Abstract
Background
Despite existing studies favoring cemented fixation for patients older than 75 years, a trend toward increased use of uncemented fixation has been described in a 2013 study that used arthroplasty registry data from 2006 to 2010. Updated summarized data are needed beyond 2010 to investigate contemporary trends in the usage of uncemented fixation, especially in patients older than 75 years, and to draw attention to a potential continuing conflict between trends in fixation choice and reported revision risk. Thus, healthcare policy and practice can change and surgeons can make better implant fixation choices.
Questions/purposes
(1) Has the percentage of primary THAs performed with uncemented fixation changed since 2010? (2) Has the percentage of primary THAs performed in patients older than 75 years performed with uncemented fixation changed since 2010? (3) After stratifying by age, which fixation strategy (cemented versus uncemented and hybrid versus uncemented) is associated with the lowest risk of revision?
Methods
National annual reports from hip arthroplasty registers were identified, and data were extracted from registers published in English or a Scandinavian language, with at least 3 years of reported data in the period from 2010 to 2017. These included Australia, Denmark, England-Wales, Finland, the Netherlands, New Zealand, Romania, Norway, Sweden, and Switzerland, which are all countries with high completeness rates. Data regarding rates of revisions (all causes) related to fixation methods and secondary to different age groups, were taken directly from the registers and no re-analysis was done. The risk estimates were presented as either hazard ratios, rate per 100 component years or as Kaplan-Meier estimates of revision. The age groups compared for Denmark were younger than 50, 50-59, 60-69,70-79, and older than 80 years, and for Australia, New Zealand, England-Wales, and Finland, they were younger than 55, 55-64, 65-74, and older than 75 years. No data were pooled across the registers.
Results
The current use of uncemented fixation in primary THAs varies between 24% (Sweden) and 71% (Denmark). Increasing use of uncemented fixation has been reported in Norway, Denmark, and Sweden, whereas decreasing use of uncemented fixation has been reported in England-Wales, Australia, New Zealand, and Finland. Examining the group of patients older than 75 years, we found that the use of uncemented fixation has been stable in Netherlands, Sweden, New Zealand, and England-Wales. The use of uncemented fixation is still increasing in Denmark and Australia. In Finland, the use of uncemented fixation has decreased (from 43 % to 24 %) from 2010 to 2017. When compared with uncemented fixation, the risk of revision for hips using cemented fixation was lower in patients older than 75 years for all registers surveyed, except for the oldest males in the Finnish register. In this group, no difference was found between cemented and uncemented fixation.
Conclusion
Our findings should be used in healthcare policy as feedback on current THAs being performed so as to direct surgeons to choose the right implant fixation, especially in patients older than 75 years, thereby reducing revision risk and increasing the long-term survival of primary THAs. It appears that femoral stem fixation may be the most important revision risk factor in older patients, and future studies should examine this perspective.
Level of Evidence
Level III, therapeutic study.
Introduction
The most appropriate implant fixation choice in THA remains a matter for debate. Uncemented fixation was introduced to reduce the rates of aseptic loosening [33] seen with cemented fixation, which was originally attributed to “cement disease” [17]. Despite later studies showing that aseptic loosening occurred with all fixation types [7, 21], surgeons continued to use uncemented fixation. In a previous study, we found a worldwide shift toward uncemented fixation, which we described as an “uncemented paradox” [32]. However, arthroplasty registry studies have also shown that uncemented fixation is associated with higher revision rates, particularly in older patients [6, 14, 19, 20, 26, 30, 32]. In addition, the increasing use of uncemented fixation may be associated with increasing rates of periprosthetic fractures [1, 18, 31].
The population of older people continues to grow both in United States and Europe, and the demand for primary THAs is likely to increase [10, 16, 23]. Therefore, continued efforts to keep the revision burden as low as possible are warranted. In 2013, our group examined publicly available annual reports of hip arthroplasty registries worldwide from 2006 to 2010 to highlight the use of uncemented fixation in THAs [32]. That study showed a general increasing use of uncemented fixation in THAs; further, the registry data suggested that cemented fixation in patients older than 75 years is associated with the lowest risk of revision. Updated, summarized, worldwide data are needed as a follow-up to these findings, especially in patients older than 75 years. Using registry data as feedback on the surgical work completed since 2010, it is possible to draw attention to a potential continuing conflict between trends in fixation choice and reported revision risk. As a result, healthcare policy and practice can change, leading to surgeons making better implant fixation choices, which may increase THA survivorship.
