Abstract
Modulation of immune responses by nutrients is an important area of study in cellular biology and clinical sciences in the context of cancer therapies and anti-pathogen-directed immune responses in health and disease. We review metabolic pathways that influence immune cell function and cellular persistence in chronic infections. We also highlight the role of nutrients in altering the tissue microenvironment with lessons from the tumor microenvironment that shapes the quality and quantity of cellular immune responses. Multiple layers of biological networks, including the nature of nutritional supplements, the genetic background, previous exposures, and gut microbiota status have impact on cellular performance and immune competence against molecularly defined targets. We discuss how immune metabolism determines the differentiation pathway of antigen-specific immune cells and how these insights can be explored to devise better strategies to strengthen anti-pathogen-directed immune responses, while curbing unwanted, non-productive inflammation.
Keywords: Infection, Cancer, Immunometabolism, Immunotherapy, Inflammation, Microbiome, Tuberculosis, MTB, T cell, Innate immune cell, Cytokine, Nutrition, Mitochondria
Introduction
Clinical immunologists have (re)discovered that the profile of cellular metabolism shapes the outcome of cellular development and immune functions: immunometabolism [1–3]. This prompted cross-fertilizing preclinical and clinical research between immunology, nutrition, and biochemistry [4]. The field of immunometabolism is marked by the impact of metabolic reprograming on the immune response as well as studying the fate of immune cells [5, 6]. The immunometabolic profile of cells influences their activation, their proliferative capacity, their quiescent state in tissues and in the systemic circulation. The functional specificity of each immune cell subset determines its biochemical requirements which is associated with different metabolic phenotypes [2, 7, 8]. These phenotypes are linked with variations in nutrient and oxygen availability, pH, as well as fluctuations during immune cell trafficking [2]. Thus, a well-founded understanding of molecular interactions between nutrient availability, biochemical requirements, and cellular metabolism is crucial to recognize how these components jointly affect immunodynamics in pathological conditions and ultimately shape the host immune response [9, 10]. We review therefore here more recent insights in immunometabolism in infections and cancer—a timely exercise since (i) nutrients are often limited in resource-constrained countries, (ii) immunonutritional concepts are often not considered in vaccine or adjuvant treatment protocols in patients with infections, (iii) similar molecular pathways are functional in “chronic antigen stimulation” in patients with bacterial and viral infections or cancer. Insights from curbing immunopathology and eliciting protective immune responses in patients with cancer will therefore cross-fertilize the advancement of new treatment concepts of patients with infectious diseases—particularly where nutrients are limited. We would also like to point out that such a review provides the platform of discussing individual mechanistic concepts. However, although a more individual approach in patient management is scientifically sound, the clinical reality is often different: individuals have a different genetic background, they have been exposed to different pathogens/commensals and may suffer from different infections—at the same time or in different orders that may shape the quality and quantity of immune responses. A more recent, prominent example [11] is the acquired capacity of the organism—in early life—to differentiate between commensal bacterial that colonize the skin versus potential pathogenic bacterial species, where antigen-specific regulatory T-cells (Tregs), tolerance mechanisms, and the IL-1-receptor–IL-1β axis play a prominent role. It is obvious that age, the country, nature of exposure to commensals and potential pathogens plays a pivotal role. The need to integrate these variations in different networks—and to extract biologically and clinically relevant concepts—is appreciated and fueled the discussion to obtain better models that integrate anatomical and biological diversity [12].
The study of metabolism has revealed six core biochemical pathways which impact on immune cell reprograming: glycolysis, tricarboxylic acid (TCA) cycle, fatty acid oxidation (FAO), fatty acid synthesis (FAS), pentose phosphate pathway (PPP), and amino acid synthesis (AAS) [13, 14]. Additional pathways have been described as modulators of the complexity of the immune response, mainly those leading to the biosynthesis of polyamines, cholesterol, hexosamines, and nucleotides [15]. The biochemical demands of each immune cell type are intrinsically liked to its function, especially those related to quiescence/memory and activation/proliferation [14, 16]. That said, different immune cell functions are, in fact, associated with distinct metabolic configurations: resting immune cells utilize energetically efficient processes such as the tricarboxylic acid (TCA), linked to the generation of ATP via oxidative phosphorylation (OXPHOS), whereas activated cells prefer glycolysis to generate adequate levels of energy storage to support survival and produce numerous biosynthetic intermediates to allow for cellular growth and proliferation [14]. CD8+ T-cells are believed to be dependent on FAO in regard to immune effector functions and tissue homing, yet more recent evidence suggests that memory T-cells may use alternate pathways for these immune effector functions [17–22]. This plasticity of immune cells modulates metabolic reprogramming from an inflammatory to anti-inflammatory or immunomodulatory phenotype or vice versa [7, 8, 23], which is of special interest for exploitation as an anti-tumor immune-based strategy [24]. In fact, cancer cells behave more like activated immune cells with increased biochemical demands and rely on glycolysis for survival [25–27].
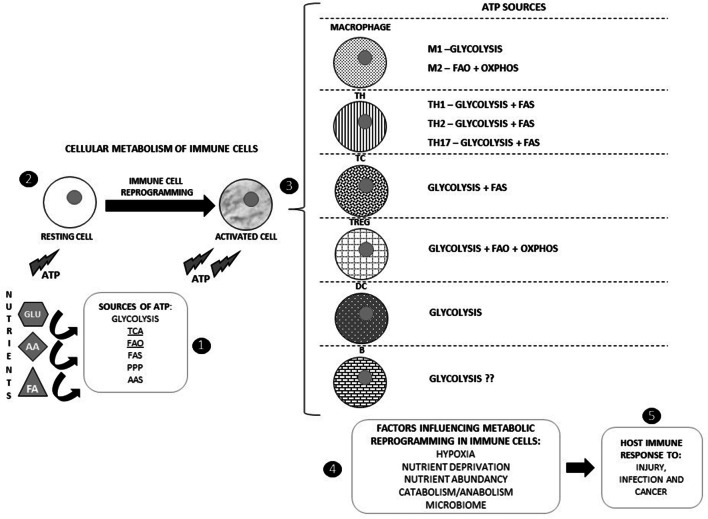
Nutrients play a pivotal role in the context of immune cell metabolic phenotypes, further supported (and influenced) by gut microbiota and gastrointestinal organs such as the pancreas, colon, and liver [28, 29]. Immunonutrition is a growing biomedical discipline [30] that aims to affect immune cell functions directly by delivering signaling metabolites by regulating nutrient availability [31]. Figure 1 summarizes different metabolic pathways and biological cell functions.
Fig. 1.
Cellular metabolism of immune cells and factors influencing metabolic reprogramming. (1) Six core metabolic pathways are involved in fueling cells for biological functions and differentiation, generating ATP from nutrients. (2) Resting immune cells usually rely on TCA and FAO for obtaining ATP and require immune reprogramming for activation. (3) Activated immune cells use different metabolic pathways to obtain ATP for proliferation. (4) Some external factors condition metabolic reprogramming of immune cells, such as hypoxia, nutrient deprivation and abundancy, catabolism, anabolism, and the microbiome. (5) These factors influence quality and quantity of immune reactivity in infection(s) and cancer. GLU, glucose; AA, amino acids; FA, fatty acids; TCA, tricarboxylic acid cycle; FAO, fatty acid oxidation; FAS, fatty acid synthesis; PPP, pentose phosphate pathway; AAS, amino acid synthesis
Integration of metabolism and immunity
Cellular metabolism of immune cells
As stated earlier, the main metabolic pathways involved in immune cell survival, proliferation, and activation are glycolysis, TCA cycle, PPP, FAO, FAS, and AAS (particularly those of glutamine, arginine, and tryptophan). Glycolysis occurs in the cytosol and generates two ATP molecules by substrate-level phosphorylation and pyruvate that enter mitochondria and are converted to acetyl–coenzyme A (acetyl CoA). Glycolysis is a relatively inefficient pathway for the generation of cellular ATP but is involved in several processes due to its capacity of being rapidly activated via the induction of key enzymes such as pyruvate kinase, glyceraldehyde 3 phosphate dehydrogenase, aldolase, and enolase [32, 33]. Cells requiring rapid production of ATP will switch to glycolysis as increased cell growth kinetics demand an equally (if not higher) turnover of biosynthetic intermediates [13, 34–36]. For example, glycolysis inhibition by modulation of pyruvate kinase M2 induces the polarization of macrophages towards an alternatively activated phenotype (M2 macrophages) in terms of gene expression, in addition to boosting IL-10 production [32, 37, 38]. It has been recognized that activating cell signals such as cytokines may lead to the generation of ATP, which will support the TCA cycle in providing intermediates for PPP, glycosylation reactions, and the biosynthesis of key biomass constituents like serine, glycine, alanine, and acetyl-CoA [13, 33]. This is true for macrophages (phagocytosis, inflammatory cytokine production) [39, 40], dendritic cells (Ag presentation) [41], as well as T-cells (effector cytokines, IL-17 for Th17) [42].
PPP is a metabolic pathway parallel to glycolysis. It generates NADPH, pentoses, and ribose 5-phosphate [43]. This pathway involves oxidation of glucose but is an anabolic pathway rather than a catabolic one [43]. NADPH is generated during the oxidative phase, whereas pentoses are produced during the non-oxidative phase of PPP. NADPH will, therefore, be used to generate ROS during respiratory burst and as a counterbalance to generate glutathione and other antioxidants. This is used by macrophages differently according to their phenotype [44, 45].
The TCA cycle (also known as the citric acid cycle or Krebs cycle) is a metabolic pathway for generating ATP and carbon dioxide through the oxidation of acetyl-CoA derived from carbohydrates, fats, and proteins [46]. Additionally, the TCA cycle also provides NADH to be used in diverse biochemical reactions while TCA cycle-derived citrate, uridine diphosphate N-acetylglucosamine (UDP-GlcNAc), itaconic acid, and succinate are important for immune cell physiology [46]. The TCA cycle operates both in normoxia and hypoxia [33, 38].
Fatty acid (FA) metabolism consists of both (energy-generating) catabolic and anabolic processes necessary for the synthesis of important biological building blocks such as triglycerides, phospholipids, secondary messengers (arachidonic acid and free fatty acids), hormones, and ketone bodies. When compared to other macronutrient classes, FAs generate the most ATP on an energy per gram basis when completely oxidized to CO2 and water by beta oxidation and the TCA cycle. Many immune cells that are not inflammatory in nature and exhibit increased cellular lifespans (M2 macrophages, regulatory T-cells (Treg), memory CD8+ T-cells) have been demonstrated to rely on FAO, as previously mentioned [20, 47, 48]. Nevertheless, FAS seems to positively regulate the generation and function of pro-inflammatory innate and adaptive immune cells [49]. The efficacy of lipid oxidation for energy generation and the necessity of lipid synthesis for biosynthesis and cell growth suggest that pro-inflammatory and regulatory immune cells show fundamental differences in their reliance on ATP generation for growth [20].
Glutamine, arginine, and tryptophan are the most well-studied amino acids affecting the immune system. Insufficient supply of glutamine has been related to increased mobilization from muscles and low plasma levels [50, 51]. Human studies have demonstrated that these low plasma levels of glutamine are related to reduced B-cell differentiation [52], decreased IL-2 production (and IL-2R expression), downregulation of HLA class II expression on and reduced antigen presentation by macrophages [51, 53]. Glutamine can be used by macrophages for NADPH production [53]. Murine macrophages and neutrophils involved in pinocytosis have, in fact, been shown to prefer/require NADPH supplied by glutamine metabolism rather than PPP, since glucose supplied by the latter pathway is used for fat storage [54]. In murine T-cells, glutamine is used as a resource in nucleic acid synthesis and as an energy source [55]. Pertaining to arginine metabolism and immune cells, arginase-1 is responsible for the breakdown of arginine to ornithine and plays a role in the immune function regulation of activated T-cells through depletion of arginine in the local microenvironment (as controlling arginine bioavailability leads to control of nitric oxide production), which has been described in experimental models of cancer and tuberculosis [56–58]. Arginine depletion has been related to T-cell suppression, mainly by reduced expression of the CD3-ζ chain (and concomitant lower expression of the TCR complex) as well as downregulation and subdued enzymatic activity of the cyclin D3/CDK4 complex which is known to regulate cell cycle progression [59, 60]. Interestingly, elevated levels of arginase-1 have been found in the splenocytes of tumor-bearing mice [61]. Moreover, cancer and postoperative patients present with a lack of the CD3-ζ chain, dysfunction and reduced number of T-cells, and increased arginase-1 activity [62–64]. Idoleamine-2,3 dioxygenase (IDO), which oxidatively degrades tryptophan in the kynurenine pathway, has been considered a key enzyme in host immune function [65]. The properties exhibited by some innate immune cells, i.e., human CD123+ DC subset (CD11c+ CD8α+ DC subset in mice) and macrophages to induce IDO, have been demonstrated to be responsible for the modulation of not only T-cell function mainly via tryptophan depletion but also IDO-cytotoxic metabolites [65–67], although the latter mechanism requires further elucidation.
Aerobic glycolysis appears to be a characteristic feature of many rapidly dividing cells, including cancer and immune cells, even when sufficient oxygen is present to support OXPHOS [8, 35]. In proliferating cells, the increase in lactate production may result from the contribution of growth factor-mediated increases in glucose uptake, increased ATP consumption associated with cell growth, and low NAD+/NADH ratio secondary to oxidative biosynthesis [68–70]. The advantage of this metabolic phenotype in proliferating cells is to help meeting the biochemical requirements of biosynthesis and allow differentiation [71]. Aerobic respiration produces a larger fraction of cellular ATP from mitochondrial OXPHOS, while glycolytic cells produce relatively more ATP from glycolysis [72]. Some immune cells transition between OXPHOS and glycolytic metabolic phenotypes over the course of an immune response; manipulation of this dichotomy can have an effect on the regulation of host immunity [73]. Increased glycolysis (the Warburg effect) has been described as a feature of inflammatory as well as cancer cells (for adaptation [74]), whereas cells involved in immunoregulation or in the resolution of inflammation display FAO and an intact TCA cycle as hallmarks of their metabolism [33, 75], inevitably affecting their cellular phenotypes as will be discussed in the following subsection.
Systemic metabolism and immune cell ontogeny
Macrophages and metabolism
Macrophages have several functions in tissue homeostasis and inflammation, with their metabolic characteristics reflecting functionality [76]. Immunometabolism has been recently studied in macrophages, as metabolic pathways not only provide energy but also regulate macrophage phenotype and function [77, 78]. In this regard, comparison between classically activated, pro-inflammatory macrophages (M1) and alternatively activated, anti-inflammatory macrophages (M2) with reparative capacity, reflecting functional polarity, is of especial relevance [73, 76]. The expression of toll-like receptors (TLRs) on the surface of macrophages promotes a M1 phenotype (mainly TLR2 and TLR4), whereas IL-4 and efferocytosis promote a M2 phenotype [79, 80]. These two phenotypes are distinct in their function as well as the preferential biological mediators produced. M1 macrophages are known for their ability to produce pro-inflammatory cytokines (IL-1β, IL-18, IL-12, TNF-α, IL-6) and reactive oxygen species (ROS), while M2 macrophages release anti-inflammatory cytokines (IL-4, IL-10, TGF-β) and promote angiogenesis and fibrosis [73, 81].
The differences between the M1 and M2 macrophage phenotypes are also evident in their cellular metabolic profiles. In general, M1 macrophages are highly glycolytic, whereas M2 macrophages use FAO metabolism and OXPHOS [37, 49, 80, 82]. In M1 macrophages, glycolysis would allow for rapid ATP production to fuel activation during acute inflammation [80, 82], while in M2 macrophages, OXPHOS occurs during the lengthy process of resolving tissue inflammation and repair or in promoting anti-parasite immunity [80, 82, 83].
Metabolomic and transcriptomic data have provided useful insights into revealing the metabolic changes in macrophage polarization. In fact, the presence of two breaks in the TCA cycle of M1 macrophages has been described [73], thereby suggesting an “interrupted” TCA cycle for this phenotype. One of the breaks was described at the isocyanate dehydrogenase step and the other after the succinate step, with evidence for a variant of the pathway: the aspartate-arginosuccinate shunt [41, 84]. This disruption in the TCA cycle in M1 macrophages leads to the accumulation of citrate and nitric oxide (NO) production [41]. Jha and colleagues showed that the TCA cycle in M1 macrophages is rather a fractionated than an undisrupted cycle [73]. Interestingly, inhibition of aspartate aminotransferase (a key enzyme in the TCA shunt pathway) suppressed IL-6 and NO production, revealing the importance of the arginosuccinate shunt for M1 macrophage function [73]. M1 macrophages convert arginine into NO through inducible NO synthase (iNOS) activity [85], while in M2 macrophages, arginine is metabolized by arginase-1 [86]. Despite the core belief that glycolysis is merely associated with inflammation and OXPHOS with anti-inflammatory responses, it is now accepted that this dogma is more fluid that previously perceived and demands revision [39, 77, 79, 80]. Macrophage metabolism remains a very interesting field especially in modalities with an urgent need for novel therapeutic targets, i.e., cancer. This subject will be discussed later.
T and B cells and metabolism
Oxidative metabolism is preferred by resting lymphocytes, where glycolysis or aerobic glycolysis meets their cellular demands after stimulation [87]. Resting precursor T-cells require energy and active replenishment of basic biological building blocks for survival and migration as they continually migrate through lymphoid tissue for immune surveillance [88]. These ATP-intensive functions are mainly achieved by FA β-oxidation as well as pyruvate and glutamine oxidation via the TCA cycle [87]. It is also known that mature resting T-cells exhibit a dynamic regulatory pattern rather than fixed metabolism [89].
During activation, and to sustain rapid clonal proliferation, the increased metabolic needs of T-cells are met by converting glucose to lactate through aerobic glycolysis—that increases glucose and glutamine metabolism while decreasing lipid oxidation as cell proliferation requires the activity of mammalian target of rapamycin (mTOR)-dependent pathways [55, 90]. It is known that OXPHOS can still be used by activated T-cells as a source of energy; however, strong evidence supports the induction of the glycolytic pathway as a lineage-decisive event for Th1, Th2, and Th1 development [89]. These lineages display a strong bias towards glycolysis over mitochondrial metabolism; Th17 development, for instance, involves hypoxia-inducible factor 1 alpha (HIF-1α), which is an oxygen-sensitive transcription factor also responsible for glycolytic gene expression regulation in Th17 cells [47, 91]. Conversely, induced Treg lineage displays a mixed metabolic signature involving glycolysis, lipid oxidation, and OXPHOS [91]. Also, blocking glycolysis during Th17 differentiation may favor Tregs over Th17 development [91], which may be detrimental in early stages of infections [92, 93] and potentially in patients with cancer [94, 95]. Interestingly, decreased T-cell proliferation and activation, T-cell anergy or cell death may be observed if inadequate nutrient supply or metabolic inhibition occur during T-cell ontogeny [89].
Much less is known about how metabolism directs the fate of normal B cells. As these cells develop into specialized antibody-secreting plasma cells and memory cells [9, 96], specific metabolic and nutritional requirements may be at play. Anergic human peripheral blood B-cells, following LPS stimulation, have been shown to only moderately increase their glycolytic rate, while unstimulated B-cells exhibited a balanced upregulation of lactate production and aerobic glycolysis concomitant with a steady increase of glucose transporter 1 (Glut1) expression following LPS or B-cell receptor (BCR) activation [97]. Indeed, BCR-mediated B-cell proliferation is stunted following inhibition of glycolysis [96], reminiscent of the scenario in activated T-cells. How B cell subsets are metabolically regulated in different human diseases and stages warrants further investigation using appropriate clinically welldefined samples.
Dendritic cells and metabolism
The activation of DCs implies phenotypic, secretory, and functional modifications that cause an increase in glucose uptake and lactate production; however, a metabolic reprogramming from OXPHOS towards glycolysis occurs after DC activation by TLRs [7, 98, 99]. During cellular activation, ATP is generated by OXPHOS, and therefore, lactate production does not reflect commitment to the Warburg effect [100]. Moreover, the need for citrate by activated DCs for fueling FAS involved in ER and Golgi apparatus turnover seems to be biochemically supported by glycolysis [100]. This glycolytic metabolism is dependent on the activation of HIF-1α and PI3K/Akt pathways and indicates a possible role for mTOR downstream of PI3K/Akt [99, 101], whereas induction of the OXPHOS mediator AMPK antagonizes the glycolytic pathway, inhibiting DC maturation [102]. Nevertheless, DCs with immunogenic (promoting effector T-cells) and tolerogenic (promoting suppressive Tregs) functions have different metabolic profiles that reflect their function [103]. Tolerogenic DCs are predominantly catabolic and rely on OXPHOS and FAO for ATP production, with low glycolytic potential [103]. In contrast, immunogenic DCs exhibit anabolic metabolism and are mainly glycolytic, with reduced OXPHOS and FAO. Anabolic demands of DC activation require rapid induction of glycolysis as an integral component of TLR signaling, where the TBK1, IKKɛ, and Akt kinases seem to be essential for engaging the mitochondrial glycolytic enzyme HK-II [104]. The rapid loss of mitochondrial OXPHOS by TLR-triggered inflammatory DCs may be explained by the NOS-2-mediated NO production, which accompanies the glycolytic switch that is able to direct inhibit the mitochondrial ETC in an autocrine as well as paracrine manner [105]. Conventional DCs, on the other hand, do not express NOS-2 nor are they amenable to NOS-2 induction by TLRs or inflammatory cytokines [105]. An interesting insight into energy and mitochondrial homeostasis in DC, supporting immune activation, was highlighted by Thwe et al. in mouse DC cultures [106]. In their research, early glycolytic metabolism was observed during DC activation, supported by utilization of intracellular glycogen reserves [106]. Moreover, the authors also saw that glycogen-derived carbons preferentially contributed to the TCA-dependent citrate pool, when compared to glucose directly catabolized by mouse DCs [106]. IDO1 phosphorylation and subsequent cellular signalling in CD11c+, IL-4, IFN-γ or TGF-β activated DCs has been shown to be dependent on prior expression of Arg1 and Arg1-dependent production of polyamines [107]. The latter are either produced by DCs or released by Arg1+ myeloid-derived suppressor cells (MDSCs) and may skew DCs towards an IDO1-dependent, immunosuppressive phenotype (via Src kinase activation) [107]. DC metabolism and its potential edit the quality and quantity of immune responses are likely to influence the design of immunotherapeutic strategies.
Cancer, the tumor microenvironment, and metabolism
Immune cell competition for nutrients
In a more molecular perspective, we can objectify the relationship between nutrients and immune cells through the role of the former in the control of cellular responses of the latter. In fact, there are immune microenvironments where some degree of nutrient limitation is present, which provide the opportunity to study changes in signal transduction driven by nutrients and to understand the relevance of nutrient availability in regulating immune responses (elegantly reviewed in [108]). As the concept of unequal nutrient availability to immune cells is emerging [6], competitive nutrient uptake in immune microenvironments seems to be of major importance for immune responses, hinting at nutrients’ role in regulating the fate of immune cells. As will be discussed later, competition for nutrients can be observed in the tumor microenvironment (TME) and at sites of pathogen infection [108]. Solid tumors exhibit an increased demand for glucose to support growth and proliferation, despoiling extracellular levels of glucose by increasing blood supply into the TME via neovascularization [108]. There is also evidence that in some tumors, competition for glutamine may lead to limiting glutamine resource levels in the TME. This restriction of glucose and glutamine supply in the tumor seems to inhibit immune cell infiltration, as observed in local resistance to to adoptive T-cell therapy [108, 109], which will be revisited later in this review. A similar competition for nutrients has been observed in virus-infected cells, which are reprogrammed for increased glucose metabolism, glycolysis, and glutaminolysis (glutamine breakdown) and decreasing extracellular concentrations of these nutrients in the surrounding microenvironment [108, 110, 111].
Role of nutrients metabolism in the TME
The metabolism of proliferating cells is quite different from that of non-proliferating ones (which obtain energy from OXPHOS) [112]. Proliferating cells, like cancer cells, show increased requirements of energy and nutrients for rapid growth and dissemination (metastasis) and exhibit an increase in the uptake of glucose, amino-acids, fatty acids, minerals, and vitamins [113]. In fact, a central feature of nearly all cancers is impaired cellular energy metabolism [112]. To respond to the high energy demands of active proliferation, cancer cells convert great amounts of glucose into pyruvate (aerobic glycolysis), in a low-efficiency pathway – albeit their dependence on glucose for survival and growth [114]– thus the Warburg effect [115, 116]. Cancer cells use glucose catabolism via glycolysis as a major energy-generating pathway, generating several biosynthetic molecules and NADPH. Depriving cancer cells of glucose can, in fact, promote mutations in the KRAS pathway which, in turn, induces increased sensitivity to glucose in transformed cells, leading to GLUT1 upregulation and enhanced glucose uptake from the immediate microenvironment [117]. The Warburg effect can be described as a state of mitochondrial dysfunction, as cancer cells are unable to undergo mitochondrial OXPHOS [112]. Metabolic reprogramming of cancer cells can be viewed as an enhancer of adaptation to intratumoral metabolic stress and immune surveillance, contributing to maintaining “cancer stemness” [118]. This has been considered indispensable and to the advantage of the pathological biological processes occurring in cancer cells [119].
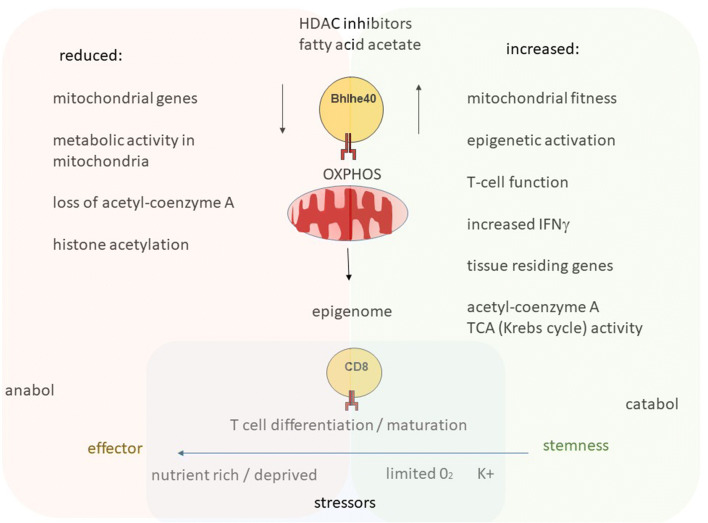
The TME is also characterized by extracellular acidosis resulting from lactate accumulation [119–121]. This is due to the synergy between HIF-1α and Myc in promoting expression of glycolytic enzymes driving glucose influx and lactate production in response to the (i) poor clearance of acid accumulation outside the TME (generating a low pH within the TME) and (ii) upregulation of monocarboxylate transporter (MCT) 4, favoring the migration of extracellular lactate to the extracellular matrix [114, 119]. MCT4 upregulation is especially relevant, as it is transcriptionally upregulated by the hypoxia-driven HIF-1αε enzyme, and tumor cells usually localize in hypoxic environments [122]. While not applicable to the entire TME, there may be distinct hypoxic areas due to aberrant neovascularization and subsequent impaired access to nutrients, metabolic changes that may promote disease progression [27]. Vascular endothelial growth factor (VEGF), the cardinal mediator of angiogenesis, is aberrantly expressed in several cancers and is clinically targeted cancers of different histology [123]. Nevertheless, it has been shown in patients with breast cancer that VEGF blockade with bevacizumab—under hypoxic conditions—leads to reoxygenation of the TME but also promotes acute hypoxia in treatment-resistant patients [124]. Anti-angiogenic therapy would deprive the tumor of nutrients necessary for survival—which would inevitably also affect the immune cell compartment therein. In fact, to escape from anticipated senescence or death, tumor cells engage autophagy to survive the potentially hostile TME [125, 126]. Thus, overexpression of GLUT and downstream glycolytic enzymes (pyruvate kinase isozymes M2, serine hydroxymethyltransferase, carbonic anhydrase 9) [118] has been observed in several cancers [127–131]. Oncogenes (Akt, PI3K, mTOR, Ras, Raf) [132] and loss of tumor suppressor genes (VHL, PTEN, p53) also contribute to the increasing growth and metabolic activity of tumor cells [132]. Glucose can either be used in glycolysis or metabolized by PPP, promoting production of glutathione, FAs, sterols and nucleic acids, which are considered relevant for reducing oxidative stress and increasing DNA repair in cancer cells, conferring resistance to cancer treatments [133, 134]. Figure 2 presents a schematic compilation of stressors in TME.
