Abstract
The aim of the present study is to share the experience of chronic peritoneal dialysis (PD) at King Hussein Medical Center, Amman, Jordan, and to highlight the complications of this procedure. This is a retrospective chart review study for all the children from day 1 of life to 14 years, who underwent chronic PD for end-stage renal disease (ESRD) during the period of 10 years extending from 2009 to 2019. The following data were collected: mode of dialysis, type of peritoneal dialysis, age of starting peritoneal dialysis, gender, aetiology of ESRD, duration on PD, complications and outcome. A total number of 269 children were included: 229 patients received haemodialysis and 40 children (22 boys and 18 girls) received PD. Of those, two children were on automated PD and 38 children were on continuous ambulatory peritoneal dialysis. The mean age at the start of PD was 62 ± 38 months. The mean duration of PD was 43 months. The mean catheter duration was 34 months. Six patients were shifted to haemodialysis permanently and four patients received a kidney transplant. Eleven patients died. The most common complications were peritonitis (52.5%), exit-site infection (30%) and malfunctioning catheter (12.5%). The rate of peritonitis was one episode per 22 patient-months. Peritoneal dialysis is a promising mode of dialysis for children in Jordan. Peritonitis is the most common complication associated with PD. Kidney transplantation is the best modality of renal replacement therapy in terms of long-term survival and quality of life and should be encouraged on national level.
Keywords: End-stage renal disease, Child, Jordan, Chronic peritoneal dialysis, Hemodialysis, Kidney transplant
INTRODUCTION
In the past few decades, peritoneal dialysis (PD) started to get more acceptance as the first paediatric dialysis modality [1–6], and now, it is the most common modality of dialysis with end-stage renal disease (ESRD) in many countries [7–9]. Before 1982, fewer than 100 paediatric patients had been treated with continuous ambulatory peritoneal dialysis (CAPD), whereas continuous cycler peritoneal dialysis for children was virtually unknown [10].
In Jordan, the first intermittent peritoneal dialysis (IPD) was performed at Jordan University Hospital IPD in 1979. Later, when CAPD became popular, the first CAPD was performed in Al-Bashir Hospital in 1986 [11]. Nowadays, acute PD is available in the Ministry of Health Hospital, university hospitals and private sector. Chronic PD in the form of automated peritoneal dialysis is available at Prince Hamza Hospital and King Hussein Medical Center [12]. In the hospital, King Hussein Medical Center, the paediatric haemodialysis was started in 1999, but PD was delayed until 2009, and since then, the number of patients who were started on this mode of dialysis increased.
The number of children who underwent a kidney transplant in Jordan during the same period is around 150 patients, which is relatively small and may be attributed to the paucity of available kidneys for transplant as we depend mainly on relative living donor. Hence, usually, the patient is kept on haemodialysis or PD for a long time, and more complications with these two modalities will arise.
In this article, we share the experience in paediatric PD over a 10-year period, including complications, prognosis and outcome at Queen Rania Al Abdallah Hospital for Children, King Hussein Medical Center, Amman, Jordan
MATERIALS AND METHODS
This was a retrospective chart review observational study for all paediatric patients with age range from Day 1 to 14 years, who received PD at Queen Rania Al Abdallah Hospital for Children, from 2009 to 2019. This hospital is a referral hospital for kidney diseases in Jordan. The following data were collected: mode of dialysis, type of PD, age of starting PD, gender, aetiology of ESRD, duration on PD, complications and outcome.
The selection criteria for CAPD/APD treatment patients were: patient and family preference, good compliance history, failure to insert vascular access, complication and failure of haemodialysis and no major medical or surgical contraindications for PD.
The diagnosis of peritonitis is made if the peritoneal effluent is cloudy, the effluent white blood cell count is greater than 100/mm3, at least 50% of the WBCs are polymorphonuclear leukocytes and positive culture. A negative culture does not exclude bacterial peritonitis [13]. In the hospital, we use a double-cuff straight peritoneal catheter which is placed in a paramedian or lateral site of the abdomen. Prophylactic antibiotic cefazolin is given immediately before placement of the PD catheter.
