Abstract
Social support and social networks are important correlates of elder mistreatment. This study tests hypothesized associations between perceived social support, social network size, and financial exploitation (FE). A population-based survey of 903 older adults (60+) in Allegheny County (Pittsburgh, Pennsylvania) found that lower perceived social support and larger social networks were simultaneously associated with higher risk for FE since age 60, controlling for known risk factors. The same associations were found for FE in the last 6 months. Older adults with larger social networks combined with lower perceived social support were most likely to report FE. When it comes to the role of social relationships and risk for FE, “more may not always be better.” Encouragement to widen the social network by “making new friends” should be stressed less than making sure these new network members will truly be supportive of the older adult.
Keywords: elder abuse, social relationships, risk factors
Introduction
Social networks and social support are key correlates of health, subjective well-being, and quality of life. Larger social networks and higher perceived availability of social support are related to decreased morbidity and mortality, better psychological well-being, and reduced health-risk behaviors (Cohen, 2004; Wills & Ainette, 2012). There have been hundreds of studies exploring the effects of social networks and social support on health-related outcomes in both general and clinical populations (see Wills & Ainette, 2012; Wills & Fegan, 2001, for reviews). Structural measures of social integration like social network size have typically been shown to have “main effects” on health (e.g., larger social networks predict reduced mortality), whereas functional measures of perceived social support have shown “stress buffering” effects (e.g., reduced negative health effects of stress for those having high perceived social support; Cohen, 2004). Of particular interest here, most studies tend not to include both structural and functional measures (Seeman, 1996), and those that do include both tend to show that they are not highly correlated and relate differentially to health outcomes (Wills & Ainette, 2012).
Social networks and social support have also been examined in the context of elder mistreatment (Institute of Medicine [IOM] & National Research Council [NRC], 2014; National Research Council, 2003). The dominant theoretical framework for research on elder mistreatment was proposed by the National Research Council (2003). The model lays out the sociocultural context within which elder mistreatment may occur and prominently features “social embeddedness” in the form of ties to family and friends as a key factor in the dynamics of mistreatment. Empirical research linking social networks and support to elder mistreatment has focused primarily on living arrangements (IOM & NRC, 2014; Lachs, Williams, O’Brien, Hurst, & Horwitz, 1997; National Research Council, 2003; Paveza et al., 1992; Pillemer & Finkelhor, 1988; Pillemer & Suitor, 1992) and social isolation (Compton, Flanagan, & Gregg, 1997; IOM & NRC, 2014; Lachs, Berkman, Fulmer, & Horwitz, 1994; National Research Council, 2003). This research has shown that shared household living arrangements and social isolation are both risk factors for elder mistreatment, which may seem somewhat paradoxical. The research suggests that shared living arrangements increase opportunities for contact, and thus household conflict and mistreatment are also more likely. The social isolation findings are generally interpreted in the context of families that isolate the older adult from the broader social network, thus enabling the mistreatment to remain hidden from view.
A U.S. national elder mistreatment prevalence study by Acierno and colleagues (2010) also highlighted the importance of lack of social support as a risk factor for elder mistreatment. They found “low social support” (i.e., perceived emotional, instrumental, and appraisal support) was the most consistent risk factor for emotional, physical, and sexual mistreatment, and potential neglect, but low social support was not a risk factor for financial mistreatment by family. In another U.S. national study, Laumann, Leitsch, and Waite (2008) found that married older adults were at lower risk of financial mistreatment than those who were not married, but that marital status was not related to verbal mistreatment. A national prevalence study in Canada found that victims of “material abuse” (i.e., financial exploitation [FE]) were less likely to have “someone to trust and confide in,” and “someone who would help them if they became ill” (Podnieks, 1993). Podnieks (1993) also found that victims of material abuse were less likely to be married, in contrast to verbal and physical abuse victims, who were more likely to be married. In sum, the national prevalence studies in the United States and Canada suggest that the role of social support may differ somewhat for FE than for other types of elder mistreatment such as verbal/psychological and physical abuse (Acierno et al., 2010; Laumann et al., 2008; Podnieks, 1993).
Two recent studies using the same national data as the Laumann et al. (2008) study provided a more detailed picture of social networks, social support, and elder mistreatment. Luo and Waite (2011) found that “positive social support” predicted lower likelihood of any mistreatment (emotional, physical, or financial not separately examined), whereas criticism from close relationships and perceived social isolation were related to higher likelihood of mistreatment. Interestingly, greater “social participation” was also related to higher levels of mistreatment. Schafer and Koltai (2015) found that older adults with more “dense social networks”—measured as the proportion of all listed network members who saw or spoke to each other more than once a year—were less likely to report any mistreatment, whereas simple “network size” was unrelated to risk for mistreatment. Interestingly, they also found that while close to half of the perpetrators of emotional and physical mistreatment were network members, only slightly more than 20% of those perpetrating financial mistreatment were network members.
