028 | 1.11 (0.97–1.27) | 0.127 | 1.34 (1.10–1.62) | 0.003 | 1.36 (1.11–1.66) | 0.003 |
| Moderate | 1.46 (1.21–1.75) | <0.001 | 1.38 (1.15–1.67) | 0.001 | 1.58 (1.23–2.01) | <0.001 | 1.62 (1.24–2.10) | <0.001 |
| Severe malnutrition | 2.26 (1.54–3.31) | <0.001 | 2.17 (1.48–3.18) | <0.001 | 2.52 (1.56–4.08) | <0.001 | 2.72 (1.65–4.50) | <0.001 |
Model 1: adjusted for age and sex. Model 2: adjusted for age, sex, body mass index, diabetes, hypertension and statins. Model 3: adjusted for age, sex, body mass index, diabetes, hypertension, statins, LDL and HDL.
3.3. Additional Predictive Values after Considering CONUT in Predicting Future Risk in CAD Patients after PCI
Adding the CONUT score to a baseline model improved the prediction of cardiac death (p = 0.0062), nonfatal MI (p = 0.0483), CHF (p = 0.001), MACEs (p < 0.001) and total CV events (p = 0.0053), as shown by the significant increase in the C-index (Table 4). Reclassification through the addition of the CONUT score also showed a significant integrated discrimination improvement (IDI) of 0.0135 (p < 0.001) with a 12.29% increase in net reclassification improvement (NRI) (p = 0.0151) in cardiac death and MACEs (NRI: 0.0244, p = 0.0481; IDI: 0.0035, p = 0.039). This suggests that adding the CONUT score could provide significantly better predictive value than traditional risk factors for CAD patients after PCI, especially for cardiac death and major adverse events.
Table 4.
Improvement in discrimination performance and calibration for risk prediction of cardiovascular events in the multivariate-adjusted model after including CONUT score.
| C-index (95% CI) | p Value | NRI (95% CI) | p Value | IDI (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| AMI | ||||||
| Traditional risks (Age, Gender, HTN, DM) | 0.6029 (0.5628–0.6430) | Ref. | Ref. | Ref. | ||
| Traditional risks + CONUT | 0.6239 (0.5820–0.6658) | 0.0483 | 0.0295 (−0.0031-0.0621) | 0.0762 | 0.0005 (−0.0003–0.0014) | 0.2318 |
| CHF | ||||||
| Traditional risks (Age, Gender, HTN, DM) | 0.6735 (0.6463–0.7007) | Ref. | Ref. | Ref. | ||
| Traditional risks + CONUT | 0.6891 (0.6629–0.7152) | 0.0010 | 0.0383 (0.0108–0.0657) | 0.0064 | 0.0003 (−0.0008–0.0013) | 0.6363 |
| CV death | ||||||
| Traditional risks (Age, Gender, HTN, DM) | 0.6846 (0.6329–0.7363) | Ref. | Ref. | Ref. | ||
| Traditional risks + CONUT | 0.7275 (0.6786–0.7764) | 0.0062 | 0.1229 (0.0238–0.2219) | 0.0151 | 0.0135 (0.0057–0.0212) | 0.0007 |
| MACE | ||||||
| Traditional risks (Age, Gender, HTN, DM) | 0.5970 (0.5674–0.6267) | Ref. | Ref. | Ref. | ||
| Traditional risks + CONUT | 0.6363 (0.6064–0.6662) | 0.0001 | 0.0244 (0.0002–0.0487) | 0.0481 | 0.0035 (0.0011–0.0058) | 0.0039 |
| Total CV events | ||||||
| Traditional risks (Age, Gender, HTN, DM) | 0.5544 (0.5362–0.5725) | Ref. | Ref. | Ref. | ||
| Traditional risks + CONUT | 0.5703 (0.5522–0.5884) | 0.0053 | 0.0011 (−0.0061–0.0082) | 0.7697 | 0.0000 (−0.0001–0.0001) | 0.8487 |
NRI, net reclassification improvement; IDI, integrated discrimination improvement; AMI, acute myocardial infarction; HTN, hypertension; DM, diabetes mellitus; CHF, congestive heart failure; CV, cardiovascular; MACE, major adverse cardiovascular event.