As a follow-up to the previous published data by Troelsen et al. [32], we therefore aimed to review the annual reports of the established arthroplasty registers worldwide (from 2010 to 2018) to answer the following questions: (1) Has the percentage of primary THAs performed with uncemented fixation changed since 2010? (2) Has the percentage of primary THAs performed in patients older than 75 years performed with uncemented fixation changed since 2010? (3) After stratifying by age, which fixation strategy (cemented versus uncemented, and hybrid versus uncemented) is associated with the lowest risk of revision?
Methods and Materials
In our previous study [32], we used national hip arthroplasty registry data from Australia, Canada, Denmark, England-Wales, New Zealand, Norway, and Sweden. We selected those registries because reports were available in English or in a Scandinavian language and had a history of more than 5 years of data collection. In March 2019, we performed a similar search. Countries with established national hip arthroplasty registries included Australia, Austria, Belgium, Canada, Croatia, Czech Republic, Denmark, England-Wales, Finland, France, Germany, Hungary, India, Ireland, Italy, Lithuania, the Netherlands, New Zealand, Norway, Pakistan, Portugal, Romania, Scotland, Slovakia, Slovenia, South Africa, Spain, Sweden, Switzerland, Turkey, and the United States.
We included national hip arthroplasty registers that (1) publish data in English or in a Scandinavian language, (2) have at least 3 years of collected data in the studied period, and (3) have data describing the current use of uncemented fixation. If an annual report was not available online, we contacted the arthroplasty register by email and requested the report.
We ultimately included national data from Australia [3], Denmark [7], England-Wales [21], Finland [11], New Zealand [22], Romania [25], Norway [24], Sweden [28], the Netherlands [9] and Switzerland [29], which are all countries with high numbers of completeness. In general data from the registers are considered reliable because compliance is high, and the validity of data is well examined. In addition, administrative databases in general account for deceased patients and those who have immigrated. We reviewed all annual reports from the included registers in March 2019. First, we extracted data regarding year of initiation, completeness, number of primary THAs reported, and last year of follow-up (Table 1). Completeness is the percentage of procedures reported to the registry of the actual number performed. We evaluated the current use of uncemented fixation in primary THAs as a percentage of all primary THAs, the current use of uncemented fixation in primary THAs as a percentage of all primary THAs in patients older than 75 years, and age-stratified risk estimates of revision when comparing different fixation techniques used during the primary THA. No data from across registries were pooled.
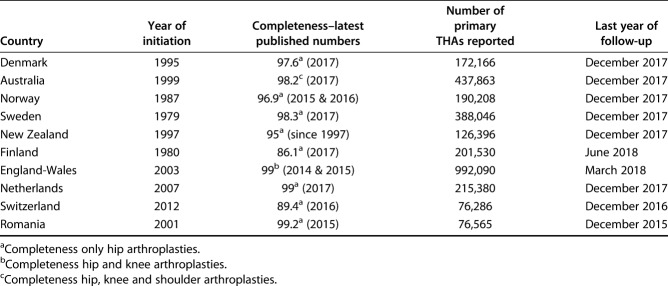
Table 1.
Registry of data for THAs
The participants included all patients who received an uncemented THA from 2010 to 2017 presented in the national registers. As for the use of uncemented fixation in primary THAs, in patients older than 75 years, the participants included all patients receiving an uncemented fixation THA in the years from 2010 to 2017.This could be extracted from Australia (older than 75), Denmark (older than 70), England and Wales (older than 75), Finland (older than 75), the Netherlands (older than 80), New Zealand (older than 75), Norway (older than 75), and Sweden (older than 80).
Our primary study outcome of interest was revision risk in different age groups (all causes) using different fixation techniques. The age groups compared for Denmark were as follows: younger than 50, 50-59, 60-69,70-79, older than 80 years while for Australia, New Zealand, England-Wales and Finland, the compared age groups were: younger than 55, 55-64, 65-74, older than 75 years. Our secondary study outcome was the level of uncemented fixation use in percentage for every year since 2010.
