Abstract
Purpose:
The provision of genetic services often occurs in a cascading fashion within families experiencing inherited diseases. This study examines whether previous family experiences with genetic services influences levels of psychological well-being of family members receiving services later.
Methods:
Two hundred ninety-seven persons from 38 families with Lynch syndrome completed questionnaires before receiving genetic services. Baseline levels of test-related distress, depressive symptoms, and cancer worries were assessed in relationship to the (1) amount of time elapsed since services were provided to the index case and (2) generation of the family member relative to the index case.
Results:
Family members in the same generation as the index case experienced significant increases in test-related distress (P = 0.003) and cancer worry (P = 0.001) with increasing time between receipt of genetic test results by the index case and provision of services to family members. Change in the number of depressive symptoms was not significant (P = 0.17).
Conclusion:
The provision of genetic services through a cascading approach significantly increases distress and worry among family members within the same generation as the index case who receive services at increasingly distant time intervals. Additional research is needed to explore social influences after the introduction of genetic services.
Keywords: genetic services, cascade genetic testing, social influence, genetic test related distress and worry, HNPCC/Lynch syndrome
The provision of genetic services (genetic education, counseling, risk assessment, and the option of genetic testing) within a family often occurs over an extended period of time due to a cascading approach used in the offer of genetic testing for inherited disorders. Numerous studies have reported on the uptake of genetic services in families using a cascading approach to notify at risk family members and offer additional genetic services.1–5 After the identification of a disease-related mutation in the index case, the offer of genetic services is extended to first-degree relatives (FDRs) and then cascades outward to increasingly more distant relatives. This approach keeps the financial costs of testing at a minimum and focused on persons at greatest risk of inheriting the predisposing mutation. The cascading approach to providing genetics services results in the periodic provision of information within families and allows for the exchange of information between family members over extended periods of time. Hypothetically, the information, experiences, attitudes, and beliefs of those having received genetic services at an earlier time point, has the potential to be shared and influence levels of disease knowledge, perceptions of genetic risks, understanding of the benefits, risks, and limitations of genetic testing among those who come to genetic services at later time points. Such social influences (Marsden and Friedkin6 define social influence as the modification of one person’s responses by the actions of another) may impact the psychological well-being and behavioral actions of those receiving services later. Understanding the impact of the periodic provision of genetic risk information and the associated communication that occurs within families seems paramount in developing and providing genetic and genomic services that target families.7
Genetic testing for dominantly inherited diseases has been available and used for nearly 2 decades. Research exploring the impact of genetic testing following comprehensive education and counseling has consistently reported no long-term adverse psychological outcomes for the majority of individuals undergoing testing and receiving results.8 However, there is evidence that psychological well-being is associated with clinically relevant outcomes. Lerman et al.5 reported that the presence of depressive symptoms significantly reduced rates of genetic testing for Lynch syndrome (LS), a dominantly inherited cancer susceptibility syndrome, which is also known as hereditary nonpolyposis colorectal cancer. Specifically, they reported that the presence of depression symptoms resulted in a 4-fold decrease in test use among women and a smaller, nonsignificant reduction among men. Additional research has shown that having high levels of cancer worry9 and intrusive thoughts about breast cancer10 are negatively associated with breast cancer screening. Collectively, these findings demonstrate the clinical importance of considering the psychological well-being of those presenting for genetic services. However, limited data exist on the psychological impact of the cascade sampling approach used to offer genetic services within families. Koehly et al.11 reported that sisters in families with inherited breast and ovarian cancer were more likely to share perceptions of their breast cancer risk and worry. In addition, their levels of anxiety and somatization were associated with strong interpersonal relationships and high levels of communication among family members. The familial context of genetic test results (e.g., portion of women, order of testing within a sibship, and knowledge of the siblings’ results) might influence an individual’s reaction to their own results including levels of distress.12 For example, male carriers of a BRCA mutation, relative to noncarriers, experienced significantly more distress if they were the first tested within their sibship than when all of their tested siblings were already known to be negative.12 Similarly, when one sibling was found to carry the family mutation for hereditary breast and ovarian cancer and the other was not, their communication patterns included more anger, and they were more likely to perceive their sibling to be less friendly and more dominant during conversations compared with sibling pairs with the matching results.13 Early studies exploring relationships between siblings undergoing presymptomatic testing for Huntington disease (linkage based) also documented that some noncarriers reported that their carrier or untested siblings were hostile or resentful toward them after receipt of genetic test results.14 In the context of families LS, perceptions about family environment such as cohesion and conflict were associated with how test recipients psychologically adapted after genetic testing.15 Although helpful, these studies provide limited insight into the psychological, emotional, and behavioral impact resulting from the most common approach to providing genetic services within families known to carry a deleterious mutation (e.g., cascade testing).