Fig. 2.
Stressors, e.g., (increased) potassium, reduced oxygen and nutrient access in tissue environment, act on T cells (Li et al., Immunity, 51, 491–507, 2019). One of the key factors modulating tissue resident T cells’ activity is the transcription factor Bhlhe40 (top) in infections and cancer. Reduced Bhlhe40 leads to reduced capacity to contain infections or cancer in preclinical models, in part via effecting mitochondrial activity—that impacts on the T-cell epigenome. OXPHO (oxidative phosphorylation) and TCA activity are associated with memory immune cells. HDAC inhibitors and the fatty acid acetate replenish mitochondrial function and cytokine production. This is a simplified sketch and clinical outcomes of HDAC treatment that may be different depending on the pathogen, previous exposures of immune cells to drugs, viral and bacterial species, as well as the nominal T-cell receptor repertoire available in the microenvironment
The TME also hosts tumor-associated macrophages (TAMs), cancer-associated fibroblasts (CAFs), and endothelial cells involved in tumor stroma formation [135]. Evidence suggests that TAMs and CAFs interact in a reciprocal manner [136, 137], have a role in tumor progression [138, 139], and are associated with cancer invasion and metastasis [135, 140]. Also, the TME is infiltrated by T-cells (tumor-infiltrating T lymphocytes, TILs), whose functions are impaired, often in association with the volume of the tumor lesion. Generally, TILs are considered a pro-inflammatory and/or cytotoxic population of T-cells able to recognize tumor antigens and, therefore, mediate tumor regression, constituting a critical clinical biomarker of prognosis [141, 142]. The complex cellular composition of the TME, along with the hostile conditions of nutrient deprivation caused by intense energy requirements of cancer cells, imposes an important question: how do cancer cells obtain enough “food” in these adverse conditions? This appears to be achieved by despoiling neighbor cells of energy and nutrients to survive and proliferate [143]. Some of these afore-mentioned nutrients, i.e., amino acids, acetate, and lactate are used as alternative fuels by cancer cells and are summarized in Table 1.
Table 1.
Non-glucose nutrients used by transformed cells as alternative fuels
| Non-glucose nutrients | Essential uses by cancer cells for survival and proliferation | References |
|---|---|---|
| Glutamine |
Carbon and nitrogen source c-Myc activation Inhibition of Akt-mediated glycolysis Lipid biogenesis by direct supply of acetyl-CoA in hypoxic conditions or in presence of IDH1 mutation Redox homeostasis |
[374–381] |
| Asparagine |
Regulation of mTORC1 activation and autophagy Regulation of serine uptake and metabolism gene expression Exchanging with extracellular essential amino acids |
[382, 383] |
| Leucine | Autophagy regulation | [384] |
| Arginine | Maintenance of viability by stability of checkpoints (mainly G1 checkpoint) | [385] |
| Methionine | Influence epigenetic state and promotion of tumor initiation | [386] |
| Cysteine |
Reduction of cell death by oxidative stress ROS detoxification |
[387, 388] |
| Serine and glycine |
Fueling one-carbon metabolism Activation of PKM2, supporting aerobic glycolysis and lactate production |
[388, 389] |
| Acetate | Activation into acetyl-CoA, used as a crucial central metabolite for TCA cycle, as a source of acetyl groups used for DNA acetylation modifications and for regulation of histone acetylation and gene expression program | [390–392] |
CoA coenzyme A, mTORC1 mammalian target of rapamycin complex 1, PKM2 pyruvate kinase muscle isozyme M2, ROS reactive oxygen species, TCA tricarboxylic acid
Some of these nutrients become crucial for cancer cells, which sometimes exhibit some degree of “addiction” [144, 145]. To prevent inadequate tumor perfusion due to low nutrient availability, cancer cells resort to multiple scavenging strategies to take up nutrients from cells in the immediate microenvironment [146]. These strategies include integrin-mediated scavenging, receptor-mediated scavenging of albumin, and scavenging via micropinocytosis and entosis [147], as a way of obtaining final products for ATP generation and anabolism [146].
The despoiling of neighboring cells nutrients is of special concern for TILs, which is evidenced by the negative impact by the TME on TIL metabolism and its contribution to functional exhaustion of TIL, also marked by the induction of programmed cell death 1 (PD-1) expression by T-cells [148]. PD-1 is a co-inhibitor that blocks CD28-mediated activation of the mTOR pathway and reduces glycolysis but enhances FA metabolism [149]. The increase in PD-1 may facilitate the metabolic switch of energy production to TCA cycle and OXPHOS, which is observed in continuous antigen-driven stimulation during chronic infections [150]. In cancer, therapeutic targeting of PD-1+ (immunologically “exhausted”) TIL has revolutionized oncotherapy and established the newly coined field of immuno-oncology [151]. Additionally, TILs must deal with the hostile environment of glucose deprivation and hypoxia, which alters their anti-tumor activity. The absence of glucose has profound effects on CD8+ T-cells, as this nutrient is crucial for the differentiation of naïve CD8+ T into effector subsets [152]. Although differentiation may still occur in this situation, effector clones present reduced effector functions [153, 154]. In this context, TILs have additional challenges as the TME is a glucose-deprived environment, and regardless of high expression of GLUT1 by TILs, tumor cells are more efficient at consuming glucose [153]. Also, high concentrations of lactate in the TME lowers pH, which inhibits PPK and consequently reduces TILs glycolysis [155]. Thus, hypoglycemia in the TME leads to reduced glycolysis, leaving TILs relying on OXPHOS. Further challenges arise with oxygen restriction; TILs face severe hypoxic conditions when infiltrating tumors from well-oxygenated peripheral blood vessels [148]. In this condition, HIF-1α is activated and performs two important functions: it adjusts metabolism by enhancing TIL glycolysis due to lactate dehydrogenase A induction and increases PDK1 expression preventing OXPHOS [156–158]. Consumption of glucose is, therefore, increased to allow glycolysis to proceed. It has been demonstrated that in hypoxic conditions, T-cell activation is inhibited, with their proliferation and capacity to cytokine production reduced [159]. In fact, oxygen deprivation negatively impacts metabolism and function of TILs, as hypoxia is immunosuppressive and induces ROS accumulation in association with the apoptosis of activated TILs [160]. Thus, hypoxia in the TME inhibits OXPHOS by TILs and reprograms their metabolism to use glycolysis; however, most solid tumors combine both hypoglycemia and hypoxia to render TILs inactive in the TME. How TILs survive in these adverse conditions is still being investigated. It has been proposed that TILs may resort to using ketone bodies, similar to other cells under the same conditions [148, 161]. What seems certain is that these conditions are unfavorable for TILs – impairing immune cell function, immune exhaustion and reducing anti-tumor reactivity. As cancer cells also rely on alternative nutrients for their metabolism, they affect not only the use of glucose by TILs but also other nutrients, i.e., amino-acids and FAs [162, 163]. Overall, low availability of these nutrients impairs both differentiation and cytokine production, which in turn reduces effector cytotoxic functions [164], as summarized in Table 2.
Table 2.
Competition between cancer cells/TAMs and T-cells for non-glucose nutrients: effect of nutrient despoiling on cellular functions
| Deprived by cancer cells and/or TAMs | Effect on T-cells | References |
|---|---|---|
| Glutamine | Reduced proliferative capacity and cytokine production | [55, 162] |
| Arginine |
Reduced effector function and survival Impaired memory subsets differentiation Impaired TCR |
[57] |
| Cystine | Reduced proliferative capacity and cytokine production | [162] |
| Tryptophan |
Downregulation of CD3-ζ chain in CD8+ T cells Inhibition of Th17 differentiation |
[393–395] |
| PUFAs | Absence of memory | [17] |
PUFAs polyunsaturated fatty acids, TAMs tumor-associated macrophages, TCR T cell receptor
Nutrient availability also impacts metabolic pathways in TAMs, which affects their functions as well as TIL immune surveillance competence. TAMs display different phenotypes which go beyond the conventional M1/M2 dichotomy. Ultimately, five TAM phenotypes are present in the TME: activated (IL-2+, MCHIIhi, iNOS+, TNF-α, CD80/CD86), immunosuppressive (Arg1+, MARCO+, IL-10+, CCL22+), angiogenic (VEGFR1+, VEGF+, CXCR4+, TIE2+), invasive (WNT signaling, EGF+, MMP9, CCL3), and metastasis-associated (VEGFR1+, VEGF+, CXCR4+, CCR2+) macrophages [165]. The nature of the TME may edit TAMs in order to compete for nutrients, mostly glucose, which reprograms TAMs towards a phenotype consistent with tumor growth, progression and metastasis [23, 166, 167]. The central features of this metabolic reprogramming have been identified as activation of glycolysis, modifications of TCA cycle that include fueling with alternative non-glucose nutrients, FA synthesis, and altered nitrogen cycle metabolism. In cell cultures, cancer-cell stimulated macrophages have exhibited upregulation of glycolysis, increased expression of hexokinase-2, activation of AKT1/mTOR, and increased lactate receptors. Upregulation of REED1, with consequent inhibition of mTOR and glycolysis, has been observed in TAMs during hypoxic conditions. This can be linked to an augmented angiogenic response and the development of vascular leakage. Lipids and amino acids have important roles in sustaining the altered TCA cycles of TAMs. TAMs exhibit increased FA biosynthesis, uptake and storage (with important intensification of arachidonic acid metabolism), while glutamine seems relevant for macrophages polarization, especially towards a M2-like phenotype although the role of different amino acids in TAMs metabolism remains poorly studied [168, 169]. Arg1 is upregulated in TAMs, consuming arginine for NO production and protein synthesis (reviewed in [170]). In terms of lipids, polyunsaturated (PU) FA linoleic acid (18:3) and saturated FA (SFA) stearic acid (18:0) have been considered relevant for macrophage polarization and function in TME. In fact, linoleic acid-enriched, as opposed to stearic acid-enriched TAMs, appear to exhibit cytotoxicity against some cancer cells [168]. Thus, TAMs also compete with TILs for nutrients, functionally impairing the latter (Table 2). MDSCs also play relevant roles in the TME and in modulating the efficacy of anti-cancer therapies (recently reviewed by Yan et al. [171]). Tumor-infiltrating MDSCs, as opposed to their circulating (peripheral blood) counterparts, appear to have preference for FAO as energy source in comparison, suggesting that they undergo metabolic reprogramming—like macrophages—in the TME [171]. Also, the switch from glycolysis to FAO demands an increase in lipid uptake that is associated with tumor progression and suppression of T-cells [171]. Targeting lipid metabolism in MSDCs may, therefore, be a potential target in anti-cancer strategies and warrants further investigation.
All aspects of the TME, including empowering anti-cancer ability of TILs, have been considered potential therapeutic targets for more rationally designed cancer treatments. For example, metformin treatment may improve memory CD8+ T-cell responses by targeting AMPK (inducing activation) as well as mTOR (inhibitory effect leading to c-Myc and HIF-1α downregulation) [17, 172, 173], which manifest in improved FA metabolism in CD8+ T-cells leading to memory generation. Table 3 shows a non-exhaustive list of approved drugs and candidates in clinical trials targeting some TME characteristics as well as immunometabolism for patients with solid cancer as a paradigm how these repurposed drugs can be used in the treatment of patients with infectious diseases (reviewed for pulmonary infections in reference [174]).
Table 3.
Examples of approved drugs and candidates in clinical trials targeting some TME characteristics and immunometabolism in solid tumors
| Target | Drug | Mechanism | Type of cancer | Situation (Ref.) |
|---|---|---|---|---|
| Hypoxia and acidosis | Panzem (2-methoxyestradiol, 2ME2) + temozolomid | Inhibition of HIF-1α and HIF-2α protein synthesis | Recurrent glioblastoma multiforme | Phase 2: NCT00481455 |
| Topotecan | Inhibition of HIF-1α expression, angiogenesis, and tumor growth in human xenograft models | Ovarian and small cell lung cancers | Phase 1: NCT00117013 [396] | |
| Metformin | Oxygen concentration improvement in cancer tissue | Head and neck SCC cancer | Proof of principle: NCT03510390 (completion for 12/2020) | |
| Everolimus (RAD001) | Inhibition of tumor cell HIF-1 activity, VEGF production, and VEGF-induced proliferation of endothelial cells | Advanced renal cell cancer | Phase 4: NCT01206764 (completed, first data posted 24/06/2019) | |
| Everolimus (RAD001) + lenvatinib | Inhibition of tumor cell HIF-1 activity, VEGF production, and VEGF-induced proliferation of endothelial cells | Renal cell carcinoma | Phase 2: NCT03324373 (completion for 4/2021) | |
| Digoxin (DIG-HIF1) |
Inhibition of VEGFR1,2 and 3; FGFR1, 2, 3, and 4; PDGFRα, KIT, and RET Blockade of HIF-1α |
Operable breast cancer | Phase 2: NCT01763931 (completion for 7/2020) | |
| Angiogenesis | Pazopanib | Inhibition of VEGFR, PDGFA and -B receptors and c-Kit | Advanced renal cell carcinoma and soft tissue sarcoma | Approved for clinical use |
| Sunitinib | Inhibition of c-kit activity | Several | Approved for clinical use | |
| Sorafenib | Inhibition of tyrosine kinase and Raf kinase activity | Several | Approved for clinical use | |
| LY01008 + bevacizumab | Anti-VEGF; inhibition of neovascularization | Non-small cell lung | Phase 3: NCT03533127 (completion for 12/2020) | |
| Cediranib | Anti-VEGF; inhibition of neovascularization | Ovarian | Phase 3: NCT03278717 (completion for 12/2023) | |
| Ramucirumab (LY3009806) | Anti-VEGF; inhibition of neovascularization | Gastric and gastroesophageal cancers | Phase 3: NCT02898077 (completion for 8/2020) | |
| Everolimus (RAD001) | Inhibition of VEGF production, and VEGF-induced proliferation of endothelial cells | Advanced renal cell | Phase 4: NCT01206764 (completed, first data posted on 24/06/2019) | |
| Aflibercept | Anti-VEGF; inhibition of neovascularization | Large choroidal melanoma |
Phase 3: NCT03172299 (completion for 12/2024) Phase 3: NCT02885753 (completion for 6/2023) |
|
| TAMS, MDSCs | Pexidartinib | Inhibition of CSF1R, recruitment blockade | Giant cell | Phase 3: NCT02371369 (completion for 12/2019) |
| PDR001 + MCS110 | Inhibition of CSF1R, recruitment blockade | Gastric | Phase 2: NCT03694977 (completion for 12/2019) | |
| ARRY-382 + pembrolizumab | Inhibition of CSF1R, recruitment blockade | Advanced solid | Phase 1b/2: NCT02880371 | |
| Emactuzumab | Anti-CSF1R, recruitment blockade | Advanced squamous cell | Phase 2: NCT03708224 (completion for 11/2025) | |
| Cabiralizumab | Anti-CSF1R, recruitment blockade | Metastatic pancreatic | Phase 2: NCT03697564 (completion for 12/2021) | |
| Biliary tract | Phase 2: NCT03768531 (completion for 1/2023) | |||
| Vemurafenib | Inhibition of BRAF kinase, recruitment blockade | Metastatic melanoma | Approved for clinical use [397] | |
| Aerobic glycolysis | Dichloroacetate | Inhibition of glycolysis, by PDK inhibition | Head & Neck SCC | Phase 2: NCT01386632 (completion for 10/2019) |
| AZD3965 | Inhibition of glycolysis, by MCT1 inhibition | Several advanced | Phase 1: NCT01003769 (completion for 6/2020) | |
| Amino acids | CB-839 | Inhibition of glutamine metabolism | Renal cell carcinoma, melanoma, and non-small cell lung cancer | Phase 1: NCT02771626 (concluded 6/2019) |
| Solid tumors | Phase 1: NCT02071862 (completion for 9/2019) | |||
| ADI-PEG | Degradation of circulating arginine | Tumors requiring arginine | Phase 1: NCT02029690 (completion for 5/2020) | |
| Hepatocellular carcinoma | Phase 1: NCT02102022 (completion for 10/2020) |
BRAF proto-oncogene B-Raf, CSF1R colony-stimulating factor 1 receptor, HIF hypoxia-inducible factor, MCT monocarboxylate transporter, PDGFA platelet-derived growth factor subunit A, PDGFR platelet-derived growth factor receptors, PDK pyruvate dehydrogenase kinase, RET RET proto-oncogene, VEGF vascular endothelial growth factor, VEGFR vascular endothelial growth factor receptor
Nutritional status, nutrient metabolism, and susceptibility to infection
Infections and parasitic diseases are the most common cause of death [175] in low-income countries, where malnutrition appears to be the precipitating factor [176]. Children and adolescents with lower BMI-for-age, as well as underweight adults, are at higher risk for infections and infection-associated morbidity and mortality [175–177], e.g., for malaria and pulmonary tuberculosis [178, 179]. Nutrition, infection(s), and subsequently altered immune function(s) affect each other [180]: changes in nutritional status (especially energy and protein depletion) are associated with alterations in the systemic metabolism that affects immune cell regulation, immune competence, and disease susceptibility. Host factors associated with infectious diseases lead to increased metabolism (catabolism) paired with decreased appetite and subsequently to malnutritional [179]. However, the nutritional status favors maintenance of T-cells with “stem cell-like features” that are important for long-term immune memory [181].
Although malnutrition remains a concern in low-income countries, it is also present—in a “different format” in higher-income countries. Economic disparities within a country (poverty, malnutrition, and obesity) represent a major challenge for twenty-first century societies and health professionals. Obesity is no longer considered to be a consequence of the abundance of food, but rather a result of poor education, lower income, and access to affordable high-energy-dense food along with the lack of physical activity [182] and, possibly, the composition of the microbiome [183]. In general, changes in the nutritional status of populations shape immune competence, the ability to resist, fight off infections and to productively respond to vaccinations [184–186].
The relationship between malnutrition and immunity will be discussed in detail below; immunometabolism and the implications for protective immune responses and host-directed therapies have been extensively reviewed in Rao and coworkers [174].
Nutritional immunology
Definition and historical aspects
Beginning with J.F. Menkel’s notes on thymic function and adequate nutrition in the nineteenth century, malnutrition has been related to alteration(s) in organs of the immune system [187]. However, the publication Interactions of nutrition and infection by Scrimshaw et al [188] in 1959 postulated the first steps pertaining to nutritional immunology. Almost a decade later, the World Health Organization (WHO) released the first edition of an extended monograph with a similar sounding concept [189]. The name of Professor Nevin Scrimshaw (1918–2013) will, thus, remain forever associated with nutritional immunology, not only due to these two publications but also owing to other works devoted to understanding the interrelationship between nutrition and infection, and the evidence of higher mortality in malnourished populations [190–198]. Since the 1969 WHO monograph, the hallmark of nutritional immunology as a discipline has been the recognition that almost any specific and sufficiently severe nutritional deficiency can interfere with immunological functions, affecting infectionassociated morbidity and mortality [191, 199].
The synergistic relationship of nutrient reserves and immune responses
Early observations following the advent of nutritional immunology showed that malnourished patients were more susceptible to infection and presented with an increased risk of mortality due to sepsis [200]. In fact, the impact of malnutrition on immune defense constituted, for many years, the core of and justification for immunonutrition in immunosuppressed patients—inclusively referred to as nutritionally acquired immune deficiency syndrome. The new challenges faced by humanity, mainly overnutrition, aging, and stressors, are redirecting research in the field of nutritional immunology and rewriting the applications of immunonutrition.
Nutrition and immunology have a multi-level synergistic interaction that has been described in conjunction with the 4 “Is”—Infection, Immunity, Inflammation, and Injury [31]. However, as stated above, the relationship between nutrition and immunology was first confined to the effect of poor nutrition due to the risk of infectious diseases as well as recovery after a bout of infection [191]. This was understandable in a context were nutrition was seen merely as protein and energy, and nutritional problems as “protein-energy” malnutrition (PEM). In fact, malnutrition was always a considerable clinical issue at hospital admission. Epidemiological evidence that malnutrition screening at admission and nutritional intervention during hospitalization positively impact patients’ quality of life, reduce hospital stay, increase resistance to infection, and reduce costs have been instrumental recognizing the impact of nutrition in preventing and recovering from infection [201, 202]. The relationship between PEM and infection, especially the impact on immune cells and non-cellular components are summarized in Table 4.
Table 4.
Relationship between protein-energy malnutrition (PEM) and infection: effects of PEM on immune cells and non-cellular components
| Effect of PEM | ||
|---|---|---|
| Innate immunity | Adaptive immunity | Organs |
|
Mucus: reduced production and altered structure Intestinal mucosa: reduced integrity Complement: reduced C3 concentration in blood NK cell: reduced activity Neutrophils: reduced respiratory burst and bacterial killing Acute phase proteins: reduced concentration in blood Monocytes/macrophages: reduced production of TNF, IL-1, and IL-6 |
WBC counts: increased or maintained CD3+ proliferation: reduced CD3+CD4+: reduced counts and IL-2 and IFN-γ production CD3+CD8+: reduced counts Antibodies: increased or maintained concentration in blood; decreased or maintained response to immunization; reduced concentration of IgA in saliva and tears |
Thymus, lymph nodes, spleen, tonsils: reduced weight |
C3 complement protein C3, PEM protein-energy malnutrition, WBC white blood cells
A relationship between nutrition and immunity was established following recognition of multiple micronutrient deficiencies which affect immune cells and other components of the immune system, for example ascorbic acid deficiency and scurvy accompanying states of malnutrition. In fact, the idea that proper nutrition also nourishes the immune system gained scientific credibility [203]. Vitamins and minerals exert profound effects on immune cells—in terms of physiology and ontogenesis—that should be considered when treating a patient. Also, the acknowledgement that nutrition may be used to re-establish immunity provides a new perspective for this adjuvant therapy. Table 5 summarizes the main effects of selected vitamins and minerals on the immune system, with significant knowledge arising from studies undertaken to obtain a better picture of nutritional deficiencies in relation to immunity.
Table 5.
Relationship between nutrition and immunity: effect of selected vitamins and minerals on innate and adaptive immunity
| Vitamins/minerals | Innate immunity | Adaptive immunity |
|---|---|---|
| A |
Generation of antibacterial and anti-fungal immune responses Maintenance of barrier integrity, gut permeability, and mucus secretion Killing through NK cells, macrophages, and neutrophils Maintenance of ILCs homeostasis, balancing ILC2 and ILC3 subsets Differentiation of pre-μDCs into CCR9+ plasmacytoid DCs and conventional DCs subsets, preferentially developed into intestinal CD103+ conventional DCs [398, 399] |
Promotion of gut-associated immunity by facilitating induction of IgA-producing B cells, gut-tropic CD4+ and CD8+ T cells, Th17, γδ T cells Generation of mucosal and splenic CD11b+ DC subsets with important role in the generation of Th2, Th17, and antibody responses Balancing of Th1/Th2 subsets, favoring Th2 polarization |
| C |
Enhancing chemotaxis and phagocytosis and thereby promotes microbial killing Protection of phagocytes against ROS-induced damage Reduction endothelial cell expression of the adhesion molecule ICAM-1 in response to TNF-alpha Suppression of systemic neutrophil extravasation during bacterial infections Inhibition of p38 MAPK pathway and endothelial NF-kappa B activity Suppression of endothelial permeability and vascular leakage |
Enhancing of differentiation and proliferation of T cells, particularly enhancing the selection of functional TCRαβ after the stage of β-selection Balancing of Th1/Th2 subsets, favoring Th1 and Th17 differentiation Increasing the induction of CTLs due to production of IL-15 and IL-12 by DCs Regulation of Treg function via epigenetic regulation of Foxp3? |
| D3 | Increasing cathelicidin transcription (VDRE, C/EBPα, SWI/SNF complex) in monocytes/macrophages, keratinocytes, IECs, placental trophoblasts, and LECs |
Suppression of IL-2 transcription in Th1, by blockade of NFAT/AP1 complex and sequestration of Runx1 Suppression of IFN-γ transcription in Th1 Induction of Foxp3 transcription in Treg (VDRE in the conserved non-coding region of the Foxp3 gene) Suppression of IL-17 transcription in Th17, by blockade of NFAT binding, sequestration of Runx1, and inhibition of RORγt |
| Selenium | Improving NK cell activity |
Increasing of lymphocyte proliferation Increasing expression of IL-2R Balancing of Th1/Th2 subsets, favoring Th1 |
| Zinc | Increase of phagocytosis, NK cell activity |
Cytosolic defense against oxidative stress Induction of DTH and antibody response Induction of CTLs |
| Iron | Differentiation of NK cells, monocytes, and macrophages and enhancing of cytotoxic activity | Differentiation and proliferation of Th1, IL-2 production, increasing in immunoglobulin levels |
AP activator protein, DC dendritic cell, Foxp3 forkhead box P3, ILCs innate lymphoid cells, C/EBPα CCAAT/enhancer-binding protein alpha, CTL cytotoxic T-cell, DTH delayed type hypersensitivity, ICAM intercellular adhesion molecule, IEC intraepithelial cell, LEC lymphatic endothelial cell, MAPK mitogen-activated protein kinase, NFAT nuclear factor of activated T-cells, ROR retinoic acid receptor-related orphan receptor, SWI/SNF SWItch/sucrose non-fermentable, TCR T-cell receptor, TNF tumor necrosis factor, VDRE vitamin D response element
The increase in prevalence of chronic non-communicable diseases and the recognition of adipose tissue as a metabolic organ with the capacity to produce specific cytokines (adipokines) and infiltrated with specialized macrophages marked the era of inflammation research. In the inflamed visceral adipose tissue, a phenotype switch in macrophages occurs, establishing the prevalence of classically activated (M1) over alternatively activated (M2) subsets. This increase in HIF-1α and iNOS, thus, provides a propitious environment to metabolize l-arginine into NO, increasing hypoxia and insulin resistance and altering the expression of adhesion molecules responsible for the homeostasis of the vascular endothelium [204–208]. This low-grade chronic inflammation underlies several pathological conditions and is considered a hallmark of obesity, diabetes, coronary arterial disease, chronic infections (tuberculosis) [209, 210], to some extent, sequelae associated with cancer [206, 211]. The central role of inflammation and metabolism in chronic non-communicable diseases has strengthened the relationship between nutrition and immunology. “Classical” obesity and the paradigm of sarcopenic obesity have been gradually replacing PEM as major problems at hospital admission, independently of the underlying pathology [212–214]. Cachexia and sarcopenic obesity are relatively common in patients with cancer and are extremely challenging for clinicians and researchers. Skeletal muscle morphology is now recognized to reflect a relevant prognostic factor for these patients, as the role of skeletal muscle mass (SMM) and metabolism in health and disease is being established [215–218]. SMM loss, as observed in sarcopenia and cancer-related cachexia, is driven by the increase of systemic inflammation [219–221]. Intracellular signaling responsible for muscle wasting is regulated by IL-6, TNF-α, and transforming growth factor beta (TGF-β) in response to several distinct stimuli [219–222]. These cytokines have been mechanistically linked to SMM wasting and disruption of metabolic homeostasis in cancer-related cachexia [223]. Evidence also suggests that these pro-inflammatory cytokines can reduce mitochondrial biogenesis by decreasing the activity of the peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), which in turn has an effect on nuclear respiratory factor 1 (NRF-1) and sirtuin 1 (Sirt-1) expression in cells [220]. Cachectic muscle shows increased autophagy (through induction of microtubule-associated protein light chain 3 (LC3B) Beclin-1, p62, Atg 5, and Bnip3, and dysregulated dynamics (increased FIS-1 and Drp-1 and decreased MFN-1, MFN-2, and OPA-1 expression). These factors contribute to decreased mitochondrial function and ATP synthesis in skeletal muscle. Mitochondrial damage induced by mild oxidative stress can be repaired by mitophagy (targeted autophagic clearance of mitochondria), whereas high levels of oxidative stress lead to mitochondrial fission and ultimately enhanced ROS production [224]. The evidence that loss of SMM is present even when patients seem well nourished (sarcopenic obesity) is sparking more extensive research into the area of body muscle composition as compared to classical assessment based on an individual’s physical stature. In patients with cancer, recovery of SMM has been related to weight maintenance, as sarcopenia is associated with delayed recovery and longer hospital stays postsurgery [225], increased susceptibility to toxicity of chemotherapy, and reduced quality of life and survival [226]. Therefore, SMM reflects a negative prognosis for patients with cancer and warrants greater attention in treatment regimens.