Statistical Analysis
Descriptive statistics were applied. Data regarding the current use of uncemented fixation in the included countries were presented as percentages of all fixation techniques used, thus establishing a trend of uncemented fixation for each country in the period of 2011 to 2018.
The current use of uncemented in patients older than 75 years has been presented as a percentage of all fixation techniques used in this age group. For New Zealand, England-Wales and Australia though, these data could not be extracted directly from the annual reports and data was therefore extracted by using previous reports to subtract historical data from the data reported. This was done in Excel. The data regarding age-stratified risk estimates of revision was extracted directly from the annual report of the registries. For England-Wales and Finland, the risk estimated were reported for each sex separately. For Denmark and Australia, the risk estimates were reported as hazard ratios, for New Zealand as rate per 100 component years and for England-Wales and Finland as Kaplan-Meier estimates of revision (see Appendix, Supplemental Digital Content 1, http://links.lww.com/CORR/A287). We then grouped and colored the age-stratified risk estimates of revision according to whether statistical significance was observed. No re-analysis was done. Statistical significance was defined as p value < 0.05.
Results
The Trend of Uncemented Fixation in THAs from 2010-2017
In the Scandinavian countries, the percentage of primary THAs performed with uncemented fixation have slowly been increasing since 2010, while the rest of the included countries have decreasing numbers of uncemented fixation.
In 2017, the use of uncemented fixation varied between 24% (Sweden) and 71% (Denmark) of all THAs reported in the included arthroplasty registers (Fig. 1). From 2010 to 2017, the use of uncemented fixation increased: Norway (25%-38%), Denmark (68%-71%), and Sweden (15%-24%). In contrast, use has slowly decreased during the past 7 years in England-Wales (43%-37.8%), Australia (65%-63%), New Zealand (51%-48%), and Finland (71%-49%). Switzerland had the highest number of uncemented fixation procedures, which was stable from 2012 to 2016; 2017 numbers were not available.
Fig. 1.
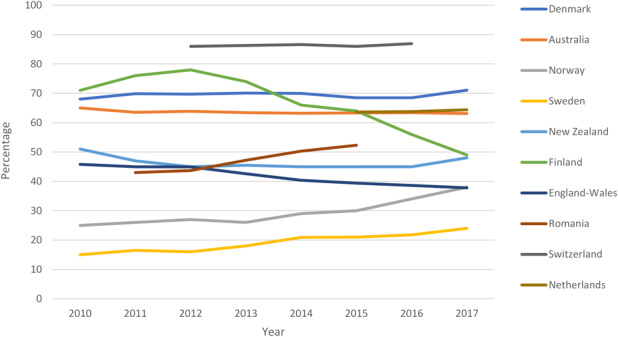
This graph shows the percentages of uncemented fixation of all primary THAs performed each year from 2011 to 2017. Romania only had data from 2011 to 2015, the Netherlands only had data from 2015 to 2017, and Switzerland only had data from 2012 to 2016. Numbers from 2010 are from the study of Troelsen et al. [32].
Trend of Uncemented Fixation in THAs from 2010-2017 in Patients Older Than 75 years
The use of uncemented fixation in patients older than 75 years still varies substantially between the included countries. From 2010 to 2017, the use of uncemented fixation in patients older than 75 years increased in Denmark (42%-53%) and Australia (40%-47%). In comparison, the use of uncemented fixation declined between 2010 and 2017 in Finland (43%-24%) and Norway (21%-15%). During this same approximate timeframe, uncemented fixation use has generally been stable in Sweden (2.5%-2%), the Netherlands (37.5%-38.6%), New-Zealand (12%-15%) and England-Wales (24%-25%) (Fig. 2). Data from the Netherlands was not available for this group before 2015.
Fig. 2.
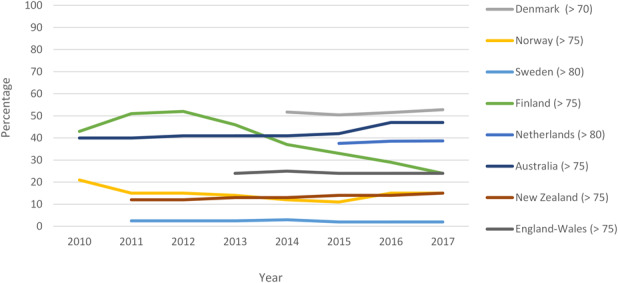
This graph shows the percentages of uncemented fixation of all THAs performed in patients older than 70 years from 2011 to 2017. Data could not be extracted for Denmark from 2011 to 2013 and from the Netherlands from 2011 to 2015. Numbers from 2010 are from the study by Troelsen et al. [32].