Additional empirical work is needed to further clarify the association between perceived social support, social networks, and FE. The National Center on Elder Abuse (NCEA) defines FE as the “illegal taking, misuse, or concealment of funds, property, or assets of a vulnerable elder.” Although the literature to date is fairly consistent in showing that low perceived social support is a risk factor for elder mistreatment, the role of more objective social network indicators is less clear. Shared living arrangements have been shown to be a risk factor for certain types of elder mistreatment, but being married seems to protect older adults against FE. “Dense” social networks have been related to lower risk for mistreatment, but “social participation” was related to increased risk. Does having a large social network and being in frequent contact with people protect older adults from FE? Or does such a large social network place the older adult at higher risk because it increases the opportunity for FE? How do perceived social support and social network size relate to FE when considered simultaneously? Do social network size and perceived social support interact to affect risk for FE?
This study extends previous research in this area by simultaneously assessing the effects of perceived social support and social network size on FE. We predict that higher levels of perceived social support will be related to lower risk for FE (Hypothesis 1) and larger social networks will be related to higher risk for FE (Hypothesis 2). We will test these hypotheses both when the variables are examined separately, as in previous studies, and simultaneously. We will also extend prior research by exploring statistical interactions between social network size and perceived social support as predictors of FE, but offer no hypotheses. Perhaps having large social networks combined with high perceived support puts the older adult at the lowest risk for FE; or a large network combined with low perceived support produces the highest risk. To better understand social network dynamics and FE, we also conduct supplemental analyses separately exploring family and non-family network size and FE.
Method
More detailed survey methods on sample design, procedures, and response rates have been reported elsewhere (Beach, Schulz, Castle, & Rosen, 2010; Beach, Schulz, Degenholtz, et al., 2010). Here, we provide a summary overview of these methods, along with a description of study measures and statistical analysis methods. All study procedures were approved by the University of Pittsburgh Institutional Review Board.
Survey Sample Design, Procedures, and Response Rate
The target population was adults 60 years and older residing in households with landline telephones in Allegheny County (Pittsburgh, Pennsylvania). Additional eligibility criteria included English speaking and no severe cognitive impairment (see below). Random digit dialing (RDD) telephone sampling with screening for age was used to recruit the sample. The study involved a randomized survey mode experiment, results of which are presented elsewhere (Beach, Schulz, Degenholtz, et al., 2010). This article reports on results of the four methods combined (two telephone-based and two in-person), and all multivariate analyses (see below) include experimental condition as a control variable. Interviews were conducted between May, 2007, and January, 2008. The interviews took an average of 45 min to complete. Participants were offered US$10 (telephone) or US$20 (in-person) supermarket gift cards as incentives. The goal was to complete 900 surveys. To achieve this, 35,162 telephone numbers were dialed. Among the 2,395 numbers which screened eligible for the survey (at least one person 60 or older in household), we completed 903 interviews for an interview completion rate of 37.7%.
Measures
This study focuses on FE since turning 60 to be consistent with the elder abuse statutes in the state of Pennsylvania. Analyses of more recently occurring FE (in the past 6 months) were also conducted.
FE was measured with four items, adapted from work by Quinn and Tomita (1986): (a) Have you signed any forms or documents that you didn’t quite understand? (b) Has anyone asked you to sign anything without explaining what you were signing? (c) Has anyone taken your checks without permission? and (d) Have you suspected that anyone was tampering with your savings or other assets? The items were in a yes/no format and asked for occurrence since turning 60, and if yes, in the last 6 months. Those responding “yes” to any of the four questions were considered to have experienced FE. This measure has been used as a primary outcome in previous research reports (Beach, Schulz, Castle, & Rosen, 2010; Beach, Schulz, Degenholtz, et al., 2010).
Perceived social support was measured using the 12-item “Interpersonal Support Evaluation List” (ISEL; Cohen, Mermelstein, Kamarck, & Hoberman, 1985). This is a widely used scale which measures three domains, containing four items each: (a) “appraisal” support (availability of someone to talk to about problems), “tangible” support (availability of material aid), and “belonging” support (availability of people one can do things with). Items, which were worded both positively and negatively, use a 4-point scale (1 = definitely false, 2 = probably false, 3 = probably true, 4 = definitely true), and were scored such that high scores mean higher perceived support. We used the total 12-item score for the current analyses (Cronbach’s α = .81).
Social network size was measured with the “Social Network Index” (SNI; Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997), specifically the “number of people in social network” measure. This is the number of people with whom the respondent has regular contact (i.e., at least once every 2 weeks). The number of network members is computed across 12 respondent social roles—spouse, parent, child, child-in-law, close relative, close friend, church/temple member, student, employee, neighbor, volunteer, and group member. A screener question for the presence of each role (e.g., presence of children, living parents, employed or not, student or not, etc.) is followed (if applicable) by a question asking how many people in that role the respondent has contact with once at least every 2 weeks. The SNI does not ask about co-residence with network members.