The statistical analysis was performed using the SPSS version 25 and the results were expressed as mean + standard deviation (SD) or median (range).
The study was approved by the Human Research Ethics Committee of the Royal Medical Services, Amman, Jordan. Waiver of informed consent was obtained, and confidentiality was ensured at all levels.
RESULTS
During the study period, which extends from 2009 to 2019, the total number of paediatric patients who presented with ESRD and needed dialysis was 269 patients. The age ranges between 1 day and 14 years. Forty children (14.9%, 22 boys and 18 girls) received PD, whereas 229 children (85.1%) received haemodialysis. Two children were on APD and 38 children were on CAPD. The mean age at the start of PD was 62 ± 38 months (Table 1), and the mean duration of PD was 43 months. Thirty-two patients were started on PD as the initial mode of treatment, and six patients were started first on Hemodialysis (HD) and then shifted to PD.
Table 1.
Distribution of children on PD according to age.
| Age at starting PD | Numbers of patients/percentage |
|---|---|
| <1 year | 6/15% |
| 2–5 years | 21/52.5% |
| 5–10 years | 9/22.5% |
| 10–14 years | 4/10% |
PD = peritoneal dialysis.
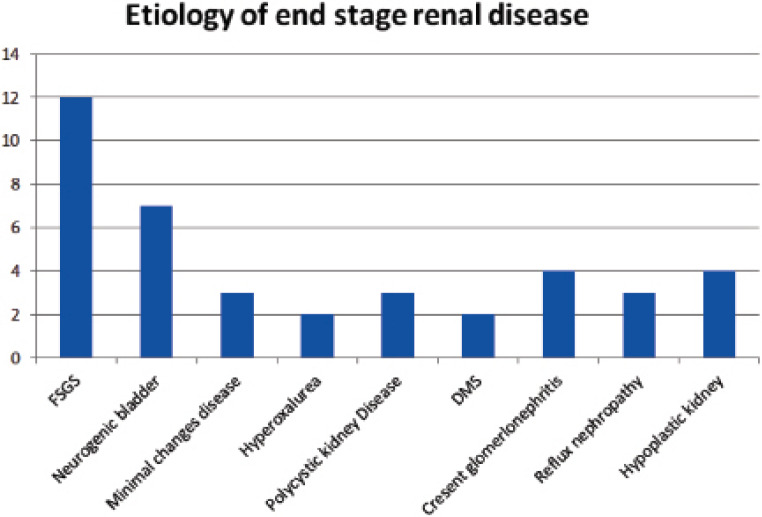
The most common causes of ESRD for patients treated with PD (Figure 1) were focal segmental glomerulosclerosis in 12 patients (30%), neurogenic bladder in 7 patients (17.5%) and crescent glomerulonephritis in 4 patients (10%). The most common complications were peritonitis (52.5%), exit-site infection (30%) and malfunctioning catheter (12.5%, Table 2). The rate of peritonitis was one episode per 22 patient-months.
Figure 1.
Aetiology of ESRD in paediatric patients on PD. Diffuse mesengial sclerosis (DMS), diffuse mesangial sclerosis; focal segmental glomerulosclerosis (FSGS), focal segmental glomerulosclerosis.
Table 2.
Complications associated with peritoneal dialysis in paediatric patients.