Rolland and Williams16 provide a theoretical framework for considering the psychosocial challenges of individuals and families facing inherited disease and receiving genetic services over time through the Family System Genetic Illness (FSGI) model. The model puts forth key factors such as disease likelihood based on the specific mutation, clinical severity, timing of disease onset within the life cycle, and whether effective treatments exist to alter the disease onset or progression. This model suggests that for disorders in which predictive or susceptibility testing are available and comprehensive information is provided, salient developmental challenges exist pre and posttesting for family members. These challenges may affect how individuals and families respond to the information and result in differing cognitive or emotional responses dependent on the individual’s position within their life cycle. For example, individuals who are (1) below an age typical for disease onset or (2) older and whom have not been diagnosed with the family’s disease may not experience the same level of distress as those within an age range during which the disease is most likely to occur. On the basis of the FSGI model, we hypothesize that family members, who are of similar chronological age as the family index case, will experience higher levels of distress compared with family members who are either older or younger.
As noted, the FSGI model puts forth the concept of time phases as a way to think about the ongoing process of an individual’s adaptation to disease risk in response to the receipt of genetic services. However, the cumulative affects resulting from the recurring provision of genetic risk information within the family are not fully considered within the model. At any point of time, some family members will be in the process of becoming aware of the hereditary nature and associated risks for disease, whereas others will be considering the option of genetic testing, going through the process of testing or adapting to genetic test results. Overlaying these challenges will be an incidental diagnosis of disease or possibly the loss of a family member to the inherited disease, which may further complicate the psychosocial responses. The unfolding of this dynamic process has the potential to challenge (1) relationships within the family, (2) previous beliefs about one’s risk for disease, (3) attitudes about genetic testing, (4) uptake of medical screening, and (5) the psychological well-being of those presenting for genetic services. Therefore, it seems plausible that those coming into the system later have greater potential to be influenced by the ever-growing levels of family knowledge, experience, beliefs, and perspectives about their risk for hereditary disease.
In an effort to understand this dynamic process, we used Pescosolido’s Network Episode model.17 Pescosolido’s model proposes that an individual does not always make health-related decisions alone or necessarily in a rational manner. Specifically, the model proposes that family members, health care providers, close friends, and others may heavily influence an individual’s entry into health care services. The model takes into account preceding events, information, and beliefs in a dynamic manner, respecting the sequence of those events and the multiple options available at any given point in time. Thus, actions, decisions, and outcomes become interwoven in a social process that involves the individual within a network that changes over time. For families receiving genetic services through a cascading approach, this network is periodically infused with new disease risk information and experiences with disease, which may challenge previously held beliefs, perspectives, and psychological well-being. The application of this model seems particularly appropriate when considering the cascading approach to genetic services and the heavy reliance on family to recruit, educate, support, and encourage other at-risk family members both before and after the receipt of genetic services. On the basis of this model, we hypothesize that pretest psychological and emotional distress will increase for persons who receive genetic services at increasingly distant points in time from when the index case received service.
To investigate the validity of the proposed hypotheses, we examined whether previous family experiences with genetic services for an inherited cancer susceptibility syndrome known as LS were associated with a decline or increase in baseline levels of depressive symptoms, disease worry, and genetic test-related distress among family members who receive genetic services at more distant time intervals. LS, also known as hereditary nonpolyposis colorectal cancer, is a dominantly inherited cancer susceptibility syndrome that predisposes mutation carriers to early onset of colorectal, endometrial, stomach, and ovarian cancer, as well as other, less commonly occurring LS-associated cancers.18 The lifetime risks for the development of colorectal cancer have been estimated to be between 52% (women) and 69% (men), whereas risks for endometrial cancer in women are estimated to be approximately 54%.19 Mutations in four mismatch repair (MMR) genes have been associated with LS (MSH2, MLH1, MSH6, and PMS2) and are clinically available for the purpose of genetic testing. Mutation carriers who initiate colonoscopic screening at an early age with periodic follow-up screening can significantly reduce their risks for developing colon cancer or increase the identification of colon cancer at early stages reducing the mortality and morbidity associated with diagnoses made at later stages.20,21
MATERIALS AND METHODS
The data presented in this article were collected through a protocol approved and monitored by the Institutional Review Boards at the National Human Genome Research Institute (Protocol No. 95-HG-0165) and the National Naval Medical Center (NNMC.1995.0045). All participants received comprehensive information about the protocol and provided written consent before participation. This prospective family cohort study offered genetic counseling and the option of genetic testing to individuals within families identified to have a deleterious mutation in a MMR gene associated with LS.4
The study began by recruiting index cases with a LS-associated cancer that exhibited clinical (early age of onset, multiple primary LS-associated cancers, and family history of LS cancers) and pathologic characteristics (microsatellite instability) of LS.4 After informed consent, the index case completed a baseline questionnaire, which collected demographic information and the dependent variables of interest (depressive symptoms, worry about colon cancer, and distress related to genetic testing), which was followed by their participation in comprehensive genetics education and counseling sessions. The education session was scripted to ensure that all participants received the same information. The education session included information on the genetic and disease risks associated with LS, cancer screening recommendations, risk reduction options and the potential benefits, risks, and limitations associated with genetic testing. The education session was followed by a client-centered counseling session that focused on assisting the participant in making an informed decision regarding genetic testing; both sessions occurred during the initial face-to-face encounter with the participant.
