PRESENTATION
A 13-year-old boy without a significant medical history presents with a painful erection that has persisted for 3 days. He denies any known stimulus, trauma, or new medications. He has not had any other symptoms except for vague headaches and leg pain in the past month. He has seen 2 providers in the past 3 days, who prescribed therapies including lidocaine, oral pseudoephedrine, and antibiotics without relief. No laboratory tests were obtained at either visit.
On physical examination he is afebrile, his blood pressure is 146/76 mm Hg, and his heart rate is 117 beats/min. He appears uncomfortable from penile pain but is nontoxic. On abdominal examination, his spleen is palpable 4 cm below the costal margin, and his genitourinary examination reveals an erect penis that is erythematous, tender to palpation, and without any obvious perfusion defects. The remainder of his examination findings are normal.
Pediatric urology is urgently consulted for management of priapism, and laboratory studies are sent, which reveal the etiology of his symptoms.
DISCUSSION
A complete blood cell (CBC) count reveals a white blood cell (WBC) count of 350,000/μL (350×109/L), hemoglobin level of 8.5 g/dL (85 g/L), and platelet count of 450×103/μL (450×109/L). The differential count includes 67% neutrophils, 5% lymphocytes, 2% monocytes, 1% basophils, 13% metamyelocytes, 9% myelocytes, 1% promyelocytes, and 2% blasts (Fig 1). Levels of electrolytes, blood urea nitrogen, creatinine, liver enzymes, and uric acid are all normal. Flow cytometry of the blood shows granulocytosis with no increase in blasts. Priapism secondary to chronic myelogenous leukemia (CML) with leukostasis is diagnosed.
Figure 1.
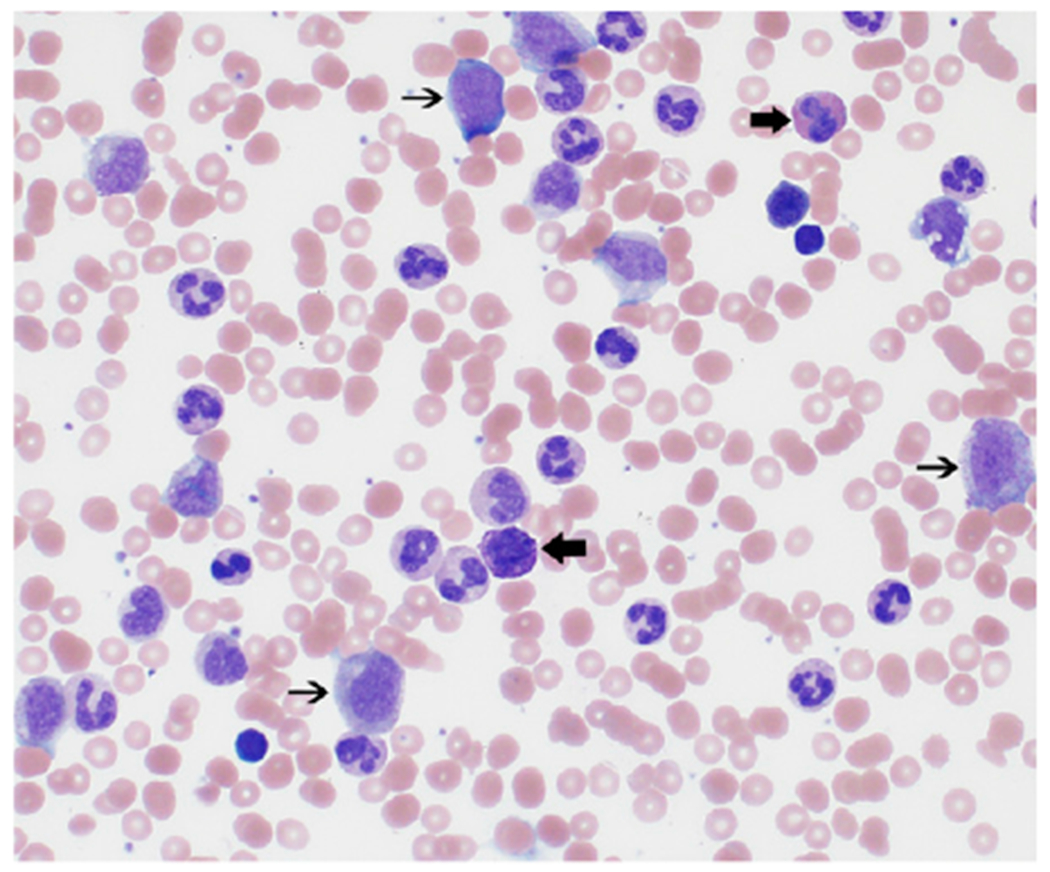
The peripheral blood smear shows a marked leukocytosis consisting predominantly of myeloid elements, including left-shifted myeloid forms (thin arrows) and scattered basophils and eosinophils (thick arrows).