4. Discussion
Our present study showed that patients with higher CONUT scores had an increased risk of cardiac death, nonfatal MI, congestive heart failure and major adverse cardiovascular events (MACEs), suggesting that CONUT independently represents a useful predictive value regarding the long-term outcomes of CAD patients. Subgroup analyses emphasized that the CONUT score is an independent marker for risk stratification after adjusting for other cardiovascular risk factors in high-risk CAD populations. In addition, the CONUT score significantly improved the risk stratification of cardiac death and MACEs compared to conventional risk factors in CAD patients. This indicates that the CONUT could be used as an easy and practical indicator for identifying high-risk CAD patients who will develop major events after PCI.
Nutrition status plays an important role in maintaining vital organ function in the human body [17,18]. Malnutrition is associated with worse outcomes in the elderly, critically ill patients, chronic kidney disease, heart failure and ischemic stroke [5,19,20,21]. Although nutrition status is very important, the correlation between malnutrition and cardiovascular disease has focused mainly on the CHF population. Our previous study demonstrated that a low serum albumin concentration worsens the prognosis of patients with stable CAD [22], suggesting the important role that nutrition status plays in determining the long-term outcomes in CAD patients.
The CONUT score consists of three laboratory markers: albumin, cholesterol and lymphocyte count. Albumin levels are not related solely to nutritional status. They are also related to the acute phase reaction. Albumin is a serologic marker of inflammation superimposed on malnutrition, which has inflammatory effects on the vascular endothelium and lipoprotein structure [23]. Lower albumin levels may be a marker of persistent injury to the arteries and the progression of atherosclerosis and thrombosis [24]. Cholesterol homeostasis occurs as part of innate immune response and its disruption may augment inflammatory responses, leading to atherosclerosis [23,25]. The link between elevated serum cholesterol levels and cardiovascular disease was confirmed with the discoveries of the low-density lipoprotein (LDL) receptor and statins [26]. However, the lipid paradox has been reported in several clinical studies including myocardial infarction and heart failure patients [27]. Though the cause of the lipid paradox remains undetermined, possible explanations are that these patients have a high vascular inflammation status even though their LDL is not very high. Low lipid levels may be markers of advanced disease and systemic inflammatory activation [28], and could be a reflection of malnutrition and cachexia, which are known to be associated with increased mortality in different chronic diseases [5,19,20,21]. Lower LDL levels may be associated with poor nutritional status, making patients more vulnerable to future events. Furthermore, these patients may not receive aggressive statin therapy because of their lower baseline LDL levels, and relatively low statin use may be responsible for the higher risk in the high CONUT score group. To elucidate this issue, our current study adjusted for confounding factors including statin use, LDL and HDL values, and a higher CONUT score was still independently associated with the risk of a future adverse event in CAD patients after PCI. Lymphocyte counts reflect the host immunity and have been studied with respect to their association with nutritional status [29]. Lymphocytopenia may reflect neurohormonal activation in CAD patients and may represent a marker of the physiological stress response [30,31]. A low lymphocyte percentage was shown to be independently and significantly associated with CAD and could be used as a predictor of worse prognosis [32]. These elements contribute to the pathophysiology of coronary artery disease [33]. This makes the CONUT score a reasonable tool for determining the nutritional status of the CAD population. In previous studies, the CONUT score was shown to predict outcomes in populations with acute heart failure [8], acute ischemic stroke [6], elderly hypertension [34], and cancers including mesothelioma and gastric cancer [7,35].
Recently H. Wada et al. disclosed that nutritional status as assessed by the PNI is useful in predicting long-term cardiovascular outcomes in stable CAD patients that underwent elective PCI [11]. In this study, the lowest PNI group was significantly associated with MACEs and all-cause death compared to the highest PNI group even after adjustments for other risk factors. Our study showed similar results with nutritional evaluation using the CONUT score, but our cohort included patients presenting with acute coronary syndromes. Furthermore, our study demonstrated that an increased CONUT score was independently associated with an increased future risk of AMI, CV death, CHF, MACEs and total CV events, extending the predictive value of nutrition scoring in CAD patients after PCI.
