Abstract
Introduction: Oral cancer remains prevalent, despite being largely preventable. The widespread use of technology at chairside, combined with advances in electronic health record (EHR) capabilities, present opportunities to improve oral cancer screening by dentists, especially for disadvantaged patients with severe health needs.
Design and methods: Using a mixed-methods approach, we will evaluate the feasibility and acceptability of integrating a telementoring component into the identification of oral lesions using the following 3 methods: 1) administering provider surveys that consist of a checklist of 10 key components of the intervention based on process, and asking the dental provider subjects if each one was covered; 2) conducting semi-structured interviews informed by the Consolidated Framework for Implementation Research and the Implementation Outcomes Framework with dental resident subjects to assess specific barriers to sustaining the intervention and strategies for addressing these barriers to facilitate integration of the intervention into the routine workflow of the dental clinics; and 3) administering brief exit interviews with patient subjects regarding the acceptability of the intervention to assess satisfaction with the use of intra-oral cameras at chairside to screen for and refer patients with oral lesions and identification of these oral lesions via EHR and secure e-mail tele-mentoring with an oral pathology expert.
Expected impact of the study for public health: If successful, then later clinical trials will maximize the external validity of the intervention and facilitate the widespread implementation and dissemination of the model for the teaching of dentists and residents, with the ultimate goal of improving patient care.
Significance for public health.
This protocol demonstrates how to utilize implementation science methods to conduct a feasibility and acceptability study designed to integrate a tele-mentoring component into the identification of oral lesions at the 6 dental clinics of a Federally Qualified Health Center in Brooklyn, NY. It provides a model for embedded implementation research in a low-resource setting that may be adapted for diverse community health centers throughout the United States and the Caribbean. The study will evaluate whether or not the use of intra-oral cameras and a tele-mentoring component that facilitates consultation with an oral pathology expert aids in the detection and identification of oral lesions during routine dental visits.
Key words: Tele-dentistry, dental clinics, oral cancer screening, oral health care, intra-oral cameras
Introduction
Oral cancer risks in low-income, racial/ethnic minority, and immigrant communities
In 2020, an estimated 53,260 people in the United States will be diagnosed with oral cavity and oropharyngeal cancer, and an estimated 10,750 people will die of these cancers.1 The primary risk factors for oral cavity cancer are tobacco and alcohol use,1,2 whereas the primary risk factor for oropharyngeal cancer is human papillomavirus (HPV) infection, particularly types 16 and 18.1,3 Oral cancer risks are compounded in low-income, racial/ethnic minority, and immigrant communities by difficulties in accessing health care services and multiple linguistic, cultural, economic, and social barriers.4 Immigrants who have lived in the United States for longer periods of time and possess higher degrees of acculturation may have different cancer risks (e.g., consumption of tobacco and/or alcohol, sexual behaviors) than immigrants who report fewer years of US residence or lesser degrees of acculturation. 5,6 For all population groups, cultural beliefs influence both health care choices and service use. For instance, among certain Asian subgroups, a strong sense of group collectivism exists, and individuality is submerged in the interest of group welfare.7 Friends, neighbors, and family members are often accessed and consulted before turning to formal health care services,7 which may delay the identification and diagnosis of cancer, including oral cancer, especially in rural and other remote communities where pathology expertise may be absent.8,9
Cancer incidence rates for sites within the oral cavity have generally shown a downward trend over recent decades in the United States, while incidence rates for oropharyngeal cancer have increased during this same time period.10,11 One evidence-based strategy for reducing or preventing cancers at oral cavity sites is to attenuate or eliminate exposures to oral cancer risk factors through education, behavior change, and HPV vaccination, while a second evidence-based strategy is the identification of oral lesions suspicious for pre-malignancy or malignancy by dentists as part of preventive dental visits.12 Suspicious lesions ought to undergo biopsy, whereas any other identified lesions ought to be reevaluated within 7-14 days and possibly undergo cytologic evaluation.13
Promise of tele-dentistry