| Complication | Number of patients (percentage) |
|---|---|
| Peritonitis | 21 (52.5%) |
| Exit-site infection | 12 (30%) |
| Obstruction | 3 (7.5%) |
| Leak | 2 (5%) |
| Hernia | 2 (5%) |
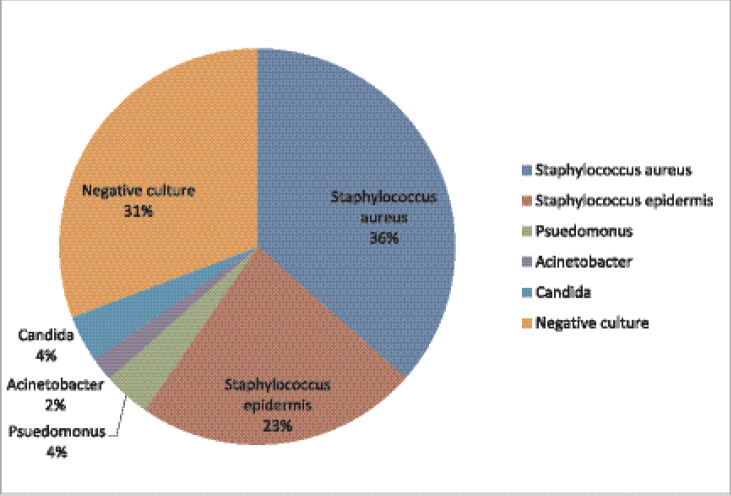
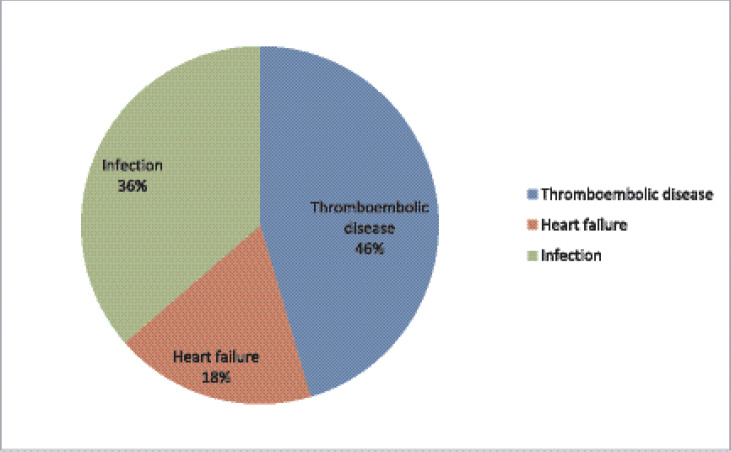
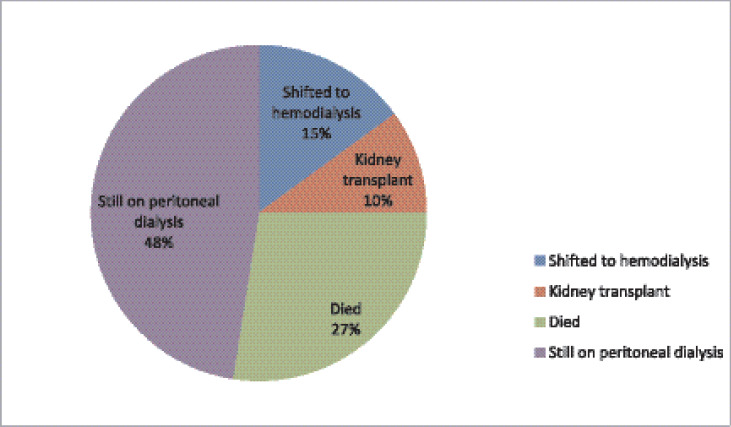
The total number of peritonitis was 52 episodes in 21 patients, as 14 of them had recurrent peritonitis. The most common organisms involved in peritonitis (Figure 2) were Gram positive [59.6%, Staphylococcus aureus (36.5%) and Staphylococcus epidermidis: 23.1%]. These were followed by gram negative organisms [5.8%, Pseudomonas aeruginosa (3.8%) and Acinetobacter: 2%], candida (3.8%) and unknown (30.8%). Peritoneal dialysis catheters were removed in 13 patients due to recurrent peritonitis (8 patients) and malfunctioning (5 patients). The mean catheter duration was 34 months. Eleven (27.5%) patients died during the study period; of which, 5 patients (46%) died due to thromboembolic disease, 4 patients (36%) due to severe infection and 2 patients (18%) due to heart failure (Figure 3). Six patients were shifted to haemodialysis permanently and four patients had a kidney transplant (Figure 4).