Knowing that inflammation and body composition (fat mass, SMM, free fat mass, and water) are related, it is important to also understand how nutrients may reverse chronic inflammation. Tocopherols (many with the properties of vitamin E), retinol (vitamin-A1-alcohol), zinc, essential fatty acids (omega-3/omega-6 balance), amino acids and nucleotides are able to modulate the intensity of inflammatory responses, more specifically metaflammation or chronic metabolic inflammation [227]. This may in part be responsible why individuals in countries with a high burden of infectious diseases are more susceptible to severe pathology, as many of those who succumb to infectious diseases under-nourished, particularly children [228]. Perinatal nutrition and supply of micronutrients to neonates, including via breast feeding, has already been discussed in light of their paramount importance in priming innate immune responses against bacterial infections in very early childhood [229, 230]. While nutrition is indispensable for muscle mass anabolism, the regulation and fine-tuning of inflammation and immune cell composition in tissue compartments by micronutrients deserves a closer look in clinical studies. It is, therefore, necessary to design future clinical trials (vaccines, drugs, immunotherapy) and treatment plans with the inclusion of the fundamental aspects of nutrition, metabolism, and inflammation.
The relationship between nutrition and immunology can also be extended to injury. It has been widely accepted that nutrition and wound healing are closely related, so that proper nutrition is required to allow progression through all stages of wound healing: inflammatory, proliferative, and remodeling/maturation phases. PEM or nutrient deficiencies negatively impact wound healing by extending the inflammatory phase, decreasing fibroblast proliferation, and reversing collagen synthesis [231]. Malnourished patients are recognized to be at risk of pressure ulcers, infections, delayed wound healing, and chronic non-healing.
Nutrition has been considered one of the most relevant modifiable factors influencing chronic non-communicable diseases. The importance of nutrition is being increasingly recognized by clinicians as a biologically and clinically factor in clinical performance and recovery [232–234], more well-designed clinical studies are need combining clinical endpoints with biological marker analyses, particularly in patients with cancer [235–239]. Recent data from the PREDyES® study revealed that nutritional risk is present at hospital admission in 33.9% of patients, with an increase at discharge from hospital (36.4%) [239]. In a recent report involving a prospective cohort including 1588 patients with cancer, Byung-Gon Na and colleagues demonstrated that malnutrition appears to be more frequent in patients with esophageal, pancreaticobiliary, or lung cancer (52.9%, 47.6%, and 42.8%), followed by stomach, liver, and colon cancers (29.1%, 24.7%, and 15.9%,) [240]. Also, malnourished, patients with cancer who underwent surgical procedures had longer hospital stays and poorer quality of life than those who were well nourished [240].
Nutritional immunology is now considered clinically relevant, to pave the way for novel research paths with the ultimate aim to provide improved nutrition, increased, competent immune function and overall 'better' healthcare.
The role of the microbiome in regulating nutrient bioavailability and immune responses
The study of the microbiome is an emerging area of research with an influence on all aspects of health—cancer [241–243], depression [244], metabolic disease [245], and susceptibility to and control of infections [246, 247]. The gut microbiota is directly involved in the metabolism of drugs [248], thus forming an additional layer of pharmacokinetics further to the role of the liver and kidneys in relation to treatment efficacy.
The gut is considered a unique organ in humans due to the sheer diversity of microflora performing a myriad of functions, in addition to its direct exposure to the external environment. A healthy microbiome—also in other mucosal tissues, i.e., lungs, skin, gums—is directly associated with general well-being [249]. There are psychological, environmental, and physical stressors that affect microbiome composition and function (reviewed in [250]). A major nutritional component linked to immune regulation are short- and long-chain fatty acids (SCFAs and LCFAs) produced by gut commensals. These have been shown to influence memory T-cell formation and maintenance as well as activation of effector cell populations in tissue [251]. The biosynthesis of micronutrients such as vitamins and amino acids by gut commensals including lactic acid bacteria (LAB) would—in the first place—affect the physiology of parenchymal tissues, i.e., epithelial-cell functions, for instance [252]. In fact, the microbiome is also responsible for biosynthesis of vitamins like cobalamin, folic acid, biotin, thiamine, riboflavin, nicotinic acid, pyrodixine, pantothenic acid, and vitamin K [252, 253]. The potential link between SMM and gut dysbiosis, particularly with respect to aging, is being actively explored. Changes in gut microbiota composition have been related to enrichment of certain bacterial species, i.e., Bacteroidetes sp., Escherichia sp., and reduced frequencies of Ruminococcus sp. which have been observed in individuals older than 65 years of age in northern Europe [254, 255]. Also, SMM due to aging has been associated with gut microbiota alterations, which contribute to increased risks of systemic inflammation as well as fat accumulation in skeletal tissue [256]. Consumption of particular types of food have also been investigated as inducers of predictable alterations in existing host microbiota (reviewed in [257]). All dietary proteins contribute to microbial diversity; however, the sources of the protein seem to determine the effect on specific bacterial genera. Animal proteins, particularly red meat, favor Bacteroides, Alistipes, Bilophila, and Ruminococcus, while reducing Bidobacterium; this phenomenon has been associated with increased levels of trimethylamine-N-oxide (proatherogenic) [258] and reduction of SCFA [257]. Proteins of plant origin favor Bidobacteria and Lactobacillus and reduce Bacteroides and Clostridium perfringens, which has been associated with increased production of SCFA and an improved gut barrier, Treg induction, and amelioration of inflammation [257]. Unsaturated fat favors Streptococcus, Lactobacillus, and Bifidobacteria that seem to downregulate TLR activation and white adipose tissue inflammation, while saturated fat is associated with increases in Bacteroides, Bilophila, and Faecalibacterium prausnitzzi promoting white adipose tissue inflammation, TLR activation and impaired insulin sensitivity [257, 259, 260]. Concerning carbohydrates, natural and artificial sweeteners promote different effects on microbiota composition: natural sweeteners tend to increase Bifidobacteria and reduce Bacteroides, while artificial sweeteners seem to have the opposite effect [257]. There is no doubt that the Western diet is associated with dysbiosis (increase in Bacteroides and Enterobacteria and reduction in Bifidobacteria, Lactobacillus, and Eubacteria) [261], while the Mediterranean diet appears to have opposite and beneficial effects on the gut microbiome [262]. In this context, both obesity and malnutrition (despite the few studies available) have a severe impact on gut microbiota as well as individual micronutrient deficiencies [263]. Malnutrition results in persistent impaired maturation of the intestinal microbiota that seems difficult to revert even with refeeding [264]. As such, this topic deserves further investigation in multicohort clinical studies. A healthy “microbiome” does not sufficiently describe the commensal–host relationship and different layers of shaping immune responses. Analysis of the “dark viral matter,” i.e., known and not yet known viral sequences in the gut revealed that a healthy gut microbiome is defined by integrated prophages versus the shift from lysogenic to lytic replication, associated with inflammatory bowel disease [265, 266].
Pertaining to individual micronutrients, vitamin D is an interesting but somewhat controversial paradigm. Vitamin D is necessary for the biosynthesis of cathelicidin (human LL-37), a crucial antimicrobial peptide that is also produced in the gut and linked to the IFN-γ, IL-32, and IL-15 signaling axis [267, 268]. Several studies have gone further to show that LL-37 has anti-cancer properties based on its ability to kill cancer cells in vitro (reviewed by Kuroda et al. in [269]). LL-37 bioavailability in the colon, however, can affect gut microbiota viability and potentially perpetrate dysbiosis, as shown in chickens in the context of CATH-2 [270]. However, mice lacking the antimicrobial peptide CRAMP (CRAMP-KO) displayed oral dysbiosis following co-housing with wild-type mice, possibly transferred to the gut of the CRAMP-KO animals due to CRAMP presence in the feces of the latter [271]. Strikingly, CRAMP-deficient mice exhibited compromised intestinal morphology, i.e., reduced crypt length but increased inflammatory events leading to tissue enlargement. Due to the very high likelihood of inter-organ communication pathways, i.e., gut-lung axis, LL-37 produced in the lungs during an acute bacterial infection could translocate to the bowel and eliminate certain commensal populations—a phenomenon which can also occur in vice versa, at least with regard to microbial metabolites and immune cells [272–274]. Further clinical studies in addition to relevant and well-designed translational models are necessary to better understand how antimicrobial peptide biology plays into nutrient uptake and immune response development in humans. For instance, fecal microbiota transplantation (FMT) for the treatment of recurrent Clostridium difficile infections (CDI) leads not only to clinical improvement in patients but also the establishment of a corrective mechanism to introduce gut-friendly commensals which would compete with C. difficile for nutrients and ameliorate pathology [275]. Correcting the local immunoregulatory networks using FMT also appears to be clinically beneficial in patients with ulcerative colitis [276], where prebiotic therapy helps remodel damaged colon tissue, as is likely the case in recurrent CDI. It would be helpful if a more broader, objective appreciation of mucosal dysbiosis could be performed. This could help to devise more robust clinical studies measuring immune-competence and clinical endpoints in patients with infectious diseases or cancer.
Diet is most often seen as having a circular relationship with the microbiome. However, it has been proposed that a distinction be made between the role of the microbiome in mediating the effects of diet on metabolism and the microbiome itself as a modifier of the host response to diet [277].
Future directions: is there a role for tailor-made nutrition in cancer and infections?
Cancer cachexia, muscle wasting, and metabolism
Along with the immunosuppression that results from a reprogrammed TME, patients with cancer experience profound alterations in body composition as a result of wasting disease and anti-cancer directed treatments [278]. These alterations are most evident in SMM, as muscle as well as adipose tissue wasting are common features in cancer (affecting nearly 80% of late-stage patients) and the major causes of morbidity and mortality [279]. As SMM and adipose tissue are depleted during cancer progression, patients experience weakness, frailty, and loss of mobility [280], followed by a rapid decline in total body weight and severe compromise of immune functions [223]. SMM and adipose tissue depletion are closely connected to increased levels of TNF-α, IL-1, and IL-6, the key mediators of cancer-associated cachexia [281–283]. TNF-α has a direct catabolic effect on MM by induction of the ubiquitin-proteasome system (full form), which dictates an increase in gluconeogenesis, proteolysis and a decrease in protein, lipid, and glycogen synthesis [283]. A comprehensive review of the metabolic changes during cancer cachexia was published recently [284]. However, besides the knowledge that patients with cancer present with hypermetabolism induced by cachexia [285], the effective role of metabolism in muscle consumption deserves further investigation. Patients with cancer exhibit altered glucose metabolism clearly marked by sluggish glucose uptake, reduction of the conversion rate of glucose to glycogen, lactate or CO2, and suppression of enzymes that support glycolysis and glucose oxidation [284]. Lipogenesis has been found to be lower in preclinical cachexia (murine) models. However, lipolysis and FAO rates seem similar in patients with cancer and healthy controls during fasting [286, 287]. Not only protein synthesis and degradation contribute to muscle atrophy, yet also age-related defects in autophagy signalling [288, 289]. In fact, p38β MAPK was identified as a key mediator of cancer-induced autophagy activation in SMM of tumor-bearing mice [290]. The authors demonstrated that this occurs through ULK1 activation and upregulation of C/EBPβ-controlled LC3b and Gabarapl1 genes [290]. Fukawa and colleagues also demonstrated, using human muscle stem cell-based models and human cancer-induced cachexia models in mice, that progressive muscle wasting was associated with excessive FA catabolism triggered by complex pro-inflammatory factors, increased oxidative stress, and activation of the p38 signaling pathway [279]. Mitochondrial dysfunction also seems to underlie SMM consumption in cancer [220], with mitochondrial dynamics and mitophagy signaling being identified as aberrant checkpoints of the muscular-mitochondrial quality control axis associated with cancer cachexia [291].
Chemotherapy-induced cachexia was recently associated with metabolic dysregulation [292]. In a murine Colon26 adenocarcinoma xenograft model, the authors compared the metabolic derangements associated with cancer-induced cachexia with a chemotherapy-induced cachexia model using FOLFIRI (5-fluorouracil, irinotecan, and leucovorin) [292]. Using metabolomic techniques, FOLFIRI-induced cachexia perpetrated slightly higher amino acid catabolism and carbon flux through the TCA cycle and β-oxidation pathways, as compared with cancer cachexia per se [292]. This study highlights the heterogeneity of cachectic phenotypes induced by cancer and chemotherapy may be considered in future study designs. Other clinical studies and reviews drawn a link between chemotherapy and cachexia induction [293–295] as well as overall body composition [296–299]. This reveals that cancer- and treatment-induced cachexia is complex, multifactorial, and personalized for each patient, especially in respect of the circulating mediators secreted and pathways disrupted. The understanding that this complexity and singularity makes each patient unique, strongly argues for nutrition as an integral component of personalized cancer treatment.
Immunonutrients: cancer and infection
Attempts to manipulate the complex network of cells and circulating molecules of the human immune system have been made throughout modern medical history. Considering nutrition as part of these attempts, publications on the dietary manipulation of inflammatory responses date back to the late 1980s and early 1990s [300–303]. Nutrients studied for their possible role on modulating immune responses were considered “immunonutrients,” wherein important contributions have been made by Robert F. Grimble (main reviews [200, 301, 304, 305]). Immunonutrients have been historically divided into omega 3 PUFAs (EPA and DHA), sulfur-containing amino acids, their precursors and other thiol compounds (methionine, cysteine, N-acetyl cysteine and l-2-oxothiazolidine-4carboxylate lipoic acid), glutamine, arginine, and nucleotides [200]. Other nutrients such as antioxidants can also be used for this purpose [306]. These immunonutrients have been studied in supra-physiological doses, administered enterally or parenterally, to achieve some degree of immune response modulation in different pathological conditions [200, 301]. The role of nutrients for immune cell function and competence was discussed earlier in this review. Therefore, profound metabolic and immunological alterations characteristic of cancer provide a unique opportunity for the study of nutritional modulation, especially in the age of personalized precision medicine.
Currently, the nutritional recommendations for patients with cancer, among other aspects, require the following: (i) provision of adequate nutrition to prevent malnutrition, (ii) avoidance of dietary provisions that restrict energy intake in patients with or at risk of malnutrition, (iii) avoidance of supplementation with branched-chain or other amino acids as well as metabolites to improve fat-free mass, and (iv) supplementation with EPA and DHA or fish oil to stabilize or improve appetite, food intake, lean body mass, and body weight [307]. However, some research questions were raised in these guidelines: the influence of fasting or diets mimicking the effects of anti-cancer drugs, the effect of leucine or hydroxy methylbutyrate in unwanted weight loss assessed by large randomized clinical trials (RCTs), the effect of EPA and DHA on body composition and clinical outcome in patients with cancer undergoing treatment, and the effect of omega 3 on quality of life (QoL) and clinical outcome in cachexic patients with cancer. These recommendations, nevertheless, are in need of well-designed clinical trials to obtain solid real-world evidence for clinical practice. Another important issue is the missing link between the nutritional and immunological variables in most clinical studies. Commonly, nutritional publications on the effect of nutrition in clinical outcomes do not account for immunological profiles or immune response parameters. Published studies describing the effect of a single nutrient on immunity or inflammation frequently fail to consider the evaluation of dietary intake or body composition. This is also true for studies evaluating the effect of immunonutrition in cancer.
Three fundamental aspects should be addressed when considering immunonutrition administration and its effect on the overall result: (i) route and (ii) timing of administration as well as (iii) genetic variation among patients [200, 308]. Immunonutrition may be delivered enterally or parenterally, as single nutrient(s) or combinations of two or more immunonutrients. In the early days of immunonutrition, enteral or parenteral formulas were the preferred route for administration of immunonutrients, as the need to resort to artificial nutrition was an opportunity to test the usefulness of these nutrients [309, 310]. Enteral delivery of immunonutrients may be achieved by tube feeding or using oral nutritional supplements (ONS). Currently, oral formulations as capsules are also used, alone or in combination with ONS [311, 312]. The major difference between parenteral and enteral routes is that when the latter route is used, metabolic processing by the liver is bypassed, affecting clinical outcome [200]. Although debated for several years now, there is no consensus on the best route for immunonutrition administration [31, 200, 313, 314]. Regarding timing, preoperative administration of immunonutrition has been studied in the context of surgical critical care, cancer surgery [315–320], as well as perioperative administration [321–323]. Whether immunonutrition should be delivered at the peak of or prior to an inflammatory response remains to be answered. Genetic variation is also an important factor to be considered when evaluating immunonutrition efficacy [324–326]. Hundreds of genes may shape host response to nutrition, contributing to some degree of variability in results with immunonutrients [327–329]. Among others, single-nucleotide polymorphisms (SNPs) have been associated with lipemia owing to dietary lipids and the ability of fish oil to abate TNF production [330–332].
Studies on the effect of single immunonutrients or immunonutrition formulas are heterogenous pertaining to the routes of administration, time of initiation and duration of immunonutrition treatment, the number and characteristics of patients, cancer diagnoses, as well as the outcomes evaluated. Gastrointestinal (GI) malignancies are prevalent worldwide with a vast impact on nutritional status [333–336]. Table 6 presents a compilation of clinical trials on the effect of immunonutrition on GI cancers addressing body composition and immunological parameters/immune responses as outcomes published for the 10 years. Besides several ongoing clinical trials with immunonutrients in cancer, an interesting phase 2b clinical trial on the effect of omega 3 supplementation before radical prostatectomy on prostate cancer proliferation, inflammation, and QoL (NCT02333435) is expected to be concluded in due course [337]. Once again, this study does not address whether immunonutrition may contribute to modulation of immune cell phenotype, especially in the TME. In-depth immunological analyses are desirable in future clinical studies assessing complete dietary evaluation and full nutritional status assessment of patients prior and after intervention.
Table 6.
RCTs testing the effect of immunonutrition on nutritional and immunological outcomes in digestive cancers, published during the last 10 years
| Study (ref.) | Participants | Intervention | Outcomes | Results | |||
|---|---|---|---|---|---|---|---|
| Type | Route | Daily dose | Timing | ||||
| Ida et al., 2017 [400] |
Gastric cancer undergoing gastrectomy N = 63 (46 males) 65.1 (31–79) years |
Omega 3 | Enteral ONS | 2.3 g EPA | 7 days to 1 day prior to surgery | BW, CRP | No effect |
| Miyata et al., 2017 [401] |
Esophageal cancer N = 31 (27 males) 64.5 ± 8.4 years |
Omega 3 |
Enteral ONS |
900 mg EPA + DHA | After CT initiation from day 3 to day 12 (total: 10 days) |
Caloric intake BW, IL-6, TNF-α Toxicity |
Reduced toxicity |
| Sorensen et al., 2014 [402] |
CRC undergoing surgery N = 74 (44 males) 69 ± 11 years |
Omega 3 |
Enteral ONS |
2 g EPA 1 g DHA |
7 days before surgery |
5-HEPE, 5-HETE LTB5, LTB4 |
Reduction in LTB4 production Increase in LTB5 and 5-HEPE production |
| Mocellin et al., 2013 [403] |
CRC undergoing CT N = 6 (3 males) 55.2 ± 7.7 years |
Omega 3 |
Oral Capsules |
350 mg EPA 240 mg DHA |
9 weeks | IL-1β, IL-10, IL-17A, TNF-α, CRP, BW, % BF, LM | Reduction of CRP levels |
| Silva et al., 2012 [404] |
CRC undergoing CT N = 11 (8 males) 50.1 ± 8.2 years |
Omega 3 |
Oral Capsules |
600 mg EPA + DHA 3 mg cholesterol |
9 weeks | TNF-α, IL-1β, IL-6, CRP, BW |
Reduction of CRP levels Improved BW |
| Bonatto et al., 2012 [405] |
Gastrointestinal in CT and after surgery N = 19 (12 males) 53.8 ± 2.4 years |
Omega 3 |
Oral Capsules |
300 mg EPA 400 mg DHA |
8 weeks |
Number and function of PMN BW |
Maintenance of PMN number and function Improved BW |
| Trabal et al., 2010 [406] |
Advanced CRC in CT N = 8 (4 males) 61.5 ± 15.8 years |
Omega 3 |
Enteral ONS |
1.6 g EPA | 12 weeks | BW, dietary intake | Improved BW and appetite |
| Rotovnik Kozjek et al., 2011 [407] |
Rectal cancer receiving RT N = 14 (no reference to gender distribution) 60.5 ± 4.2 years |
AA |
Oral Powder |
30 g glutamine | At start of RT and for subsequent 5 weeks |
IL-6, blood count CRP |
Reduction of IL-6 |
| Martin et al., 2017 [315] |
Pancreatic cancer undergoing surgery N = 44 (30 males) 60 (27–61) years |
Combined |
Enteral ONS |
12.6 g l-arginine 3.3 g EPA + DHA 1.29 g RNA |
5 days prior to surgery | BW, NRI | Decrease in NRI |
| Seguin et al., 2016 [408] |
Liver cancer undergoing surgery N = 18 (14 males) 68 ± 6 years |
Combined |
Oral Powder |
11.4 g l-ARGININE 3 g EPA 1.2 g RNA |
10 days prior to surgery | CD3+, CD4+, CD8+, NK, B cells, phagocytosis capacity | Increased phagocytosis capacity in monocytes |
| Marano et al., 2013 [409] |
Gastric cancer undergoing surgery N = 54 (34 males) 66.6 (55–78) years |
Combined |
Enteral Tube feeding |
24 g l-arginine 3.3 g EPA + DHA 2.3 g RNA |
From 6 h after surgery to 7th day | CD4+, CD8+, leukocyte count | Less impact of surgery on CD4+ |
| Okamoto et al., 2009 [410] |
Gastric cancer N = 30 (20 males) 66.9 ± 11.5 years |
Combined |
Enteral ONS |
9.6 g l-arginine 3.1 g EPA + DHA 0.96 g RNA |
7 days prior to surgery | CD3+, CD4+, CD8+, NK, phagocytosis capacity, HLA-DR expression on monocytes, BW | Maintenance of CD3+, CD4+, CD8+, NK |
Age is presented as mean ± standard deviation or median (range)
AA amino acids, BF body fat, BW body weight, CRC colorectal cancer, CRP C-reactive protein, CT chemotherapy, DHA docosahexaenoic acid, EPA eicosapentaenoic acid, HEPE hydroxyeicosapentaenoic acid, HETE hydroxyeicosatetraenoic acid, LM lean mass, LT leukotriene, NK natural killer, NRI nutritional risk index, ONS oral nutritional supplements, PMN polymorphonuclear leukocytes, RNA ribonucleic acid, RT radiotherapy
Beyond classical immunonutrients, other dietary interventions are currently under investigation for their potential to modulate the TME. One example is fasting, fasting-mimicking diets, and ketogenic diets [338]. Metabolic pathways are activated in response to caloric restriction, promoting inhibition of the mTORC1 pathway to contribute to reduced cancer growth. Additionally, modulation of the ATP/ADP and NADPH/NADP+ ratio, reduction of acetyl-CoA, and decreased serum insulin, glucose, and IGF-1 levels have been associated with caloric restriction [338]. Although not yet recommended for clinical practice (as already discussed here), research in this area is aligned with open questions raised by scientific societies [307]. Fasting, long-term fasting, fasting-mimicking diets, and ketogenic diets are currently under investigation in lung (NCT03700437; NCT01419587), breast (NCT03595540, NCT03162289, NCT01304251; NCT03962647; NCT03535701; NCT02092753), colorectal (NCT03595540), ovarian (NCT03162289), pancreatobiliary (NCT03510429; NCT02964806), pancreatic (NCT01419483), head and neck (NCT01975766), and prostate (NCT02710721) cancers, as well as malignant CNS tumors (NCT03451799; NCT03278249; NCT03075514; NCT02983942; NCT02939378; NCT02302235; NCT02046187; NCT01865162; NCT01754350; NCT01092247; NCT00575146) and studies involving multiple indications (NCT03340935, NCT01954836, NCT01175837, NCT00936364; NCT03162289; NCT03160599; NCT00936364; NCT01175837; NCT01716468; NCT02516501).