We collected standard demographic information including sex, race, age, and education level. Race was categorized as African American, White, and Other (which were combined for analyses). Age was analyzed as a continuous variable. Education was coded into four categories (less than high school, high school graduate, some college or technical school, college graduate), and high school graduate (the most common) was used as the reference category.
Household living arrangements were assessed with two questions: (a) “Excluding yourself, how many other people live in your home?” and (if one or more others live with the elder) (b) “Who all lives in your home?” The second question was coded for spouse, son, daughter, other family members, and non-family and these were entered as separate indicator variables in the models (along with whether the older adult lived alone).
Physical disability was assessed with six standard yes/no format Instrumental Activities of Daily Living (IADL) difficulty (heavy housework, light housework, shopping, preparing meals, managing money, and using phone) and six Activities of Daily Living (ADL) difficulty (eating, dressing, bathing, using the toilet, walking around the home, and bed/chair transfers) items. Presence of any IADL and any ADL difficulties (entered separately) was used for statistical analysis.
Depression symptoms were assessed using the 10-item version of the Center for Epidemiologic Studies Depression Scale (CESD; Shrout & Yager, 1989). Based on the traditional cutoff of 16 or higher suggested for the original 20-item CESD (Radloff, 1977), scores of 8 or higher on the scale were used to indicate risk for clinical depression. The dichotomized variable was used for statistical analysis.
Cognitive function was assessed with the brief measure of cognitive status designed for administration over the telephone for the Asset and Health Dynamics Among the Oldest Old (AHEAD) study described by Herzog and Wallace (1997). The measure taps memory (immediate and delayed free recall, working memory), knowledge, language, and orientation. A total score ranging from 0 to 25 is derived and the authors suggest scores of 8 or below indicate severe cognitive impairment. If the respondent had made it to this point in the interview (which occurred fairly early), anyone scoring 8 or below was not interviewed further and considered to be ineligible. A total of nine respondents were screened ineligible due to cognitive impairment. Cognitive function is analyzed as a continuous variable.
Statistical Analysis
This article focuses on associations between perceived social support, social network size, and FE since turning 60 and in the last 6 months. Note that those reporting FE in the last 6 months are a subset of those reporting FE since age 60. Sample descriptions use percentages for categorical variables, and means and standard deviations for continuous variables. Bivariate associations with FE are tested using t tests for continuous variables (perceived social support, social network size, age, cognitive function) and χ2 methods for the remaining categorical covariates. Associations between perceived social support, social network size, and FE are tested in a multivariate context through logistic regression models, and odds ratios and standard errors are reported. For comparative purposes, separate logistic models are tested with perceived social support only (plus all other covariates), social network size only (plus covariates), and a model including both perceived social support and social network size (plus covariates). Other covariates in all models include gender, race, age, education level, household living arrangements, physical disability, cognitive function, and risk for clinical depression. All models also control for mode of data collection from the randomized experiment (see above; results not shown). Statistical interactions between perceived social support and social network size are tested using mean-centered cross-product terms (Aiken & West, 1991).
For the bivariate comparisons, separate tests are conducted comparing (a) older adults with no reported FE since turning 60 versus those reporting FE since age 60, and comparing (b) older adults with no reported FE in the last 6 months versus those reporting FE in the last 6 months. All available data are used for the bivariate tests. In the multivariate models, only the 864 cases having data on all covariates and the perceived social support and social network size measures are included (n = 39 cases with missing data on at least one covariate are dropped from the multivariate analyses). There were no significant differences between the 39 missing cases and the 864 analysis cases on gender, race, education, physical disability, depression, and household composition. The missing cases were significantly older (M = 76.7 vs. 72.4, p < .01) and had significantly lower cognitive scores (M = 19.5 vs. 22.1, p < .01) than those included.
Statistical weights were applied prior to analysis to incorporate the complex survey design, which included an over-sample of African Americans. The weight contained two components: (a) a base design weight for the probability of selection of the phone number, and (b) a post-stratification adjustment based on six Gender × Age cells (60-64, 65-74, 75 and older) using the most recent American Community Survey (ACS) estimates for the county. The post-stratification weight adjusted for differential non-response across the gender/age cells. Analyses were performed using the complex survey module (“svy” commands) in STATA version 10.0.
