Corona virus disease 2019 (COVID-19) is primarily associated with respiratory failure but both renal and circulatory failure is a common occurrence in patients with more severe disease that require intensive care [1], or die of the disease [2]. The developing guidelines for treating COVID-19 patients in intensive care suggest a frugal fluid strategy to avoid acute respiratory distress syndrome [3]. However, this may leave fluid resuscitation insufficient for renal and circulatory function increasing the risk of acute kidney injury (AKI). This case series is part of a study approved by the National Ethical Review Agency (EPM; No. 2020-01623). Informed consent was obtained from the patient, or next of kin if the patient was unable give consent. The Declaration of Helsinki and its subsequent revisions were followed. Plasma renin as well as biochemistry was collected with routine clinical sampling in the morning and analysed by the clinical chemistry department at Uppsala University Hospital according to standard procedures. We present a case series where we found pronounced hyperreninemia in association with hypernatremia, hyperchloremia and low glomerular filtration rate primarily in patients late in their intensive care stay (Table 1).
TABLE 1.
Biochemistry of patients ordered by days after intensive care admission
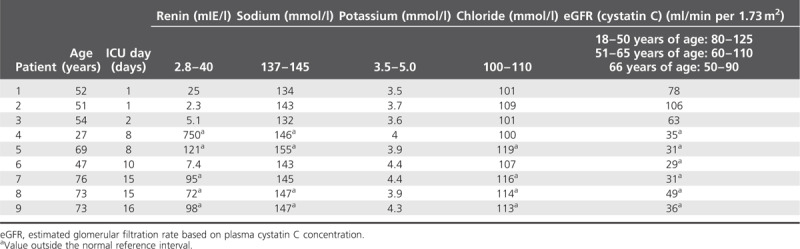
There are several possible explanations for these findings. One is that the ACE2 affinity of SARS-COV-2 [4] directly affects the renin–angiotensin system and drives renin secretion despite high circulating sodium chloride. However, the association with high sodium and chloride suggests extra cellular fluid contraction and for the kidneys excessively restrictive fluid therapy with hypovolemia and water deficit. An alternative is a virus-induced or cytokine-induced renin release acting as a pseudohypovolemia. In this setting, the combination of high renin and high chloride may interact through the tubuloglomerular feedback system to supress glomerular filtration rate, thereby contributing to the development of AKI in COVID-19 patients. The data may also suggest that this is an iatrogenic cause during intensive care as we do not see it in recently admitted patients. The restrictive use of fluid resuscitation in COVID-19 may be beneficial for the lungs but may also promote AKI. However, if coagulopathy and microthrombi contribute importantly to the progression as has been suggested, low circulating volume may impair pulmonary flow regulation and thereby oxygenation as well. Significantly, the use of renin–angiotensin blockers have been found to be associated with improved outcome [5], and the present data may suggest that ameliorating the overactivation of the renin–angiotensin system may be a mechanism.
In conclusion, patients with COVID-19 tend to develop hyperreninemia combined with hypernatremia and hyperchloremia in intensive care, which is associated with AKI in a way that suggests hypovolemia or pseudohypovolemia.
ACKNOWLEDGEMENTS
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of COVID-19 in New York City. N Engl J Med 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with corona virus disease 2019: retrospective study. BMJ 2020; 368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579:270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