Those interested in pursuing genetic testing had a blood sample collected and sent to a Clinical Laboratory Improvement Amendment-approved laboratory for sequencing of the MMR genes for which clinical testing was available (MLH1, MSH2, and in some cases MSH6). Genetic testing was offered without cost to participants. Participants were provided mutation results in person. Those found to carry a deleterious mutation could invite their adult, FDRs into the study following the same procedures outlined earlier. Subsequent family members found to carry the family mutation, could then invite their FDR into the study reflecting a cascade sampling approach. Thus, the invitation to consider genetic testing was necessarily dependent on biological relatedness and the mutation status of the FDR. In a few cases, second-degree relatives were invited if the intervening relative was deceased.
To investigate the questions put forth, we selected families that had a disease causing mutation identified, had at least two family members who completed baseline questionnaires, and received genetic services through the study on separate occasions.
Variables of interest
The outcome variables of interest included baseline levels of depressive symptoms, worry about cancer, and distress related to genetic testing.
To assess depressive symptoms, we used the 20-item Center for Epidemiology Studies-Depression Scale.22 The Center for Epidemiology Studies-Depression Scale has been widely used in general population samples and in previous research on the impact of genetic testing for LS.23,24 The scale assesses depressive symptomatology and has been shown to correlate with clinical ratings of the severity of depression22; however, it is not an assessment of a psychiatric diagnosis. Scores range from 0 to 60 with higher scores indicating a greater frequency and/or intensity of depressive symptoms. Published guidelines suggest individuals who score 16 or higher are experiencing clinically significant symptoms of depression.22
To assess the level of worry about colon cancer, we used the Cancer Worries Scale,5 adapted for colon cancer. The Cancer Worries Scale is a 3-item scale, which assesses the frequency of worry about colon cancer and the impact of worry on mood and daily activities. Scores can range from 3 to 12 with higher scores indicating a greater impact of worry on mood and daily activities. To our knowledge, scores indicating clinically significant levels of cancer worry have not been suggested.
To assess distress associated with genetic testing for cancer susceptibility, we used the 15-item Impact of Events Scale-Revised.25 This scale measures the extent to which an individual is experiencing symptoms of intrusive thoughts (Intrusive subscale) and periods of avoidance, blocking, or denial of distress (Avoidance subscale). Overall scores ranged from 0 to 75, with higher scores indicating greater distress. Total scores of 26 or higher are considered to reflect high levels of stress.
The independent variables considered within the analyses included (1) time (calculated in months) since genetic test results were provided to the index case and (2) the generation of the family member relative to index case. The generation of each participant was categorized as the (1) same, if the family member was a sib, first or second cousin, (2) older, if the family member was a parent, uncle/aunt, or grandparent, or (3) younger, if the family member was a child, grandchild, nephew, or niece.
Statistical analyses
Growth curve models were fitted using SPSS 17.026; generalized estimating equations, based on a first-order autocorrelation, were used to account for the clustering of members within families. The first-order autocorrelation structure assumes that psychological responses that occur proximal in time will be more correlated than responses that occur more distant in time. Covariates included within all fitted models were the individual’s gender, personal history of cancer, number of FDRs with a history of cancer, and the participant’s perceived likelihood of being a mutation carrier. Analyses examined the effect of the number of months since disclosure of results to the index case (time) and whether this effect varied due to the generation of the family member relative to the index case. Thus, the index case’s psychological response is the referent at time equal to zero. Models were fitted in two steps. First, controlling for covariates, the effect of time between the provision of genetic services to the family member and the index case was tested. Then, the interaction between time and generation of the family member relative to the index case was tested. Analyses focused on the linear effects of time for two reasons. First, in six families, only two members participated in genetics education and counseling on different dates, reducing the information these families could provide to a curvilinear model. Second, the small number of respondents in the older generation subgroup (n = 36 participants) limited the power to estimate curvilinear effects for this subgroup and increased the potential to overfit the model.
RESULTS
Table 1 provides characteristics of the sample, which included 297 individuals from 38 families with an identified deleterious mutation in a MMR gene. The mean age of the sample was 42 years (range: 18–83 years) and 59% were women. The sample was predominantly white (96%), health insured (95%), and employed (72%). Twenty-five percent reported a personal history of cancer.
Table 1.