After Stratifying by Age, Which Fixation Strategy (Cemented Versus Uncemented and Hybrid Versus Uncemented) Is Associated with the Lowest Risk of Revision?
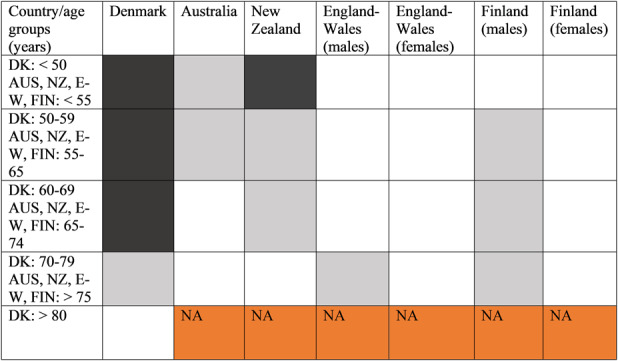
In patients older than 75 years, cemented THA has the overall lowest risk of revision, this was followed by hybrid fixation and then uncemented fixation. Comparing cemented fixation with uncemented fixation, the above pattern was true in Denmark (older than 70 years), Australia (older than 75 years), England and Wales (older than 75 years), New Zealand (older than 75 years) and Finland (females older than 75 years). The pattern was not seen in Finnish males (older than 75 years), where there was no difference in the risk of revision (Fig. 3).
Fig. 3.
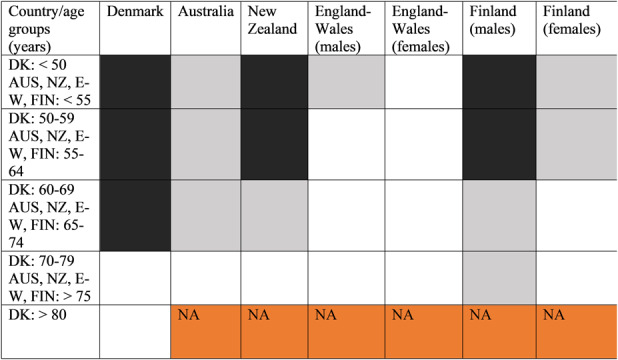
This figure shows the risk profiles for cemented fixation and uncemented fixation. White = statistically significant lower risk of revision after cemented versus uncemented fixation (p < 0.05). Gray = no statistically significant difference in the risk of revision after cemented versus uncemented fixation. Black = statistically significant greater risk of revision after cemented fixation versus uncemented fixation (p < 0.05). Orange = data not available. DK = Denmark; AUS = Australia; NZ = New Zealand; E-W = England-Wales; FIN = Finland.
Comparing hybrid fixation (cemented femur) with uncemented fixation the pattern was true in Denmark (older than 80 years), Australia (older than 75 years), New Zealand (older than 75 years) England and Wales (females older than 75 years), and Finland (females older than 75 years).
We did not see this pattern in Denmark (70-79 years), England and Wales (males older than 75 years), or Finland (males older than 75 years), where we found no difference in revision rates (Fig. 4). In a younger population of males, uncemented fixation still has a clear advantage.
Fig. 4.
This figure shows the risk profiles for hybrid fixation (cemented femur) and uncemented fixation. White = statistically significant lower risk of revision after hybrid versus uncemented fixation (p < 0.05). Gray = no statistically significant difference in the risk of revision after hybrid versus uncemented fixation. Black = statistically significant greater risk of revision after hybrid versus uncemented fixation (p < 0.05). Orange = data not available. DK = Denmark; AUS = Australia; NZ = New Zealand; E-W = England-Wales; FIN = Finland.