Clinical Course
Urology performed a penile phenylephrine injection, without improvement. The patient was admitted to the PICU for leukapheresis and was started on fluids, hydroxyurea, and allopurinol. Leukapheresis was performed with reduction of the posthydration WBC count from 255,000/μL (255×109/L) to 222,000/μL (222×109/L). Urology then performed corporeal irrigation twice within 12 hours, both with initial detumescence and nearly immediate return of the erection. Bone marrow biopsy was performed, and cytogenetic studies revealed the Philadelphia chromosome, confirming the diagnosis of CML (Figs 2–4). He was started on imatinib, with further improvement of his leukocytosis. He underwent a third corporeal irrigation with a distal shunt procedure 36 hours after the previous irrigation. At the time of hospital discharge, his genitourinary examination was improved but still with some phallus rigidity and tenderness.
Figure 2.
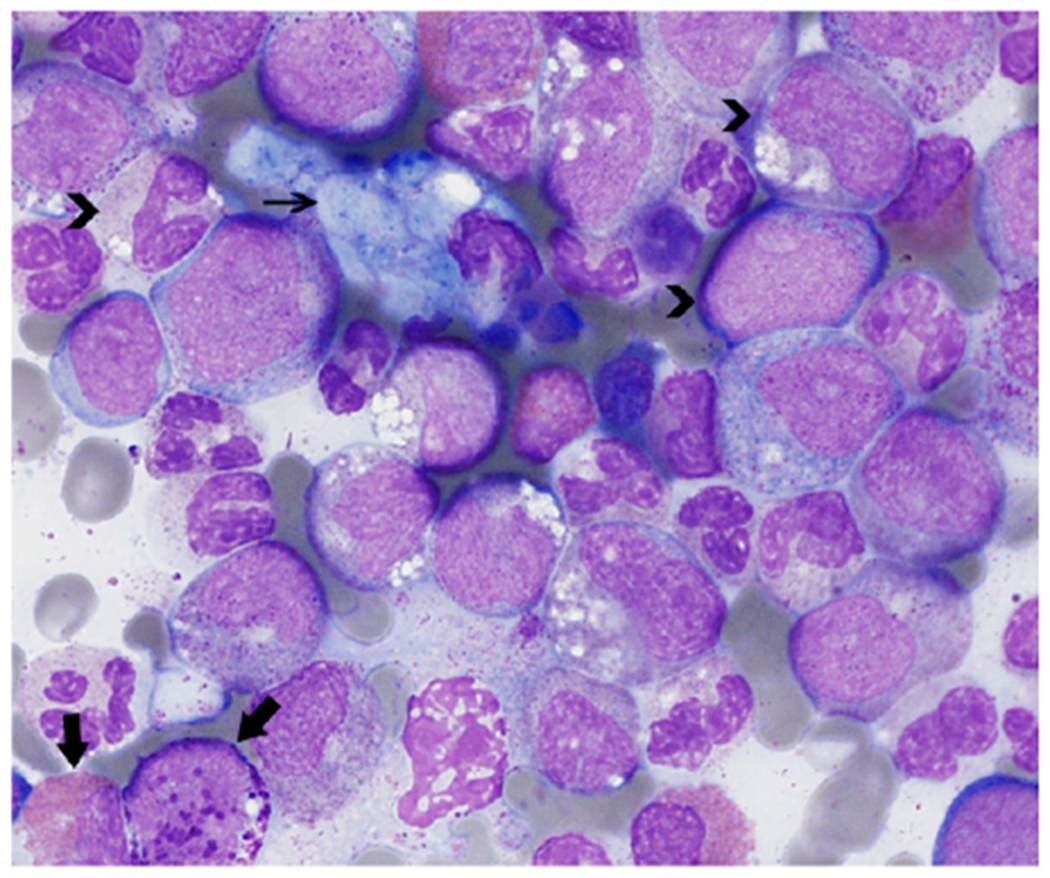
The bone marrow aspirate smear shows myeloid hyperplasia with a full range of maturation (arrowheads) as well as eosinophilia and basophilia (thick arrows) with no increase in blasts. Sea-blue histiocytes (thin arrow) are present. Megakaryocytes (not pictured) include small, hypolobated forms.
Figure 4.