Sample characteristics
| Generation (relative to index case) |
|||||
|---|---|---|---|---|---|
| Demographics | Complete cohort | Index cases | Same | Younger | Older |
| No. participants/No. families | 297/38 | 38/38 | 117/25 | 106/29 | 36/15 |
| Age (yr) | |||||
| Mean | 42 | 49 | 45 | 29 | 61 |
| Range | 18–83 | 22–79 | 18–69 | 18–47 | 40–83 |
| SD | 15.2 | 12.0 | 11.9 | 8.5 | 11.5 |
| Personal history of cancer (%) | 25 (n = 75/297) | 97 (n = 37/38)a | 17 (n = 20/117) | 8 (n = 8/106) | 28 (n = 10/36) |
| Gender (% female) | 59 | 61 | 60 | 59 | 53 |
| Race (% non-Hispanic white) | 96 | 92 | 99 | 93 | 100 |
| Health insured (%) | 95 | 95 | 96 | 94 | 94 |
| Employed (% full or part time) | 72 | 66 | 74 | 81 | 47 |
| CES-D (raw scores) | |||||
| Mean | 10.0 | 10.7 | 9.9 | 10.3 | 9.1 |
| Range | 0–41 | 0–37 | 0–41 | 0–36 | 0–27 |
| SD | 8.2 | 7.7 | 8.6 | 8.5 | 6.1 |
| % scoring at 16 or higherb | 19 (n = 55/285) | 26 (n = 9/35) | 17 (n = 19/112) | 23 (n = 24/104) | 9 (n = 3/34) |
| Cancer worries (raw scores) | |||||
| Mean | 4.6 | 6.1 | 4.5 | 4.4 | 3.9 |
| Range | 3–12 | 3–12 | 3–11 | 3–11 | 3–9 |
| SD | 1.8 | 2.6 | 1.6 | 1.6 | 1.4 |
| % scoring 9 or higherc | 4 (n = 12/288) | 17 (n = 6/35) | 3 (n = 3/113) | 2 (n = 2/105) | 3 (n = 1/35) |
| IES scores (raw scores) | |||||
| Mean | 14.6 | 21.9 | 15.3 | 12.1 | 11.2 |
| Range | 0–61 | 0–61 | 0–57 | 0–51 | 0–44 |
| SD | 14.0 | 15.4 | 14.6 | 12.3 | 12.9 |
| % scoring at 26 or higherb | 20 (58/284) | 40 (n = 13/35) | 23 (27/116) | 13 (13/101) | 13 (4/31) |
| Time (mo)d | |||||
| Mean | 10.2 | NA | 6.5 | 18.3 | 9.0 |
| Range | 0–102 | NA | 0–43 | 0–102 | 1–35 |
| SD | 15.6 | NA | 8.5 | 21.3 | 10.3 |
One index case presented with a MSI high, adenomatous polyp in the presence of a family history meeting Amsterdam criteria.
Scores suggesting symptoms of clinical significance.
Report frequent thoughts (1) about developing cancer; (2) that affects their mood; and (3) that affects their daily living activities.
Time between genetic risk notification and provision of genetic services to at risk relative.
SD, standard deviation; IES, Impact of Events Scale; MSI, microsatellite instability.
Depressive symptoms
Considering the main effect for time, our analyses indicate that there is no significant change in the mean number of depressive symptoms reported at baseline due to the increasing time interval between the provision of genetic test results to the family’s index case and the baseline assessment of the participant (P = 0.17) when controlling for covariates and family clustering. Similarly, there was no significant variation in the mean number of depressive symptoms reported when considering the generation of the family member relative to the index case.
Worry about cancer
In regards to participants’ level of worry about colorectal cancer, there was no significant change (P > 0.20) in worry about colon cancer as the interval of time increased between genetic services to family members. Figure 1 presents expected changes in levels of cancer worry over time (the number of months since disclosure to the index case) as a function of generation of the family member. The analyses controlled for covariates and are presented for each generation. As Figure 1 illustrates, there was significant variation (P = 0.001) depending on the generation of the family member, with members in the same generation as the index case reporting a significant increase in levels of cancer worry as the time interval increased. In contrast, there were no significant trends in worry about cancer for those members in the older or younger generation (P values >0.20).
Fig. 1.
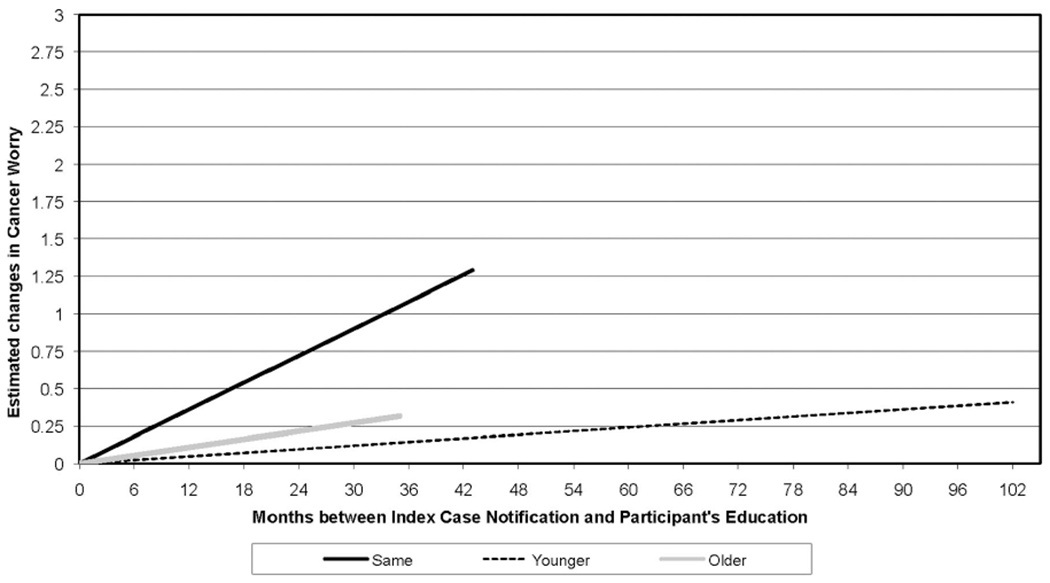
Estimated change in cancer worry. The y-axis represents the estimated change in Cancer Worry Score based on the linear growth model. The x-axis represents the interval of time in months between the provision of genetic test results to the index case and the provision of genetic counseling to family members. Separate lines are provided for each generation. The zero point on the x-axis represents the index case, thus the line represents expected change in cancer worry relative to the index case’s cancer worry, controlling for covariates. Lines were truncated at the point at which data ended within each generation.