Discussion
The most appropriate choice for implant fixation in THA remains a matter for debate, with both cemented and uncemented methods yielding high levels of durable success. However, arthroplasty registry studies have also shown that uncemented fixation is associated with higher revision rates, particularly in older patients. In a previous study, we found a worldwide shift toward uncemented fixation, which we described as an “uncemented paradox.” Since that study 10 years ago, substantially more patients have undergone hip arthroplasty, and many more countries have instituted registries. Thus, we reviewed the annual reports of the established arthroplasty registers worldwide (from 2010 to 2018) to answer the following questions: (1) Has the percentage of primary THAs performed with uncemented fixation changed since 2010? (2) Has the percentage of primary THAs performed in patients older than 75 years performed with uncemented fixation changed since 2010? (3) After stratifying by age, which fixation strategy (cemented versus uncemented and hybrid versus uncemented) is associated with the lowest risk of revision?
Limitations
This study is based on publicly available annual reports from hip arthroplasty registers. We could not assess raw data from the registers; therefore, we could not adjust for confounders such as bearing surface, activity, and comorbidities, and we could not perform an additional analysis on raw data. Regarding the age-stratified risk estimated for revision, this data represents all-cause revisions, and therefore, we did not adjust for the reason for revision. Of course, some reasons for revision are unrelated to fixation, but we believe this confounder may be equally distributed across the registries. It was neither possible to account for different bearing surfaces (for example metal-on-metal and cross-linked polyethylene liners). However, we believe that this does not interfere substantially with our findings as our main focus has been on patients older than 75 years, and many of the novel bearings, such as metal-on-metal, were used primarily in younger patients. We also note that different arthroplasty registers do not report data using uniform outcome measures and risk stratification (hazard ratios, revision rate per 100 component years, and Kaplan-Meier cumulative revision risk), and the same registers may even present the data differently from year to year, which makes it more difficult to compare data. Despite this limitation, the registers provide information on large numbers of patients with high levels of followup. Therefore, the results from the registers provide some of the best estimates of revision risk. The registries we used arise from countries that differ substantially in terms of population as well as levels of ethnic and social homogeneity, but we do not find that data quality depends on country size and population numbers. Of interest, several Scandinavian countries, such as Denmark, Norway, and Sweden have similarly homogeneous populations, but demonstrate substantial variations in the use of uncemented or cemented fixation.
Proportion of THAs Performed with Cementless Fixation
In the Scandinavian countries, we found the percentage of primary THAs performed with uncemented fixation has slowly been increasing since 2010, while the rest of the included countries have decreasing numbers of uncemented fixation. There is substantial variation from country to country in how much uncemented fixation are used (24% to 71%). In our previous study, an increasing trend toward the use of uncemented fixation was observed up until 2010, irrespective of geography [32]. This seems to have changed, probably because of the increased worldwide focus on this trend. The increasing use trend in the Scandinavian countries is difficult to explain because these countries have very substantial variation in their use of uncemented fixation.
Proportion of THAs Performed with Cementless Fixation in Patients Older Than 75 years
We found that the use of uncemented fixation in patients older than 75 years still varies between the included countries. In some countries, the number of uncemented fixations have remained constant since 2010, whereas there has been a drop or an increase in other countries. The stabilization and the drop in the use of uncemented fixation in patients older than 75 years can be attributable to an increased awareness in these countries of the benefits of cemented fixation in this age group, shown by our previous study [32] and other studies that support this evidence [14, 20, 30]. We caution, however, that most of these reflect data from only one register. Thus, updated summarized data from more than one register may be needed to better assess worldwide trends.
Risk of Revision by Fixation Type
We found that in patients older than 75 years, cemented THA has the overall lowest risk of revision, followed by hybrid fixation and then by uncemented fixation. This confirms our previous findings [32]. This does not appear to be related to variations in performance of specific implants. Reviewing Australian registry data, Tanzer et al. [30] found that uncemented fixation in patients older than 75 years was associated with a higher early rate of revision, even when only the best-performing prostheses were compared. In 2017, using registry data from Australia, Finland, Denmark and Italy, Hughes et al. [15] showed that certain cemented prostheses performed better than the best uncemented prosthesis. Additionally, Sheridan et al. [26] showed that cemented THAs have the best 10-year all-cause revision rates. Because we found that hybrid fixation has a lower risk of revision compared with cementless fixation, we surmise that the use of cemented stems could actually be the most important aspect regarding revision risk in patients older than 75 years. This could be explained by the general loss of bone mass and bone strength as well as anatomic change of the femoral canal in older people, which increase fracture risk [5, 8]. However, we found no difference between hybrid fixation and uncemented fixation looking at males older than 75 years in England and Wales and Finland, although there was a clear difference in females. This may reflect better bone quality in male patients and a lower prevalence of osteoporosis, which may also account for a higher risk of periprosthetic fractures in female patients than in male patients [2, 4, 8, 12, 27]. In addition, uncemented fixation has been associated with increasing rates of periprosthetic fractures [1, 12, 31]. Therefore, the choice of fixation technique in older female patients needs additional scrutiny. Further studies comparing cemented fixation with hybrid fixation may be helpful. Considering the role of primary femoral fixation in survival of a first revision arthroplasty, Gromov et al. [13] found an increased risk of re-revision of primary THAs with a cementless femoral component. Despite adjustment for potential confounders, this was seen in all patients. This finding further highlights the importance of best choice of fixation technique in primary THAs because it affects the revision burden and patterns until the second revision.