Dental provider shortages, remoteness, funding challenges, and decreased costs, coupled with advances in technology and the ongoing coronavirus virus 19 (COVID-19) pandemic, have increased interest in the use of tele-medicine applications.14,15 In recent years, the field of dentistry has benefitted from myriad technological innovations, as is the case with medicine and other health care sectors. Among the most important of these advances in dentistry are the use of computers, tele-communications technology, digital diagnostic imaging services, and specialized hardware and software for patient screening and follow-up.16 Technological capabilities that were considered implausible only a few decades ago are now possible in dental care, but implementing and evaluating them in diverse, low-resource dental settings requires the active engagement of key organizational stakeholders and clinical, technological, and scientific experts.17 By leveraging advanced information technologies, the field of dentistry has unprecedented potential to progress far more in the next decade than it has since its professionalization in the United States in the mid-nineteenth century.18 New information technologies have not only improved the quality of dental patient management, but have also made it possible to achieve partial or complete management remotely, even at distances of thousands of miles from community health center training sites or dental experts. Networking, the sharing of digital dentistry information, and distant consultations, workups, and analyses are handled by a specific branch of dentistry-related telemedicine known as tele-dentistry.19,20
Use of diagnostic-imaging multiformat cameras for identification of oral lesions
Routine screening of the entire oral mucosa, together with risk status assessment, should be recorded in the patient’s chart at every dental visit (both negative and positive findings).21 Low-cost intra-oral cameras may facilitate the identification of previously hidden and often overlooked defects in teeth and other parts of the oral cavity.22 Previous reports have documented their use in recording carious lesion appearance in the patient record, and they may also be of significant benefit in monitoring early lesions over time following their detection.23,24 This benefit extends not only to dentists but also to patients, for whom it may be a useful educational and motivational tool.23 To the best of our knowledge, there are no prior findings in the extant literature regarding the use, accuracy, and cost-effectiveness of intra-oral cameras to screen for oral cancer during preventive dental visits. Hence, the proposed study and other research involving tele-dentistry applications are needed to assess the feasibility and acceptability of intra-oral cameras in the detection of non-malignant, pre-malignant, and malignant oral lesions during routine screening by dentists at chairside.24
Rationale for study design
Dental practitioners have been called “the primary vanguards against oral cancer”13 and are in a unique position to opportunistically examine the oral cavity and, to a lesser extent, the oropharynx during routine dental visits.12 Moreover, their educational background includes knowledge of the normal and pathological presentation of oral subsites,12 which is further enhanced during dental residency training. Nonetheless, the detection and identification of lesions is hampered by difficulties in visualizing lesions intra-orally and lack of expertise among general dentists in oral cancer detection. We hypothesize that the oral pathology asynchronous tele-mentoring intervention will be both feasible to implement in the dental clinic setting and acceptable to dental patients who visit dental clinics for routine visits.
Trial registration
ClinicalTrials.gov, NCT04166214, registered 15 November 2019, available at: https://clinicaltrials.gov/ct2/show/NCT04166214?term=NCT04166214&draw=2&rank=1
Materials and Methods
The aim of the proposed study is to evaluate the feasibility and acceptability of integrating a tele-mentoring component into the identification of oral lesions at the 6 dental clinics of Family Health Centers at NYU Langone, a Federally Qualified Health Center in Brooklyn, NY. The primary objective of this study is to assess the feasibility of the oral pathology asynchronous tele-mentoring intervention in the dental clinic setting. The secondary objective of this study is to assess the acceptability of the asynchronous tele-mentoring pilot intervention to adult dental patients in the dental clinic setting.
Approach of study
Using a mixed-methods approach, we will evaluate the feasibility and acceptability of integrating a tele-mentoring component into the identification of oral lesions at the following 6 dental clinics of Family Health Centers at NYU Langone in Brooklyn, NY. This will be achieved through the following 3 methods: 1) administering provider surveys (n=12) that consist of a checklist of 10 key components of the intervention based on process, and asking the dental provider subjects at each of the 6 Family Health Centers at NYU Langone dental sites if each one was covered; 2) conducting semi-structured interviews (n=6) with dental resident subjects at each of the 6 Family Health Centers at NYU Langone sites to assess specific barriers to sustaining the intervention and strategies for addressing these barriers to facilitate integration of the intervention into the routine workflow of the dental clinics—the interviews will be informed by the Consolidated Framework for Implementation Research25 (CFIR) and the Implementation Outcomes Framework26 (IOF); and 3) administering brief exit interviews (n=30) with patient subjects at each of the 6 Family Health Centers at NYU Langone dental sites regarding the acceptability of the intervention (the survey will assess patient satisfaction with the use of intra-oral cameras at chairside to screen for and refer patients with oral lesions and identification of these oral lesions via tele-mentoring with an oral pathology expert).