Psychological distress related to the receipt of genetic services
Our analyses of the data on distress associated with the provision of genetic services identified no significant change in test-related distress as the interval of time increased between results notification to the index case and their own genetic services (P > 0.20). Figure 2 presents expected changes in levels of distress over time (the number of months since disclosure to the index case) as a function of generation of the family member. The analyses controlled for covariates and are presented for each generation. As Figure 2 illustrates, an interesting interaction was observed between the generation of the family member and the interval of time elapsed. Specifically, family members in the same generation as the index case demonstrated a significant increase (P = 0.003) in distress associated with the receipt of genetic services with increasing intervals of time from when the index case first received their test results. There seemed to be no significant trends for those members in the older and younger generation (P > 0.20).
Fig. 2.
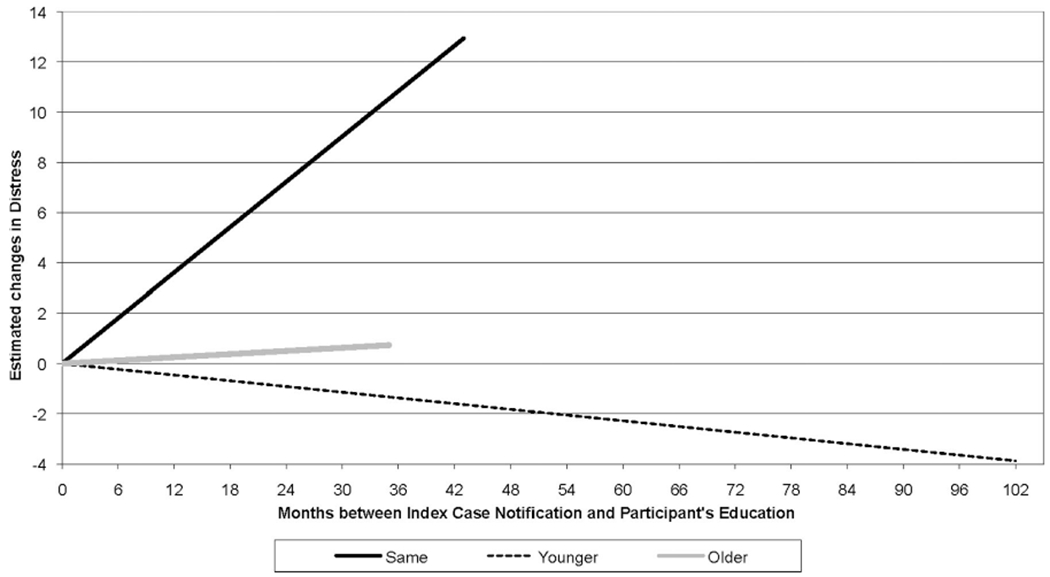
Estimated change in distress related to genetic testing. The y-axis represents the estimated change in Impact of Events Score (distress) based on the linear growth model. The x-axis represents the interval of time in months between the provision of genetic test results to the index case and the provision of genetic counseling to family members. Separate lines are provided for each generation. The zero point on the x-axis represents the index case, thus the line represents expected change in distress relative to the index case’s distress, controlling for covariates. Lines were truncated at the point at which data ended within each generation. Negative values presented within the younger generation reflect scores that are lower than the Index case rather than negative scores on the Impact of Events Scale.
DISCUSSION
To our knowledge, this is the first study to report on the psychological implications associated with the cascading provision of genetic risk information to families with an inherited disease. Understanding the influence of the cascading approach on family members who are yet to receive genetic services seems imperative as the genomic influences of both common and rare diseases continue to unfold and become available to the Public. The findings provide important insights for the clinical provision of information and counseling for families with LS and potentially other inherited or familial diseases. Our findings also have significance for the development of research investigating social influences (e.g., family environment, and culture) and communication practices of family members receiving genetics services.