Apart from restriction in total calorie intake, restricting specific nutrients may also be an interesting addition to therapeutic strategies. It has been proposed that specific nutrient deprivations, for example K+, may allow TILs to persist in the TME in a less differentiated status associated with strong anti-tumor responses, rather than contribute to T-cell limitation as it is observed for other nutrients [339]. This hypothesis has been explored in publications [339–341] and deserves further clinical investigation.
Immunonutrients are less well studied within clinical trials concerning MTB. Experimental studies suggested that EPA and DHA may improve host defense against infections by limiting excessive inflammation and improving immune responses [342]. For example, in an experimental study with guinea pigs infected with M. tuberculosis, McFarland and colleagues demonstrated that omega 3 intake (13% w/w) for 3 or 6 weeks was associated with decreased lymphoproliferative responses and increased lung bacterial load compared to intake of omega 6-enriched diet [343]. Transgenic mice (producing PUFAs endogenously, Fat-1-trangenic mice) were demonstrated to be more susceptible to MTB infection compared to WT [344]. On the contrary, experimental incorporation of amino acids seems to stimulate TNF-α production by M. tuberculosis-infected macrophages along with antibacterial activity [345]. Epidemiological studies on this subject have provided conflicting results. In selected populations as the Inuit, higher intake of fish has been associated to increased MTB incidence [346–348]. Yet in a large cohort of Chinese men and women (63,257 participants aged 45–74 years old), Soh and colleagues observed that marine omega 3 intake was associated with reduced risk of active MTB in a dose-dependent manner [349]. Regarding amino acids and MTB infection, two RCTs were conducted, to the best of our knowledge, and published during the last 10 years. Ralph et al. studied the effect of 6 g/daily of l-arginine hydrochloride for 8 weeks in MTB clinical outcomes of 99 participants, but no effect was observed [350]. Schön et al. studied the effect of daily intake of arginine-supplemented foods (wheat crackers 0.1 g arginine + 30 g peanuts 1 g arginine) for 4 weeks in patients with smear positive pulmonary tuberculosis, with no observed effects on the outcomes addressed [351]. At this point, biologically relevant clinical studies are needed that take the insights of immune cell activation and differentiation into account.
Immunonutrition as a form of host-directed therapy—ideation for future clinical possibilities
The vastly expanding fields of personalized nutrition and immunometabolism deserve thorough clinical investigation to allow immunonutrition be part of clinical practice in precision immuno-oncology. A specialized clinical immunonutritionist, as a member of the medical care team, would be able to perform a complete evaluation of nutritional demands for each patient and to draft an immunonutrition scheme tailor-made for each individual. For example, the formulation of molecularly defined immunonutrition recipes—akin to “molecular gastronomy” but built on scientifically and medically sound bases—warrants testing in a patient-specific manner, representing a form of personalized host-directed therapy (HDT). There may also be patient groups who could benefit from a particular immunonutrition package, presenting “off-the-shelf” options. Also the routes and time schedule of administration of such 'immunonutrition' has to be considered. Patients may require a certain set of nutrients at a particular juncture and to be given via a particular route (more of one nutrient and less of another and administered in a specific anatomical location). These immunonutrition packages may also be considered at the same time as personalized cancer vaccines are being delivered (potentially with adjuvant-like properties) and/or during the monitoring phase, which may enhance the immune functions of T and B cells and partly compensate for nutrient despoiling by cancer cells [114]. Equally important are well-designed clinical trials evaluating the effect of immunonutrients on phenotypic changes of cells infiltrating the TME during immunotherapy. These can be pursued in translational studies as well as early-phase RCTs at suitable healthcare facilities.
Novel concepts in long-term memory in protective immune responses and mitochondrial fitness
TIL that resemble tissue resident memory T-cells are particularly effective against solid cancers as well as against pathogens. Immune checkpoint blockers target this distinct T-cell population [352]. This is of particular interest since pulmonary tissue resident T-cells (Trm) are abundant in the healthy lung and may play an important role in the first encounters of adaptive immune cells and pathogens invading into pulmonary tissue: T-cells that invade into the pulmonary tissue to form the granuloma could therefore stem from Trm, from regional lymph nodes or, not mutually exclusive, from peripheral blood. However, the phenotypes of Trm, i.e., CD8+, CD69, CD103+, are also shared by exhausted or activated TIL that express as well these markers [353], which makes it challenging to define what is a TIL and what a bona fide Trm. TIL as well as Trm have been studied in the context of cancer and chronic infections—and the key genes responsible for immune protection have been identified. TIL and Trm display both expression of transcription factors such as Hobit, Runx3f and Bhlhe-40 [354, 355], with the latter factor promoting TIL and Trm functions and tissue persistence [354]. Bhlhe-40 favored Th1-type responses and was therefore found to be associated with IFN and granzyme B expression—conversely, Bhhe-40-deficient mice were shown to be inferior in containing melanoma or influenza infections [354]. TIL and Trem did not only share a similar phenotype but also the response and transcription pattern as compared to peripheral T-cells, described as “mitochondrial” fitness [356]. Mitochondria do not only provide energy via ATP but also shape the epigenome. Memory T-cells use oxidative phosphorylation (see above), a concept that was corroborated by the observation that skin Trm access fatty acids and fuel them into the tricarboxylic acid cycle (TCA); a feature that is again shared between Trm and TIL, but not by peripheral T-cells. Bhlhe-40 is preferentially expressed in TCF-1 low cells (see below) that resemble rather Trm. This reflects an important biological function, it designates stem cell-like antigen-specific T-cells in the tissue, defined by strong TCF-1 and low Tim3 expression. These T-cells appear to respond to ICBs and give rise of PD1 high-positive cells that mediate immune protection [356, 357]. HDAC inhibitors, as well as acetate, have been shown to increase IFN-γ production in TIL where Bhlhe40 was downregulated [354] or in antigen-specific T-cells in an “immune exhaustion”-rich environment with high potassium [340]. Increased serum acetate, as a response to bacterial infection, is required for CD8+ T-cell memory formation showing that exposure to pathogens does not only lead to immunopathology but also shapes biologically and clinically relevant anti-target-directed cellular immune responses [358].
Similarly to extrinsic factors, i.e., increased potassium in the tumor microenvironment, or increased serum acetate in infections, may shape the quality and quantity of cellular immune responses: Acetylation has been described in the context of histone modification, yet more detailed analysis, using modern proteomic methodologies, showed that other proteins, involved in cellular maintenance are also acetylated in cellular physiology and pathophysiology. This is mediated by enzymatic reactions, i.e., the transfer of an acetyl-group, and also occur via non-enzymatic reactions where acetyl-CoA plays a major role (reviewed in [359]). Acetyl-CoA, present in mitochondria as well as in the cytosol, is produced from a key enzyme in tumor cells, i.e., acetyl-CoA synthetase enzyme, ACSS2, and contributes to (tumor cell) proliferation. ACSS2, via the production of acetyl-CoA mediates the majority of acetate uptake into cells [360, 361] and presents an alternate mechanisms to provide acetate.
Mitochondrial stress and mitochondrial fitness versus “mitochondrial health” has also been shown to play a biologically relevant role in TB and protective immune responses [362]. Type I interferons, i.e., IFNα and IFNβ are helpful to curb viral pathogens, yet they may be detrimental in MTB infections [363–365]. In contrast to type I interferons, IL-1 production has been shown to be protective in MTB, in part by limiting type I interferon production [366]. This dichotomy between type I interferon and IL-1 production may be dependent on the timing, whether the infection is newly acquired or chronic. Drug-induced, e.g., zileutin, reduction of IFNβ leads to less pro-inflammatory, negative effects of infections. The use of Zileutin has been explored as an adjunct therapy in addition to standard antibiotic treatments of patients with TB. IFNα and INFβ are produced during MTB infection dependent on (i) MTB access to the cytosol in hosT-cells and (ii) STING (stimulator of interferon’ signaling) via mycobacterial DNA (mDNA) binding to the GMP-AMP synthase. A third mechanism has been described [362] where cGAS, a cytosolic DNA sensing structure that binds to dsDNA from stressed mitochondria, leads subsequently to IFNβ production [367]. This links the observation that Bhlh40 provides “mitochondrial health” and immune cell fitness with the notion that mitochondria are able to sense “danger” as well as to signal “danger” via the release of mitochondrial (mt) DNA and reactive oxygen radicals, which has been corroborated in other diseases, e.g., preclinical autoimmune diseases and viral-associated, type I interferon responses [368–370]. Thus, promoting “mitochondrial fitness” may help to curb non-productive inflammation, via downregulation of type I interferon(s) and to enhanced immune effector functions in antigen-specific tissues—resident T-cells and Trm. Re-wiring immune responses by increasing mitochondrial health both in T-cells and (infected) macrophages is not only associated with mitochondrial functions but also with improved cellular metabolism [371]. For instance, MTB reduces glycolysis and the use of the TCA cycle along with oxidative phosphorylation in macrophages—with gradual differences between MTB and BCG. MTB reprograms macrophages to use exogenous fatty acids as compared to endogenous. MTB infection leads to reduced mitochondrial dependence on glucose and to increased use of fatty acids. Thus, acetate and HDAC inhibitors, which have been shown to “reprogram” mitochondria (in TIL and Trm), impact on MTB-associated effects on the mitochondrial competence in macrophages to produce reactive oxygen radicals and oxidizing fatty acids, glutamine, and glucose. The MTB-imprinted microenvironment is reminiscent of the tumor microenvironment that is characterized by “functional starvation,” defined by increased potassium, altered mitochondrial metabolism, depletion of acetyl–coenzyme A (CoA) and methionine intermediates, thereby limiting histone acetylation and the possibility of epigenetic programming and inducing effector molecules and T-cell differentiation [340]. Increased potassium in the (extracellular) space, most likely derived from necrotic cells [341], resulted in a “starvation” program of immune cells associated with increased TCF-1 expression, increased autophagy, and decreased nucleocytosolic acetyl–coenzyme A (AcCoA). That provides stronger persistence of (potentially anti-target-directed) T-cells in TIL or granuloma-associated lymphocytes (GAL) [372] which are associated with stemness, reminiscent of the recent observation that MTB granuloma lesions obtained from a non-human primate model of TB did not exhibit strong expression of immune exhaustion [373]. Thus, there may be similarities between the TME and MTB granuloma lesions, i.e., that hypoxia, necrosis, subsequent high potassium, and a particularly nutrient pattern impose a starvation program facilitating immune cell stemness. A better understanding of these intricate pathway may help to individually map the patients “immune situation” and guide therapeutic options to eradicate or to contain the pathogen (or transformed cells), while preserving long-term memory and avoid overt tissue damage by non-productive inflammation.
Conclusions
Modulating the immune system using nutrient supply may benefit future treatment regimens for patients with cancer or infections at healthcare centers. In addition, ongoing clinical trials evaluating vaccine and drug efficacy may also consider including molecularly defined nutrients and the microbiome as part of their monitoring schemes. The same applies to studies on the microbiome and host directed therapies. Clinical responses in patients with cancer or infections may be improved if 'holistic' treatment modalities, include immmunonutrition and consider the patients unique genetic and immunological background.
Acknowledgements
Prof Giuseppe Ippolito, and Sir Prof Alimuddin Zumla are members of the Pan-African Network on Emerging and Re-emerging Infections (PANDORA-ID-NET), funded by the European & Developing Countries Clinical Trials Partnership, supported under Horizon 2020. Sir Zumla is in receipt of a National Institutes of Health Research senior investigator award. Prof Maeurer acknowledges support from and is funded by the Champalimaud Foundation. Prof Ippolito acknowledges support from the Italian Ministry of Health (Ricerca Corrente Linea 1)
Author contributions
All authors conceptualized and reviewed all available data and clinical trials. RR and MM wrote the first draft. All authors finalized the review.
Compliance with ethical standards
Conflict of interest
All authors are members of THE GLOBAL ALLIANCE BETWEEN CLINICAL CANCER AND INFECTIOUS DISEASE RESEARCH with a particular focus on the COVID-19 pandemic, to better understand the nature of COVID-19 pathophysiology and to take forward host-directed therapies. (Website: https://fchampalimaud.org/covid19/aci/).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Emambokus N, Granger A, Mott R, Helenius T. The immunometabolism choreography. Cell Metab. 2017;26(1):1. doi: 10.1016/j.cmet.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 2.Pearce EJ, Pearce EL (2017) Immunometabolism in 2017: driving immunity: all roads lead to metabolism. Nat Rev Immunol. 10.1038/nri.2017.139 [DOI] [PMC free article] [PubMed]
- 3.Mathis D, Shoelson SE. Immunometabolism: an emerging frontier. Nat Rev Immunol. 2011;11(2):81. doi: 10.1038/nri2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Neill LA, Kishton RJ, Rathmell J. A guide to immunometabolism for immunologists. Nat Rev Immunol. 2016;16(9):553–565. doi: 10.1038/nri.2016.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Neill L. Immunometabolism and the land of milk and honey. Nat Rev Immunol. 2017;17(4):217. doi: 10.1038/nri.2017.22. [DOI] [PubMed] [Google Scholar]
- 6.Loftus RM, Finlay DK. Immunometabolism: cellular metabolism turns immune regulator. J Biol Chem. 2016;291(1):1–10. doi: 10.1074/jbc.R115.693903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly B, O’Neill LA. Metabolic reprogramming in macrophages and dendritic cells in innate immunity. Cell Res. 2015;25(7):771–784. doi: 10.1038/cr.2015.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cao Y, Rathmell JC, Macintyre AN. Metabolic reprogramming towards aerobic glycolysis correlates with greater proliferative ability and resistance to metabolic inhibition in CD8 versus CD4 T cells. PLoS One. 2014;9(8):e104104. doi: 10.1371/journal.pone.0104104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosa Neto JC, Lira FS, Roy S, Festuccia W. Immunometabolism: molecular mechanisms, diseases, and therapies 2016. Mediat Inflamm. 2017;2017:8230298. doi: 10.1155/2017/8230298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schertzer JD, Steinberg GR. Immunometabolism: the interface of immune and metabolic responses in disease. Immunol Cell Biol. 2014;92(4):303. doi: 10.1038/icb.2014.12. [DOI] [PubMed] [Google Scholar]
- 11.Leech JM, Dhariwala MO, Lowe MM, Chu K, Merana GR, Cornuot C, Weckel A, Ma JM, Leitner EG, Gonzalez JR, Vasquez KS, Diep BA, Scharschmidt TC. Toxin-triggered interleukin-1 receptor signaling enables early-life discrimination of pathogenic versus commensal skin bacteria. Cell Host Microbe. 2019;26(6):795–809. doi: 10.1016/j.chom.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rood JE, Stuart T, Ghazanfar S, Biancalani T, Fisher E, Butler A, Hupalowska A, Gaffney L, Mauck W, Eraslan G, Marioni JC, Regev A, Satija R. Toward a common coordinate framework for the human body. Cell. 2019;179(7):1455–1467. doi: 10.1016/j.cell.2019.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pearce EL, Pearce EJ. Metabolic pathways in immune cell activation and quiescence. Immunity. 2013;38(4):633–643. doi: 10.1016/j.immuni.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norata GD, Caligiuri G, Chavakis T, Matarese G, Netea MG, Nicoletti A, O’Neill LA, Marelli-Berg FM. The cellular and molecular basis of translational immunometabolism. Immunity. 2015;43(3):421–434. doi: 10.1016/j.immuni.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Puleston DJ, Villa M, Pearce EL. Ancillary activity: beyond core metabolism in immune cells. Cell Metab. 2017;26(1):131–141. doi: 10.1016/j.cmet.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prochnicki T, Latz E. Inflammasomes on the crossroads of innate immune recognition and metabolic control. Cell Metab. 2017;26(1):71–93. doi: 10.1016/j.cmet.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Pearce EL, Walsh MC, Cejas PJ, Harms GM, Shen H, Wang LS, Jones RG, Choi Y. Enhancing CD8 T-cell memory by modulating fatty acid metabolism. Nature. 2009;460(7251):103–107. doi: 10.1038/nature08097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Windt GJ, Everts B, Chang CH, Curtis JD, Freitas TC, Amiel E, Pearce EJ, Pearce EL. Mitochondrial respiratory capacity is a critical regulator of CD8+ T cell memory development. Immunity. 2012;36(1):68–78. doi: 10.1016/j.immuni.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Sullivan D, van der Windt GJ, Huang SC, Curtis JD, Chang CH, Buck MD, Qiu J, Smith AM, Lam WY, DiPlato LM, Hsu FF, Birnbaum MJ, Pearce EJ, Pearce EL. Memory CD8(+) T cells use cell-intrinsic lipolysis to support the metabolic programming necessary for development. Immunity. 2014;41(1):75–88. doi: 10.1016/j.immuni.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lochner M, Berod L, Sparwasser T. Fatty acid metabolism in the regulation of T cell function. Trends Immunol. 2015;36(2):81–91. doi: 10.1016/j.it.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Pan Y, Tian T, Park CO, Lofftus SY, Mei S, Liu X, Luo C, O’Malley JT, Gehad A, Teague JE, Divito SJ, Fuhlbrigge R, Puigserver P, Krueger JG, Hotamisligil GS, Clark RA, Kupper TS. Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature. 2017;543(7644):252–256. doi: 10.1038/nature21379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raud B, Roy DG, Divakaruni AS, Tarasenko TN, Franke R, Ma EH, Samborska B, Hsieh WY, Wong AH, Stuve P, Arnold-Schrauf C, Guderian M, Lochner M, Rampertaap S, Romito K, Monsale J, Bronstrup M, Bensinger SJ, Murphy AN, McGuire PJ, Jones RG, Sparwasser T, Berod L. Etomoxir actions on regulatory and memory T cells are independent of Cpt1a-mediated fatty acid oxidation. Cell Metab. 2018;28(3):504–515.e507. doi: 10.1016/j.cmet.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mills EL, O’Neill LA. Reprogramming mitochondrial metabolism in macrophages as an anti-inflammatory signal. Eur J Immunol. 2016;46(1):13–21. doi: 10.1002/eji.201445427. [DOI] [PubMed] [Google Scholar]
- 24.Zhang L, Romero P. Metabolic control of CD8(+) T cell fate decisions and antitumor immunity. Trends Mol Med. 2018;24(1):30–48. doi: 10.1016/j.molmed.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10. doi: 10.1016/j.immuni.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Andrejeva G, Rathmell JC. Similarities and distinctions of cancer and immune metabolism in inflammation and tumors. Cell Metab. 2017;26(1):49–70. doi: 10.1016/j.cmet.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen R, Neuzillet C, Tijeras-Raballand A, Faivre S, de Gramont A, Raymond E. Targeting cancer cell metabolism in pancreatic adenocarcinoma. Oncotarget. 2015;6(19):16832–16847. doi: 10.18632/oncotarget.4160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arsenault RJ, Kogut MH. Immunometabolism and the kinome peptide array: a new perspective and tool for the study of gut health. Front Vet Sci. 2015;2:44. doi: 10.3389/fvets.2015.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McPhee JB, Schertzer JD. Immunometabolism of obesity and diabetes: microbiota link compartmentalized immunity in the gut to metabolic tissue inflammation. Clin Sci (Lond) 2015;129(12):1083–1096. doi: 10.1042/cs20150431. [DOI] [PubMed] [Google Scholar]
- 30.Ponton F, Wilson K, Cotter SC, Raubenheimer D, Simpson SJ. Nutritional immunology: a multi-dimensional approach. PLoS Pathog. 2011;7(12):e1002223. doi: 10.1371/journal.ppat.1002223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zapatera B, Prados A, Gomez-Martinez S, Marcos A. Immunonutrition: methodology and applications. Nutr Hosp. 2015;31(Suppl 3):145–154. doi: 10.3305/nh.2015.31.sup3.8762. [DOI] [PubMed] [Google Scholar]
- 32.Cheng SC, Quintin J, Cramer RA, Shepardson KM, Saeed S, Kumar V, Giamarellos-Bourboulis EJ, Martens JH, Rao NA, Aghajanirefah A, Manjeri GR, Li Y, Ifrim DC, Arts RJ, van der Veer BM, Deen PM, Logie C, O’Neill LA, Willems P, van de Veerdonk FL, van der Meer JW, Ng A, Joosten LA, Wijmenga C, Stunnenberg HG, Xavier RJ, Netea MG. mTOR- and HIF-1alpha-mediated aerobic glycolysis as metabolic basis for trained immunity. Science. 2014;345(6204):1250684. doi: 10.1126/science.1250684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Palsson-McDermott EM, O’Neill LA. The Warburg effect then and now: from cancer to inflammatory diseases. Bioessays. 2013;35(11):965–973. doi: 10.1002/bies.201300084. [DOI] [PubMed] [Google Scholar]
- 34.Fadaka A, Ajiboye B, Ojo O, Adewale O, Olayide I, Emuowhochere R. Biology of glucose metabolization in cancer cells. J Oncol Sci. 2017;3(2):45–51. doi: 10.1016/j.jons.2017.06.002. [DOI] [Google Scholar]
- 35.Jiang B. Aerobic glycolysis and high level of lactate in cancer metabolism and microenvironment. Genes Dis. 2017;4(1):25–27. doi: 10.1016/j.gendis.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao Y. Cancer metabolism as we know it today: a prologue to a special issue of cancer metabolism. Genes Dis. 2017;4(1):4–6. doi: 10.1016/j.gendis.2017.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tan Z, Xie N, Cui H, Moellering DR, Abraham E, Thannickal VJ, Liu G. Pyruvate dehydrogenase kinase 1 participates in macrophage polarization via regulating glucose metabolism. J Immunol. 2015;194(12):6082–6089. doi: 10.4049/jimmunol.1402469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palsson-McDermott EM, Curtis AM, Goel G, Lauterbach MA, Sheedy FJ, Gleeson LE, van den Bosch MW, Quinn SR, Domingo-Fernandez R, Johnston DG, Jiang JK, Israelsen WJ, Keane J, Thomas C, Clish C, Vander Heiden M, Xavier RJ, O’Neill LA. Pyruvate kinase M2 regulates Hif-1alpha activity and IL-1beta induction and is a critical determinant of the Warburg effect in LPS-activated macrophages. Cell Metab. 2015;21(1):65–80. doi: 10.1016/j.cmet.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shapiro H, Lutaty A, Ariel A. Macrophages, meta-inflammation, and immuno-metabolism. ScientificWorldJournal. 2011;11:2509–2529. doi: 10.1100/2011/397971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Curi R, de Siqueira MR, de Campos Crispin LA, Norata GD, Sampaio SC, Newsholme P. A past and present overview of macrophage metabolism and functional outcomes. Clin Sci (Lond) 2017;131(12):1329–1342. doi: 10.1042/cs20170220. [DOI] [PubMed] [Google Scholar]
- 41.Ryan DG, O’Neill LAJ. Krebs cycle rewired for macrophage and dendritic cell effector functions. FEBS Lett. 2017;591(19):2992–3006. doi: 10.1002/1873-3468.12744. [DOI] [PubMed] [Google Scholar]
- 42.Almeida L, Lochner M, Berod L, Sparwasser T. Metabolic pathways in T cell activation and lineage differentiation. Semin Immunol. 2016;28(5):514–524. doi: 10.1016/j.smim.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Stincone A, Prigione A, Cramer T, Wamelink MM, Campbell K, Cheung E, Olin-Sandoval V, Gruning NM, Kruger A, Tauqeer Alam M, Keller MA, Breitenbach M, Brindle KM, Rabinowitz JD, Ralser M. The return of metabolism: biochemistry and physiology of the pentose phosphate pathway. Biol Rev Camb Philos Soc. 2015;90(3):927–963. doi: 10.1111/brv.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barcia-Vieitez R, Ramos-Martinez JI. The regulation of the oxidative phase of the pentose phosphate pathway: new answers to old problems. IUBMB Life. 2014;66(11):775–779. doi: 10.1002/iub.1329. [DOI] [PubMed] [Google Scholar]