Conclusions
We found little evidence for sustained worldwide trends in changes of the proportion of cemented versus uncemented femoral fixation. In Scandinavia, the percentage of primary THAs performed with uncemented fixation has increased since 2010, in contrast to other countries that show decreases. We also found that in patients older than 75 years, cemented THA still has the overall lowest risk of revision followed by hybrid fixation and then uncemented fixation. As such, we recommend that cemented femoral stems be considered the implants of choice for older patients. Continued evaluation of hybrid fixation versus fully cemented fixation, particularly in patients older than 75 years of age, should be encouraged. Finally, both trainees and practicing arthroplasty surgeons should ensure that they acquire and maintain the technical skills needed to perform cemented hip arthroplasty.
Supplementary Material
Acknowledgments
We thank all those involved in the worldwide registry effort.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Copenhagen University Hospital, Hvidovre, Denmark.
References
- 1.Abdel MP, Houdek MT, Watts CD, Lewallen DG, Berry DJ. Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties: a 40-year experience. Bone Joint J . 2016;98:468-474. [DOI] [PubMed] [Google Scholar]
- 2.Alswat KA. Gender disparities in osteoporosis. J Clin Med Res . 2017;9:382-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Orthopaedic Association. 2018. Annual Reports - AOANJRR. Available at: https://aoanjrr.sahmri.com/annual-reports-2018. Accessed November 13, 2019.
- 4.Berend ME, Smith A, Meding JB, Ritter MA, Lynch T, Davis K. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty. 2006;21:53-59. [DOI] [PubMed] [Google Scholar]
- 5.Boskey AL, Coleman R. Aging and bone. J Dent Res . 2010;89:1333-1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corbett KL, Losina E, Nti AA, Prokopetz JJZ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:13520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danish Orthopaedic Society. Danish Hip Arthroplasty register. National report 2018. Available at: http://danskhoftealloplastikregister.dk/wp-content/uploads/2016/04/DHR-årsrapport-2018_til-offentliggørelse.pdf. Accessed November 13, 2019.
- 8.Dorr LD, Absatz M, Gruen TA, Saberi MT, Doerzbacher JF. Anatomic porous replacement hip arthroplasty: first 100 consecutive cases. Semin Arthroplasty. 1990;1:77-86. [PubMed] [Google Scholar]
- 9.Dutch Arthroplasty Register (LROI). LROI annual report 2018. Available at: http://www.lroi-rapportage.nl/media/pdf/PDF%20Online_LROI_annual_report_2018.pdf. Accessed November 13, 2019.
- 10.European Commission, Directorate-General for Economic and Financial Affairs, Economic Policy Committee of the European Communities. The 2018 ageing report: underlying assumptions and projection methodologies . 2017. Available at: https://ec.europa.eu/info/sites/info/files/economy-finance/ip065_en.pdf. Accessed October 30, 2019.
- 11.Finnish Society of Orthopaedic Surgeons. Finnish Arthroplasty register. Available at: https://www.thl.fi/far/#index. Accessed November 13, 2019.