Figure 2.
Causative organisms of peritonitis in paediatric patients on chronic PD.
Figure 3.
Causes of death in PD patients.
Figure 4.
Outcome of the 40 patients who were on PD.
DISCUSSION
Haemodialysis still remains the main modality of dialysis in adult patients [14], but peritoneal dialysis is the preferred renal replacement therapy in children until renal transplantation can be received [5,6,15,16].
In Jordan, we still depend on haemodialysis as the primary mode of dialysis more than peritoneal dialysis even in paediatric patients. A report published in 2015 by the National Registry of End Stage Renal Disease in Jordan states that only 17% of paediatric patients are on peritoneal dialysis and 83% are on haemodialysis [17]. In the hospital, the paediatric peritoneal dialysis was adopted on 2009 and before that only few cases received CAPD (those who cannot offer three visits per week to the hospital for haemodialysis as the primary mode of end-stage renal disease). Since 2009, the number of patients who are on peritoneal dialysis has increased.
The PD modality is presented to the family as a modality of choice for RRT in cases with no contraindications, family education and training by paediatric nephrologist, and a well-trained PD nurse is also provided. The main obstacle is the family fear of taking responsibility in the treatment of their child at home and most of them preferred dialysis at hospital since the haemodialysis team is the one who performs all the dialysis procedures.
Peritoneal dialysis (PD) can be performed either manually as in CAPD or using mechanical devices as in APD. The number of patients on APD has increased over the recent years [18], but no difference between CAPD and APD for clinically important outcomes has been found [19]. In the institution, the number of APD patients is low (5%) since the cycler is not covered by the medical insurance plan yet. We have only two patients on automated PD, so we cannot compare between the two modalities.
More than half of the patients were below 5 years (67.5%) as the PD is the preferred mode of dialysis in small children due to difficulty in establishing a vascular access for haemodialysis [20,21]. A study from Saudi Arabia [22] reported that the mean age was 7.3 years, but the mean duration of peritoneal dialysis was less than what we found in this study which could be explained by the shortage of available kidneys for transplant in Jordan. The median duration on PD was high in the hospital compared to others [23] because most of the children were below 5 years and due to the paucity of available kidneys for transplant.
The North American Pediatric Renal Trials and Collaborative Studies 2011 annual dialysis report showed that the most common primary diagnoses in all dialysis patients were (FSGS, 14.4%), hypoplastic dysplastic kidney disorders (14.2%) and obstructive uropathy (12.6%) [6]. However, a study from Saudi Arabia [24] showed that the most common cause of chronic renal failure of paediatric patients who are on PD was posterior urethral valves followed by nephrolithiasis. In this study, the most common cause was focal segmental glomerulonephritis followed by neurogenic bladder. This can be explained by the fact that familial nephrotic syndrome is relatively common due to the high rate of consanguineous marriage.
Peritonitis is a major cause of PD failure (65.1%) and conversion to long-term haemodialysis [25]. Each PD unit should examine its own pattern of infection, causative organisms and sensitivities to establish its own guidelines for the treatment of peritonitis.
The incidence of peritonitis decreased in both adult and children over the past several decades [26–30]. In this study, 52% of the patients had at least one episode of peritonitis with a rate of peritonitis being 1 episode per 22 patient-months [20,23,31]. This is considered to be low rate in comparison to others: one episode of peritonitis every 4.3–18 patient-months [32–34].
A Gram-positive organism is the most common cause of peritonitis in adults [14]. In children, S. aureus (52%) and P. aeruginosa (32%) are the most common causes of exit-site infection and peritonitis [35]. In the hospital, the Gram-positive organisms are still the most common cause of peritonitis similar to what has been found in many studies [16,25]. The Gram-negative organism as a cause of peritonitis is found to be low in our hospital as it accounted for only 5.8%, but a study from Saudi Arabia reported a high incidence of Gram-negative organisms as a cause of peritonitis reaching to 43.5% [22]. Peritonitis due to fungal infection is considered to be rare globally, 8.1% in the USA [36], 2.9% in the Netherlands [37] and 3.1% in Canada [38]. Only two patients were found to have candida infection over the past 10 years. Culture-negative peritonitis accounts for about one-third of the patients. Many studies reported culture-negative episodes to be very high (59.2%) [25].