Results
Sample Descriptive Statistics
Tables 1 (categorical covariates) and 2 (continuous covariates) present unweighted descriptive statistics (column 2). The sample was predominantly female (73.3%), and 23.3% were African Americans, with the remainder primarily White non-Hispanic. Mean age of the sample was 72.5 (SD = 8.1) years. More than 50% had at least some college, and nearly half lived alone (48.4%). Thirty-six percent lived with a spouse, less than 10% lived with a son (8.5%) or daughter (6.9%), 10.6% lived with other family members and 2.2% lived with non-relatives. Slightly less than half the sample (43.6%) reported at least one IADL difficulty, with 13.7% reporting at least one ADL difficulty. Cognitive function was high in the sample (M = 22 of 25 maximum), whereas 29.2% met our criteria for “risk for depression.” On the key social network size measure, the sample had a mean of 18.6 (SD = 9.6) people with whom they frequently contact. The mean score on the ISEL (40.5 out of 48; SD = 6.4) indicates high levels of perceived social support. Perceived social support and social network size were moderately positively correlated (r = .39, p < .01).
Table 1.
Sample Descriptive Statistics and Bivariate Tests of Association Between Categorical Covariates and FE.
| Sample descriptive statistics % (n) (un-weighted) | FE since age 60 (weighted %) | FE in last 6 months (weighted %) | |
|---|---|---|---|
| Total sample | 100 (903) | 9.9 | 3.5 |
| Gender | |||
| Male | 26.7 (241) | 8.8 | 3.1 |
| Female | 73.3 (662) | 10.7 | 3.8 |
| Race | |||
| White (not African American) | 76.7 (693) | 8.4 | 2.4 |
| African American | 23.3 (210) | 23.0** | 12.9** |
| Education | |||
| Less than high school | 12.0 (108) | 15.0 | 5.8 |
| High school graduate | 34.7 (313) | 10.0 | 3.3 |
| Some college | 29.5 (266) | 8.5 | 2.4 |
| College graduate | 23.7 (214) | 9.5 | 4.1 |
| IADL disability | |||
| No IADL difficulty | 56.4 (509) | 7.1 | 2.7 |
| IADL difficulty | 43.6 (394) | 14.3** | 4.6 |
| ADL disability | |||
| No ADL difficulty | 86.3 (779) | 9.6 | 3.6 |
| ADL difficulty | 13.7 (124) | 12.5 | 2.2 |
| Risk for depressiona | |||
| No | 70.8 (639) | 7.2 | 2.3 |
| Yes | 29.2 (264) | 17.6** | 6.9** |
| Household living arrangements | |||
| Live alone | 48.4 (436) | 9.8 | 2.9 |
| Do not live alone | 51.6 (465) | 10.0 | 3.9 |
| Live with spouse | 36.0 (325) | 8.4 | 3.8 |
| Do not live with spouse | 64.0 (578) | 11.1 | 3.3 |
| Live with son | 8.5 (77) | 7.4 | 3.4 |
| Do not live with son | 91.5 (826) | 10.2 | 3.5 |
| Live with daughter | 6.9 (62) | 16.6 | 2.5 |
| Do not live with daughter | 93.1 (841) | 9.4 | 3.6 |
| Live with other family | 10.6 (96) | 20.0 | 5.1 |
| Do not live with other family | 89.4 (807) | 9.0** | 3.3 |
| Live with non-family | 2.2 (20) | 5.5 | 4.2 |
| Do not live with non-family | 97.8 (883) | 10.0 | 3.5 |
Note. Descriptive statistics and sample sizes are un-weighted; all other analyses are weighted. All available data are presented for each cell (i.e., pairwise deletion is used). FE = financial exploitation; IADL = instrumental activities of daily living; ADL = activities of daily living; CESD = Center for Epidemiological Studies Depression Scale.
Score of 8 or higher on CESD.
p < .05.
p < .01 in bivariate χ2 tests for differences in FE since turning 60 and in last 6 months by predictor variable. All significance testing accounted for complex survey design (see text).
Table 2.
Sample Descriptive Statistics and Bivariate Tests of Association Between Continuous Covariates and FE.
| Sample descriptive statistics (un-weighted) | No FE since age 60 (weighted) | FE since age 60 (weighted) | No FE in last 6 months (weighted) | FE in last 6 months (weighted) | |
|---|---|---|---|---|---|
| Age | |||||
| M (SD) | 72.5 (8.1) | 72.6 (8.7) | 73.1 (7.5) | 72.7 (8.6) | 71.4 (7.2) |
| Cognitive functiona | |||||
| M (SD) (possible = 0-25) | 22.0 (4.7) | 22.2 (4.4) | 21.6 (5.6) | 22.2 (4.5) | 20.9 (5.0) |
| Social network sizeb | |||||
| M (SD) (range = 0-49) | 18.6 (9.6) | 18.7 (9.6) | 18.7 (9.3) | 18.6 (9.6) | 20.3 (9.4) |
| Perceived social supportc | |||||
| M (SD) (possible 12-48) | 40.5 (6.4) | 41.2 (5.9) | 36.6 (8.1)** | 40.9 (6.2) | 37.0 (8.5)* |
Note. Descriptive statistics and sample sizes are un-weighted; all other analyses are weighted. All available data are presented for each cell (i.e., pairwise deletion is used). FE = financial exploitation; HRS AHEAD = Health and Retirement Study Asset and Health Dynamics Among the Oldest Old; SNI = Social Network Index; ISEL = interpersonal support evaluation list.
p < .05.
p < .01 in bivariate ANOVA tests for differences in FE since turning 60 and in last 6 months by predictor variable. All significance testing accounted for complex survey design (see text).