- 12.Gromov K, Bersang A, Nielsen CS, Kallemose T, Husted H, Troelsen A. Risk factors for post-operative periprosthetic fractures following primary total hip arthroplasty with a proximally coated double-tapered cementless femoral component. Bone Joint J . 2017;99:451-457. [DOI] [PubMed] [Google Scholar]
- 13.Gromov K, Pedersen AB, Overgaard S, Gebuhr P, Malchau H, Troelsen A. Do rerevision rates differ after first-time revision of primary THA with a cemented and cementless femoral component? Clin Orthop Relat Res. 2015;473:3391-3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop . 2010;81:34-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hughes RE, Batra A, Hallstrom BR. Arthroplasty registries around the world: valuable sources of hip implant revision risk data. Curr Rev Musculoskelet Med . 2017;10:240-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, Lewallen DG, Trousdale RT, Jiranek WA, Stamos VP, Parsley BS. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg. Am. 2008;90:1598-1605. [DOI] [PubMed] [Google Scholar]
- 17.Jones LC, Hungerford DS. Cement disease. Clin Orthop Relat Res . 1987:192-206. [PubMed] [Google Scholar]
- 18.Lindberg-Larsen M, Jørgensen CC, Solgaard S, Kjersgaard AG, Kehlet H, Lunbeck Foundation Centre for Fast-track Hip and Knee Replacement. Increased risk of intraoperative and early postoperative periprosthetic femoral fracture with uncemented stems. Acta Orthop . 2017;88:390-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMinn DJW, Snell KIE, Daniel J, Treacy RBC, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop . 2007;78:315-326. [DOI] [PubMed] [Google Scholar]
- 21.National Joint registry. 15th Annual Report 2018. Available at: https://www.hqip.org.uk/wp-content/uploads/2018/11/NJR-15th-Annual-Report-2018.pdf. Accessed November 13, 2019.
- 22.New Zealand Orthopaedic Association Joint Registry. NZJR 19 Year Report. Available at: https://nzoa.org.nz/system/files/DH8152_NZJR_2018_Report_v6_4Decv18.pdf. Accessed November 13, 2019.
- 23.Nho SJ, Kymes SM, Callaghan JJ, Felson DT. The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg . 2013;21 (Suppl 1):S1-6. [DOI] [PubMed] [Google Scholar]
- 24.Norwegian Orthopaedic Association. Norwegian Arthroplasty Register. Report June 2018. Available at: http://nrlweb.ihelse.net/eng/Rapporter/Report2018_english.pdf. Accessed November 13, 2019.
- 25.Romanian Arthroplasty register. Hip Biennial Report 2015. Available at: http://www.rne.ro/rnemedia/download/83548eca694de29dd5abfdf8bb68ff68. Accessed November 13, 2019.
- 26.Sheridan GA, Kelly RM, McDonnell SM, Walsh F, O’Byrne JM, Kenny PJ. Primary total hip arthroplasty: registry data for fixation methods and bearing options at a minimum of 10 years. Ir J Med Sci . 2019;188:873-877. [DOI] [PubMed] [Google Scholar]
- 27.Singh JA, Jensen MR, Harmsen SW, Lewallen DG. Are gender, comorbidity, and obesity risk factors for postoperative periprosthetic fractures after primary total hip arthroplasty? J Arthroplasty. 2013;28:126-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swedish Orthopaedic Association. Swedish Hip Arthroplasty Register. Annual Report 2017. Available at: https://registercentrum.blob.core.windows.net/shpr/r/Eng_Arsrapport_2017_Hoftprotes_final-Syx2fJPhMN.pdf. Accessed November 13, 2019. [Google Scholar]
- 29.Swiss National Joint Registry. Annual Report of the Swiss National Joint Registry, Hip and Knee 2012-2016. Available at: https://www.anq.ch/wp-content/uploads/2018/09/ANQ_Akut_SIRIS_Jahresbericht_2012-16.pdf. Accessed November 13, 2019.
- 30.Tanzer M, Graves SE, Peng A, Shimmin AJ. Is cemented or cementless femoral stem fixation more durable in patients older than 75 years of age? A comparison of the best-performing stems. Clin Orthop Relat Res . 2018;476:1428-1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomsen MN, Jakubowitz E, Seeger JB, Lee C, Kretzer JP, Clarius M. Fracture load for periprosthetic femoral fractures in cemented versus uncemented hip stems: an experimental in vitro study. Orthopedics. 2008;31:653. [PubMed] [Google Scholar]
- 32.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013;471:2052-2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wechter J, Comfort TK, Tatman P, Mehle S, Gioe TJ. Improved survival of uncemented versus cemented femoral stems in patients aged < 70 years in a community total joint registry. Clin Orthop Relat Res . 2013;471:3588-3595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.