The mechanism linking poor nutrition to worse adverse outcomes is considered to be multifactorial. Malnutrition may decrease underlying fibrinolysis ability, platelet inhibition and antioxidant capacity and increase blood viscosity, leading to the occurrence of adverse outcomes. Our study is consistent with the finding of M. Yokoyama who reported the independent predictive value of CONUT score-based malnutrition status in peripheral arterial disease [36]. In addition, the subgroup analyses showed that the association of the CONUT score existed independently of other established cardiovascular risk factors, especially among these high-risk patients. This suggests that the CONUT score is an independent prognosis predictor in CAD patients. Furthermore, the addition of the CONUT score to the clinical model improved not only the predictive power for major cardiovascular events such as cardiac death and major adverse cardiac events (as assessed by the receiver operating characteristic (ROC) curves) but also the reclassification of the subjects into different risk categories via the IDI and NRI. This implies that a high CONUT score is an independent prognostic marker of future adverse events and increases the predictive value for adverse events among CAD patients.
This study has several potential limitations due to its retrospective nature and patient enrollment at a single institution. The study period is quite long, and the treatment of coronary artery disease including the statin intensity and prescription practice has changed during this period. Additionally, due to a lack of data, we could not determine the effects of the serial changes in nutritional status. However, we showed that malnutrition is common in patients with coronary artery disease, which could add as a prognostic factor for clinical outcomes in addition to the established risk factors. The use of the CONUT score, which comprises cholesterol levels, might be affected by the use of statins, which is common in patients with coronary artery disease. This issue has been adjusted for by considering statin use in the Cox regression analysis in Model 2 and Model 3 as shown in Table 3. In addition, the subgroup analysis of statin use shows an independent association of the CONUT score and future CV events in patients after PCI (as demonstrated in Supplementary Figures S1–S5). Finally, the role of nutritional support was well established in surgical patients [37]. Nutritional support was associated with fewer complications and a shorter length of stay in patients at nutritional risk [38]. However, there was lack of research regarding the impact of nutrition therapy in patients with coronary artery disease. This can be a focus of attention for future research.
5. Conclusions
This study shows that the CONUT score is an independent predictor of long-term cardiovascular disease to identify outcomes in patients with coronary artery disease, including those presenting with acute coronary syndromes. This suggests the usefulness of the CONUT score, in addition to the well-established cardiovascular risk factors, for risk stratification in these patients prior to PCI.
Acknowledgments
We thank Hsiu-Wen Liao and Yi-Hsuan Huang for their assistant in performing the study.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/12/5/1295/s1, Figure S1: Forest plot of hazard ratio for CHF, Figure S2: Forest plot of hazard ratio for AMI, Figure S3: Forest plot of hazard ratio for CV Death, Figure S4: Forest plot of hazard ratio for Total CV Event, Figure S5: Forest plot of hazard ratio for MACE.
Author Contributions
S.-C.C. and H.-B.L. conceived of the overall idea and designed the study. S.-C.C. and H.-B.L. performed the statistical analyses and S.-C.C. wrote the first draft of the manuscript. All authors revised the manuscript critically and All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
All the authors declare no conflict of interest.