- 45.Nagy C, Haschemi A. Time and demand are two critical dimensions of immunometabolism: the process of macrophage activation and the pentose phosphate pathway. Front Immunol. 2015;6:164. doi: 10.3389/fimmu.2015.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Akram M. Citric acid cycle and role of its intermediates in metabolism. Cell Biochem Biophys. 2014;68(3):475–478. doi: 10.1007/s12013-013-9750-1. [DOI] [PubMed] [Google Scholar]
- 47.Berod L, Friedrich C, Nandan A, Freitag J, Hagemann S, Harmrolfs K, Sandouk A, Hesse C, Castro CN, Bahre H, Tschirner SK, Gorinski N, Gohmert M, Mayer CT, Huehn J, Ponimaskin E, Abraham WR, Muller R, Lochner M, Sparwasser T. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat Med. 2014;20(11):1327–1333. doi: 10.1038/nm.3704. [DOI] [PubMed] [Google Scholar]
- 48.Alvarez-Curto E, Milligan G. Metabolism meets immunity: the role of free fatty acid receptors in the immune system. Biochem Pharmacol. 2016;114:3–13. doi: 10.1016/j.bcp.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 49.Namgaladze D, Brune B. Macrophage fatty acid oxidation and its roles in macrophage polarization and fatty acid-induced inflammation. Biochim Biophys Acta. 2016;1861(11):1796–1807. doi: 10.1016/j.bbalip.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 50.Holecek M, Vodenicarovova M, Siman P. Acute effects of phenylbutyrate on glutamine, branched-chain amino acid and protein metabolism in skeletal muscles of rats. Int J Exp Pathol. 2017;98(3):127–133. doi: 10.1111/iep.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cruzat V, Macedo Rogero M, Noel Keane K, Curi R, Newsholme P (2018) Glutamine: metabolism and immune function, supplementation and clinical translation. Nutrients 10(11). 10.3390/nu10111564 [DOI] [PMC free article] [PubMed]
- 52.Ren W, Wang K, Yin J, Chen S, Liu G, Tan B, Wu G, Bazer FW, Peng Y, Yin Y. Glutamine-induced secretion of intestinal secretory immunoglobulin A: a mechanistic perspective. Front Immunol. 2016;7:503. doi: 10.3389/fimmu.2016.00503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sartori T, Galvao Dos Santos G, Nogueira-Pedro A, Makiyama E, Rogero MM, Borelli P, Fock RA. Effects of glutamine, taurine and their association on inflammatory pathway markers in macrophages. Inflammopharmacology. 2018;26(3):829–838. doi: 10.1007/s10787-017-0406-4. [DOI] [PubMed] [Google Scholar]
- 54.Moinard C, Caldefie-Chezet F, Walrand S, Vasson MP, Cynober L. Evidence that glutamine modulates respiratory burst in stressed rat polymorphonuclear cells through its metabolism into arginine. Br J Nutr. 2002;88(6):689–695. doi: 10.1079/bjn2002724. [DOI] [PubMed] [Google Scholar]
- 55.Carr EL, Kelman A, Wu GS, Gopaul R, Senkevitch E, Aghvanyan A, Turay AM, Frauwirth KA. Glutamine uptake and metabolism are coordinately regulated by ERK/MAPK during T lymphocyte activation. J Immunol. 2010;185(2):1037–1044. doi: 10.4049/jimmunol.0903586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim SH, Roszik J, Grimm EA, Ekmekcioglu S. Impact of L-arginine metabolism on immune response and anticancer immunotherapy. Front Oncol. 2018;8:67. doi: 10.3389/fonc.2018.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Geiger R, Rieckmann JC, Wolf T, Basso C, Feng Y, Fuhrer T, Kogadeeva M, Picotti P, Meissner F, Mann M, Zamboni N, Sallusto F, Lanzavecchia A. L-Arginine modulates T cell metabolism and enhances survival and anti-tumor activity. Cell. 2016;167(3):829–842.e813. doi: 10.1016/j.cell.2016.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Duque-Correa MA, Kuhl AA, Rodriguez PC, Zedler U, Schommer-Leitner S, Rao M, Weiner J, 3rd, Hurwitz R, Qualls JE, Kosmiadi GA, Murray PJ, Kaufmann SH, Reece ST. Macrophage arginase-1 controls bacterial growth and pathology in hypoxic tuberculosis granulomas. Proc Natl Acad Sci U S A. 2014;111(38):E4024–E4032. doi: 10.1073/pnas.1408839111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rodriguez PC, Ochoa AC, Al-Khami AA. Arginine metabolism in myeloid cells shapes innate and adaptive immunity. Front Immunol. 2017;8:93. doi: 10.3389/fimmu.2017.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rodriguez PC, Zea AH, Culotta KS, Zabaleta J, Ochoa JB, Ochoa AC. Regulation of T cell receptor CD3zeta chain expression by L-arginine. J Biol Chem. 2002;277(24):21123–21129. doi: 10.1074/jbc.M110675200. [DOI] [PubMed] [Google Scholar]
- 61.Korrer MJ, Zhang Y, Routes JM. Possible role of arginase-1 in concomitant tumor immunity. PLoS One. 2014;9(3):e91370. doi: 10.1371/journal.pone.0091370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Saligan LN, Lukkahatai N, Zhang ZJ, Cheung CW, Wang XM. Altered Cd8+ T lymphocyte response triggered by arginase 1: implication for fatigue intensification during localized radiation therapy in prostate cancer patients. Neuropsychiatry. 2018;8(4):1249–1262. doi: 10.4172/Neuropsychiatry.1000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rodriguez PC, Ochoa AC. Arginine regulation by myeloid derived suppressor cells and tolerance in cancer: mechanisms and therapeutic perspectives. Immunol Rev. 2008;222:180–191. doi: 10.1111/j.1600-065X.2008.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Raber P, Ochoa AC, Rodriguez PC. Metabolism of L-arginine by myeloid-derived suppressor cells in cancer: mechanisms of T cell suppression and therapeutic perspectives. Immunol Investig. 2012;41(6–7):614–634. doi: 10.3109/08820139.2012.680634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu H, Gong J, Liu Y. Indoleamine 2, 3-dioxygenase regulation of immune response (review) Mol Med Rep. 2018;17(4):4867–4873. doi: 10.3892/mmr.2018.8537. [DOI] [PubMed] [Google Scholar]
- 66.Brochez L, Chevolet I, Kruse V. The rationale of indoleamine 2,3-dioxygenase inhibition for cancer therapy. Eur J Cancer. 2017;76:167–182. doi: 10.1016/j.ejca.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 67.Wang XF, Wang HS, Wang H, Zhang F, Wang KF, Guo Q, Zhang G, Cai SH, Du J. The role of indoleamine 2,3-dioxygenase (IDO) in immune tolerance: focus on macrophage polarization of THP-1 cells. Cell Immunol. 2014;289(1–2):42–48. doi: 10.1016/j.cellimm.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 68.Husain Z, Huang Y, Seth P, Sukhatme VP. Tumor-derived lactate modifies antitumor immune response: effect on myeloid-derived suppressor cells and NK cells. J Immunol. 2013;191(3):1486–1495. doi: 10.4049/jimmunol.1202702. [DOI] [PubMed] [Google Scholar]
- 69.Hirschhaeuser F, Sattler UG, Mueller-Klieser W. Lactate: a metabolic key player in cancer. Cancer Res. 2011;71(22):6921–6925. doi: 10.1158/0008-5472.can-11-1457. [DOI] [PubMed] [Google Scholar]
- 70.Haas R, Smith J, Rocher-Ros V, Nadkarni S, Montero-Melendez T, D’Acquisto F, Bland EJ, Bombardieri M, Pitzalis C, Perretti M, Marelli-Berg FM, Mauro C. Lactate regulates metabolic and pro-inflammatory circuits in control of T cell migration and effector functions. PLoS Biol. 2015;13(7):e1002202. doi: 10.1371/journal.pbio.1002202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324(5930):1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vazquez A, Liu J, Zhou Y, Oltvai ZN. Catabolic efficiency of aerobic glycolysis: the Warburg effect revisited. BMC Syst Biol. 2010;4:58. doi: 10.1186/1752-0509-4-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jha AK, Huang SC, Sergushichev A, Lampropoulou V, Ivanova Y, Loginicheva E, Chmielewski K, Stewart KM, Ashall J, Everts B, Pearce EJ, Driggers EM, Artyomov MN. Network integration of parallel metabolic and transcriptional data reveals metabolic modules that regulate macrophage polarization. Immunity. 2015;42(3):419–430. doi: 10.1016/j.immuni.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 74.Epstein T, Gatenby RA, Brown JS. The Warburg effect as an adaptation of cancer cells to rapid fluctuations in energy demand. PLoS One. 2017;12(9):e0185085. doi: 10.1371/journal.pone.0185085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lu J, Tan M, Cai Q. The Warburg effect in tumor progression: mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. 2015;356(2 Pt A):156–164. doi: 10.1016/j.canlet.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhu L, Zhao Q, Yang T, Ding W, Zhao Y. Cellular metabolism and macrophage functional polarization. Int Rev Immunol. 2015;34(1):82–100. doi: 10.3109/08830185.2014.969421. [DOI] [PubMed] [Google Scholar]
- 77.Van den Bossche J, O’Neill LA, Menon D. Macrophage immunometabolism: where are we (going)? Trends Immunol. 2017;38(6):395–406. doi: 10.1016/j.it.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 78.Torres A, Makowski L, Wellen KE (2016) Immunometabolism: metabolism fine-tunes macrophage activation. Elife 5. 10.7554/eLife.14354 [DOI] [PMC free article] [PubMed]
- 79.Diskin C, Palsson-McDermott EM. Metabolic modulation in macrophage effector function. Front Immunol. 2018;9:270. doi: 10.3389/fimmu.2018.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou D, Huang C, Lin Z, Zhan S, Kong L, Fang C, Li J. Macrophage polarization and function with emphasis on the evolving roles of coordinated regulation of cellular signaling pathways. Cell Signal. 2014;26(2):192–197. doi: 10.1016/j.cellsig.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 81.Artyomov MN, Sergushichev A, Schilling JD. Integrating immunometabolism and macrophage diversity. Semin Immunol. 2016;28(5):417–424. doi: 10.1016/j.smim.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Biswas SK, Mantovani A. Orchestration of metabolism by macrophages. Cell Metab. 2012;15(4):432–437. doi: 10.1016/j.cmet.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 83.Bosca L, Gonzalez-Ramos S, Prieto P, Fernandez-Velasco M, Mojena M, Martin-Sanz P, Alemany S. Metabolic signatures linked to macrophage polarization: from glucose metabolism to oxidative phosphorylation. Biochem Soc Trans. 2015;43(4):740–744. doi: 10.1042/bst20150107. [DOI] [PubMed] [Google Scholar]
- 84.O’Neill LA. A broken Krebs cycle in macrophages. Immunity. 2015;42(3):393–394. doi: 10.1016/j.immuni.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 85.Lirk P, Hoffmann G, Rieder J. Inducible nitric oxide synthase—time for reappraisal. Curr Drug Targets Inflamm Allergy. 2002;1(1):89–108. doi: 10.2174/1568010023344913. [DOI] [PubMed] [Google Scholar]
- 86.Rath M, Muller I, Kropf P, Closs EI, Munder M. Metabolism via arginase or nitric oxide synthase: two competing arginine pathways in macrophages. Front Immunol. 2014;5:532. doi: 10.3389/fimmu.2014.00532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Starling S. Immunometabolism: T cells activate the fear. Nat Rev Immunol. 2017;17(12):730–731. doi: 10.1038/nri.2017.126. [DOI] [PubMed] [Google Scholar]
- 88.MacIver NJ, Michalek RD, Rathmell JC. Metabolic regulation of T lymphocytes. Annu Rev Immunol. 2013;31:259–283. doi: 10.1146/annurev-immunol-032712-095956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen H, Yang T, Zhu L, Zhao Y. Cellular metabolism on T-cell development and function. Int Rev Immunol. 2015;34(1):19–33. doi: 10.3109/08830185.2014.902452. [DOI] [PubMed] [Google Scholar]
- 90.Waickman AT, Powell JD. mTOR, metabolism, and the regulation of T-cell differentiation and function. Immunol Rev. 2012;249(1):43–58. doi: 10.1111/j.1600-065X.2012.01152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shi LZ, Wang R, Huang G, Vogel P, Neale G, Green DR, Chi H. HIF1alpha-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. J Exp Med. 2011;208(7):1367–1376. doi: 10.1084/jem.20110278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bayes HK, Ritchie ND, Evans TJ. Interleukin-17 is required for control of chronic lung infection caused by Pseudomonas aeruginosa. Infect Immun. 2016;84(12):3507–3516. doi: 10.1128/iai.00717-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gopal R, Monin L, Slight S, Uche U, Blanchard E, Fallert Junecko BA, Ramos-Payan R, Stallings CL, Reinhart TA, Kolls JK, Kaushal D, Nagarajan U, Rangel-Moreno J, Khader SA. Unexpected role for IL-17 in protective immunity against hypervirulent Mycobacterium tuberculosis HN878 infection. PLoS Pathog. 2014;10(5):e1004099. doi: 10.1371/journal.ppat.1004099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lereclus E, Tout M, Girault A, Baroukh N, Caulet M, Borg C, Bouche O, Ternant D, Paintaud G, Lecomte T, Raoul W. A possible association of baseline serum IL-17A concentrations with progression-free survival of metastatic colorectal cancer patients treated with a bevacizumab-based regimen. BMC Cancer. 2017;17(1):220. doi: 10.1186/s12885-017-3210-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fabre JAS, Giustinniani J, Garbar C, Merrouche Y, Antonicelli F, Bensussan A (2018) The interleukin-17 family of cytokines in breast cancer. Int J Mol Sci 19(12). 10.3390/ijms19123880 [DOI] [PMC free article] [PubMed]
- 96.Doughty CA, Bleiman BF, Wagner DJ, Dufort FJ, Mataraza JM, Roberts MF, Chiles TC. Antigen receptor-mediated changes in glucose metabolism in B lymphocytes: role of phosphatidylinositol 3-kinase signaling in the glycolytic control of growth. Blood. 2006;107(11):4458–4465. doi: 10.1182/blood-2005-12-4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Caro-Maldonado A, Wang R, Nichols AG, Kuraoka M, Milasta S, Sun LD, Gavin AL, Abel ED, Kelsoe G, Green DR, Rathmell JC. Metabolic reprogramming is required for antibody production that is suppressed in anergic but exaggerated in chronically BAFF-exposed B cells. J Immunol. 2014;192(8):3626–3636. doi: 10.4049/jimmunol.1302062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.O’Neill LA, Pearce EJ. Immunometabolism governs dendritic cell and macrophage function. J Exp Med. 2016;213(1):15–23. doi: 10.1084/jem.20151570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Al-Khami AA, Rodriguez PC, Ochoa AC. Energy metabolic pathways control the fate and function of myeloid immune cells. J Leukoc Biol. 2017;102(2):369–380. doi: 10.1189/jlb.1VMR1216-535R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pearce EJ, Everts B. Dendritic cell metabolism. Nat Rev Immunol. 2015;15(1):18–29. doi: 10.1038/nri3771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jantsch J, Chakravortty D, Turza N, Prechtel AT, Buchholz B, Gerlach RG, Volke M, Glasner J, Warnecke C, Wiesener MS, Eckardt KU, Steinkasserer A, Hensel M, Willam C. Hypoxia and hypoxia-inducible factor-1 alpha modulate lipopolysaccharide-induced dendritic cell activation and function. J Immunol. 2008;180(7):4697–4705. doi: 10.4049/jimmunol.180.7.4697. [DOI] [PubMed] [Google Scholar]
- 102.Krawczyk CM, Holowka T, Sun J, Blagih J, Amiel E, DeBerardinis RJ, Cross JR, Jung E, Thompson CB, Jones RG, Pearce EJ. Toll-like receptor-induced changes in glycolytic metabolism regulate dendritic cell activation. Blood. 2010;115(23):4742–4749. doi: 10.1182/blood-2009-10-249540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sim WJ, Ahl PJ, Connolly JE. Metabolism is central to tolerogenic dendritic cell function. Mediat Inflamm. 2016;2016:2636701. doi: 10.1155/2016/2636701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Everts B, Amiel E, Huang SC, Smith AM, Chang CH, Lam WY, Redmann V, Freitas TC, Blagih J, van der Windt GJ, Artyomov MN, Jones RG, Pearce EL, Pearce EJ. TLR-driven early glycolytic reprogramming via the kinases TBK1-IKKvarepsilon supports the anabolic demands of dendritic cell activation. Nat Immunol. 2014;15(4):323–332. doi: 10.1038/ni.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pantel A, Teixeira A, Haddad E, Wood EG, Steinman RM, Longhi MP. Direct type I IFN but not MDA5/TLR3 activation of dendritic cells is required for maturation and metabolic shift to glycolysis after poly IC stimulation. PLoS Biol. 2014;12(1):e1001759. doi: 10.1371/journal.pbio.1001759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Thwe PM, Amiel E. The role of nitric oxide in metabolic regulation of dendritic cell immune function. Cancer Lett. 2018;412:236–242. doi: 10.1016/j.canlet.2017.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mondanelli G, Bianchi R, Pallotta MT, Orabona C, Albini E, Iacono A, Belladonna ML, Vacca C, Fallarino F, Macchiarulo A, Ugel S, Bronte V, Gevi F, Zolla L, Verhaar A, Peppelenbosch M, Mazza EMC, Bicciato S, Laouar Y, Santambrogio L, Puccetti P, Volpi C, Grohmann U. A relay pathway between arginine and tryptophan metabolism confers immunosuppressive properties on dendritic cells. Immunity. 2017;46(2):233–244. doi: 10.1016/j.immuni.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kedia-Mehta N, Finlay DK. Competition for nutrients and its role in controlling immune responses. Nat Commun. 2019;10(1):2123. doi: 10.1038/s41467-019-10015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cascone T, McKenzie JA, Mbofung RM, Punt S, Wang Z, Xu C, Williams LJ, Wang Z, Bristow CA, Carugo A, Peoples MD, Li L, Karpinets T, Huang L, Malu S, Creasy C, Leahey SE, Chen J, Chen Y, Pelicano H, Bernatchez C, Gopal YNV, Heffernan TP, Hu J, Wang J, Amaria RN, Garraway LA, Huang P, Yang P, Wistuba II, Woodman SE, Roszik J, Davis RE, Davies MA, Heymach JV, Hwu P, Peng W. Increased tumor glycolysis characterizes immune resistance to adoptive T cell therapy. Cell Metab. 2018;27(5):977–987.e974. doi: 10.1016/j.cmet.2018.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bowden SD, Rowley G, Hinton JC, Thompson A. Glucose and glycolysis are required for the successful infection of macrophages and mice by Salmonella enterica serovar Typhimurium. Infect Immun. 2009;77(7):3117–3126. doi: 10.1128/iai.00093-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thai M, Thaker SK, Feng J, Du Y, Hu H, Ting Wu T, Graeber TG, Braas D, Christofk HR. MYC-induced reprogramming of glutamine catabolism supports optimal virus replication. Nat Commun. 2015;6:8873. doi: 10.1038/ncomms9873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Courtnay R, Ngo DC, Malik N, Ververis K, Tortorella SM, Karagiannis TC. Cancer metabolism and the Warburg effect: the role of HIF-1 and PI3K. Mol Biol Rep. 2015;42(4):841–851. doi: 10.1007/s11033-015-3858-x. [DOI] [PubMed] [Google Scholar]
- 113.Dang CV, Kim JW. Convergence of cancer metabolism and immunity: an overview. Biomol Ther. 2018;26(1):4–9. doi: 10.4062/biomolther.2017.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Renner K, Singer K, Koehl GE, Geissler EK, Peter K, Siska PJ, Kreutz M. Metabolic hallmarks of tumor and immune cells in the tumor microenvironment. Front Immunol. 2017;8:248. doi: 10.3389/fimmu.2017.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Warburg O, Wind F, Negelein E. The metabolism of tumors in the body. J Gen Physiol. 1927;8(6):519–530. doi: 10.1085/jgp.8.6.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koppenol WH, Bounds PL, Dang CV. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat Rev Cancer. 2011;11(5):325–337. doi: 10.1038/nrc3038. [DOI] [PubMed] [Google Scholar]
- 117.Yun J, Rago C, Cheong I, Pagliarini R, Angenendt P, Rajagopalan H, Schmidt K, Willson JK, Markowitz S, Zhou S, Diaz LA, Jr, Velculescu VE, Lengauer C, Kinzler KW, Vogelstein B, Papadopoulos N. Glucose deprivation contributes to the development of KRAS pathway mutations in tumor cells. Science. 2009;325(5947):1555–1559. doi: 10.1126/science.1174229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lee N, Kim D. Cancer metabolism: fueling more than just growth. Mol Cell. 2016;39(12):847–854. doi: 10.14348/molcells.2016.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huang R, Zong X. Aberrant cancer metabolism in epithelial-mesenchymal transition and cancer metastasis: mechanisms in cancer progression. Crit Rev Oncol Hematol. 2017;115:13–22. doi: 10.1016/j.critrevonc.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 120.Corbet C, Feron O. Tumour acidosis: from the passenger to the driver’s seat. Nat Rev Cancer. 2017;17(10):577–593. doi: 10.1038/nrc.2017.77. [DOI] [PubMed] [Google Scholar]
- 121.Damaghi M, Tafreshi NK, Lloyd MC, Sprung R, Estrella V, Wojtkowiak JW, Morse DL, Koomen JM, Bui MM, Gatenby RA, Gillies RJ. Chronic acidosis in the tumour microenvironment selects for overexpression of LAMP2 in the plasma membrane. Nat Commun. 2015;6:8752. doi: 10.1038/ncomms9752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Luo F, Zou Z, Liu X, Ling M, Wang Q, Wang Q, Lu L, Shi L, Liu Y, Liu Q, Zhang A. Enhanced glycolysis, regulated by HIF-1alpha via MCT-4, promotes inflammation in arsenite-induced carcinogenesis. Carcinogenesis. 2017;38(6):615–626. doi: 10.1093/carcin/bgx034. [DOI] [PubMed] [Google Scholar]
- 123.Lien S, Lowman HB. Therapeutic anti-VEGF antibodies. Handb Exp Pharmacol. 2008;181:131–150. doi: 10.1007/978-3-540-73259-4_6. [DOI] [PubMed] [Google Scholar]
- 124.Ueda S, Saeki T, Osaki A, Yamane T, Kuji I. Bevacizumab induces acute hypoxia and cancer progression in patients with refractory breast cancer: multimodal functional imaging and multiplex cytokine analysis. Clin Cancer Res. 2017;23(19):5769–5778. doi: 10.1158/1078-0432.Ccr-17-0874. [DOI] [PubMed] [Google Scholar]
- 125.Cheong H. Integrating autophagy and metabolism in cancer. Arch Pharm Res. 2015;38(3):358–371. doi: 10.1007/s12272-015-0562-2. [DOI] [PubMed] [Google Scholar]
- 126.Goldsmith J, Levine B, Debnath J. Autophagy and cancer metabolism. Methods Enzymol. 2014;542:25–57. doi: 10.1016/b978-0-12-416618-9.00002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Brown RS, Wahl RL. Overexpression of Glut-1 glucose transporter in human breast cancer. An immunohistochemical study. Cancer. 1993;72(10):2979–2985. doi: 10.1002/1097-0142(19931115)72:10<2979::AID-CNCR2820721020>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 128.Canpolat T, Ersoz C, Uguz A, Vardar MA, Altintas A. GLUT-1 expression in proliferative endometrium, endometrial hyperplasia, endometrial adenocarcinoma and the relationship between GLUT-1 expression and prognostic parameters in endometrial adenocarcinoma. Turk Patoloji Derg. 2016;32(3):141–147. doi: 10.5146/tjpath.2015.01352. [DOI] [PubMed] [Google Scholar]
- 129.Cho H, Lee YS, Kim J, Chung JY, Kim JH. Overexpression of glucose transporter-1 (GLUT-1) predicts poor prognosis in epithelial ovarian cancer. Cancer Investig. 2013;31(9):607–615. doi: 10.3109/07357907.2013.849722. [DOI] [PubMed] [Google Scholar]
- 130.Li CX, Sun JL, Gong ZC, Lin ZQ, Liu H. Prognostic value of GLUT-1 expression in oral squamous cell carcinoma: a prisma-compliant meta-analysis. Medicine (Baltimore) 2016;95(45):e5324. doi: 10.1097/md.0000000000005324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yang J, Wen J, Tian T, Lu Z, Wang Y, Wang Z, Wang X, Yang Y. GLUT-1 overexpression as an unfavorable prognostic biomarker in patients with colorectal cancer. Oncotarget. 2017;8(7):11788–11796. doi: 10.18632/oncotarget.14352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nagarajan A, Malvi P, Wajapeyee N. Oncogene-directed alterations in cancer cell metabolism. Trends Cancer. 2016;2(7):365–377. doi: 10.1016/j.trecan.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Boros LG, Torday JS, Lim S, Bassilian S, Cascante M, Lee WN. Transforming growth factor beta2 promotes glucose carbon incorporation into nucleic acid ribose through the nonoxidative pentose cycle in lung epithelial carcinoma cells. Cancer Res. 2000;60(5):1183–1185. [PubMed] [Google Scholar]
- 134.Marchiq I, Pouyssegur J. Hypoxia, cancer metabolism and the therapeutic benefit of targeting lactate/H(+) symporters. J Mol Med. 2016;94(2):155–171. doi: 10.1007/s00109-015-1307-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Komohara Y, Takeya M. CAFs and TAMs: maestros of the tumour microenvironment. J Pathol. 2017;241(3):313–315. doi: 10.1002/path.4824. [DOI] [PubMed] [Google Scholar]
- 136.Hashimoto O, Yoshida M, Koma Y, Yanai T, Hasegawa D, Kosaka Y, Nishimura N, Yokozaki H. Collaboration of cancer-associated fibroblasts and tumour-associated macrophages for neuroblastoma development. J Pathol. 2016;240(2):211–223. doi: 10.1002/path.4769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang A, Qian Y, Ye Z, Chen H, Xie H, Zhou L, Shen Y, Zheng S. Cancer-associated fibroblasts promote M2 polarization of macrophages in pancreatic ductal adenocarcinoma. Cancer Med. 2017;6(2):463–470. doi: 10.1002/cam4.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Miyake M, Hori S, Morizawa Y, Tatsumi Y, Nakai Y, Anai S, Torimoto K, Aoki K, Tanaka N, Shimada K, Konishi N, Toritsuka M, Kishimoto T, Rosser CJ, Fujimoto K. CXCL1-mediated interaction of cancer cells with tumor-associated macrophages and cancer-associated fibroblasts promotes tumor progression in human bladder cancer. Neoplasia. 2016;18(10):636–646. doi: 10.1016/j.neo.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Comito G, Giannoni E, Segura CP, Barcellos-de-Souza P, Raspollini MR, Baroni G, Lanciotti M, Serni S, Chiarugi P. Cancer-associated fibroblasts and M2-polarized macrophages synergize during prostate carcinoma progression. Oncogene. 2014;33(19):2423–2431. doi: 10.1038/onc.2013.191. [DOI] [PubMed] [Google Scholar]