The T half-life of dialysis catheter was 34 months which is comparable to the developed countries [20]. The main reasons for the removal of PD catheter were recurrent peritonitis followed by catheter malfunction. Shifting to haemodialysis in all patients was due to recurrent peritonitis.
Eleven patients (27.5%) died during the study period. This percentage, which is considered to be high in comparison to other countries [39–41], is due to a prolonged waiting list for kidney transplant, which is the best mode of treatment for ESRD. In patients on renal replacement therapy, the main causes of death are cardiovascular diseases, both in adults and children [42,43]. The causes of death in haemodialysis and PD are different. In patients on haemodialysis, the most common cause of death is haemorrhagic stroke [44]. In contrast, in PD patients, the most common causes are both cardiovascular complications (heart failure and arterio-/atherothrombotic) and infections [6]. In this study, cardiovascular diseases were also the most common cause of death, mainly the thromboembolic disease (46%), but heart failure was responsible for only 18% of deaths. Severe infection is the cause of about one-third of deaths in the patients, which highlights the importance of prevention and aggressive management of infection.
CONCLUSION
Peritoneal dialysis is a promising mode of dialysis for children in Jordan. Having a well-trained staff, who can deal with PD and train families of PD patients, will decrease the complications in developing countries. Peritonitis is the most common complication associated with PD. Kidney transplantation is the best modality of renal replacement therapy in terms of long-term survival and quality of life and should be encouraged at the national level.
CONFLICTS OF INTEREST
None.
FUNDING
None.
ETHICAL APPROVAL
The study was approved by Human Research Ethics Committee of the Royal Medical Services, Amman, Jordan. Waiver of Informed Consent was obtained and confidentiality was ensured at all levels.
REFERENCES
- 1.Watson AR, Gartland C. European Paediatric Peritoneal Dialysis Working Group Guidelines by European committee for elective chronic peritoneal dialysis in pediatric patients. Perit Dial Int. 2001;21:240–44. [PubMed] [Google Scholar]
- 2.Tsai HL, Yang LY, Chin TW, Wang HH, Liu CS, Wei CF, et al. Outcome and risk factors for mortality in pediatric peritoneal dialysis. Perit Dial Int. 2010;30:233–39. doi: 10.3747/pdi.2008.00278. https://doi.org/10.3747/pdi.2008.00278. [DOI] [PubMed] [Google Scholar]
- 3.Phan J, Stanford S, Zaritsky JJ, DeUgarte DA. Risk factors for morbidity and mortality in pediatric patients with peritoneal dialysis catheters. J Pediatr Surg. 2013;48:197–202. doi: 10.1016/j.jpedsurg.2012.10.035. https://doi.org/10.1016/j.jpedsurg.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 4.Fraser N, Hussain FK, Connell R, Shenoy MU. Chronic peritoneal dialysis in children. Int J Nephrol Renovasc Dis. 2015;8:125–37. doi: 10.2147/IJNRD.S82419. https://doi.org/10.2147/IJNRD.S82419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fadrowski JJ, Frankenfield D, Amaral S, Brady T, Gorman GH, Warady B, et al. Children on long-term dialysis in the United States: findings from the 2005 ESRD clinical performance measures project. Am J Kidney Dis. 2007;50:958–66. doi: 10.1053/j.ajkd.2007.09.003. https://doi.org/10.1053/j.ajkd.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 6.North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) Annual Dialysis Report. [2017 Dec];2011 Available from: https://web.emmes.com/study/ped/annlrept/annualrept 2011.pdf .