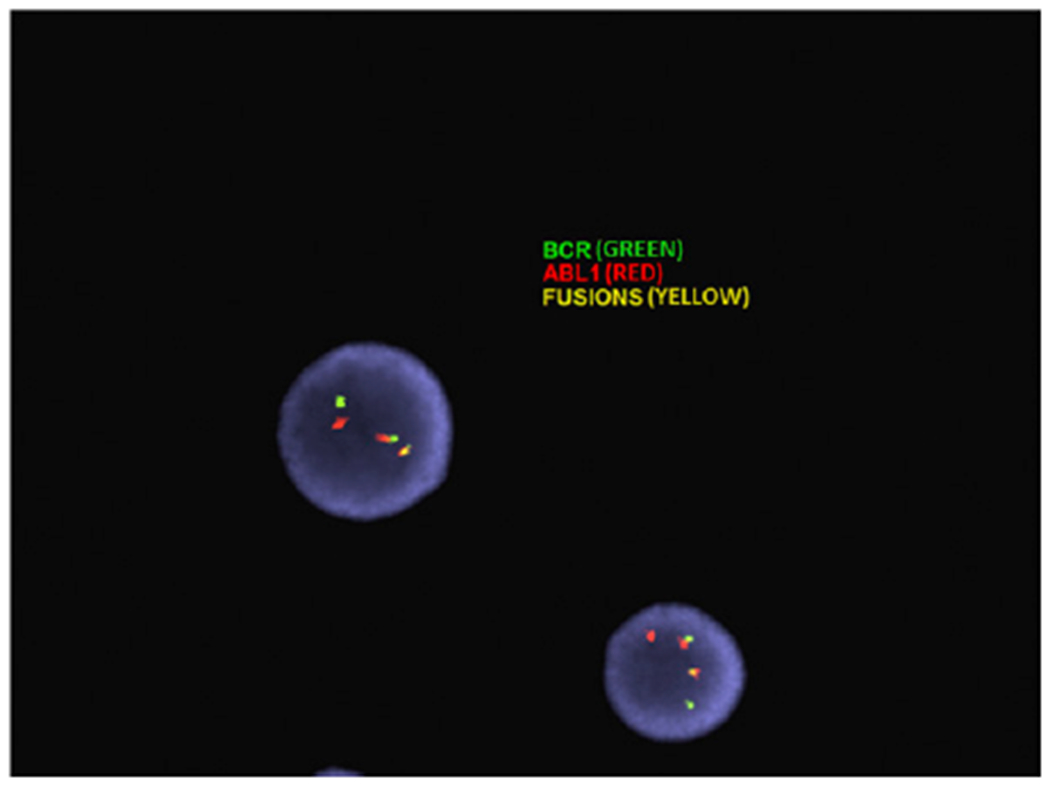
Dual-color-dual-fusion fluorescence in situ hybridization analysis confirms a BCR/ABL1 rearrangement in 95% of analyzed cells.
The Presenting Condition
Priapism is rare in children but requires urgent intervention. The most common type is ischemic priapism, classified by painful venous occlusion and subsequent tissue ischemia. Much less common is nonischemic priapism, caused by painless high arterial flow fistulization, typically secondary to trauma.
In children presenting with priapism, approximately 65% of cases are attributable to sickle cell disease, and in rare instances, sickle cell trait. Ten percent of cases are secondary to leukemia, 10% are secondary to trauma, 10% are idiopathic, and the remaining 5% are secondary to medications. Of the 10% secondary to leukemia, approximately half are CML.
Management of priapism should involve primary measures of analgesia and attempts to ease the erection with cold packs, urination, ejaculation, and/or physical exercise, along with urgent urologic consultation. Laboratory testing should include a CBC count and electrolytes to assess for common pathologies associated with priapism. When priapism is secondary to an underlying disease process, addressing the primary pathology in addition to performing the necessary urologic procedures is recommended. In patients with sickle cell disease, priapism may be treated with exchange transfusion, although evidence supporting such therapy is sparse. When hyperleukocytosis with leukostasis is present, treatment of the malignancy and/or leukapheresis can be useful in improving symptoms and preventing complications.
Timeliness of care is of utmost importance because ischemic priapism without proper treatment can lead to progressive penile necrosis and fibrosis, with the long-term complication of erectile dysfunction. The likelihood of erectile dysfunction increases with the duration of symptoms. (1)
The Underlying Condition
In children, CML is rare, making up 2% to 3% of all leukemia diagnoses. Its hallmark is the Philadelphia chromosome, an abnormal chromosome 22 that is created by the reciprocal translocation t(9;22)(q34.1;q11.2), which fuses the ABL gene on chromosome 9 to the BCR gene on chromosome 22. The BCR-ABL fusion protein leads to overproduction of granulocytes at all stages of maturation, resulting in marrow replacement. The treatment of CML has been dramatically altered by tyrosine kinase inhibitors (TKIs), which directly inhibit the BCR-ABL fusion protein. Before the use of these targeted agents, stem cell transplant was the only curative option. The optimal length of TKI therapy, the cost analysis of TKI versus stem cell transplant, and the potential consequences of long-term TKI use in children are not completely known.