- 140.Kumar V, Donthireddy L, Marvel D, Condamine T, Wang F, Lavilla-Alonso S, Hashimoto A, Vonteddu P, Behera R, Goins MA, Mulligan C, Nam B, Hockstein N, Denstman F, Shakamuri S, Speicher DW, Weeraratna AT, Chao T, Vonderheide RH, Languino LR, Ordentlich P, Liu Q, Xu X, Lo A, Pure E, Zhang C, Loboda A, Sepulveda MA, Snyder LA, Gabrilovich DI. Cancer-associated fibroblasts neutralize the anti-tumor effect of CSF1 receptor blockade by inducing PMN-MDSC infiltration of tumors. Cancer Cell. 2017;32(5):654–668.e655. doi: 10.1016/j.ccell.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hendry S, Salgado R, Gevaert T, Russell PA, John T, Thapa B, Christie M, van de Vijver K, Estrada MV, Gonzalez-Ericsson PI, Sanders M, Solomon B, Solinas C, Van den Eynden G, Allory Y, Preusser M, Hainfellner J, Pruneri G, Vingiani A, Demaria S, Symmans F, Nuciforo P, Comerma L, Thompson EA, Lakhani S, Kim SR, Schnitt S, Colpaert C, Sotiriou C, Scherer SJ, Ignatiadis M, Badve S, Pierce RH, Viale G, Sirtaine N, Penault-Llorca F, Sugie T, Fineberg S, Paik S, Srinivasan A, Richardson A, Wang Y, Chmielik E, Brock J, Johnson DB, Balko J, Wienert S, Bossuyt V, Michiels S, Ternes N, Burchardi N, Luen SJ, Savas P, Klauschen F, Watson PH, Nelson BH, Criscitiello C, O’Toole S, Larsimont D, de Wind R, Curigliano G, Andre F, Lacroix-Triki M, van de Vijver M, Rojo F, Floris G, Bedri S, Sparano J, Rimm D, Nielsen T, Kos Z, Hewitt S, Singh B, Farshid G, Loibl S, Allison KH, Tung N, Adams S, Willard-Gallo K, Horlings HM, Gandhi L, Moreira A, Hirsch F, Dieci MV, Urbanowicz M, Brcic I, Korski K, Gaire F, Koeppen H, Lo A, Giltnane J, Rebelatto MC, Steele KE, Zha J, Emancipator K, Juco JW, Denkert C, Reis-Filho J, Loi S, Fox SB (2017) Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immuno-oncology biomarkers working group: part 2: TILs in melanoma, gastrointestinal tract carcinomas, non-small cell lung carcinoma and mesothelioma, endometrial and ovarian carcinomas, squamous cell carcinoma of the head and neck, genitourinary carcinomas, and primary brain tumors. Adv Anat Pathol. 10.1097/PAP.0000000000000161 [DOI] [PMC free article] [PubMed]
- 142.Reiser J, Banerjee A. Effector, memory, and dysfunctional CD8(+) T cell fates in the antitumor immune response. J Immunol Res. 2016;2016:8941260. doi: 10.1155/2016/8941260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kamphorst JJ, Gottlieb E. Cancer metabolism: friendly neighbours feed tumour cells. Nature. 2016;536(7617):401–402. doi: 10.1038/nature19420. [DOI] [PubMed] [Google Scholar]
- 144.Abu Aboud O, Habib SL, Trott J, Stewart B, Liang S, Chaudhari AJ, Sutcliffe J, Weiss RH. Glutamine addiction in kidney cancer suppresses oxidative stress and can be exploited for real-time imaging. Cancer Res. 2017;77(23):6746–6758. doi: 10.1158/0008-5472.Can-17-0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Niklison-Chirou MV, Erngren I, Engskog M, Haglof J, Picard D, Remke M, McPolin PHR, Selby M, Williamson D, Clifford SC, Michod D, Hadjiandreou M, Arvidsson T, Pettersson C, Melino G, Marino S. TAp73 is a marker of glutamine addiction in medulloblastoma. Genes Dev. 2017;31(17):1738–1753. doi: 10.1101/gad.302349.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Finicle BT, Jayashankar V, Edinger AL. Nutrient scavenging in cancer. Nat Rev Cancer. 2018;18(10):619–633. doi: 10.1038/s41568-018-0048-x. [DOI] [PubMed] [Google Scholar]
- 147.Fais S, Overholtzer M. Cell-in-cell phenomena in cancer. Nat Rev Cancer. 2018;18(12):758–766. doi: 10.1038/s41568-018-0073-9. [DOI] [PubMed] [Google Scholar]
- 148.Zhang Y, Ertl HC. Starved and asphyxiated: how can CD8(+) T cells within a tumor microenvironment prevent tumor progression. Front Immunol. 2016;7:32. doi: 10.3389/fimmu.2016.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Patsoukis N, Bardhan K, Chatterjee P, Sari D, Liu B, Bell LN, Karoly ED, Freeman GJ, Petkova V, Seth P, Li L, Boussiotis VA. PD-1 alters T-cell metabolic reprogramming by inhibiting glycolysis and promoting lipolysis and fatty acid oxidation. Nat Commun. 2015;6:6692–6692. doi: 10.1038/ncomms7692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Saeidi A, Zandi K, Cheok YY, Saeidi H, Wong WF, Lee CYQ, Cheong HC, Yong YK, Larsson M, Shankar EM. T-cell exhaustion in chronic infections: reversing the state of exhaustion and reinvigorating optimal protective immune responses. Front Immunol. 2018;9:2569. doi: 10.3389/fimmu.2018.02569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Darvin P, Toor SM, Sasidharan Nair V, Elkord E. Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp Mol Med. 2018;50(12):165–165. doi: 10.1038/s12276-018-0191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Palmer CS, Hussain T, Duette G, Weller TJ, Ostrowski M, Sada-Ovalle I, Crowe SM. Regulators of glucose metabolism in CD4(+) and CD8(+) T cells. Int Rev Immunol. 2016;35(6):477–488. doi: 10.3109/08830185.2015.1082178. [DOI] [PubMed] [Google Scholar]
- 153.Chang CH, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD, Chen Q, Gindin M, Gubin MM, van der Windt GJ, Tonc E, Schreiber RD, Pearce EJ, Pearce EL. Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell. 2015;162(6):1229–1241. doi: 10.1016/j.cell.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cham CM, Driessens G, O’Keefe JP, Gajewski TF. Glucose deprivation inhibits multiple key gene expression events and effector functions in CD8+ T cells. Eur J Immunol. 2008;38(9):2438–2450. doi: 10.1002/eji.200838289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Turkcan S, Kiru L, Naczynski DJ, Sasportas LS, Pratx G. Lactic acid accumulation in the tumor microenvironment suppresses (18)F-FDG uptake. Cancer Res. 2019;79(2):410–419. doi: 10.1158/0008-5472.Can-17-0492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kim JW, Tchernyshyov I, Semenza GL, Dang CV. HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3(3):177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 157.Papandreou I, Cairns RA, Fontana L, Lim AL, Denko NC. HIF-1 mediates adaptation to hypoxia by actively downregulating mitochondrial oxygen consumption. Cell Metab. 2006;3(3):187–197. doi: 10.1016/j.cmet.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 158.Noman MZ, Hasmim M, Messai Y, Terry S, Kieda C, Janji B, Chouaib S. Hypoxia: a key player in antitumor immune response. A review in the theme: cellular responses to hypoxia. Am J Phys Cell Physiol. 2015;309(9):C569–C579. doi: 10.1152/ajpcell.00207.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Larbi A, Zelba H, Goldeck D, Pawelec G. Induction of HIF-1alpha and the glycolytic pathway alters apoptotic and differentiation profiles of activated human T cells. J Leukoc Biol. 2010;87(2):265–273. doi: 10.1189/jlb.0509304. [DOI] [PubMed] [Google Scholar]
- 160.Tao JH, Barbi J, Pan F. Hypoxia-inducible factors in T lymphocyte differentiation and function. A review in the theme: cellular responses to hypoxia. Am J Phys Cell Physiol. 2015;309(9):C580–C589. doi: 10.1152/ajpcell.00204.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Takahashi S, Iizumi T, Mashima K, Abe T, Suzuki N (2014) Roles and regulation of ketogenesis in cultured astroglia and neurons under hypoxia and hypoglycemia. ASN Neuro 6(5). 10.1177/1759091414550997 [DOI] [PMC free article] [PubMed]
- 162.Sikalidis AK. Amino acids and immune response: a role for cysteine, glutamine, phenylalanine, tryptophan and arginine in T-cell function and cancer? Pathol Oncol Res. 2015;21(1):9–17. doi: 10.1007/s12253-014-9860-0. [DOI] [PubMed] [Google Scholar]
- 163.Sukumar M, Roychoudhuri R, Restifo NP. Nutrient competition: a new axis of tumor immunosuppression. Cell. 2015;162(6):1206–1208. doi: 10.1016/j.cell.2015.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Anderson KG, Stromnes IM, Greenberg PD. Obstacles posed by the tumor microenvironment to T cell activity: a case for synergistic therapies. Cancer Cell. 2017;31(3):311–325. doi: 10.1016/j.ccell.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Poh AR, Ernst M. Targeting macrophages in cancer: from bench to bedside. Front Oncol. 2018;8:49. doi: 10.3389/fonc.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Huang SC, Smith AM, Everts B, Colonna M, Pearce EL, Schilling JD, Pearce EJ. Metabolic reprogramming mediated by the mTORC2-IRF4 signaling axis is essential for macrophage alternative activation. Immunity. 2016;45(4):817–830. doi: 10.1016/j.immuni.2016.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Liu D, Chang C, Lu N, Wang X, Lu Q, Ren X, Ren P, Zhao D, Wang L, Zhu Y, He F, Tang L. Comprehensive proteomics analysis reveals metabolic reprogramming of tumor-associated macrophages stimulated by the tumor microenvironment. J Proteome Res. 2017;16(1):288–297. doi: 10.1021/acs.jproteome.6b00604. [DOI] [PubMed] [Google Scholar]
- 168.Netea-Maier RT, Smit JWA, Netea MG. Metabolic changes in tumor cells and tumor-associated macrophages: a mutual relationship. Cancer Lett. 2018;413:102–109. doi: 10.1016/j.canlet.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 169.Ocana MC, Martinez-Poveda B, Quesada AR, Medina MA (2018) Metabolism within the tumor microenvironment and its implication on cancer progression: an ongoing therapeutic target. Med Res Rev. 10.1002/med.21511 [DOI] [PubMed]
- 170.Mazzone M, Menga A, Castegna A. Metabolism and TAM functions—it takes two to tango. FEBS J. 2018;285(4):700–716. doi: 10.1111/febs.14295. [DOI] [PubMed] [Google Scholar]
- 171.Yan D, Adeshakin AO, Xu M, Afolabi LO, Zhang G, Chen YH, Wan X. Lipid metabolic pathways confer the immunosuppressive function of myeloid-derived suppressor cells in tumor. Front Immunol. 2019;10:1399. doi: 10.3389/fimmu.2019.01399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Eikawa S, Nishida M, Mizukami S, Yamazaki C, Nakayama E, Udono H. Immune-mediated antitumor effect by type 2 diabetes drug, metformin. Proc Natl Acad Sci U S A. 2015;112(6):1809–1814. doi: 10.1073/pnas.1417636112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zarrouk M, Finlay DK, Foretz M, Viollet B, Cantrell DA. Adenosine-mono-phosphate-activated protein kinase-independent effects of metformin in T cells. PLoS One. 2014;9(9):e106710. doi: 10.1371/journal.pone.0106710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Rao M, Dodoo E, Zumla A, Maeurer M. Immunometabolism and pulmonary infections: implications for protective immune responses and host-directed therapies. Front Microbiol. 2019;10:962. doi: 10.3389/fmicb.2019.00962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.De Vita MV, Scolfaro C, Santini B, Lezo A, Gobbi F, Buonfrate D, Kimani-Murage EW, Macharia T, Wanjohi M, Rovarini JM, Morino G. Malnutrition, morbidity and infection in the informal settlements of Nairobi, Kenya: an epidemiological study. Ital J Pediatr. 2019;45(1):12. doi: 10.1186/s13052-019-0607-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ibrahim MK, Zambruni M, Melby CL, Melby PC. Impact of childhood malnutrition on host defense and infection. Clin Microbiol Rev. 2017;30(4):919–971. doi: 10.1128/cmr.00119-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.DeBoer MD, Scharf RJ, Leite AM, Ferrer A, Havt A, Pinkerton R, Lima AA, Guerrant RL. Systemic inflammation, growth factors, and linear growth in the setting of infection and malnutrition. Nutrition. 2017;33:248–253. doi: 10.1016/j.nut.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Das D, Grais RF, Okiro EA, Stepniewska K, Mansoor R, van der Kam S, Terlouw DJ, Tarning J, Barnes KI, Guerin PJ. Complex interactions between malaria and malnutrition: a systematic literature review. BMC Med. 2018;16(1):186. doi: 10.1186/s12916-018-1177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Martin SJ, Sabina EP. Malnutrition and associated disorders in tuberculosis and its therapy. J Diet Suppl. 2019;16(5):602–610. doi: 10.1080/19390211.2018.1472165. [DOI] [PubMed] [Google Scholar]
- 180.Scrimshaw NS, SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr. 1997;66(2):464s–477s. doi: 10.1093/ajcn/66.2.464S. [DOI] [PubMed] [Google Scholar]
- 181.Kishton RJ, Sukumar M, Restifo NP. Metabolic regulation of T cell longevity and function in tumor immunotherapy. Cell Metab. 2017;26(1):94–109. doi: 10.1016/j.cmet.2017.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zukiewicz-Sobczak W, Wroblewska P, Zwolinski J, Chmielewska-Badora J, Adamczuk P, Krasowska E, Zagorski J, Oniszczuk A, Piatek J, Silny W. Obesity and poverty paradox in developed countries. Ann Agric Environ Med. 2014;21(3):590–594. doi: 10.5604/12321966.1120608. [DOI] [PubMed] [Google Scholar]
- 183.Harrison CA, Taren D. How poverty affects diet to shape the microbiota and chronic disease. Nat Rev Immunol. 2018;18(4):279–287. doi: 10.1038/nri.2017.121. [DOI] [PubMed] [Google Scholar]
- 184.Kumar H. Immunity and its role in white plague and obesity. Int Rev Immunol. 2019;38(4):129–130. doi: 10.1080/08830185.2019.1659528. [DOI] [PubMed] [Google Scholar]
- 185.Green WD, Beck MA. Obesity impairs the adaptive immune response to influenza virus. Ann Am Thorac Soc. 2017;14(Supplement_5):S406–s409. doi: 10.1513/AnnalsATS.201706-447AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Tagliabue C, Principi N, Giavoli C, Esposito S. Obesity: impact of infections and response to vaccines. Eur J Clin Microbiol Infect Dis. 2016;35(3):325–331. doi: 10.1007/s10096-015-2558-8. [DOI] [PubMed] [Google Scholar]
- 187.Beisel WR. History of nutritional immunology: introduction and overview. J Nutr. 1992;122(3 Suppl):591–596. doi: 10.1093/jn/122.suppl_3.591. [DOI] [PubMed] [Google Scholar]
- 188.Scrimshaw NS, Taylor CE, Gordon JE. Interactions of nutrition and infection. Am J Med Sci. 1959;237(3):367–403. [PubMed] [Google Scholar]
- 189.Scrimshaw NS, Taylor CE, Gordon JE. Interactions of nutrition and infection. WHO Chron. 1969;23(8):369–374. [PubMed] [Google Scholar]
- 190.Scrimshaw NS. Synergistic and antagonistic interactions of nutrition and infection. Fed Proc. 1966;25(6):1679–1681. [PubMed] [Google Scholar]
- 191.Scrimshaw NS. Historical concepts of interactions, synergism and antagonism between nutrition and infection. J Nutr. 2003;133(1):316s–321s. doi: 10.1093/jn/133.1.316S. [DOI] [PubMed] [Google Scholar]
- 192.Scrimshaw NS. INCAP studies of nutrition and infection. Food Nutr Bull. 2010;31(1):54–67. doi: 10.1177/156482651003100107. [DOI] [PubMed] [Google Scholar]
- 193.Ghosh S, Pellett PL, Aw-Hassan A, Mouneime Y, Smriga M, Scrimshaw NS. Impact of lysine-fortified wheat flour on morbidity and immunologic variables among members of rural families in northwest Syria. Food Nutr Bull. 2008;29(3):163–171. doi: 10.1177/156482650802900302. [DOI] [PubMed] [Google Scholar]
- 194.Ghosh S, Smriga M, Vuvor F, Suri D, Mohammed H, Armah SM, Scrimshaw NS. Effect of lysine supplementation on health and morbidity in subjects belonging to poor peri-urban households in Accra, Ghana. Am J Clin Nutr. 2010;92(4):928–939. doi: 10.3945/ajcn.2009.28834. [DOI] [PubMed] [Google Scholar]
- 195.Scrimshaw NS. INCAP studies of endemic goiter and its prevention. Food Nutr Bull. 2010;31(1):111–117. doi: 10.1177/156482651003100111. [DOI] [PubMed] [Google Scholar]
- 196.Scrimshaw NS. The origin and development of INCAP. Food Nutr Bull. 2010;31(1):4–8. doi: 10.1177/156482651003100102. [DOI] [PubMed] [Google Scholar]
- 197.Scrimshaw NS. History and early development of INCAP. J Nutr. 2010;140(2):394–396. doi: 10.3945/jn.109.114694. [DOI] [PubMed] [Google Scholar]
- 198.Scrimshaw NS, Viteri FE. INCAP studies of kwashiorkor and marasmus. Food Nutr Bull. 2010;31(1):34–41. doi: 10.1177/156482651003100105. [DOI] [PubMed] [Google Scholar]
- 199.Scrimshaw NS. Prologue: historical introduction. Immunonutrition in health and disease. Br J Nutr. 2007;98(Suppl 1):S3–S4. doi: 10.1017/s0007114507833034. [DOI] [PubMed] [Google Scholar]
- 200.Grimble RF. Immunonutrition. Curr Opin Gastroenterol. 2005;21(2):216–222. doi: 10.1097/01.mog.0000153360.90653.82. [DOI] [PubMed] [Google Scholar]
- 201.Cangelosi MJ, Rodday AM, Saunders T, Cohen JT. Evaluation of the economic burden of diseases associated with poor nutrition status. JPEN J Parenter Enteral Nutr. 2014;38(2 Suppl):35s–41s. doi: 10.1177/0148607113514612. [DOI] [PubMed] [Google Scholar]
- 202.Krawinkel MB. Interaction of nutrition and infections globally: an overview. Ann Nutr Metab. 2012;61(Suppl 1):39–45. doi: 10.1159/000345162. [DOI] [PubMed] [Google Scholar]
- 203.Calder PC. Feeding the immune system. Proc Nutr Soc. 2013;72(3):299–309. doi: 10.1017/s0029665113001286. [DOI] [PubMed] [Google Scholar]
- 204.Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13(11):633–643. doi: 10.1038/nrendo.2017.90. [DOI] [PubMed] [Google Scholar]
- 205.Jun JC, Devera R, Unnikrishnan D, Shin MK, Bevans-Fonti S, Yao Q, Rathore A, Younas H, Halberg N, Scherer PE, Polotsky VY. Adipose HIF-1alpha causes obesity by suppressing brown adipose tissue thermogenesis. J Mol Med. 2017;95(3):287–297. doi: 10.1007/s00109-016-1480-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ryan S. Adipose tissue inflammation by intermittent hypoxia: mechanistic link between obstructive sleep apnoea and metabolic dysfunction. J Physiol. 2017;595(8):2423–2430. doi: 10.1113/jp273312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Takikawa A, Mahmood A, Nawaz A, Kado T, Okabe K, Yamamoto S, Aminuddin A, Senda S, Tsuneyama K, Ikutani M, Watanabe Y, Igarashi Y, Nagai Y, Takatsu K, Koizumi K, Imura J, Goda N, Sasahara M, Matsumoto M, Saeki K, Nakagawa T, Fujisaka S, Usui I, Tobe K. HIF-1alpha in myeloid cells promotes adipose tissue remodeling toward insulin resistance. Diabetes. 2016;65(12):3649–3659. doi: 10.2337/db16-0012. [DOI] [PubMed] [Google Scholar]
- 208.Karki S, Ngo DTM, Farb MG, Park SY, Saggese SM, Hamburg NM, Carmine B, Hess DT, Walsh K, Gokce N. WNT5A regulates adipose tissue angiogenesis via antiangiogenic VEGF-A165b in obese humans. Am J Physiol Heart Circ Physiol. 2017;313(1):H200–h206. doi: 10.1152/ajpheart.00776.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Beigier-Bompadre M, Montagna GN, Kuhl AA, Lozza L, Weiner J, 3rd, Kupz A, Vogelzang A, Mollenkopf HJ, Lowe D, Bandermann S, Dorhoi A, Brinkmann V, Matuschewski K, Kaufmann SHE. Mycobacterium tuberculosis infection modulates adipose tissue biology. PLoS Pathog. 2017;13(10):e1006676. doi: 10.1371/journal.ppat.1006676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Han SJ, Glatman Zaretsky A, Andrade-Oliveira V, Collins N, Dzutsev A, Shaik J, Morais da Fonseca D, Harrison OJ, Tamoutounour S, Byrd AL, Smelkinson M, Bouladoux N, Bliska JB, Brenchley JM, Brodsky IE, Belkaid Y. White adipose tissue is a reservoir for memory T cells and promotes protective memory responses to infection. Immunity. 2017;47(6):1154–1168.e1156. doi: 10.1016/j.immuni.2017.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Hopkins BD, Goncalves MD, Cantley LC. Obesity and Cancer mechanisms: cancer metabolism. J Clin Oncol. 2016;34(35):4277–4283. doi: 10.1200/jco.2016.67.9712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Perna S, Peroni G, Faliva MA, Bartolo A, Naso M, Miccono A, Rondanelli M. Sarcopenia and sarcopenic obesity in comparison: prevalence, metabolic profile, and key differences. A cross-sectional study in Italian hospitalized elderly. Aging Clin Exp Res. 2017;29(6):1249–1258. doi: 10.1007/s40520-016-0701-8. [DOI] [PubMed] [Google Scholar]
- 213.Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia among hospitalized patients—a cross-sectional study. Clin Nutr. 2015;34(6):1239–1244. doi: 10.1016/j.clnu.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 214.Lee DC, Shook RP, Drenowatz C, Blair SN. Physical activity and sarcopenic obesity: definition, assessment, prevalence and mechanism. Future Sci OA. 2016;2(3):Fso127. doi: 10.4155/fsoa-2016-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31(12):1539–1547. doi: 10.1200/jco.2012.45.2722. [DOI] [PubMed] [Google Scholar]
- 216.Liu J, Motoyama S, Sato Y, Wakita A, Kawakita Y, Saito H, Minamiya Y. Decreased skeletal muscle mass after neoadjuvant therapy correlates with poor prognosis in patients with esophageal cancer. Anticancer Res. 2016;36(12):6677–6685. doi: 10.21873/anticanres.11278. [DOI] [PubMed] [Google Scholar]
- 217.Blauwhoff-Buskermolen S, Versteeg KS, de van der Schueren MA, den Braver NR, Berkhof J, Langius JA, Verheul HM. Loss of muscle mass during chemotherapy is predictive for poor survival of patients with metastatic colorectal cancer. J Clin Oncol. 2016;34(12):1339–1344. doi: 10.1200/jco.2015.63.6043. [DOI] [PubMed] [Google Scholar]
- 218.Cespedes Feliciano EM, Lee VS, Prado CM, Meyerhardt JA, Alexeeff S, Kroenke CH, Xiao J, Castillo AL, Caan BJ. Muscle mass at the time of diagnosis of nonmetastatic colon cancer and early discontinuation of chemotherapy, delays, and dose reductions on adjuvant FOLFOX: the C-SCANS study. Cancer. 2017;123(24):4868–4877. doi: 10.1002/cncr.30950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Argiles JM. The 2015 ESPEN sir David Cuthbertson lecture: inflammation as the driving force of muscle wasting in cancer. Clin Nutr. 2017;36(3):798–803. doi: 10.1016/j.clnu.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 220.VanderVeen BN, Fix DK, Carson JA. Disrupted skeletal muscle mitochondrial dynamics, mitophagy, and biogenesis during cancer cachexia: a role for inflammation. Oxidative Med Cell Longev. 2017;2017:3292087. doi: 10.1155/2017/3292087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Londhe P, Guttridge DC. Inflammation induced loss of skeletal muscle. Bone. 2015;80:131–142. doi: 10.1016/j.bone.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kim J, Lee J. Role of transforming growth factor-beta in muscle damage and regeneration: focused on eccentric muscle contraction. J Exerc Rehabil. 2017;13(6):621–626. doi: 10.12965/jer.1735072.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Flint TR, Fearon DT, Janowitz T. Connecting the metabolic and immune responses to cancer. Trends Mol Med. 2017;23(5):451–464. doi: 10.1016/j.molmed.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 224.Jezek J, Cooper KF, Strich R (2018) Reactive oxygen species and mitochondrial dynamics: the yin and yang of mitochondrial dysfunction and cancer progression. Antioxidants 7(1). 10.3390/antiox7010013 [DOI] [PMC free article] [PubMed]
- 225.Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107(6):931–936. doi: 10.1038/bjc.2012.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Pin F, Couch ME, Bonetto A. Preservation of muscle mass as a strategy to reduce the toxic effects of cancer chemotherapy on body composition. Curr Opin Support Palliat Care. 2018;12(4):420–426. doi: 10.1097/spc.0000000000000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542(7640):177–185. doi: 10.1038/nature21363. [DOI] [PubMed] [Google Scholar]
- 228.Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. 2018;31(3):231–236. doi: 10.1097/qco.0000000000000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Cunningham-Rundles S, Lin H, Ho-Lin D, Dnistrian A, Cassileth BR, Perlman JM. Role of nutrients in the development of neonatal immune response. Nutr Rev. 2009;67(Suppl 2):S152–S163. doi: 10.1111/j.1753-4887.2009.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 231.Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25(1):61–68. doi: 10.1177/0884533609358997. [DOI] [PubMed] [Google Scholar]
- 232.Keller HH, Vesnaver E, Davidson B, Allard J, Laporte M, Bernier P, Payette H, Jeejeebhoy K, Duerksen D, Gramlich L. Providing quality nutrition care in acute care hospitals: perspectives of nutrition care personnel. J Hum Nutr Diet. 2014;27(2):192–202. doi: 10.1111/jhn.12170. [DOI] [PubMed] [Google Scholar]
- 233.Rosen BS, Maddox PJ, Ray N. A position paper on how cost and quality reforms are changing healthcare in America: focus on nutrition. JPEN J Parenter Enteral Nutr. 2013;37(6):796–801. doi: 10.1177/0148607113492337. [DOI] [PubMed] [Google Scholar]
- 234.Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. Medsurg Nurs. 2013;22(3):147–165. [PubMed] [Google Scholar]