Impact of study
If this pilot study proves successful, NYU Langone Health is equipped with both clinical and organizational expertise in faculty development activities, as well as the existing NYU Langone Dental Medicine national network of video-teleconferencing and web-based educational technology, to scale up the proposed oral pathology asynchronous tele-mentoring intervention for the teaching of dental educators and residents, with the ultimate goal of improving patient care.
Assessment of primary study endpoints
Feasibility will be assessed using provider surveys, semi-structured interviews, and EHR data. We developed a checklist of 10 key components of the intervention based on process and will ask the participating dentists and residents at the 6 Family Health Centers at NYU Langone dental clinics if each was covered (see Appendix 1). This will be completed only once at the end of the implementation phase for each consented dental provider subject, and refer to the intervention experience with a specific consented patient subject. Endorsement of 8 of the 10 checklist items (80%) by the dental provider subjects will be considered as the feasibility criterion. Moreover, we will allow for open-ended collection of feedback on the feasibility of using the intra-oral cameras for identification of oral lesions as part of the tele-mentoring intervention.
Semi-structured interviews will also be conducted with dental resident subjects (see Appendix 2). We anticipate conducting 6 interviews before obtaining data saturation. The questions will be informed by the CFIR25 and IOF26 constructs and will assess specific barriers to implementing and sustaining the intervention and strategies for addressing those barriers to facilitate integration of the intervention into the routine workflow of the Family Health Centers at NYU Langone dental clinics.
Assessment of secondary study endpoints
Acceptability will be assessed using patient exit interviews27 (PEIs) conducted immediately after the dental visit is completed. Specifically, research staff will conduct a brief exit interview with 5 patients at each of the 6 Family Health Centers at NYU Langone dental clinics with language interpretation services available regarding the acceptability of the intervention. We developed 5 statements on patient satisfaction with the intra-oral cameras and the overall tele-mentoring intervention that will constitute the PEI (see Appendix 3). Patients will be asked the extent to which they agree with each statement (e.g., Dentists should discuss with me ways to prevent and screen for oral cancer: strongly agree, agree, disagree, or strongly disagree). The acceptability criterion of the intervention will be that 80% or more of patients rate all 5 administered acceptability questions as “strongly agree” or “agree.”
Study device
Below we describe the SOPROCARE® intra-oral camera to be used in this study (a full description is available from: https://www.acteongroup.com/us/products/imaging/diagnosticcameras/ soprocare). The SOPROCARE® intra-oral camera is available via commercial vendors to health care providers and is intended for the practice of general dentistry to aid in the diagnosis of pit and fissure caries, visualize anatomical details that are invisible to the naked eye or with a mirror, and highlight dental plaque and gingival inflammation. With regard to oral lesions, the magnification capability of SOPROCARE® helps to improve detection and identification. Images can be captured and stored in any imaging software, including the Dexis program within the Dentrix EHR, providing the necessary technological tools to practice minimally invasive dentistry.
Procedures for training interventionalists and monitoring intervention fidelity
The PI will train and supervise the dental providers, who will implement the study. Since the training and practice of the attending dentists and the residents they supervise tends to vary across sites and is a key factor in whether educational interventions work, close attention will be paid to implementation fidelity. The PI has extensive experience in training dental providers to deliver interventions with fidelity, and the NYU Langone Dental Medicine Postdoctoral Residency Program emphasizes both quality clinical care and advanced research training.