This study found that the generation of the family member interacts with the time interval of service provision, such that family members in the same generation as the index case experience increasing worry about cancer and distress related to genetic testing with increasing time intervals between the provisions of genetic services. For the sake of clarity, this means that if multiple family members in the same generation as the index case (siblings and cousins) receive genetic services at different times, the relative who received services in closer time proximity to the index case would be predicted to have lower levels of worry about cancer and test-related distress than relatives arriving for services later. Although we had hypothesized independent influences of time and generation on psychological well-being, our results show significance only occurred through their interaction.
The reported interactions are quite plausibly, the result of varying and complex etiologies such as (1) the ever growing number of relatives identified as mutation carriers within the family, (2) contradictions in actual mutation results compared with expected results, especially for socially close family members, or (3) the possibility that individuals with higher levels of disease worry or distress postpone obtaining genetic services compared with those with lower levels. Our data do not allow definitive conclusions to be drawn in this regard. However, considering the dynamic nature of a family’s experience with inherited disease and the genetic testing process, arguments can be made for the noted increases to be the result of “contagion effects” within the generation of the index case. Within this context, contagion effects refer to the communication and spread of influential ideas, doctrines, or emotional states related to the family’s experience with cancer and genetic risk information. We suggest that the contagion effects occur as genetic information is repeatedly provided to and then revisited (shared) within the family over time, resulting in changes in perceptions about risk and psychological well-being. The exchange of information within the family is likely to include a dynamic mix of facts, beliefs, feelings, observations, experiences, and interpretations that ultimately increase cancer worry and test-related distress, consistent with the Network Episode model.
The fact that our significant findings were limited to family members within the same generation as the index case is of interest. LS has been reported to have a median age of diagnosis ranging from 44 to 61 years.19 The mean age of family members within our study and in same generation as the index case was 45 years. As described within the FSGI model, the timing or anticipated onset of the disease within the life cycle is one of the more significant psychosocial factors facing individuals at risk for inherited disease. In our sample, individuals within the same generation as the index case are not only within the age typical of clinical onset but may also face additional concerns as their adolescent and young adult children near the age when recommendations for colon cancer screenings starts. These challenges may compound pretest levels of psychological well-being as the information and risks become clarified, and personal meanings are adjusted through the repeated exposure of the family to genetic services.
In contrast, younger family members may not feel that the information and potential risks have an immediate impact, which may allow them to process the genetic risk information differently. The lack of change in psychological well-being relative to the index case with increasing time intervals may partly be due to a tendency of younger family members to focus on the present, i.e., issues of most immediate relevance.27 In our cohort, the younger generation had a mean age of 29 years, which is below the median ages reported for diagnosis of LS-associated cancers. This potentially serves to lessen the psychological challenges of younger generations receiving genetic risk information and is consistent with postulates put forth within the FSGI model. Existing literature also suggests that the interactions with younger family members may be less difficult than those that occur with relatives of similar ages. For example, among families with mutations in genes associated with inherited breast and ovarian cancers (BRCA1/2), Wagner Costalas et al.28 reported that the communication of genetic risk information between the index case and siblings (same generation) was perceived as significantly more difficult than communications with their children (younger generation). The perceived difficulty in communications between individuals in the same generation of the index case may serve to heighten distress and worry about disease as the interval of time increases within this generation.
For family members in generations older than the index case, developing evidence-based rationale for the lack of change in cancer worry and test-related distress becomes more problematic. It is feasible that persons in older generations, particularly those who have not been diagnosed with disease and potentially out of the typical age range for cancer diagnosis within their family, may feel some level of optimism (psychological reassurance) that they will not develop the family disease, thereby lessening the psychological challenges to both themselves and their children. This psychological reassurance does indeed have objective support when considering Bayesian concepts; those family members who reach increasingly older ages without the diagnosis of cancer have decreasing probabilities of being carriers of a MMR mutation.
Although further studies are needed to replicate these findings, we encourage an examination of the traditional approaches used in providing genetic services to families (cascading approach) when considering the education and counseling aspects of genetic services. Certainly, caution is needed in developing intervention trials or instituting new approaches in providing genetics education and counseling, as the complex issues related to the family’s social influence and communication practices are not likely to be addressed by a “one size fits all” approach.7 Research focused on identifying or developing feasible and effective family-based strategies to facilitate this process is warranted with the goal of lessening the distress associated with the processes.
Furthermore, because both time and social influence are suggested to play a role in pretest psychological well-being, researchers and health care providers may consider providing information and counseling to greater numbers of family members soon after the identification of a family mutation, most notably to those family members within the same generation as the index case. Lynch29 suggested a family information service as one possible model to facilitate the dissemination of information within families. This model also provides an opportunity for the professional to discuss issues that are typically seen as difficult or uncomfortable between relatives.30–32 The simultaneous delivery of information to multiple family members reduces the reliance on the family to accurately share complicated information, may facilitate support within the family, and addresses the variability in time intervals between the provisions of genetic services. Meeting family members soon after the initial detection of the family mutation and providing basic information about genetic susceptibility, cancer prevention, and detection strategies and addressing issues related to cancer worry and test-related distress may provide an opportunity to alleviate detrimental effects reported especially among those who are in the same generation as the index case. This approach will ideally allow health professionals to facilitate family cohesion and decrease family conflict, which have been associated with better psychological well-being.15 Such a family-based approach presents some obvious challenges from a practical perspective and at a minimum would require a more active role by genetics professionals in facilitating the dissemination of information and counseling within families. Furthermore, the delivery of services to multiple family members within one setting raises concerns regarding privacy especially for family members not wishing to share their decisions or test results.33 Other methods may also be considered, which use technologies such as video and teleconferencing or internet-based approaches to provide information and counseling to family members.