- 235.Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, Erickson N, Laviano A, Lisanti MP, Lobo DN, McMillan DC, Muscaritoli M, Ockenga J, Pirlich M, Strasser F, de van der Schueren M, Van Gossum A, Vaupel P, Weimann A. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187–1196. doi: 10.1016/j.clnu.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 236.Caillet P, Liuu E, Raynaud Simon A, Bonnefoy M, Guerin O, Berrut G, Lesourd B, Jeandel C, Ferry M, Rolland Y, Paillaud E. Association between cachexia, chemotherapy and outcomes in older cancer patients: a systematic review. Clin Nutr. 2017;36(6):1473–1482. doi: 10.1016/j.clnu.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 237.Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N, Miyake M, Hama N, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T. Prevalence of malnutrition among gastric cancer patients undergoing gastrectomy and optimal preoperative nutritional support for preventing surgical site infections. Ann Surg Oncol. 2015;22(Suppl 3):S778–S785. doi: 10.1245/s10434-015-4820-9. [DOI] [PubMed] [Google Scholar]
- 238.Kang MC, Kim JH, Ryu SW, Moon JY, Park JH, Park JK, Park JH, Baik HW, Seo JM, Son MW, Song GA, Shin DW, Shin YM, Ahn HY, Yang HK, Yu HC, Yun IJ, Lee JG, Lee JM, Lee JH, Lee TH, Yim H, Jeon HJ, Jung K, Jung MR, Jeong CY, Lim HS, Hong SK. Prevalence of malnutrition in hospitalized patients: a multicenter cross-sectional study. J Korean Med Sci. 2018;33(2):e10. doi: 10.3346/jkms.2018.33.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Planas M, Alvarez-Hernandez J, Leon-Sanz M, Celaya-Perez S, Araujo K, Garcia de Lorenzo A. Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES(R) study. Support Care Cancer. 2016;24(1):429–435. doi: 10.1007/s00520-015-2813-7. [DOI] [PubMed] [Google Scholar]
- 240.Na BG, Han SS, Cho YA, Wie GA, Kim JY, Lee JM, Lee SD, Kim SH, Park SJ. Nutritional status of patients with cancer: a prospective cohort study of 1,588 hospitalized patients. Nutr Cancer. 2018;70(8):1228–1236. doi: 10.1080/01635581.2019.1578392. [DOI] [PubMed] [Google Scholar]
- 241.Matson V, Fessler J, Bao R, Chongsuwat T, Zha Y, Alegre ML, Luke JJ, Gajewski TF. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science. 2018;359(6371):104–108. doi: 10.1126/science.aao3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillere R, Fluckiger A, Messaoudene M, Rauber C, Roberti MP, Fidelle M, Flament C, Poirier-Colame V, Opolon P, Klein C, Iribarren K, Mondragon L, Jacquelot N, Qu B, Ferrere G, Clemenson C, Mezquita L, Masip JR, Naltet C, Brosseau S, Kaderbhai C, Richard C, Rizvi H, Levenez F, Galleron N, Quinquis B, Pons N, Ryffel B, Minard-Colin V, Gonin P, Soria JC, Deutsch E, Loriot Y, Ghiringhelli F, Zalcman G, Goldwasser F, Escudier B, Hellmann MD, Eggermont A, Raoult D, Albiges L, Kroemer G, Zitvogel L. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359(6371):91–97. doi: 10.1126/science.aan3706. [DOI] [PubMed] [Google Scholar]
- 243.Wirbel J, Pyl PT, Kartal E, Zych K, Kashani A, Milanese A, Fleck JS, Voigt AY, Palleja A, Ponnudurai R, Sunagawa S, Coelho LP, Schrotz-King P, Vogtmann E, Habermann N, Nimeus E, Thomas AM, Manghi P, Gandini S, Serrano D, Mizutani S, Shiroma H, Shiba S, Shibata T, Yachida S, Yamada T, Waldron L, Naccarati A, Segata N, Sinha R, Ulrich CM, Brenner H, Arumugam M, Bork P, Zeller G. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat Med. 2019;25(4):679–689. doi: 10.1038/s41591-019-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Cheung SG, Goldenthal AR, Uhlemann AC, Mann JJ, Miller JM, Sublette ME. Systematic review of gut microbiota and major depression. Front Psychiatry. 2019;10:34. doi: 10.3389/fpsyt.2019.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Lazar V, Ditu LM, Pircalabioru GG, Picu A, Petcu L, Cucu N, Chifiriuc MC. Gut microbiota, host organism, and diet trialogue in diabetes and obesity. Front Nutr. 2019;6:21. doi: 10.3389/fnut.2019.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Lee KH, Gordon A, Shedden K, Kuan G, Ng S, Balmaseda A, Foxman B. The respiratory microbiome and susceptibility to influenza virus infection. PLoS One. 2019;14(1):e0207898. doi: 10.1371/journal.pone.0207898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Namasivayam S, Sher A, Glickman MS, Wipperman MF (2018) The microbiome and tuberculosis: early evidence for cross talk. MBio 9(5). 10.1128/mBio.01420-18 [DOI] [PMC free article] [PubMed]
- 248.Zimmermann M, Zimmermann-Kogadeeva M, Wegmann R, Goodman AL (2019) Separating host and microbiome contributions to drug pharmacokinetics and toxicity. Science 363(6427). 10.1126/science.aat9931 [DOI] [PMC free article] [PubMed]
- 249.Thomas S, Izard J, Walsh E, Batich K, Chongsathidkiet P, Clarke G, Sela DA, Muller AJ, Mullin JM, Albert K, Gilligan JP, DiGuilio K, Dilbarova R, Alexander W, Prendergast GC. The host microbiome regulates and maintains human health: a primer and perspective for non-microbiologists. Cancer Res. 2017;77(8):1783–1812. doi: 10.1158/0008-5472.Can-16-2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Karl JP, Hatch AM, Arcidiacono SM, Pearce SC, Pantoja-Feliciano IG, Doherty LA, Soares JW. Effects of psychological, environmental and physical stressors on the gut microbiota. Front Microbiol. 2018;9:2013. doi: 10.3389/fmicb.2018.02013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Picca A, Fanelli F, Calvani R, Mule G, Pesce V, Sisto A, Pantanelli C, Bernabei R, Landi F, Marzetti E. Gut dysbiosis and muscle aging: searching for novel targets against sarcopenia. Mediat Inflamm. 2018;2018:7026198. doi: 10.1155/2018/7026198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.LeBlanc JG, Milani C, de Giori GS, Sesma F, van Sinderen D, Ventura M. Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr Opin Biotechnol. 2013;24(2):160–168. doi: 10.1016/j.copbio.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 253.Mills S, Stanton C, Lane JA, Smith GJ, Ross RP (2019) Precision nutrition and the microbiome, part I: current state of the science. Nutrients 11(4). 10.3390/nu11040923 [DOI] [PMC free article] [PubMed]
- 254.Claesson MJ, Cusack S, O’Sullivan O, Greene-Diniz R, de Weerd H, Flannery E, Marchesi JR, Falush D, Dinan T, Fitzgerald G, Stanton C, van Sinderen D, O’Connor M, Harnedy N, O’Connor K, Henry C, O’Mahony D, Fitzgerald AP, Shanahan F, Twomey C, Hill C, Ross RP, O’Toole PW. Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4586–4591. doi: 10.1073/pnas.1000097107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Claesson MJ, Jeffery IB, Conde S, Power SE, O’Connor EM, Cusack S, Harris HM, Coakley M, Lakshminarayanan B, O’Sullivan O, Fitzgerald GF, Deane J, O’Connor M, Harnedy N, O’Connor K, O’Mahony D, van Sinderen D, Wallace M, Brennan L, Stanton C, Marchesi JR, Fitzgerald AP, Shanahan F, Hill C, Ross RP, O’Toole PW. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488(7410):178–184. doi: 10.1038/nature11319. [DOI] [PubMed] [Google Scholar]
- 256.Grosicki GJ, Fielding RA, Lustgarten MS. Gut microbiota contribute to age-related changes in skeletal muscle size, composition, and function: biological basis for a gut-muscle axis. Calcif Tissue Int. 2018;102(4):433–442. doi: 10.1007/s00223-017-0345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, Abrouk M, Farahnik B, Nakamura M, Zhu TH, Bhutani T, Liao W. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15(1):73. doi: 10.1186/s12967-017-1175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Romano KA, Vivas EI, Amador-Noguez D, Rey FE. Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. MBio. 2015;6(2):e02481. doi: 10.1128/mBio.02481-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Bibbo S, Ianiro G, Giorgio V, Scaldaferri F, Masucci L, Gasbarrini A, Cammarota G. The role of diet on gut microbiota composition. Eur Rev Med Pharmacol Sci. 2016;20(22):4742–4749. [PubMed] [Google Scholar]
- 260.Coelho OGL, Candido FG, Alfenas RCG (2018) Dietary fat and gut microbiota: mechanisms involved in obesity control. Crit Rev Food Sci Nutr:1–9. 10.1080/10408398.2018.1481821 [DOI] [PubMed]
- 261.Wu GD, Chen J, Hoffmann C, Bittinger K, Chen YY, Keilbaugh SA, Bewtra M, Knights D, Walters WA, Knight R, Sinha R, Gilroy E, Gupta K, Baldassano R, Nessel L, Li H, Bushman FD, Lewis JD. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334(6052):105–108. doi: 10.1126/science.1208344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Lopez-Legarrea P, Fuller NR, Zulet MA, Martinez JA, Caterson ID. The influence of Mediterranean, carbohydrate and high protein diets on gut microbiota composition in the treatment of obesity and associated inflammatory state. Asia Pac J Clin Nutr. 2014;23(3):360–368. doi: 10.6133/apjcn.2014.23.3.16. [DOI] [PubMed] [Google Scholar]
- 263.Biesalski HK. Nutrition meets the microbiome: micronutrients and the microbiota. Ann N Y Acad Sci. 2016;1372(1):53–64. doi: 10.1111/nyas.13145. [DOI] [PubMed] [Google Scholar]
- 264.Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, Alam MA, Benezra A, DeStefano J, Meier MF, Muegge BD, Barratt MJ, VanArendonk LG, Zhang Q, Province MA, Petri WA, Jr, Ahmed T, Gordon JI. Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature. 2014;510(7505):417–421. doi: 10.1038/nature13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Clooney AG, Sutton TDS, Shkoporov AN, Holohan RK, Daly KM, O’Regan O, Ryan FJ, Draper LA, Plevy SE, Ross RP, Hill C. Whole-virome analysis sheds light on viral dark matter in inflammatory bowel disease. Cell Host Microbe. 2019;26(6):764–778 e765. doi: 10.1016/j.chom.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 266.Shkoporov AN, Clooney AG, Sutton TDS, Ryan FJ, Daly KM, Nolan JA, McDonnell SA, Khokhlova EV, Draper LA, Forde A, Guerin E, Velayudhan V, Ross RP, Hill C. The human gut virome is highly diverse, stable, and individual specific. Cell Host Microbe. 2019;26(4):527–541 e525. doi: 10.1016/j.chom.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 267.Tabatabaeizadeh SA, Tafazoli N, Ferns GA, Avan A, Ghayour-Mobarhan M. Vitamin D, the gut microbiome and inflammatory bowel disease. J Res Med Sci. 2018;23:75. doi: 10.4103/jrms.JRMS_606_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Montoya D, Inkeles MS, Liu PT, Realegeno S, Teles RM, Vaidya P, Munoz MA, Schenk M, Swindell WR, Chun R, Zavala K, Hewison M, Adams JS, Horvath S, Pellegrini M, Bloom BR, Modlin RL. IL-32 is a molecular marker of a host defense network in human tuberculosis. Sci Transl Med. 2014;6(250):250ra114. doi: 10.1126/scitranslmed.3009546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Kuroda K, Okumura K, Isogai H, Isogai E. The human cathelicidin antimicrobial peptide LL-37 and mimics are potential anticancer drugs. Front Oncol. 2015;5:144. doi: 10.3389/fonc.2015.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Cuperus T, Kraaij MD, Zomer AL, van Dijk A, Haagsman HP. Immunomodulation and effects on microbiota after in ovo administration of chicken cathelicidin-2. PLoS One. 2018;13(6):e0198188. doi: 10.1371/journal.pone.0198188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Yoshimura T, McLean MH, Dzutsev AK, Yao X, Chen K, Huang J, Gong W, Zhou J, Xiang Y, J HB, O’Huigin C, Thovarai V, Tessarollo L, Durum SK, Trinchieri G, Bian XW, Wang JM. The antimicrobial peptide CRAMP is essential for colon homeostasis by maintaining microbiota balance. J Immunol. 2018;200(6):2174–2185. doi: 10.4049/jimmunol.1602073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Dang AT, Marsland BJ. Microbes, metabolites, and the gut-lung axis. Mucosal Immunol. 2019;12(4):843–850. doi: 10.1038/s41385-019-0160-6. [DOI] [PubMed] [Google Scholar]
- 273.Bacher P, Hohnstein T, Beerbaum E, Rocker M, Blango MG, Kaufmann S, Rohmel J, Eschenhagen P, Grehn C, Seidel K, Rickerts V, Lozza L, Stervbo U, Nienen M, Babel N, Milleck J, Assenmacher M, Cornely OA, Ziegler M, Wisplinghoff H, Heine G, Worm M, Siegmund B, Maul J, Creutz P, Tabeling C, Ruwwe-Glosenkamp C, Sander LE, Knosalla C, Brunke S, Hube B, Kniemeyer O, Brakhage AA, Schwarz C, Scheffold A. Human anti-fungal Th17 immunity and pathology rely on cross-reactivity against Candida albicans. Cell. 2019;176(6):1340–1355.e1315. doi: 10.1016/j.cell.2019.01.041. [DOI] [PubMed] [Google Scholar]
- 274.Mjosberg J, Rao A. Lung inflammation originating in the gut. Science. 2018;359(6371):36–37. doi: 10.1126/science.aar4301. [DOI] [PubMed] [Google Scholar]
- 275.Baktash A, Terveer EM, Zwittink RD, Hornung BVH, Corver J, Kuijper EJ, Smits WK. Mechanistic insights in the success of fecal microbiota transplants for the treatment of Clostridium difficile infections. Front Microbiol. 2018;9:1242. doi: 10.3389/fmicb.2018.01242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Hudson LE, Anderson SE, Corbett AH, Lamb TJ. Gleaning insights from fecal microbiota transplantation and probiotic studies for the rational design of combination microbial therapies. Clin Microbiol Rev. 2017;30(1):191–231. doi: 10.1128/cmr.00049-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Hughes RL, Marco ML, Hughes JP, Keim NL, Kable ME (2019) The role of the gut microbiome in predicting response to diet and the development of precision nutrition models-part I: overview of current methods. Adv Nutr. 10.1093/advances/nmz022 [DOI] [PMC free article] [PubMed]
- 278.Aversa Z, Costelli P, Muscaritoli M. Cancer-induced muscle wasting: latest findings in prevention and treatment. Ther Adv Med Oncol. 2017;9(5):369–382. doi: 10.1177/1758834017698643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Fukawa T, Yan-Jiang BC, Min-Wen JC, Jun-Hao ET, Huang D, Qian CN, Ong P, Li Z, Chen S, Mak SY, Lim WJ, Kanayama HO, Mohan RE, Wang RR, Lai JH, Chua C, Ong HS, Tan KK, Ho YS, Tan IB, Teh BT, Shyh-Chang N. Excessive fatty acid oxidation induces muscle atrophy in cancer cachexia. Nat Med. 2016;22(6):666–671. doi: 10.1038/nm.4093. [DOI] [PubMed] [Google Scholar]
- 280.Sturgeon KM, Mathis KM, Rogers CJ, Schmitz KH, Waning DL. Cancer- and chemotherapy-induced musculoskeletal degradation. JBMR Plus. 2019;3(3):e10187. doi: 10.1002/jbm4.10187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Ikemoto S, Sugimura K, Yoshida N, Wada S, Yamamoto K, Kishimoto T. TNF alpha, IL-1 beta and IL-6 production by peripheral blood monocytes in patients with renal cell carcinoma. Anticancer Res. 2000;20(1a):317–321. [PubMed] [Google Scholar]
- 282.Matthys P, Billiau A. Cytokines and cachexia. Nutrition. 1997;13(9):763–770. doi: 10.1016/S0899-9007(97)00185-8. [DOI] [PubMed] [Google Scholar]
- 283.Patel HJ, Patel BM. TNF-alpha and cancer cachexia: molecular insights and clinical implications. Life Sci. 2017;170:56–63. doi: 10.1016/j.lfs.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 284.Shyh-Chang N. Metabolic changes during cancer cachexia pathogenesis. Adv Exp Med Biol. 2017;1026:233–249. doi: 10.1007/978-981-10-6020-5_11. [DOI] [PubMed] [Google Scholar]
- 285.Fearon KC, Glass DJ, Guttridge DC. Cancer cachexia: mediators, signaling, and metabolic pathways. Cell Metab. 2012;16(2):153–166. doi: 10.1016/j.cmet.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 286.Daas SI, Rizeq BR, Nasrallah GK. Adipose tissue dysfunction in cancer cachexia. J Cell Physiol. 2018;234(1):13–22. doi: 10.1002/jcp.26811. [DOI] [PubMed] [Google Scholar]
- 287.Dalal S. Lipid metabolism in cancer cachexia. Ann Palliat Med. 2019;8(1):13–23. doi: 10.21037/apm.2018.10.01. [DOI] [PubMed] [Google Scholar]
- 288.Sakuma K, Aoi W, Yamaguchi A. Molecular mechanism of sarcopenia and cachexia: recent research advances. Pflugers Arch. 2017;469(5–6):573–591. doi: 10.1007/s00424-016-1933-3. [DOI] [PubMed] [Google Scholar]
- 289.Sandri M. Protein breakdown in cancer cachexia. Semin Cell Dev Biol. 2016;54:11–19. doi: 10.1016/j.semcdb.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 290.Liu Z, Sin KWT, Ding H, Doan HA, Gao S, Miao H, Wei Y, Wang Y, Zhang G, Li YP. p38beta MAPK mediates ULK1-dependent induction of autophagy in skeletal muscle of tumor-bearing mice. Cell Stress. 2018;2(11):311–324. doi: 10.15698/cst2018.11.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Marzetti E, Lorenzi M, Landi F, Picca A, Rosa F, Tanganelli F, Galli M, Doglietto GB, Pacelli F, Cesari M, Bernabei R, Calvani R, Bossola M. Altered mitochondrial quality control signaling in muscle of old gastric cancer patients with cachexia. Exp Gerontol. 2017;87(Pt A):92–99. doi: 10.1016/j.exger.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 292.Pin F, Barreto R, Couch ME, Bonetto A, O’Connell TM. Cachexia induced by cancer and chemotherapy yield distinct perturbations to energy metabolism. J Cachexia Sarcopenia Muscle. 2019;10(1):140–154. doi: 10.1002/jcsm.12360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Belloum Y, Rannou-Bekono F, Favier FB. Cancer-induced cardiac cachexia: pathogenesis and impact of physical activity (review) Oncol Rep. 2017;37(5):2543–2552. doi: 10.3892/or.2017.5542. [DOI] [PubMed] [Google Scholar]
- 294.Coletti D. Chemotherapy-induced muscle wasting: an update. Eur J Transl Myol. 2018;28(2):7587. doi: 10.4081/ejtm.2018.7587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Moreira-Pais A, Ferreira R, Gil da Costa R. Platinum-induced muscle wasting in cancer chemotherapy: mechanisms and potential targets for therapeutic intervention. Life Sci. 2018;208:1–9. doi: 10.1016/j.lfs.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 296.Akyol M, Demir L, Alacacioglu A, Ellidokuz H, Kucukzeybek Y, Yildiz Y, Gumus Z, Bayoglu V, Yildiz I, Salman T, Varol U, Kucukzeybek B, Demir L, Dirican A, Sutcu R, Tarhan MO. The effects of adjuvant endocrine treatment on serum leptin, serum adiponectin and body composition in patients with breast cancer: the Izmir Oncology Group (IZOG) Study. Chemotherapy. 2016;61(2):57–64. doi: 10.1159/000440944. [DOI] [PubMed] [Google Scholar]
- 297.Capozzi LC, McNeely ML, Lau HY, Reimer RA, Giese-Davis J, Fung TS, Culos-Reed SN. Patient-reported outcomes, body composition, and nutrition status in patients with head and neck cancer: results from an exploratory randomized controlled exercise trial. Cancer. 2016;122(8):1185–1200. doi: 10.1002/cncr.29863. [DOI] [PubMed] [Google Scholar]
- 298.Pedersen B, Delmar C, Bendtsen MD, Bosaeus I, Carus A, Falkmer U, Groenkjaer M. Changes in weight and body composition among women with breast cancer during and after adjuvant treatment: a prospective follow-up study. Cancer Nurs. 2017;40(5):369–376. doi: 10.1097/ncc.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 299.Rier HN, Jager A, Sleijfer S, van Rosmalen J, Kock M, Levin MD. Changes in body composition and muscle attenuation during taxane-based chemotherapy in patients with metastatic breast cancer. Breast Cancer Res Treat. 2018;168(1):95–105. doi: 10.1007/s10549-017-4574-0. [DOI] [PubMed] [Google Scholar]
- 300.Blackburn GL. Nutrition and inflammatory events: highly unsaturated fatty acids (omega-3 vs omega-6) in surgical injury. Proc Soc Exp Biol Med. 1992;200(2):183–188. doi: 10.3181/00379727-200-43414. [DOI] [PubMed] [Google Scholar]
- 301.Grimble RF. Dietary manipulation of the inflammatory response. Proc Nutr Soc. 1992;51(2):285–294. doi: 10.1079/PNS19920039. [DOI] [PubMed] [Google Scholar]
- 302.Lefkowith JB, Morrison A, Lee V, Rogers M. Manipulation of the acute inflammatory response by dietary polyunsaturated fatty acid modulation. J Immunol. 1990;145(5):1523–1529. [PubMed] [Google Scholar]
- 303.Wan JM, Haw MP, Blackburn GL. Nutrition, immune function, and inflammation: an overview. Proc Nutr Soc. 1989;48(3):315–335. doi: 10.1079/PNS19890048. [DOI] [PubMed] [Google Scholar]
- 304.Grimble RF. Nutritional modulation of immune function. Proc Nutr Soc. 2001;60(3):389–397. doi: 10.1079/PNS2001102. [DOI] [PubMed] [Google Scholar]
- 305.Grimble RF. Nutritional antioxidants and the modulation of inflammation: theory and practice. New Horiz. 1994;2(2):175–185. [PubMed] [Google Scholar]
- 306.Gostner JM, Becker K, Ueberall F, Fuchs D. The good and bad of antioxidant foods: an immunological perspective. Food Chem Toxicol. 2015;80:72–79. doi: 10.1016/j.fct.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 307.Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hutterer E, Isenring E, Kaasa S, Krznaric Z, Laird B, Larsson M, Laviano A, Muhlebach S, Muscaritoli M, Oldervoll L, Ravasco P, Solheim T, Strasser F, de van der Schueren M, Preiser JC. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48. doi: 10.1016/j.clnu.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 308.Çehrelli R. Molecular nutritional immunology and cancer. J Oncol Sci. 2018;4:40–46. doi: 10.1001/jamaoncol.2017.2303. [DOI] [Google Scholar]
- 309.Grimble G (1994) Possible role of short-term parenteral nutrition with fat emulsions for development of haemophagocytosis with multiple organ failure in a patient with traumatic brain injury Roth B, Grande PO, Nillson-Ehle P and Eliasson I. Intensive Care Med 1993; 19: 111-114. Clin Nutr 13 (2):127 [DOI] [PubMed]
- 310.Grimble G (1994) Can daily dietary arginine supplement affect the function and subpopulation of lymphocytes in patients with advanced gastric cancer? Wu C-W, Chi C-W, Chiu C-C, Liu W-Y, P’eng F-K and Wang S-R. Digestion 1993; 54: 118-124. Clin Nutr 13 (2):127–128 [DOI] [PubMed]
- 311.Ramalho R, Ramalho P, Couto N, Pereira P. Omega-3 therapeutic supplementation in a patient with metastatic adenocarcinoma of the pancreas with muscle mass depletion. Eur J Clin Nutr. 2017;71(6):795–797. doi: 10.1038/ejcn.2017.47. [DOI] [PubMed] [Google Scholar]
- 312.Burns CP, Halabi S, Clamon G, Kaplan E, Hohl RJ, Atkins JN, Schwartz MA, Wagner BA, Paskett E. Phase II study of high-dose fish oil capsules for patients with cancer-related cachexia. Cancer. 2004;101(2):370–378. doi: 10.1002/cncr.20362. [DOI] [PubMed] [Google Scholar]
- 313.Rosenthal MD, Carrott PW, Patel J, Kiraly L, Martindale RG. Parenteral or enteral arginine supplementation safety and efficacy. J Nutr. 2016;146(12):2594s–2600s. doi: 10.3945/jn.115.228544. [DOI] [PubMed] [Google Scholar]
- 314.Mariette C. Immunonutrition. J Visc Surg. 2015;152(Suppl 1):S14–S17. doi: 10.1016/s1878-7886(15)30005-9. [DOI] [PubMed] [Google Scholar]
- 315.Martin RC, 2nd, Agle S, Schlegel M, Hayat T, Scoggins CR, McMasters KM, Philips P. Efficacy of preoperative immunonutrition in locally advanced pancreatic cancer undergoing irreversible electroporation (IRE) Eur J Surg Oncol. 2017;43(4):772–779. doi: 10.1016/j.ejso.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 316.Peker KD, Ozkanli SS, Akyuz C, Uzun O, Yasar NF, Duman M, Yol S. Preoperative immunonutrition regulates tumor infiltrative lymphocytes and increases tumor angiogenesis in gastric cancer patients. Arch Med Sci. 2017;13(6):1365–1372. doi: 10.5114/aoms.2016.60054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Thornblade LW, Varghese TK, Jr, Shi X, Johnson EK, Bastawrous A, Billingham RP, Thirlby R, Fichera A, Flum DR. Preoperative immunonutrition and elective colorectal resection outcomes. Dis Colon Rectum. 2017;60(1):68–75. doi: 10.1097/dcr.0000000000000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Howes N, Atkinson C, Thomas S, Lewis SJ. Immunonutrition for patients undergoing surgery for head and neck cancer. Cochrane Database Syst Rev. 2018;8:Cd010954. doi: 10.1002/14651858.CD010954.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Mueller SA, Mayer C, Bojaxhiu B, Aeberhard C, Schuetz P, Stanga Z, Giger R. Effect of preoperative immunonutrition on complications after salvage surgery in head and neck cancer. J Otolaryngol Head Neck Surg. 2019;48(1):25. doi: 10.1186/s40463-019-0345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Song GM, Tian X, Liang H, Yi LJ, Zhou JG, Zeng Z, Shuai T, Ou YX, Zhang L, Wang Y. Role of enteral immunonutrition in patients undergoing surgery for gastric cancer: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015;94(31):e1311. doi: 10.1097/md.0000000000001311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Alito MA, de Aguilar-Nascimento JE. Multimodal perioperative care plus immunonutrition versus traditional care in total hip arthroplasty: a randomized pilot study. Nutr J. 2016;15:34. doi: 10.1186/s12937-016-0153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Kamocki Z, Matowicka-Karna J, Gryko M, Zareba K, Kedra B, Kemona H. The effect of perioperative immunonutrition on the phagocytic activity of blood platelets in advanced gastric cancer patients. Clin Dev Immunol. 2013;2013:435672. doi: 10.1155/2013/435672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Plank LD, Mathur S, Gane EJ, Peng SL, Gillanders LK, McIlroy K, Chavez CP, Calder PC, McCall JL. Perioperative immunonutrition in patients undergoing liver transplantation: a randomized double-blind trial. Hepatology. 2015;61(2):639–647. doi: 10.1002/hep.27433. [DOI] [PubMed] [Google Scholar]
- 324.Camp KM, Trujillo E. Position of the academy of nutrition and dietetics: nutritional genomics. J Acad Nutr Diet. 2014;114(2):299–312. doi: 10.1016/j.jand.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 325.Cui J, Zhou B, Ross SA, Zempleni J. Nutrition, microRNAs, and human health. Adv Nutr. 2017;8(1):105–112. doi: 10.3945/an.116.013839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Fenech MF. Nutriomes and personalised nutrition for DNA damage prevention, telomere integrity maintenance and cancer growth control. Cancer Treat Res. 2014;159:427–441. doi: 10.1007/978-3-642-38007-5_24. [DOI] [PubMed] [Google Scholar]