Specifically, the tele-mentoring intervention involves training dental faculty members and residents to use intra-oral cameras to take photographs of oral lesions and place them in the Dentrix EHR, along with descriptions of the lesions. This information will then be sent via Dentrix EHR to the Director of Oral Pathology, and an initial dummy code entry will be placed in the Dentrix EHR. For each patient with a detected lesion, the Director of Oral Pathology will then review the Dentrix EHR chart and the uploaded photograph(s) of the lesion(s) found and place his observations in the Dentrix EHR. Next, the Director of Oral Pathology will discuss his findings with the involved dental faculty member / dental resident via secure NYU Langone Health e-mail. The dental provider will then enter an apt comment in the Dentrix EHR, using the following template: “Reviewed entry and contacted patient. Follow-up appointment needed / not needed (along with the date of patient contact) for an appointment on (date).” A second dummy code entry will then be placed in the patient record in the Dentrix EHR. Once a week, the Director of Oral Pathology will receive a Dentrix EHR report with the 2 affiliated dummy codes for the tele-mentoring pilot study, and assure that entries for both codes are completed, thus closing the loop on the process.
Study procedures and schedule
The protocol for the tele-mentoring study was designed by the PI and the Director of Oral Pathology, and is summarized in Figure 1. This workflow will be refined based upon the results of the planned feasibility and acceptability testing. All study activities will take place in the 6 Family Health Centers at NYU Langone dental clinics and private offices of NYU Langone Dental Medicine in Brooklyn, NY. The PEIs with patient subjects and the feasibility checklists with provider subjects will take 10-15 minutes to complete. The semi-structures interviews with dental resident subjects will take 30-45 minutes to complete, and will be digitally recorded and transcribed. The transcriptions will be stored in a secure Research Electronic Data Capture (REDCap) database. The digital files will be deleted once they are transcribed. No identifying information will be recorded.
Statistical considerations and quantitative analyses
A sample size calculation is not indicated for this feasibility and acceptability study. All quantitative analyses will be conducted by the data analyst under the direction of the biostatistician.
Provider survey. The feasibility criterion of the intervention will be the endorsement of 8 of the 10 checklist items (80%) by the dental provider subjects.
Patient exit survey. The acceptability criterion of the intervention will be that 80% or more of patients rate all 5 administered acceptability questions as “strongly agree” or “agree” on a Likert Scale.
Semi-structured interviews and qualitative analyses
Provider semi-structured interview. All interviews will be transcribed by a transcription company and coded by 2 research team members. The research team members will code individually and then meet to discuss and agree upon the final codes. The analysis of the qualitative data will utilize the techniques of narrative analysis and be guided by the constant comparison analytic approach to identify themes.
Informed consent process
A consent form and a key study information form specific to the category of subject enrolled (dental patient or dental provider) that describe in detail the study device, study procedures, and risks and possible benefits will be given to each subject and written documentation of informed consent will be required prior to beginning the study. The following consent materials were submitted with this protocol and approved by the IRB, and are available upon request from the authors:
Consent Forms (dental patient and dental provider); and
Research Subject Key Study Information Forms (dental patient and dental provider).
Patient data
All data entered into the research database (in REDCap) will be protected by confidential entry codes. Locked file cabinets will be used to store materials with identifying information (e.g., consent forms). Unique identifiers will always replace patient names in all research databases. All computer systems are protected from possible external access. No Internet access is possible with the research systems to be used for this study. In addition, computer records will be maintained in such a way that the patient’s name or other obvious identifying information is not accessible in the same file or by using the same code.
The digitally recorded interviews will be transcribed. The transcriptions will be kept in a password-protected computer. The files will be deleted once they are transcribed. No identifying information will be recorded.
Discussion
Tele-dentistry has been reported to be comparable to face-toface examination for oral screening in a systematic review that used the Quality Assessment of Studies of Diagnostic Accuracy tool to assess the methodologic quality of studies: sensitivity (25-100%), specificity (68-100%), positive predictive value (57-100%), and negative predictive value (50-100%).15 The potential of our oral pathology asynchronous tele-mentoring intervention to aid in the detection of oral lesions holds promise for reaching patients in rural areas and communities with limited access to care, especially given the COVID-19 pandemic.15 If the results of this feasibility and acceptability study indicate that further testing of the model is indicated, we plan to partner with clinical trial experts at the Perlmutter Cancer Center at NYU Langone Health to conduct a real-world efficacy trial at training sites that are part of the NYU Langone Dental Medicine network.