- 7.Hattori S, Yosioka K, Honda M, Ito H. The 1998 report of the Japanese National Registry data on pediatric end-stage renal disease patients. Pediatr Nephrol. 2002;17:456–61. doi: 10.1007/s00467-002-0848-8. https://doi.org/10.1007/s00467-002-0848-8. [DOI] [PubMed] [Google Scholar]
- 8.Verrina E, Edefonti A, Gianoglio B, Rinaldi S, Sorino P, Zacchello G, et al. A multicenter experience on patient and technique survival in children on chronic dialysis. Pediatr Nephrol. 2004;19:82–90. doi: 10.1007/s00467-003-1270-6. https://doi.org/10.1007/s00467-003-1270-6. [DOI] [PubMed] [Google Scholar]
- 9.Fadrowski J, Alexander SR, Warady B. The demographics of dialysis in children. In: Warady BA, Schaefer F, Fine RN, Alexander SR, editors. Pediatric dialysis. Dordrecht, The Netherlands: Kluwer; 2011. pp. 37–51. https://doi.org/10.1007/978-1-4614-0721-8_3. [Google Scholar]
- 10.Alexander SR, Honda M. Continuous peritoneal dialysis for children: a decade of worldwide growth and development. Kidney Int Suppl. 1993;40:S65–74. [PubMed] [Google Scholar]
- 11.Said R. Renal replacement therapy in Jordan. Saudi J Kidney Dis Transpl. 1999;10:64–5. [PubMed] [Google Scholar]
- 12.Akl KF, Albaramki JH, Hazza I. Aetiology of paediatric end stage renal failure in Jordan: a multicenter study. W Indian Med J. 2016;65:263–6. doi: 10.7727/wimj.2014.151. https://doi.org/10.7727/wimj.2014.151. [DOI] [PubMed] [Google Scholar]
- 13.Warady BA, Schaefer FS, Fine RN, Alexander SR. Pediatric Dialysis. Boston, MA, USA: Kluwer Academic; 2004. Peritonitis; pp. 393–414. https://doi.org/10.1007/978-94-007-1031-3_24. [Google Scholar]
- 14.Najafi I, Alatab S, Atabak S, Majelan N, Sanadgol H, Makhdoomi K, et al. Seventeen years experience of peritoneal dialysis in Iran: first official report of the Iranian peritoneal dialysis registry. Periton Dialysis Int. 2010;34:636–42. doi: 10.3747/pdi.2012.00054. https://doi.org/10.3747/pdi.2012.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmitt C, Bakkaloglu S, Klaus G, Schröder C, Fischbach M. Solutions for peritoneal dialysis in children: recommendations by the European Pediatric Dialysis Working Group. Pediatr Nephrol. 2011;26:1137–47. doi: 10.1007/s00467-011-1863-4. https://doi.org/10.1007/s00467-011-1863-4. [DOI] [PubMed] [Google Scholar]
- 16.Sethna CB, Bryant K, Munshi R, Warady BA, Richardson T, Lawlor J, et al. Risk factors for and outcomes of Catheter-associated peritonitis in children: the SCOPE collaborative. Clin J Am Soc Nephrol. 2016;11:1590–6. doi: 10.2215/CJN.02540316. https://doi.org/10.2215/CJN.02540316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.As Sayaideh A, AlQaisi S, Asaid M. National Registry of End stage renal disease—annual report. [2019 Dec];2015 Available from: http://www.moh.gov.jo/Echobusv3.0/SystemAssets/25708778-d442-49b5-932d-f10c96601c2a.pdf .