In considering the merits of our findings, it is important to acknowledge the limitations. Our sample was largely white, health insured, and employed, which may limit its application to broader populations. The small sample size of family members in generations older than the index case is not only likely an artifact of cascade sampling but may also serve to limit power to detect differences within that generation. As noted, this study used families with LS as a model to explore the psychological implications of the provision of genetic services through a cascading approach. Therefore, caution is necessary in extrapolating these findings to populations with other inherited diseases, including diseases arising from different genetic mechanisms (e.g., recessive and X-linked diseases and chromosomal translocations), with varying degrees of clinical severity, differences in the age of symptom onset, and availability of effective options for prevention and treatment. Furthermore, we did not control for the impact of family members who were diagnosed or died from cancer during the study. Such traumatic events may raise levels of test-related distress and worry about cancer and should be considered in future studies.
Our findings suggest that providers of genetics services should increasingly strive to consider the social influence of family on their individual patients over time, especially those within the same generation as the index case. Service providers may be able to improve psychological outcomes as genetic services are provided to families by facilitating consideration of family level issues related to (1) the process of sharing risk information within the family, (2) reactions to the outcomes of testing, (3) the perception of family culture surrounding genetic risk, and (4) the development of a plan to optimize the family environment to facilitate effective communication. We encourage additional research that broadly examines the social influence of families and as such work may result in family-based interventions that facilitate the psychological and behavioral adaptation of individuals to genetic risk information.
ACKNOWLEDGMENTS
This research was supported by the Intramural Research Programs of the National Human Genome Research Institute (Z01HG000059-11; PI: Koehly) and the National Cancer Institute at the National Institutes of Health in Bethesda, Maryland.
Jean C. Martin currently attends Indiana University School of Medicine (Indianapolis, Indiana) and Natalia Kuhn is currently employed by the Southwest Foundation for Biomedical Research (San Antonio, TX). Ms. Martin and Ms. Kuhn were post-baccalaureate trainees within the Social and Behavioral Research Branch of the National Human Genome Research Institute at the National Institutes of Health when this manuscript was conceptualized and developed.
The authors acknowledge the generosity of the families who participated in the study. They are truly grateful for their willingness to openly share their thoughts, feelings, relationships, and health behavior practices allow this work to be possible. They also thank Andrea Giroux, MHS, for her assistance in creating the figures included within the manuscript.
Footnotes
Publisher's Disclaimer: Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Departments of the Navy, Defense, Health and Human Services, nor the U.S. Government.
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.de Snoo FA, Riedijk SR, van Mil AM, et al. Genetic testing in familial melanoma: uptake and implications. Psychooncology 2008;17:790–796. [DOI] [PubMed] [Google Scholar]
- 2.Christiaans I, Birnie E, Bonsel GJ, Wilde AA, van Langen IM. Uptake of genetic counselling and predictive DNA testing in hypertrophic cardiomyopathy. Eur J Hum Genet 2008;16:1201–1207. [DOI] [PubMed] [Google Scholar]
- 3.Finlay E, Stopfer JE, Burlingame E, et al. Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test 2008;12:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hadley DW, Jenkins J, Dimond E, et al. Genetic counseling and testing in families with hereditary nonpolyposis colorectal cancer. Arch Intern Med 2003;163:573–582. [DOI] [PubMed] [Google Scholar]
- 5.Lerman C, Hughes C, Trock BJ, et al. Genetic testing in families with hereditary nonpolyposis colon cancer. JAMA 1999;281:1618–1622. [DOI] [PubMed] [Google Scholar]
- 6.Marsden PV, Friedkin NE. Network Studies of Social Influence. Sociological Methods & Research 1993;22:127–151. [Google Scholar]
- 7.Gaff CL, Clarke AJ, Atkinson P, et al. Process and outcome in communication of genetic information within families: a systematic review. Eur J Hum Genet 2007;15:999–1011. [DOI] [PubMed] [Google Scholar]