The study design includes several limitations. First, the dental clinics at Family Health Centers at NYU Langone and the Dentrix EHR protocol may not be generalizable to dental clinics at geographically diverse community health centers or other EHRs in use at these sites. Hence, adaptations to the tele-mentoring intervention, including security safeguards, may be needed in future trials. Second, while most general dentists elect to opportunistically screen their patients for oral cancer, false positive findings can manifest as unnecessary patient anxiety, and can also incur monetary costs, discomfort, and possible side-effects of subsequent biopsies.12 To reduce the potential for false-positive screening results for seemingly innocuous lesions, dentists should follow up with patients in 7-14 days to confirm persistence of the lesion after removing any possible cause.13 Conversely, false negative findings can give rise to a false sense of security and result in patients failing to pursue care should symptoms later arise.12 Thus, use of an intra-oral camera may improve the ability of general dentists to detect lesions in the oral cavity that otherwise may have been missed and merit follow-up.
Notwithstanding these limitations, this feasibility and acceptability study provides an important first step in implementing a tele-mentoring intervention that has the potential to identify and diagnosis non-malignant, pre-malignant, and malignant oral lesions and improve patient care. If successful, then later trials will maximize the external validity of the tele-mentoring model and facilitate the widespread implementation, dissemination, and sustained utilization of evidence-based oral cancer screening, referral, and care coordination guidelines.
Figure 1.
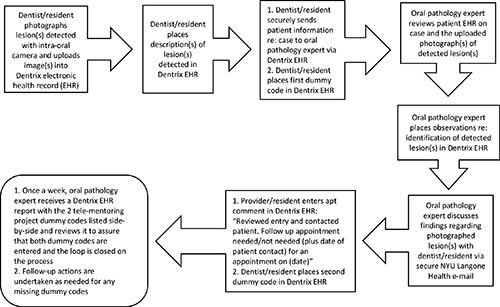
Workflow for the tele-mentoring pilot study to detect and identify oral lesions at chairside by dental faculty and residents.
Acknowledgments
The authors thank the participating site directors, dentists, dental residents, and patients, without whose support this study would not be possible.
Funding Statement
Funding: The study protocol for the project titled, Oral Pathology Asynchronous Tele-mentoring Pilot Study (PI: Dr. Nathalie Mohadjeri-Franck) was funded by the US Health Services and Services Administration (HRSA) as part of the Dental Faculty Development and Loan Repayment Program (grant T93HP30391). The Principal Investigator (PI) of the HRSA grant is Dr. Neal Demby, the Program Coordinator of the HRSA grant is Dr. Mary E. Northridge, and the Project Officer (PO) of the HRSA grant is Mr. Jesse Ungard. The funding agency (HRSA) and PO (Mr. Jesse Ungard) had no role in the study design; collection, management, analysis, and interpretation of data; writing of the report; and decision to submit the report for publication, and will have no ultimate authority over any of these activities.