- 327.Bordoni A, Capozzi F. Foodomics for healthy nutrition. Curr Opin Clin Nutr Metab Care. 2014;17(5):418–424. doi: 10.1097/mco.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 328.Ramos-Lopez O, Milagro FI, Allayee H, Chmurzynska A, Choi MS, Curi R, De Caterina R, Ferguson LR, Goni L, Kang JX, Kohlmeier M, Marti A, Moreno LA, Perusse L, Prasad C, Qi L, Reifen R, Riezu-Boj JI, San-Cristobal R, Santos JL, Martinez JA. Guide for current nutrigenetic, nutrigenomic, and nutriepigenetic approaches for precision nutrition involving the prevention and management of chronic diseases associated with obesity. J Nutrigenet Nutrigenomics. 2017;10(1–2):43–62. doi: 10.1159/000477729. [DOI] [PubMed] [Google Scholar]
- 329.Remely M, Stefanska B, Lovrecic L, Magnet U, Haslberger AG. Nutriepigenomics: the role of nutrition in epigenetic control of human diseases. Curr Opin Clin Nutr Metab Care. 2015;18(4):328–333. doi: 10.1097/mco.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 330.Minihane AM, Khan S, Leigh-Firbank EC, Talmud P, Wright JW, Murphy MC, Griffin BA, Williams CM. ApoE polymorphism and fish oil supplementation in subjects with an atherogenic lipoprotein phenotype. Arterioscler Thromb Vasc Biol. 2000;20(8):1990–1997. doi: 10.1161/01.ATV.20.8.1990. [DOI] [PubMed] [Google Scholar]
- 331.Grimble RF, Howell WM, O’Reilly G, Turner SJ, Markovic O, Hirrell S, East JM, Calder PC. The ability of fish oil to suppress tumor necrosis factor alpha production by peripheral blood mononuclear cells in healthy men is associated with polymorphisms in genes that influence tumor necrosis factor alpha production. Am J Clin Nutr. 2002;76(2):454–459. doi: 10.1093/ajcn/76.2.454. [DOI] [PubMed] [Google Scholar]
- 332.Paoloni-Giacobino A, Grimble R, Pichard C. Genomic interactions with disease and nutrition. Clin Nutr. 2003;22(6):507–514. doi: 10.1016/S0261-5614(03)00091-8. [DOI] [PubMed] [Google Scholar]
- 333.Costa MD, Vieira de Melo CY, Amorim AC, Cipriano Torres Dde O, Dos Santos AC. Association between nutritional status, inflammatory condition, and prognostic indexes with postoperative complications and clinical outcome of patients with gastrointestinal neoplasia. Nutr Cancer. 2016;68(7):1108–1114. doi: 10.1080/01635581.2016.1206578. [DOI] [PubMed] [Google Scholar]
- 334.Perez-Cruz E, Camacho-Limas CP. Association of nutritional status and functional capacity in gastrointestinal cancer patients. Gac Med Mex. 2017;153(5):575–580. doi: 10.24875/gmm.17002776. [DOI] [PubMed] [Google Scholar]
- 335.Wang Y, Zheng J, Gao Z, Han X, Qiu F. Investigation on nutritional risk assessment and nutritional support status of surgical patients with colorectal cancer. J buon. 2018;23(1):62–67. [PubMed] [Google Scholar]
- 336.Zhang L, Lu Y, Fang Y. Nutritional status and related factors of patients with advanced gastrointestinal cancer. Br J Nutr. 2014;111(7):1239–1244. doi: 10.1017/s000711451300367x. [DOI] [PubMed] [Google Scholar]
- 337.Guertin MH, Robitaille K, Pelletier JF, Duchesne T, Julien P, Savard J, Bairati I, Fradet V. Effects of concentrated long-chain omega-3 polyunsaturated fatty acid supplementation before radical prostatectomy on prostate cancer proliferation, inflammation, and quality of life: study protocol for a phase IIb, randomized, double-blind, placebo-controlled trial. BMC Cancer. 2018;18(1):64. doi: 10.1186/s12885-017-3979-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Kopeina GS, Senichkin VV, Zhivotovsky B. Caloric restriction—a promising anti-cancer approach: from molecular mechanisms to clinical trials. Biochim Biophys Acta Rev Cancer. 2017;1867(1):29–41. doi: 10.1016/j.bbcan.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 339.Lien EC, Lau AN, Vander Heiden MG. Putting the K(+) in K(+)aloric restriction. Immunity. 2019;50(5):1129–1131. doi: 10.1016/j.immuni.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 340.Vodnala SK, Eil R, Kishton RJ, Sukumar M, Yamamoto TN, Ha NH, Lee PH, Shin M, Patel SJ, Yu Z, Palmer DC, Kruhlak MJ, Liu X, Locasale JW, Huang J, Roychoudhuri R, Finkel T, Klebanoff CA, Restifo NP (2019) T cell stemness and dysfunction in tumors are triggered by a common mechanism. Science 363(6434). 10.1126/science.aau0135 [DOI] [PMC free article] [PubMed]
- 341.Eil R, Vodnala SK, Clever D, Klebanoff CA, Sukumar M, Pan JH, Palmer DC, Gros A, Yamamoto TN, Patel SJ, Guittard GC, Yu Z, Carbonaro V, Okkenhaug K, Schrump DS, Linehan WM, Roychoudhuri R, Restifo NP. Ionic immune suppression within the tumour microenvironment limits T cell effector function. Nature. 2016;537(7621):539–543. doi: 10.1038/nature19364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Husson MO, Ley D, Portal C, Gottrand M, Hueso T, Desseyn JL, Gottrand F. Modulation of host defence against bacterial and viral infections by omega-3 polyunsaturated fatty acids. J Inf Secur. 2016;73(6):523–535. doi: 10.1016/j.jinf.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 343.McFarland CT, Fan YY, Chapkin RS, Weeks BR, McMurray DN. Dietary polyunsaturated fatty acids modulate resistance to mycobacterium tuberculosis in Guinea pigs. J Nutr. 2008;138(11):2123–2128. doi: 10.3945/jn.108.093740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Paul KP, Leichsenring M, Pfisterer M, Mayatepek E, Wagner D, Domann M, Sonntag HG, Bremer HJ. Influence of n-6 and n-3 polyunsaturated fatty acids on the resistance to experimental tuberculosis. Metabolism. 1997;46(6):619–624. doi: 10.1016/s0026-0495(97)90003-2. [DOI] [PubMed] [Google Scholar]
- 345.Jordao L, Lengeling A, Bordat Y, Boudou F, Gicquel B, Neyrolles O, Becker PD, Guzman CA, Griffiths G, Anes E. Effects of omega-3 and -6 fatty acids on Mycobacterium tuberculosis in macrophages and in mice. Microbes Infect. 2008;10(12–13):1379–1386. doi: 10.1016/j.micinf.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 346.Grzybowski S, Dorken E. Tuberculosis in Inuit. Ecol Dis. 1983;2(2):145–148. [PubMed] [Google Scholar]
- 347.Kilabuk E, Momoli F, Mallick R, Van Dyk D, Pease C, Zwerling A, Potvin SE, Alvarez GG. Social determinants of health among residential areas with a high tuberculosis incidence in a remote Inuit community. J Epidemiol Community Health. 2019;73(5):401–406. doi: 10.1136/jech-2018-211261. [DOI] [PubMed] [Google Scholar]
- 348.Patterson M, Flinn S, Barker K. Addressing tuberculosis among Inuit in Canada. Can Commun Dis Rep. 2018;44(3-4):82–85. doi: 10.14745/ccdr.v44i34a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Soh AZ, Chee CB, Wang YT, Yuan JM, Koh WP. Dietary cholesterol increases the risk whereas PUFAs reduce the risk of active tuberculosis in Singapore Chinese. J Nutr. 2016;146(5):1093–1100. doi: 10.3945/jn.115.228049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Ralph AP, Waramori G, Pontororing GJ, Kenangalem E, Wiguna A, Tjitra E, Sandjaja LDB, Yeo TW, Chatfield MD, Soemanto RK, Bastian I, Lumb R, Maguire GP, Eisman J, Price RN, Morris PS, Kelly PM, Anstey NM. L-Arginine and vitamin D adjunctive therapies in pulmonary tuberculosis: a randomised, double-blind, placebo-controlled trial. PLoS One. 2013;8(8):e70032. doi: 10.1371/journal.pone.0070032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Schon T, Idh J, Westman A, Elias D, Abate E, Diro E, Moges F, Kassu A, Ayele B, Forslund T, Getachew A, Britton S, Stendahl O, Sundqvist T. Effects of a food supplement rich in arginine in patients with smear positive pulmonary tuberculosis—a randomised trial. Tuberculosis. 2011;91(5):370–377. doi: 10.1016/j.tube.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 352.Behr FM, Chuwonpad A, Stark R, van Gisbergen K. Armed and ready: transcriptional regulation of tissue-resident memory CD8 T cells. Front Immunol. 2018;9:1770. doi: 10.3389/fimmu.2018.01770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Park SL, Gebhardt T, Mackay LK. Tissue-resident memory T cells in cancer immunosurveillance. Trends Immunol. 2019;40(8):735–747. doi: 10.1016/j.it.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 354.Li C, Zhu B, Son YM, Wang Z, Jiang L, Xiang M, Ye Z, Beckermann KE, Wu Y, Jenkins JW, Siska PJ, Vincent BG, Prakash YS, Peikert T, Edelson BT, Taneja R, Kaplan MH, Rathmell JC, Dong H, Hitosugi T, Sun J. The transcription factor Bhlhe40 programs mitochondrial regulation of resident CD8(+) T cell fitness and functionality. Immunity. 2019;51(3):491–507.e497. doi: 10.1016/j.immuni.2019.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Milner JJ, Toma C, Yu B, Zhang K, Omilusik K, Phan AT, Wang D, Getzler AJ, Nguyen T, Crotty S, Wang W, Pipkin ME, Goldrath AW. Runx3 programs CD8(+) T cell residency in non-lymphoid tissues and tumours. Nature. 2017;552(7684):253–257. doi: 10.1038/nature24993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Mehta MM, Weinberg SE, Chandel NS. Mitochondrial control of immunity: beyond ATP. Nat Rev Immunol. 2017;17(10):608–620. doi: 10.1038/nri.2017.66. [DOI] [PubMed] [Google Scholar]
- 357.Philip M, Schietinger A. Heterogeneity and fate choice: T cell exhaustion in cancer and chronic infections. Curr Opin Immunol. 2019;58:98–103. doi: 10.1016/j.coi.2019.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Balmer ML, Ma EH, Bantug GR, Grahlert J, Pfister S, Glatter T, Jauch A, Dimeloe S, Slack E, Dehio P, Krzyzaniak MA, King CG, Burgener AV, Fischer M, Develioglu L, Belle R, Recher M, Bonilla WV, Macpherson AJ, Hapfelmeier S, Jones RG, Hess C. Memory CD8(+) T cells require increased concentrations of acetate induced by stress for optimal function. Immunity. 2016;44(6):1312–1324. doi: 10.1016/j.immuni.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 359.Narita T, Weinert BT, Choudhary C. Functions and mechanisms of non-histone protein acetylation. Nat Rev Mol Cell Biol. 2019;20(3):156–174. doi: 10.1038/s41580-018-0081-3. [DOI] [PubMed] [Google Scholar]
- 360.Mashimo T, Pichumani K, Vemireddy V, Hatanpaa KJ, Singh DK, Sirasanagandla S, Nannepaga S, Piccirillo SG, Kovacs Z, Foong C, Huang Z, Barnett S, Mickey BE, DeBerardinis RJ, Tu BP, Maher EA, Bachoo RM. Acetate is a bioenergetic substrate for human glioblastoma and brain metastases. Cell. 2014;159(7):1603–1614. doi: 10.1016/j.cell.2014.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Comerford SA, Huang Z, Du X, Wang Y, Cai L, Witkiewicz AK, Walters H, Tantawy MN, Fu A, Manning HC, Horton JD, Hammer RE, McKnight SL, Tu BP. Acetate dependence of tumors. Cell. 2014;159(7):1591–1602. doi: 10.1016/j.cell.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Wiens KE, Ernst JD. The mechanism for type I interferon induction by Mycobacterium tuberculosis is bacterial strain-dependent. PLoS Pathog. 2016;12(8):e1005809. doi: 10.1371/journal.ppat.1005809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.McNab F, Mayer-Barber K, Sher A, Wack A, O’Garra A. Type I interferons in infectious disease. Nat Rev Immunol. 2015;15(2):87–103. doi: 10.1038/nri3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Berry MP, Graham CM, McNab FW, Xu Z, Bloch SA, Oni T, Wilkinson KA, Banchereau R, Skinner J, Wilkinson RJ, Quinn C, Blankenship D, Dhawan R, Cush JJ, Mejias A, Ramilo O, Kon OM, Pascual V, Banchereau J, Chaussabel D, O’Garra A. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature. 2010;466(7309):973–977. doi: 10.1038/nature09247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Teles RM, Graeber TG, Krutzik SR, Montoya D, Schenk M, Lee DJ, Komisopoulou E, Kelly-Scumpia K, Chun R, Iyer SS, Sarno EN, Rea TH, Hewison M, Adams JS, Popper SJ, Relman DA, Stenger S, Bloom BR, Cheng G, Modlin RL. Type I interferon suppresses type II interferon-triggered human anti-mycobacterial responses. Science. 2013;339(6126):1448–1453. doi: 10.1126/science.1233665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Mayer-Barber KD, Andrade BB, Oland SD, Amaral EP, Barber DL, Gonzales J, Derrick SC, Shi R, Kumar NP, Wei W, Yuan X, Zhang G, Cai Y, Babu S, Catalfamo M, Salazar AM, Via LE, Barry CE, 3rd, Sher A. Host-directed therapy of tuberculosis based on interleukin-1 and type I interferon crosstalk. Nature. 2014;511(7507):99–103. doi: 10.1038/nature13489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Wu J, Sun L, Chen X, Du F, Shi H, Chen C, Chen ZJ. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science. 2013;339(6121):826–830. doi: 10.1126/science.1229963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.West AP, Shadel GS, Ghosh S. Mitochondria in innate immune responses. Nat Rev Immunol. 2011;11(6):389–402. doi: 10.1038/nri2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Murphy MP. How mitochondria produce reactive oxygen species. Biochem J. 2009;417(1):1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Immunity. 2015;42(3):406–417. doi: 10.1016/j.immuni.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Cumming BM, Addicott KW, Adamson JH, Steyn AJ (2018) Mycobacterium tuberculosis induces decelerated bioenergetic metabolism in human macrophages. Elife:7. 10.7554/eLife.39169 [DOI] [PMC free article] [PubMed]
- 372.Tully G, Kortsik C, Hohn H, Zehbe I, Hitzler WE, Neukirch C, Freitag K, Kayser K, Maeurer MJ. Highly focused T cell responses in latent human pulmonary Mycobacterium tuberculosis infection. J Immunol. 2005;174(4):2174–2184. doi: 10.4049/jimmunol.174.4.2174. [DOI] [PubMed] [Google Scholar]
- 373.Wong EA, Joslyn L, Grant NL, Klein E, Lin PL, Kirschner DE, Flynn JL (2018) Low levels of T cell exhaustion in tuberculous lung granulomas. Infect Immun 86(9). 10.1128/IAI.00426-18 [DOI] [PMC free article] [PubMed]
- 374.Yuneva M, Zamboni N, Oefner P, Sachidanandam R, Lazebnik Y. Deficiency in glutamine but not glucose induces MYC-dependent apoptosis in human cells. J Cell Biol. 2007;178(1):93–105. doi: 10.1083/jcb.200703099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Perez-Escuredo J, Dadhich RK, Dhup S, Cacace A, Van Hee VF, De Saedeleer CJ, Sboarina M, Rodriguez F, Fontenille MJ, Brisson L, Porporato PE, Sonveaux P. Lactate promotes glutamine uptake and metabolism in oxidative cancer cells. Cell Cycle. 2016;15(1):72–83. doi: 10.1080/15384101.2015.1120930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Gao P, Tchernyshyov I, Chang TC, Lee YS, Kita K, Ochi T, Zeller KI, De Marzo AM, Van Eyk JE, Mendell JT, Dang CV. c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature. 2009;458(7239):762–765. doi: 10.1038/nature07823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Yang C, Sudderth J, Dang T, Bachoo RM, McDonald JG, DeBerardinis RJ. Glioblastoma cells require glutamate dehydrogenase to survive impairments of glucose metabolism or Akt signaling. Cancer Res. 2009;69(20):7986–7993. doi: 10.1158/0008-5472.Can-09-2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Metallo CM, Gameiro PA, Bell EL, Mattaini KR, Yang J, Hiller K, Jewell CM, Johnson ZR, Irvine DJ, Guarente L, Kelleher JK, Vander Heiden MG, Iliopoulos O, Stephanopoulos G. Reductive glutamine metabolism by IDH1 mediates lipogenesis under hypoxia. Nature. 2011;481(7381):380–384. doi: 10.1038/nature10602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Wang YP, Zhou W, Wang J, Huang X, Zuo Y, Wang TS, Gao X, Xu YY, Zou SW, Liu YB, Cheng JK, Lei QY. Arginine methylation of MDH1 by CARM1 inhibits glutamine metabolism and suppresses pancreatic cancer. Mol Cell. 2016;64(4):673–687. doi: 10.1016/j.molcel.2016.09.028. [DOI] [PubMed] [Google Scholar]
- 380.Koppula P, Zhang Y, Zhuang L, Gan B. Amino acid transporter SLC7A11/xCT at the crossroads of regulating redox homeostasis and nutrient dependency of cancer. Cancer Commun. 2018;38(1):12. doi: 10.1186/s40880-018-0288-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Goto M, Miwa H, Shikami M, Tsunekawa-Imai N, Suganuma K, Mizuno S, Takahashi M, Mizutani M, Hanamura I, Nitta M. Importance of glutamine metabolism in leukemia cells by energy production through TCA cycle and by redox homeostasis. Cancer Investig. 2014;32(6):241–247. doi: 10.3109/07357907.2014.907419. [DOI] [PubMed] [Google Scholar]
- 382.Sugimoto K, Suzuki HI, Fujimura T, Ono A, Kaga N, Isobe Y, Sasaki M, Taka H, Miyazono K, Komatsu N. A clinically attainable dose of L-asparaginase targets glutamine addiction in lymphoid cell lines. Cancer Sci. 2015;106(11):1534–1543. doi: 10.1111/cas.12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Krall AS, Xu S, Graeber TG, Braas D, Christofk HR. Asparagine promotes cancer cell proliferation through use as an amino acid exchange factor. Nat Commun. 2016;7:11457. doi: 10.1038/ncomms11457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Sheen JH, Zoncu R, Kim D, Sabatini DM. Defective regulation of autophagy upon leucine deprivation reveals a targetable liability of human melanoma cells in vitro and in vivo. Cancer Cell. 2011;19(5):613–628. doi: 10.1016/j.ccr.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Scott L, Lamb J, Smith S, Wheatley DN. Single amino acid (arginine) deprivation: rapid and selective death of cultured transformed and malignant cells. Br J Cancer. 2000;83(6):800–810. doi: 10.1054/bjoc.2000.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Wang Z, Yip LY, Lee JHJ, Wu Z, Chew HY, Chong PKW, Teo CC, Ang HY, Peh KLE, Yuan J, Ma S, Choo LSK, Basri N, Jiang X, Yu Q, Hillmer AM, Lim WT, Lim TKH, Takano A, Tan EH, Tan DSW, Ho YS, Lim B, Tam WL. Methionine is a metabolic dependency of tumor-initiating cells. Nat Med. 2019;25(5):825–837. doi: 10.1038/s41591-019-0423-5. [DOI] [PubMed] [Google Scholar]
- 387.Geck RC, Toker A. Nonessential amino acid metabolism in breast cancer. Adv Biol Regul. 2016;62:11–17. doi: 10.1016/j.jbior.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 388.Locasale JW. Serine, glycine and one-carbon units: cancer metabolism in full circle. Nat Rev Cancer. 2013;13(8):572–583. doi: 10.1038/nrc3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Chaneton B, Hillmann P, Zheng L, Martin ACL, Maddocks ODK, Chokkathukalam A, Coyle JE, Jankevics A, Holding FP, Vousden KH, Frezza C, O’Reilly M, Gottlieb E. Serine is a natural ligand and allosteric activator of pyruvate kinase M2. Nature. 2012;491(7424):458–462. doi: 10.1038/nature11540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Keenan MM, Chi JT. Alternative fuels for cancer cells. Cancer J. 2015;21(2):49–55. doi: 10.1097/ppo.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Schug ZT, Vande Voorde J, Gottlieb E. The metabolic fate of acetate in cancer. Nat Rev Cancer. 2016;16(11):708–717. doi: 10.1038/nrc.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Yoshii Y, Furukawa T, Saga T, Fujibayashi Y. Acetate/acetyl-CoA metabolism associated with cancer fatty acid synthesis: overview and application. Cancer Lett. 2015;356(2 Pt A):211–216. doi: 10.1016/j.canlet.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 393.Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, Vacca C, Orabona C, Bianchi R, Belladonna ML, Volpi C, Santamaria P, Fioretti MC, Puccetti P. The combined effects of tryptophan starvation and tryptophan catabolites down-regulate T cell receptor zeta-chain and induce a regulatory phenotype in naive T cells. J Immunol. 2006;176(11):6752–6761. doi: 10.4049/jimmunol.176.11.6752. [DOI] [PubMed] [Google Scholar]
- 394.Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, Vacca C, Orabona C, Bianchi R, Belladonna ML, Volpi C, Fioretti MC, Puccetti P. Tryptophan catabolism generates autoimmune-preventive regulatory T cells. Transpl Immunol. 2006;17(1):58–60. doi: 10.1016/j.trim.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 395.Munn DH, Sharma MD, Baban B, Harding HP, Zhang Y, Ron D, Mellor AL. GCN2 kinase in T cells mediates proliferative arrest and anergy induction in response to indoleamine 2,3-dioxygenase. Immunity. 2005;22(5):633–642. doi: 10.1016/j.immuni.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 396.Duffy AG, Melillo G, Turkbey B, Allen D, Choyke PL, Chen C, Raffeld M, Doroshow JH, Murgo A, Kummar S. A pilot trial of oral topotecan (TPT) in patients with refractory advanced solid neoplasms expressing HIF-1α. J Clin Oncol. 2010;28(15_suppl):e13518–e13518. doi: 10.1200/jco.2010.28.15_suppl.e13518. [DOI] [Google Scholar]
- 397.Schilling B, Sucker A, Griewank K, Zhao F, Weide B, Gorgens A, Giebel B, Schadendorf D, Paschen A. Vemurafenib reverses immunosuppression by myeloid derived suppressor cells. Int J Cancer. 2013;133(7):1653–1663. doi: 10.1002/ijc.28168. [DOI] [PubMed] [Google Scholar]
- 398.Beijer MR, Kraal G, den Haan JM. Vitamin A and dendritic cell differentiation. Immunology. 2014;142(1):39–45. doi: 10.1111/imm.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Cassani B, Villablanca EJ, De Calisto J, Wang S, Mora JR. Vitamin A and immune regulation: role of retinoic acid in gut-associated dendritic cell education, immune protection and tolerance. Mol Asp Med. 2012;33(1):63–76. doi: 10.1016/j.mam.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Ida S, Hiki N, Cho H, Sakamaki K, Ito S, Fujitani K, Takiguchi N, Kawashima Y, Nishikawa K, Sasako M, Aoyama T, Honda M, Sato T, Nunobe S, Yoshikawa T. Randomized clinical trial comparing standard diet with perioperative oral immunonutrition in total gastrectomy for gastric cancer. Br J Surg. 2017;104(4):377–383. doi: 10.1002/bjs.10417. [DOI] [PubMed] [Google Scholar]
- 401.Miyata H, Yano M, Yasuda T, Yamasaki M, Murakami K, Makino T, Nishiki K, Sugimura K, Motoori M, Shiraishi O, Mori M, Doki Y. Randomized study of the clinical effects of omega-3 fatty acid-containing enteral nutrition support during neoadjuvant chemotherapy on chemotherapy-related toxicity in patients with esophageal cancer. Nutrition. 2017;33:204–210. doi: 10.1016/j.nut.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 402.Sorensen LS, Thorlacius-Ussing O, Rasmussen HH, Lundbye-Christensen S, Calder PC, Lindorff-Larsen K, Schmidt EB. Effects of perioperative supplementation with omega-3 fatty acids on leukotriene B(4) and leukotriene B(5) production by stimulated neutrophils in patients with colorectal cancer: a randomized, placebo-controlled intervention trial. Nutrients. 2014;6(10):4043–4057. doi: 10.3390/nu6104043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Mocellin MC, Pastore e Silva Jde A, Camargo Cde Q, Fabre ME, Gevaerd S, Naliwaiko K, Moreno YM, Nunes EA, Trindade EB. Fish oil decreases C-reactive protein/albumin ratio improving nutritional prognosis and plasma fatty acid profile in colorectal cancer patients. Lipids. 2013;48(9):879–888. doi: 10.1007/s11745-013-3816-0. [DOI] [PubMed] [Google Scholar]
- 404.Silva Jde A, Trindade EB, Fabre ME, Menegotto VM, Gevaerd S, Buss Zda S, Frode TS. Fish oil supplement alters markers of inflammatory and nutritional status in colorectal cancer patients. Nutr Cancer. 2012;64(2):267–273. doi: 10.1080/01635581.2012.643133. [DOI] [PubMed] [Google Scholar]
- 405.Bonatto SJ, Oliveira HH, Nunes EA, Pequito D, Iagher F, Coelho I, Naliwaiko K, Kryczyk M, Brito GA, Repka J, Saboia LV, Fukujima G, Calder PC, Fernandes LC. Fish oil supplementation improves neutrophil function during cancer chemotherapy. Lipids. 2012;47(4):383–389. doi: 10.1007/s11745-011-3643-0. [DOI] [PubMed] [Google Scholar]
- 406.Trabal J, Leyes P, Forga M, Maurel J. Potential usefulness of an EPA-enriched nutritional supplement on chemotherapy tolerability in cancer patients without overt malnutrition. Nutr Hosp. 2010;25(5):736–740. [PubMed] [Google Scholar]
- 407.Rotovnik Kozjek N, Kompan L, Soeters P, Oblak I, Mlakar Mastnak D, Mozina B, Zadnik V, Anderluh F, Velenik V. Oral glutamine supplementation during preoperative radiochemotherapy in patients with rectal cancer: a randomised double blinded, placebo controlled pilot study. Clin Nutr. 2011;30(5):567–570. doi: 10.1016/j.clnu.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 408.Seguin P, Locher C, Boudjema K, Hamon C, Mouchel C, Malledant Y, Bellissant E. Effect of a perioperative nutritional supplementation with oral impact(R) in patients undergoing hepatic surgery for liver cancer: a prospective, placebo-controlled, randomized, double-blind study. Nutr Cancer. 2016;68(3):464–472. doi: 10.1080/01635581.2016.1153670. [DOI] [PubMed] [Google Scholar]
- 409.Marano L, Porfidia R, Pezzella M, Grassia M, Petrillo M, Esposito G, Braccio B, Gallo P, Boccardi V, Cosenza A, Izzo G, Di Martino N. Clinical and immunological impact of early postoperative enteral immunonutrition after total gastrectomy in gastric cancer patients: a prospective randomized study. Ann Surg Oncol. 2013;20(12):3912–3918. doi: 10.1245/s10434-013-3088-1. [DOI] [PubMed] [Google Scholar]
- 410.Okamoto Y, Okano K, Izuishi K, Usuki H, Wakabayashi H, Suzuki Y. Attenuation of the systemic inflammatory response and infectious complications after gastrectomy with preoperative oral arginine and omega-3 fatty acids supplemented immunonutrition. World J Surg. 2009;33(9):1815–1821. doi: 10.1007/s00268-009-0140-1. [DOI] [PubMed] [Google Scholar]