References
- 1.Moran A.E., Forouzanfar M.H., Roth G.A., Mensah G.A., Ezzati M., Murray C.J., Naghavi M. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: The Global Burden of Disease 2010 study. Circulation. 2014;129:1483–1492. doi: 10.1161/CIRCULATIONAHA.113.004042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moran A.E., Forouzanfar M.H., Roth G.A., Mensah G.A., Ezzati M., Flaxman A., Murray C.J., Naghavi M. The global burden of ischemic heart disease in 1990 and 2010: The Global Burden of Disease 2010 study. Circulation. 2014;129:1493–1501. doi: 10.1161/CIRCULATIONAHA.113.004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavoie L., Khoury H., Welner S., Briere J.B. Burden and Prevention of Adverse Cardiac Events in Patients with Concomitant Chronic Heart Failure and Coronary Artery Disease: A Literature Review. Cardiovasc. Ther. 2016;34:152–160. doi: 10.1111/1755-5922.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agra Bermejo R.M., Gonzalez Ferreiro R., Varela Roman A., Gomez Otero I., Kreidieh O., Conde Sabaris P., Rodriguez-Manero M., Moure Gonzalez M., Seoane Blanco A., Virgos Lamela A., et al. Nutritional status is related to heart failure severity and hospital readmissions in acute heart failure. Int. J. Cardiol. 2017;230:108–114. doi: 10.1016/j.ijcard.2016.12.067. [DOI] [PubMed] [Google Scholar]
- 5.Almeida H.R.M., Santos E.M.C., Dourado K., Mota C., Peixoto R. Malnutrition associated with inflammation in the chronic renal patient on hemodialysis. Rev. Assoc. Med. Bras. (1992) 2018;64:837–844. doi: 10.1590/1806-9282.64.09.837. [DOI] [PubMed] [Google Scholar]
- 6.Naito H., Nezu T., Hosomi N., Aoki S., Kinoshita N., Kuga J., Shimomura R., Araki M., Ueno H., Ochi K., et al. Controlling nutritional status score for predicting 3-mo functional outcome in acute ischemic stroke. Nutrition. 2018;55–56:1–6. doi: 10.1016/j.nut.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki S., Kanaji S., Yamamoto M., Oshikiri T., Nakamura T., Kakeji Y. Controlling Nutritional Status (CONUT) Score Predicts Outcomes of Curative Resection for Gastric Cancer in the Elderly. World J. Surg. 2018 doi: 10.1007/s00268-018-04889-6. [DOI] [PubMed] [Google Scholar]
- 8.Iwakami N., Nagai T., Furukawa T.A., Sugano Y., Honda S., Okada A., Asaumi Y., Aiba T., Noguchi T., Kusano K., et al. Prognostic value of malnutrition assessed by Controlling Nutritional Status score for long-term mortality in patients with acute heart failure. Int. J. Cardiol. 2017;230:529–536. doi: 10.1016/j.ijcard.2016.12.064. [DOI] [PubMed] [Google Scholar]
- 9.Luo H., Yang H., Huang B., Yuan D., Zhu J., Zhao J. Geriatric Nutritional Risk Index (GNRI) Independently Predicts Amputation Inchronic Criticallimb Ischemia (CLI) PLoS ONE. 2016;11:e0152111. doi: 10.1371/journal.pone.0152111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sze S., Pellicori P., Kazmi S., Rigby A., Cleland J.G.F., Wong K., Clark A.L. Prevalence and Prognostic Significance of Malnutrition Using 3 Scoring Systems Among Outpatients With Heart Failure: A Comparison With Body Mass Index. JACC Heart Fail. 2018;6:476–486. doi: 10.1016/j.jchf.2018.02.018. [DOI] [PubMed] [Google Scholar]
- 11.Wada H., Dohi T., Miyauchi K., Jun S., Endo H., Doi S., Konishi H., Naito R., Tsuboi S., Ogita M., et al. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J. Cardiol. 2018;72:155–161. doi: 10.1016/j.jjcc.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Chen Q.J., Qu H.J., Li D.Z., Li X.M., Zhu J.J., Xiang Y., Li L., Ma Y.T., Yang Y.N. Prognostic nutritional index predicts clinical outcome in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Sci. Rep. 2017;7:3285. doi: 10.1038/s41598-017-03364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ignacio de Ulibarri J., Gonzalez-Madrono A., de Villar N.G., Gonzalez P., Gonzalez B., Mancha A., Rodriguez F., Fernandez G. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 2005;20:38–45. [PubMed] [Google Scholar]