References
- 1.American Cancer Society. Key statistics for oral cavity and oropharyngeal cancers. 2020. Available from: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html. [Google Scholar]
- 2.Rivera C. Essentials of oral cancer. Int J Clin Exp Pathol 2015;89:11884-94. [PMC free article] [PubMed] [Google Scholar]
- 3.Yete S, D’Souza W, Saranath D. High-risk human papillomavirus in oral cancer: clinical implications. Oncology 2018;94:133-41. [DOI] [PubMed] [Google Scholar]
- 4.Henshaw MM, Garcia RI, Weintraub JA. Oral health disparities across the life span. Dent Clin North Am 2018;62:177-93. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. Tobacco use among U.S. racial/ethnic minority groups--African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, Hispanics. A Report of the Surgeon General. Executive summary. MMWR Recomm Rep 1998;47:v-xv, 1-16. [PubMed] [Google Scholar]
- 6.Kalra P, Srinivasan S, Ivey S, Greenlund K. Knowledge and practice: the risk of cardiovascular disease among Asian Indians. Results from focus groups conducted in Asian Indian communities in Northern California. Ethn Dis 2004;14:497-504. [PubMed] [Google Scholar]
- 7.Esperat MC, Inouye J, Gonzalez EW, et al. Health disparities among Asian Americans and Pacific Islanders. Annu Rev Nurs Res 2004;22:135-59. [PubMed] [Google Scholar]
- 8.May M. A better lens on disease. Sci Am 2010;302:74-7. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein RS, Graham AR, Barker GR. Second-opinion telepathology services for cancer patients. Ternullo J, editor. Thought leaders project: e-health, telemedicine, connected health - the next wave of medicine. CreateSpace Independent Platform; 2012. p. 16-28. [Google Scholar]
- 10.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2016. Bethesda, MD: National Cancer Institute; Available from: https://seer.cancer.gov/archive/csr/1975_2016/ Based on November 2018 SEER data submission, posted to the SEER web site, April 2019. [Google Scholar]
- 11.Denson L, Janitz AE, Brame LS, Campbell JE. Oral cavity and oropharyngeal cancer: changing trends in incidence in the United States and Oklahoma. J Okla State Med Assoc 2016;109:339-45. [PMC free article] [PubMed] [Google Scholar]
- 12.Psoter WJ, Morse DE, Kerr AR, et al. Oral cancer examinations and lesion discovery as reported by U.S. general dentists: Findings from the National Dental Practice-Based Research Network. Prev Med 2019;124:117-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoopler ET, Sollecito TP. Oral cancer. Dent Clin North Am 2018;62:ix-x. [DOI] [PubMed] [Google Scholar]
- 14.Yoshinaga L. The use of teledentistry for remote learning applications. Pract Proced Aesthet Dent 2001;13:327-8. [PubMed] [Google Scholar]
- 15.Ather A, Patel B, Ruparel NB, et al. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod 2020. pii: S0099-2399(20)30159-X. doi: 10.1016/j.joen. 2020.03.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alabdullah JH, Daniel SJ. A systematic review on the validity of teledentistry. Telemed J E Health 2018;24:639-48. [DOI] [PubMed] [Google Scholar]
- 17.McLaren SW, Kopycka-Kedzierawski DT, Nordfelt J. Accuracy of teledentistry examinations at predicting actual treatment modality in a pediatric dentistry clinic. J Telemed Telecare 2017;23:710-5. [DOI] [PubMed] [Google Scholar]
- 18.McCauley HB. The first dental college: emergence of dentistry as an autonomous profession. J Hist Dent 2003;51:41-5. [PubMed] [Google Scholar]
- 19.Queyroux A, Saricassapian B, Herzog D, et al. Accuracy of teledentistry for diagnosing dental pathology using direct examination as a gold standard: results of the Tel-e-dent Study of older adults living in nursing homes. J Am Med Dir Assoc 2017;18:528-32. [DOI] [PubMed] [Google Scholar]
- 20.Estai M, Kanagasingam Y, Tennant M, Bunt S. A systematic review of the research evidence for the benefits of teledentistry. J Telemed Telecare 2018;24:147-56. [DOI] [PubMed] [Google Scholar]
- 21.Ogden G, Lewthwaite R, Shepherd SD. Early detection of oral cancer: how do I ensure I don't miss a tumour? Dent Update 2013;40:462-5. [DOI] [PubMed] [Google Scholar]
- 22.Pentapati KC, Siddiq H. Clinical applications of intraoral camera to increase patient compliance – current perspectives. Clin Cosmet Investig Dent 2019;23;11:267-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pretty IA, Ekstrand KR. Detection and monitoring of early caries lesions: a review. Eur Arch Paediatr Dent 2016;17:13-25. [DOI] [PubMed] [Google Scholar]
- 24.Pentapati KC, Mishra P, Damania M, et al. Reliability of intraoral camera using teledentistry in screening of oral diseases - pilot study. Saudi Dent J 2017;29:74-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Proctor EK, Landsverk J, Aarons G, et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health 2009;36:24-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pbert L, Adams A, Quirk M, et al. The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol 1999;18:183-8. [DOI] [PubMed] [Google Scholar]