- 8.Meiser B Psychological impact of genetic testing for cancer susceptibility: an update of the literature. Psychooncology 2005;14:1060–1074. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz MD, Taylor KL, Willard KS. Prospective association between distress and mammography utilization among women with a family history of breast cancer. J Behav Med 2003;26:105–117. [DOI] [PubMed] [Google Scholar]
- 10.Lerman C, Kash K, Stefanek M. Younger women at increased risk for breast cancer: perceived risk, psychological well-being, and surveillance behavior. J Natl Cancer Inst Monogr 1994;(16):171–176. [PubMed] [Google Scholar]
- 11.Koehly LM, Peters JA, Kuhn N, et al. Sisters in hereditary breast and ovarian cancer families: communal coping, social integration, and psychological well-being. Psychooncology 2008;17:812–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith KR, West JA, Croyle RT, Botkin JR. Familial context of genetic testing for cancer susceptibility: moderating effect of siblings’ test results on psychological distress one to two weeks after BRCA1 mutation testing. Cancer Epidemiol Biomarkers Prev 1999;8:385–392. [PubMed] [Google Scholar]
- 13.Hamann HA, Smith TW, Smith KR, et al. Interpersonal responses among sibling dyads tested for BRCA1/BRCA2 gene mutations. Health Psychol 2008;27:100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meissen GJ, Myers RH, Mastromauro CA, et al. Predictive testing for Huntington’s disease with use of a linked DNA marker. N Engl J Med 1988;318:535–542. [DOI] [PubMed] [Google Scholar]
- 15.Ashida S, Hadley DW, Vaughn BK, Kuhn NR, Jenkins JF, Koehly LM. The impact of familial environment on depression scores after genetic testing for cancer susceptibility. Clin Genet 2009;75:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rolland JS, Williams JK. Toward a biopsychosocial model for 21st-century genetics. Fam Process 2005;44:3–24. [DOI] [PubMed] [Google Scholar]
- 17.Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. Am J Soc 1992;97:1096–1138. [Google Scholar]
- 18.Lynch HT, Lynch PM, Lanspa SJ, Snyder CL, Lynch JF, Boland CR. Review of the Lynch syndrome: history, molecular genetics, screening, differential diagnosis and medicolegal ramifications. Clin Genet 2009;76:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hampel H, Stephens JA, Pukkala E, et al. Cancer risk in hereditary nonpolyposis colorectal cancer syndrome: later age of onset. Gastroenterology 2005;129:415–421. [DOI] [PubMed] [Google Scholar]
- 20.Jarvinen HJ, Aarnio M, Mustonen H, et al. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 2000;118:829–834. [DOI] [PubMed] [Google Scholar]
- 21.Lindor NM, Petersen GM, Hadley DW, et al. Recommendations for the care of individuals with an inherited predisposition to Lynch syndrome: a systematic review. JAMA 2006;296:1507–1517. [DOI] [PubMed] [Google Scholar]
- 22.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 23.Gritz ER, Peterson SK, Vernon SW, et al. Psychological impact of genetic testing for hereditary nonpolyposis colorectal cancer. J Clin Oncol 2005;23: 1902–1910. [DOI] [PubMed] [Google Scholar]
- 24.Claes E, Denayer L, Evers-Kiebooms G, et al. Predictive testing for hereditary nonpolyposis colorectal cancer: subjective perception regarding colorectal and endometrial cancer, distress, and health-related behavior at one year post-test. Genet Test 2005;9:54–65. [DOI] [PubMed] [Google Scholar]
- 25.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209–218. [DOI] [PubMed] [Google Scholar]
- 26.SPSS Inc [computer program]. SPSS for Windows, Rel 15.0.1. Version 15. Chicago, IL: SPSS Inc., 2006. [Google Scholar]
- 27.Wickman ME, Anderson NL, Greenberg CS. The adolescent perception of invincibilty and its influence on teen acceptance of health promotion strategies. J Pediatr Nurs 2008;23:460–468. [DOI] [PubMed] [Google Scholar]
- 28.Wagner Costalas J, Itzen M, Malick J, et al. Communication of BRCA1 and BRCA2 results to at-risk relatives: a cancer risk assessment program’s experience. Am J Med Genet C Semin Med Genet 2003;119C: 11–18. [DOI] [PubMed] [Google Scholar]
- 29.Lynch HT. Family information service and hereditary cancer. Cancer 2001; 91:625–628. [DOI] [PubMed] [Google Scholar]
- 30.Blandy C, Chabal F, Stoppa-Lyonnet D, Julian-Reynier C. Testing participation in BRCA1/2-positive families: initiator role of index cases. Genet Test 2003;7:225–233. [DOI] [PubMed] [Google Scholar]
- 31.d’Agincourt-Canning L Experiences of genetic risk: disclosure and the gendering of responsibility. Bioethics 2001;15:231–247. [DOI] [PubMed] [Google Scholar]
- 32.Bonadona V, Saltel P, Desseigne F, et al. Cancer patients who experienced diagnostic genetic testing for cancer susceptibility: reactions and behavior after the disclosure of a positive test result. Cancer Epidemiol Biomarkers Prev 2002;11:97–104. [PubMed] [Google Scholar]
- 33.Loud JT, Weissman NE, Peters JA, et al. Deliberate deceit of family members: a challenge to providers of clinical genetics services. J Clin Oncol 2006;24:1643–1646. [DOI] [PubMed] [Google Scholar]