- 18.Honda M, Iitaka K, Kawaguchi H, Hoshii S, Akashi S, Kohsaka T, et al. The Japanese national registry data on pediatric CAPD patients: aten-years experience a report of the study group of pediatric PD conference. Periton Dialysis Int. 1996;16:269–75. [PubMed] [Google Scholar]
- 19.Rabindranath KS, James Adams J, Ali TZ, MacLeod AM, Vale L, Cody JD, et al. Continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis for end-stage renal disease. [2020 Jan]; doi: 10.1002/14651858.CD006515. Cochrane Systematic Review - Intervention Version published: 18 April 2007 Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006515/abstract . https://doi.org/10.1002/14651858.CD006515. [DOI] [PMC free article] [PubMed]
- 20.Honda M. The 1997 Report of the Japanese National Registry data on pediatric peritoneal dialysis patients. Perit Dial Int. 1999;19:S473–8. [PubMed] [Google Scholar]
- 21.Mishra OM, Gupta AK, Pooniya V, Prasad R, Tiwary NK, Schaefer F. Peritoneal dialysis in children with acute kidney injury: a developing country experience. Perit Dial Int. 2012;32:431–36. doi: 10.3747/pdi.2012.00118. https://doi.org/10.3747/pdi.2012.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kari JA. Peritoneal dialysis in children. Saudi J Kidney Dis Transpl. 2005;16:348–53. [PubMed] [Google Scholar]
- 23.Chinchilla J, Sebastián K, Meléndez R, Ramay B, Lou-Meda R. Risk factors for peritonitis in a pediatric dialysis program in Guatemala, 2011-2014. Adv Nephrol. 2016;2016:6. https://doi.org/10.1155/2016/7179028. [Google Scholar]
- 24.Faraz A, Farhan MA, Shaikh K, Ali S. Experience of peritoneal dialysis in renal failure in children. Pak Armed Forces Med J. 2017;67:1015–21. [Google Scholar]
- 25.Ponce D, de Moraes TP, Pecoits-Filho R, Figueiredo AE, Barretti P. Peritonitis in children on chronic peritoneal dialysis: the experience of a large national pediatric cohort. Blood Purif. 2018;45:118–25. doi: 10.1159/000484344. https://doi.org/10.1159/000484344. [DOI] [PubMed] [Google Scholar]
- 26.Burkart J, Hylnader B, Durnell-Figel T, Roberts D. Comparison of peritonitis rates during long-term use of standard spike versus Ultraset in continuous ambulatory peritoneal dialysis (CAPD) Perit Dial Int. 1990;10:41–3. [PubMed] [Google Scholar]
- 27.Burkart J, Jordan JR, Durnell TA, Case LD. Comparison of exit-site infections in disconnect versus no disconnect systems for peritoneal dialysis. Perit Dial Int. 1992;12:317–20. [PubMed] [Google Scholar]
- 28.Valeri A, Radhakrishnan J, Vernocci L, Carmichael LD, Stern L. The epidemiology of peritonitis in acute peritoneal dialysis: a comparison between open- and closed-drainage systems. Am J Kidney Dis. 1993;21:300–9. doi: 10.1016/s0272-6386(12)80750-5. https://doi.org/10.1016/S0272-6386(12)80750-5. [DOI] [PubMed] [Google Scholar]
- 30.Monteón F, Correa-Rotter R, Paniagua R, Amato D, Hurtado ME, Medina JL, et al. Prevention of peritonitis with disconnect systems in CAPD: a randomized controlled trial. Kidney Int. 1998;54:2123–28. doi: 10.1046/j.1523-1755.1998.00190.x. https://doi.org/10.1046/j.1523-1755.1998.00190.x. [DOI] [PubMed] [Google Scholar]
- 31.Macchini F, Valadè A, Ardissino G, Testa S, Edefonti A, Torricelli M, et al. Chronic peritoneal dialysis in children: catheter related complications. A single centre experience. Ped Surgery Int. 2006;22:524–8. doi: 10.1007/s00383-006-1685-9. https://doi.org/10.1007/s00383-006-1685-9. [DOI] [PubMed] [Google Scholar]