Children with CML tend to present with elevated WBC counts (median, 225,000/μL [225×109/μL]) without increased blasts. Other symptoms often include fatigue, weight loss, night sweats, and abdominal pain and swelling from splenomegaly. Approximately 10% of patients present with signs of leukostasis, which may include vision changes, intraocular hemorrhages, dyspnea/respiratory distress, headache, altered mental status, hearing changes, aseptic osteonecrosis, and priapism.
Evidence is sparse on the utility of leukapheresis in CML, mainly because cases are rare, but it is generally considered for patients with severe symptoms or evidence of end organ dysfunction, including priapism. In this case, there was minimal change in WBC count and priapism after leukapheresis. (2)
Lessons for the Clinician
Priapism in a child or adolescent is a urologic emergency and should prompt immediate consultation with a pediatric urologist.
The most common cause of priapism in children is sickle cell disease, but leukemia should always be considered. Therefore, laboratory tests, including a complete blood cell count and electrolytes, are essential for a pediatric patient presenting with priapism, particularly for those without a history of sickle cell disease or trauma.
Children with leukemia can present with hyperleukocytosis and leukostasis, which are critical illnesses that require prompt intervention to prevent both acute and chronic morbidity.
Figure 3.
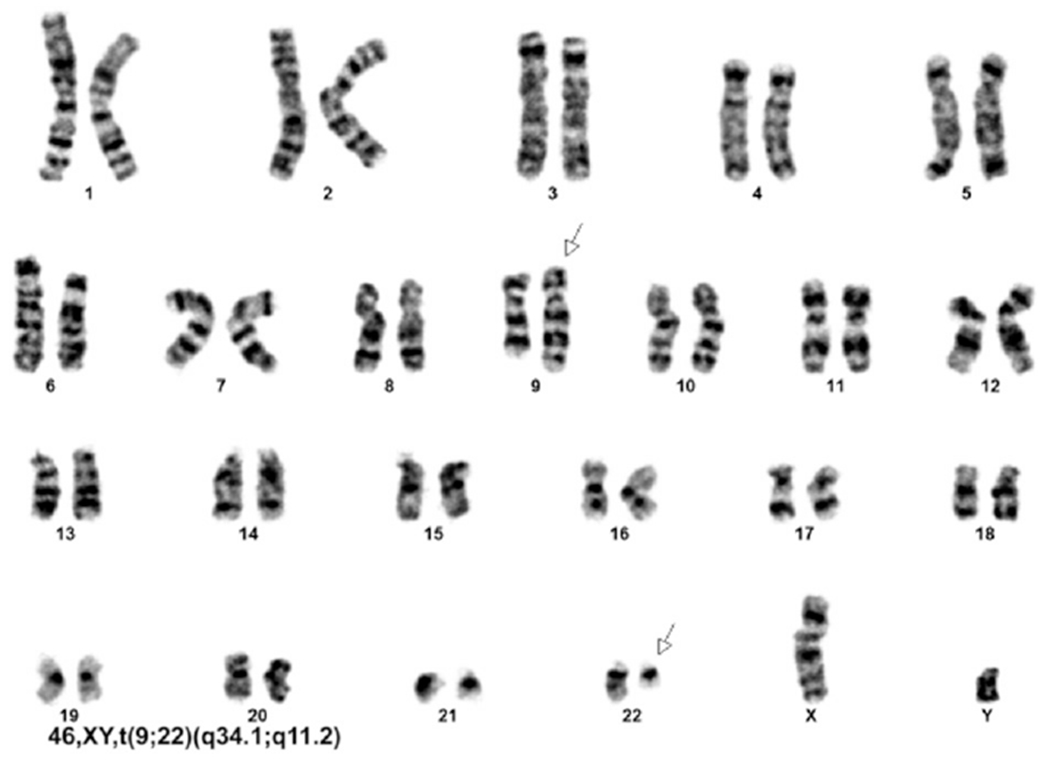
Cytogenetic analysis shows a t(9;22)(q34.1;q11.2) translocation in all 20 cells analyzed. Arrows indicate the abnormal, elongated chromosome 9 (upper arrow) and abnormal, truncated chromosome 22 (lower arrow).
Footnotes
AUTHOR DISCLOSURE Drs Clark, Hsu, Darves-Bornoz, Tanaka, Mason, and Katzenstein have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
References
- 1.Donaldson JF, Rees RW, Steinbrecher HA. Priapism in children: a comprehensive review and clinical guideline. J Pediatr Urol. 2014;10(1):11–24 [DOI] [PubMed] [Google Scholar]
- 2.Kurosawa H, Tanizawa A, Tono C, et al. Leukostasis in children and adolescents with chronic myeloid leukemia: Japanese Pediatric Leukemia/Lymphoma Study Group. Pediatr Blood Cancer. 2016; 63(3):406–411 [DOI] [PubMed] [Google Scholar]