- 14.Yang Y.L., Wu C.H., Hsu P.F., Chen S.C., Huang S.S., Chan W.L., Lin S.J., Chou C.Y., Chen J.W., Ju-Pin P., et al. Systemic immune-inflammation index (SII) Predicted Clinical Outcome in Patients With Coronary Artery Disease. Eur. J. Clin. Investig. 2020:e13230. doi: 10.1111/eci.13230. [DOI] [PubMed] [Google Scholar]
- 15.Lim S.S., Yang Y.L., Chen S.C., Wu C.H., Huang S.S., Chan W.L., Lin S.J., Chen J.W., Chou C.Y., Pan J.P., et al. Association of variability in uric acid and future clinical outcomes of patient with coronary artery disease undergoing percutaneous coronary intervention. Atherosclerosis. 2020;297:40–46. doi: 10.1016/j.atherosclerosis.2020.01.025. [DOI] [PubMed] [Google Scholar]
- 16.Chen S.C., Lin C.P., Hsu H.C., Shu J.H., Liang Y., Hsu P.F., Wang Y.J., Ding Y.Z., Liou T.L., Wang Y.W., et al. Serum bilirubin improves the risk predictions of cardiovascular and total death in diabetic patients. Clin. Chim. Acta. 2019;488:1–6. doi: 10.1016/j.cca.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 17.Bistrian B.R., Blackburn G.L., Vitale J., Cochran D., Naylor J. Prevalence of Malnutrition in General Medical Patients. JAMA. 1976;235:1567–1570. doi: 10.1001/jama.1976.03260410023017. [DOI] [PubMed] [Google Scholar]
- 18.Bistrian B.R., Blackburn G.L., Hallowell E., Heddle R. Protein Status of General Surgical Patients. JAMA. 1974;230:858–860. doi: 10.1001/jama.1974.03240060028025. [DOI] [PubMed] [Google Scholar]
- 19.Nishi I., Seo Y., Hamada-Harimura Y., Sato K., Sai S., Yamamoto M., Ishizu T., Sugano A., Obara K., Wu L., et al. Utility of Nutritional Screening in Predicting Short-Term Prognosis of Heart Failure Patients. Int. Heart J. 2018;59:354–360. doi: 10.1536/ihj.17-073. [DOI] [PubMed] [Google Scholar]
- 20.Stoppe C., Ney J., Lomivorotov V.V., Efremov S.M., Benstoem C., Hill A., Nesterova E., Laaf E., Goetzenich A., McDonald B., et al. Prediction of Prolonged ICU Stay in Cardiac Surgery Patients as a Useful Method to Identify Nutrition Risk in Cardiac Surgery Patients: A Post Hoc Analysis of a Prospective Observational Study. JPEN J. Parenter. Enter. Nutr. 2018 doi: 10.1002/jpen.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomes F., Emery P.W., Weekes C.E. Risk of Malnutrition Is an Independent Predictor of Mortality, Length of Hospital Stay, and Hospitalization Costs in Stroke Patients. J. Stroke Cerebrovasc. Dis. 2016;25:799–806. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Chien S.C., Chen C.Y., Leu H.B., Su C.H., Yin W.H., Tseng W.K., Wu Y.W., Lin T.H., Chang K.C., Wang J.H., et al. Association of low serum albumin concentration and adverse cardiovascular events in stable coronary heart disease. Int. J. Cardiol. 2017;241:1–5. doi: 10.1016/j.ijcard.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 23.Artigas A., Wernerman J., Arroyo V., Vincent J.L., Levy M. Role of albumin in diseases associated with severe systemic inflammation: Pathophysiologic and clinical evidence in sepsis and in decompensated cirrhosis. J. Crit. Care. 2016;33:62–70. doi: 10.1016/j.jcrc.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 24.Kuller L.H., Eichner J.E., Orchard T.J., Grandits G.A., McCallum L., Tracy R.P. The relation between serum albumin levels and risk of coronary heart disease in the Multiple Risk Factor Intervention Trial. Am. J. Epidemiol. 1991;134:1266–1277. doi: 10.1093/oxfordjournals.aje.a116030. [DOI] [PubMed] [Google Scholar]