- 32.Raaijmakers R, Gajjar P, Schröder C, Nourse P. Peritonitis in children on peritoneal dialysis in Cape Town, South Africa: epidemiology and risks. Pediatr Nephrol. 2010;25:2149–57. doi: 10.1007/s00467-010-1592-0. https://doi.org/10.1007/s00467-010-1592-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warady BA, Schaefer F, Holloway M, Alexander S, Kandert M, Piraino B, et al. ISPD Guidelines/ Recommendations- Consensus Guidelines for the treatment of peritonitis in pediatric patients receiving peritoneal dialysis. Dialysis Int. 2000;20:610–24. [PubMed] [Google Scholar]
- 34.Klaus G. Prevention and treatment of peritoneal dialysis-associated peritonitis in pediatric patients. Periton Dialysis Int. 2005;25:S117–19. [PubMed] [Google Scholar]
- 35.Beckwith H, Clemenger M, McGrory J, Hisole N, Chelapurath T, Newbury S, et al. Dialysis exit-site infection: definition and outcomes. Perit Dial Int. 2019;39:344–49. doi: 10.3747/pdi.2018.00216. https://doi.org/10.3747/pdi.2018.00216. [DOI] [PubMed] [Google Scholar]
- 36.Munshi R, Sethna CB, Richardson T, Rodean J, Al-Akash S, Gupta S, et al. Fungal peritonitis in the standardizing care to improve outcomes in pediatric end stage renal disease (SCOPE) collaborative. Pediatr Nephrol. 2018;33:873–880. doi: 10.1007/s00467-017-3872-4. https://doi.org/10.1007/s00467-017-3872-4. [DOI] [PubMed] [Google Scholar]
- 37.Raaijmakers R, Schröder C, Monnens L, Cornelissen E, Warris A. Fungal peritonitis in children on peritoneal dialysis. Pediatr Nephrol. 2007;22:288–93. doi: 10.1007/s00467-006-0289-x. https://doi.org/10.1007/s00467-006-0289-x. [DOI] [PubMed] [Google Scholar]
- 38.Levallois J, Nadeau-Fredette AC, Labbé AC, Laverdière M, Ouimet D, Vallée M. Ten-year experience with fungal peritonitis in peritoneal dialysis patients: antifungal susceptibility patterns in a North-American center. Int J Infect Dis. 2012;16:e41–3. doi: 10.1016/j.ijid.2011.09.016. https://doi.org/10.1016/j.ijid.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 39.Alberto E, Bruno G, Stefano R, Palma S, Graziella Z, Giancarlo L, et al. A multicenter experience on patient and technique survival in children on chronic dialysis. P Pediatr Nephrol. 2004;19:82–90. doi: 10.1007/s00467-003-1270-6. https://doi.org/10.1007/s00467-003-1270-6. [DOI] [PubMed] [Google Scholar]
- 40.Sinha R, Saha S. Continuous ambulatory peritoneal dialysis in children - experience from Eastern India. Indian Pediatr. 2015;52:531–2. [PubMed] [Google Scholar]
- 41.Akhtar N, Iftikhar S, Chaudhry A. The outcome of continuous ambulatory peritoneal dialysis in children: a single center experience. Biomedica. 2018;34 [Google Scholar]
- 42.Valderrabano F, Jones EHP, Mallick NP. Report on management of renal failure in Europe. Nephrol Dial Transpl. 1995;10:11–35. doi: 10.1093/ndt/10.supp5.1. https://doi.org/10.1093/ndt/10.supp5.1. [DOI] [PubMed] [Google Scholar]
- 43.Warady BA, Hebert D, Sullivan EK, Alexander SR, Tejani A. Renal transplantation, chronic dialysis and chronic renal insufficiency in children and adolescents. The 1995 annual report of the North American Pediatric Transplant Cooperative Study. Pediatr Nephrol. 1997;11:49–56. doi: 10.1007/s004670050232. https://doi.org/10.1007/s004670050232. [DOI] [PubMed] [Google Scholar]
- 44.Litwin M, Grenda R, Prokurat S, Abuauba M, Latoszyñska J, Jobs K, et al. Patient survival and causes of death on hemodialysis and peritoneal dialysis - single-center study. Pediatr Nephrol. 2001;16:996–1001. doi: 10.1007/s004670100012. https://doi.org/10.1007/s004670100012. [DOI] [PubMed] [Google Scholar]