Assessed by brief telephone measure of cognitive status from the HRS AHEAD study.
SNI “Number of People in Social Network” measure.
ISEL total score.
Bivariate Associations With FE
An estimated 9.9% of the sample had experienced FE since turning 60, whereas 3.5% reported FE in the last 6 months. African Americans were much more likely to experience FE than non-African Americans, both since turning 60 (23.0%) and in the last 6 months (12.9%). Racial differences in this sample are the focus of a prior published report (Beach, Schulz, Castle, & Rosen, 2010). Those reporting at least one IADL difficulty were also more likely to report FE since age 60 (14.3%). Older adults at risk for clinical depression were more likely to report FE since turning 60 (17.6%) and within the last 6 months (6.9%), a finding also highlighted in the previous report (Beach, Schulz, Castle, & Rosen, 2010). Those living with family members other than a spouse or child were also more likely to report FE since age 60 (20.0%). With regard to the key social network/social support variables, older adults reporting both FE since turning 60 (M = 36.6) and in the last 6 months (M = 37.0) had significantly lower perceived social support than those not reporting any FE. There were no significant bivariate differences in FE by social network size.
Multivariate Models for FE Since Turning 60
Table 3 shows results of the multivariate logistic regression models with any FE since turning 60 as the outcome variable (9.9% of the total sample). Three separate models are shown: (a) a model with all covariates plus social network size, (b) a model with all covariates plus perceived social support, and (c) a model with all covariates plus both social network size and perceived social support. The models explained 14.7%, 17.9%, and 20.2% of the total variance, respectively. Results for the additional covariates are basically consistent with the bivariate results just presented for all three models. African Americans, those at risk for clinical depression, and those reporting at least one IADL difficulty were more likely to report FE since turning age 60 (the IADL difficulty and depression findings reach the conventional .05 statistical significance level in only the first model including social network size). Turning to the key social network/social support measures, in Model 1, social network size was not significantly related to FE since age 60 when entered separately. In Model 2, older adults with higher perceived social support were at lower risk for FE since turning 60 (OR = 0.93, p < .001). In Model 3, when both variables are entered simultaneously, older adults reporting larger social network size had higher risk for FE since age 60 (OR = 1.05, p = .003), whereas those with higher perceived social support were at lower risk (OR = 0.90, p < .001). These results provide support for the both hypotheses, although results are more consistent for perceived social support.
Table 3.
Logistic Regression Analyses of Financial Exploitation Since Turning 60 Onto Socio-Demographic Variables, Physical Disability, Cognitive Function, Risk for Depression, Household Living Arrangements, and Social Network/Social Support Measures (n = 864).
| Social network model |
Perceived social support model |
Combined social network and perceived social support model |