- 25.Tall A.R., Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat. Rev. Immunol. 2015;15:104–116. doi: 10.1038/nri3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gotto A.M., Jr. Jeremiah Metzger Lecture: Cholesterol, inflammation and atherosclerotic cardiovascular disease: Is it all LDL? Trans. Am. Clin. Climatol. Assoc. 2011;122:256–289. [PMC free article] [PubMed] [Google Scholar]
- 27.Horwich T.B., Hernandez A.F., Dai D., Yancy C.W., Fonarow G.C. Cholesterol levels and in-hospital mortality in patients with acute decompensated heart failure. Am. Heart J. 2008;156:1170–1176. doi: 10.1016/j.ahj.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Rauchhaus M., Coats A.J.S., Anker S.D. The endotoxin-lipoprotein hypothesis. Lancet. 2000;356:930–933. doi: 10.1016/S0140-6736(00)02690-8. [DOI] [PubMed] [Google Scholar]
- 29.Leandro-Merhi V.A., Braz V.N., Aquino J.L. Is total lymphocyte count related to nutritional markers in hospitalized older adults? Arq. Gastroenterol. 2017;54:79–82. doi: 10.1590/s0004-2803.2017v54n1-16. [DOI] [PubMed] [Google Scholar]
- 30.Nelson D.H., Sandberg A.A., Palmer J.G., Tyler F.H. Blood levels of 17-hydroxycorticosteroids following the administration of adrenal steroids and their relation to levels of circulating leukocytes. J. Clin. Investig. 1952;31:843–849. doi: 10.1172/JCI102671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bergquist J., Tarkowski A., Ewing A., Ekman R. Catecholaminergic suppression of immunocompetent cells. Immunol. Today. 1998;19:562–567. doi: 10.1016/S0167-5699(98)01367-X. [DOI] [PubMed] [Google Scholar]
- 32.Bian C., Wu Y., Shi Y., Xu G., Wang J., Xiang M., Weng S., Jiang J., Ma J. Predictive value of the relative lymphocyte count in coronary heart disease. Heart Vessel. 2010;25:469–473. doi: 10.1007/s00380-010-0010-7. [DOI] [PubMed] [Google Scholar]
- 33.Hansson G.K. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 34.Sun X., Luo L., Zhao X., Ye P. Controlling Nutritional Status (CONUT) score as a predictor of all-cause mortality in elderly hypertensive patients: A prospective follow-up study. BMJ Open. 2017;7:e015649. doi: 10.1136/bmjopen-2016-015649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takamori S., Toyokawa G., Taguchi K., Edagawa M., Shimamatsu S., Toyozawa R., Nosaki K., Seto T., Hirai F., Yamaguchi M., et al. The Controlling Nutritional Status Score Is a Significant Independent Predictor of Poor Prognosis in Patients With Malignant Pleural Mesothelioma. Clin. Lung Cancer. 2017;18:e303–e313. doi: 10.1016/j.cllc.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 36.Yokoyama M., Watanabe T., Otaki Y., Watanabe K., Toshima T., Sugai T., Takahashi T., Kinoshita D., Tamura H., Nishiyama S., et al. Impact of Objective Malnutrition Status on the Clinical Outcomes in Patients With Peripheral Artery Disease Following Endovascular Therapy. Circ. J. 2018;82:847–856. doi: 10.1253/circj.CJ-17-0731. [DOI] [PubMed] [Google Scholar]
- 37.Stoppe C., Goetzenich A., Whitman G., Ohkuma R., Brown T., Hatzakorzian R., Kristof A., Meybohm P., Mechanick J., Evans A., et al. Role of nutrition support in adult cardiac surgery: A consensus statement from an International Multidisciplinary Expert Group on Nutrition in Cardiac Surgery. Crit. Care. 2017;21:131. doi: 10.1186/s13054-017-1690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang H., Wang Y., Jiang Z.-M., Kondrup J., Fang H., Andrews M., Nolan M.T., Mu S.-Y., Zhang J., Yu K., et al. Impact of nutrition support on clinical outcome and cost-effectiveness analysis in patients at nutritional risk: A prospective cohort study with propensity score matching. Nutrition. 2017;37:53–59. doi: 10.1016/j.nut.2016.12.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.