||||
|---|---|---|---|---|---|---|
| OR (SE) | p value | OR (SE) | p value | OR (SE) | p value | |
| Male | 1.16 (0.38) | .655 | 0.96 (0.31) | .888 | 1.03 (0.34) | .927 |
| African American | 3.53 (1.08) | <.001 | 3.93 (1.23) | <.001 | 3.90 (1.24) | <.001 |
| Age | 1.01 (0.02) | .489 | 1.01 (0.01) | .546 | 1.01 (0.02) | .571 |
| Educationa | ||||||
| Less than high school | 1.17 (0.53) | .733 | 1.34 (0.64) | .541 | 1.46 (0.69) | .421 |
| Some college | 0.78 (0.29) | .502 | 0.92 (0.33) | .823 | 0.82 (0.30) | .592 |
| College graduate | 1.07 (0.41) | .861 | 1.20 (0.47) | .644 | 1.03 (0.40) | .931 |
| Any IADL difficulty | 1.98 (0.61) | .027 | 1.65 (0.49) | .093 | 1.73 (0.52) | .067 |
| Any ADL difficulty | 0.73 (0.26) | .373 | 0.75 (0.28) | .440 | 0.76 (0.29) | .468 |
| Cognitive functionb | 1.01 (0.04) | .801 | 1.02 (0.04) | .572 | 1.01 (0.04) | .735 |
| Risk for depressionc | 2.68 (0.77) | .001 | 1.65 (0.50) | .097 | 1.75 (0.53) | .065 |
| Household living arrangements | ||||||
| Live alone | 0.65 (0.46) | .549 | 0.66 (0.48) | .567 | 0.58 (0.40) | .432 |
| Live with spouse | 0.76 (0.49) | .673 | 0.98 (0.63) | .972 | 0.86 (0.50) | .800 |
| Live with son | 0.59 (0.34) | .367 | 0.55 (0.30) | .276 | 0.54 (0.29) | .259 |
| Live with daughter | 1.41 (0.73) | .509 | 1.43 (0.73) | .488 | 1.43 (0.70) | .463 |
| Live with other family | 1.75 (1.01) | .334 | 1.71 (1.02) | .369 | 1.60 (0.87) | .390 |
| Live with non-family | 0.46 (0.42) | .391 | 0.37 (0.33) | .271 | 0.40 (0.37) | .318 |
| Social network sized | 1.02 (0.02) | .121 | 1.05 (0.02) | .003 | ||
| Perceived social supporte | 0.93 (0.02) | <.001 | 0.90 (0.02) | <.001 | ||
| Model R2 (Nagelkerke) | .147 | .179 | .202 | |||
Note. All analyses are weighted. All significance testing accounted for complex survey design. IADL = instrumental activities of daily living; ADL = activities of daily living; HRS AHEAD = Health and Retirement Study Asset and Health Dynamics Among the Oldest Old; CESD = Center for Epidemiological Studies Depression Scale; SNI = Social Network Index; ISEL = interpersonal support evaluation list.
Reference category is high school graduate.
Assessed by brief telephone measure of cognitive status from the HRS AHEAD study.
Score of 8 or higher on CESD.
SNI “Number of people in social network” measure.
ISEL total score.
The test of the centered cross-product interaction term for perceived social support by social network size (not shown) was statistically significant (p = .047). A plot of the interaction is shown in Figure 1 using procedures outlined by Aiken and West (1991). It shows that the protective effects of perceived social support are greatest for those with the largest social networks. The negative slope of the predicted probability of FE by ISEL score is less steep for those with small social networks (defined as 1 standard deviation below the mean SNI score), and it is steepest for those with the largest networks (1 standard deviation above the SNI mean). Older adults with large diverse social networks combined with low perceived social support were at highest risk for FE since age 60.
Figure 1.
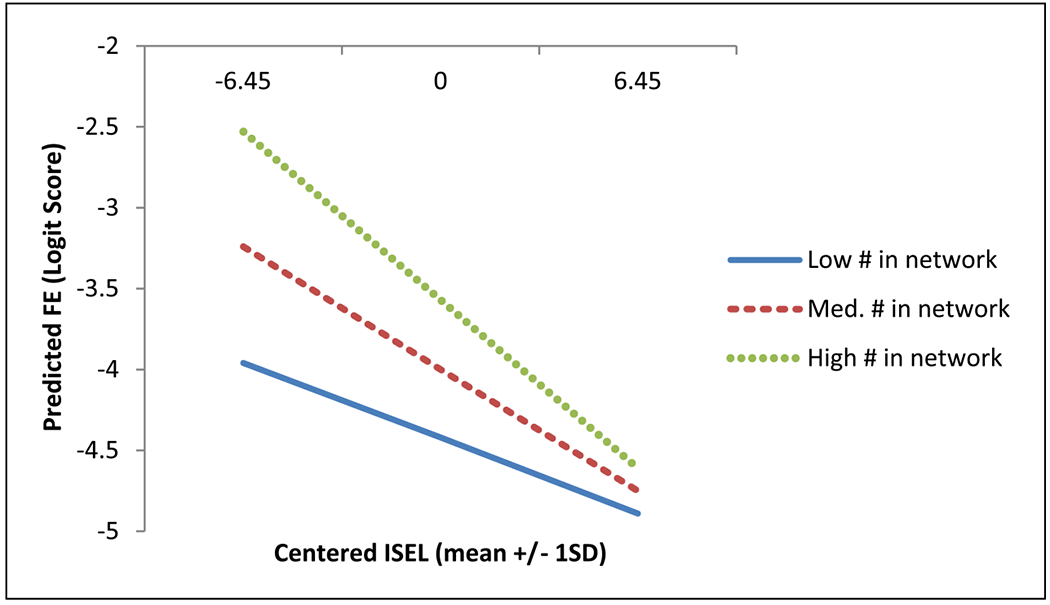
Statistical interaction between perceived social support and social network size on FE since age 60.
Note. FE = financial exploitation; ISEL = interpersonal support evaluation list.
Multivariate Models for FE in the Last 6 Months
Table 4 shows results of the multivariate logistic regression models FE in the last 6 months as the outcome variable (3.5% of the total sample). The models explained 21.8%, 22.3%, and 24.9% of the total variance, respectively. African Americans and those at risk for clinical depression were more likely to report FE in the last 6 months (although the depression effect reached the .05 level of significance in only the first model with social network size). In addition, those reporting any ADL difficulties were less likely to report FE in the last 6 months. The results for the key social network/social support measures showed that neither social network size nor perceived social support were significantly associated with FE in the last 6 months when examined separately. However, when both indicators were included simultaneously, the same pattern found for FE since age 60 was found: older adults reporting larger social network size were at higher risk for FE since age 60 (OR = 1.06, p = .021), whereas those with higher perceived social support were at lower risk (OR = 0.92, p = .017). These results provide additional support for the hypotheses. The test of the centered cross-product interaction term for perceived social support by social network size (not shown) on FE in the last 6 months was not statistically significant (p = .212).
Table 4.
Logistic Regression Analyses of Financial Exploitation in the Last 6 Months Onto Socio-Demographic Variables, Physical Disability, Cognitive Function, Risk for Depression, Household Living Arrangements, and Social Network/Social Support Measures (n = 864).
| Social network model |
Perceived social support model |
Combined social network & perceived social support model |
||||
|---|---|---|---|---|---|---|
| OR (SE) | p value | OR (SE) | p value | OR (SE) | p value | |
| Male | 0.96 (0.48) | .936 | 0.80 (0.40) | .664 | 0.86 (0.44) | .772 |
| African American | 8.25 (3.79) | <.001 | 9.39 (4.38) | <.001 | 8.98 (4.19) | <.001 |
| Age | 0.99 (0.02) | .666 | 0.99 (0.02) | .583 | 0.99 (0.02) | .610 |
| Educationa | ||||||
| Less than high school | 1.57 (1.23) | .565 | 1.56 (1.23) | .574 | 1.86 (1.50) | .442 |
| Some college | 0.71 (0.40) | .543 | 0.83 (0.42) | .709 | 0.77 (0.41) | .619 |
| College graduate | 1.62 (0.95) | .413 | 1.86 (1.06) | .280 | 1.54 (0.90) | .460 |
| Any IADL difficulty | 1.79 (0.84) | .213 | 1.45 (0.68) | .435 | 1.50 (0.71) | .398 |
| Any ADL difficulty | 0.30 (0.15) | .018 | 0.28 (0.15) | .020 | 0.30 (0.17) | .034 |
| Cognitive functionb | 0.97 (0.05) | .558 | 0.98 (0.50) | .750 | 0.97 (0.05) | .609 |
| Risk for depressionc | 3.92 (1.83) | .004 | 2.62 (1.36) | .064 | 2.67 (1.40) | .062 |
| Household living arrangements | ||||||
| Live alone | 0.37 (0.30) | .218 | 0.38 (0.32) | .258 | 0.32 (0.28) | .191 |
| Live with spouse | 0.91 (0.59) | .886 | 1.21 (0.79) | .773 | 1.08 (0.69) | .906 |
| Live with son | 0.55 (0.36) | .360 | 0.57 (0.37) | .391 | 0.56 (0.37) | .383 |
| Live with daughter | 0.45 (0.31) | .244 | 0.44 (0.31) | .244 | 0.49 (0.33) | .290 |
| Live with other family | 0.80 (0.52) | .725 | 0.70 (0.49) | .618 | 0.67 (0.46) | .566 |
| Live with non-family | 0.79 (0.97) | .847 | 0.67 (0.81) | .739 | 0.66 (0.85) | .748 |
| Social network sized | 1.04 (0.02) | .104 | 1.06 (0.03) | .021 | ||
| Perceived social supporte | 0.94 (0.03) | .069 | 0.92 (0.03) | .017 | ||
| Model R2 (Nagelkerke) | .218 | .223 | .249 | |||
Note. All analyses are weighted. All significance testing accounted for complex survey design. IADL = instrumental activities of daily living; ADL = activities of daily living; HRS AHEAD = Health and Retirement Study Asset and Health Dynamics Among the Oldest Old; CESD = Center for Epidemiological Studies Depression Scale; SNI = Social Network Index; ISEL = interpersonal support evaluation list.
Reference category is high school graduate.
Assessed by brief telephone measure of cognitive status from the HRS AHEAD study.
Score of 8 or higher on CESD.
SNI “Number of people in social network” measure.
ISEL total score.
Supplemental Analyses of Family Versus Non-Family Network Size
The SNI measures the size of both family (spouse, parent, child, child-in-law, close relative) and non-family (close friend, church/temple member, student, employee, neighbor, volunteer, group member) social networks. Results showed that larger social networks overall were related to increased risk for FE since turning 60 and in the last 6 months. Is this due to having lots of both family and non-family network members? Or does having more of one type but not the other put the older adult at risk for FE? To explore this, we calculated network size separately for family and non-family contacts and re-ran the logistic regression models shown in Tables 3 and 4 with these two measures substituted for overall network size. Results showed that the reported effects were due exclusively to larger non-family social networks. In all models, larger non-family networks were related to higher risk for FE both since turning 60 and in the last 6 months, whereas the size of the family network was not related to FE. In addition, size of non-family social networks statistically interacted with perceived social support to affect FE risk as shown in Figure 1, whereas family network size and perceived support did not interact.
Discussion
This article reports on associations between perceived social support, social network size, and FE in a population-based survey of adults age 60 and older in the Pittsburgh, Pennsylvania, region. We found that although higher perceived social support was related to lower risk of FE since turning age 60 and in the last 6 months, larger social networks were related to higher risk of FE. These contrasting effects occurred simultaneously in multivariate models controlling for a variety of known risk factors for FE. Furthermore, in supplemental follow-up analyses, we found a statistically significant interaction between perceived social support and social network size on FE since age 60. It showed that the protective effects of perceived social support are greatest for those with the largest social networks. Follow-up analyses showed that larger non-family social networks are related to risk for FE, whereas size of the family network was unrelated to FE. In sum, older adults with large non-family social networks and low perceived social support were at highest risk for FE since age 60.
The results suggest that the role of social support in FE may be more complex than previously thought. Supportive relationships are certainly protective, but having larger non-family networks can simultaneously put an older adult at risk for FE and perhaps other forms of elder mistreatment. The more people older adults are exposed to, the greater the opportunity for supportive relationships, but at the same time, there is a higher risk that network members will perpetrate FE. The significant interaction suggests that structural and functional aspects of social support may combine synergistically to affect risk for FE. Knowing lots of people outside the family combined with low perceived support seems to be especially problematic. Our results appear to be consistent with Carstensen’s socioemotional selectivity theory (Carstensen, Isaacowitz, & Charles, 1999), which argues that older adults tend to prefer smaller social networks concentrated with people who are most likely to make them feel validated and loved. The precise nature of the interplay between the perceptual/functional and objective/structural aspects of social relationships on risk for FE will require further study.
Turning to household living arrangements, we found no significant relationships between living with a spouse, son, daughter, other family, non-relatives, or living alone and FE once all other covariates, including perceived social support and social network size, were statistically controlled. These findings are in contrast to the previous studies showing shared living arrangements as a risk factor (IOM & NRC, 2014; National Research Council, 2003), and also to the national prevalence studies that showed being married was related to lower risk for FE (Laumann et al., 2008; Podnieks, 1993). It appears that the size of the non-family social network and the perceived quality of social support available from network members are stronger correlates of FE than shared living arrangements.
The other consistent predictors of FE were race and risk for depression. African Americans and those who met the CESD cutoff for risk for depression (Shrout & Yager, 1989) were at higher risk for FE. These factors were the focus of a prior paper (Beach, Schulz, Castle, & Rosen, 2010) and are not discussed in detail here. We will only note that the large racial differences in FE suggest potential cultural or family factors not measured here and certainly deserve further study. The depression findings need to be explored further in the context of longitudinal studies to better understand causal ordering.
This study has various limitations that should be acknowledged. First, the sample was drawn from a single urban county in Pennsylvania that contains the City of Pittsburgh and is thus not national in scope. The risk profiles for national or rural elder mistreatment may differ from the local urban profiles reported in this article. Second, the response rate among eligible households (37.7%) was somewhat low and may have produced somewhat biased results. Third, our four-item assessment of FE is certainly not comprehensive, and the findings may be better characterized as indicating potential risk for more serious FE, which would need to be verified through further investigation. The use of retrospective recall (e.g., since turning 60 or in last 6 months) likely resulted in some measurement error due to memory or recall biases. The cross-sectional design of the survey limits the ability to make definitive causal statements about risk factors like perceived social support or depression. It is not clear whether having low perceived social support makes an older adult more vulnerable to FE, or whether being a victim of FE causes one to perceive having less social support. The reverse causality issue may also be relevant social network size, but it is less clear how becoming the victim of FE would cause one to expand the social network. Nevertheless, longitudinal panel designs are needed to more definitively answer questions about causality. Finally, because the study is correlational, social network size or social support may be related to third variables not addressed here that may be relevant for FE risk.
Conclusions and Implications
The major finding of the article was that higher levels of perceived social support were related to reduced risk of FE, whereas larger social networks were simultaneously related to increased risk of FE. Those with large non-family networks combined with low perceived social support were most at risk. Our results are generally consistent with previous work showing that FE is more likely than other forms of elder abuse to be perpetrated by non-relatives (Jackson & Hafemeister, 2014; Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, & New York City Department for the Aging, 2011). These findings have important theoretical and practical implications. They suggest that when it comes to the role of social relationships and risk for FE, “more may not always be better,” and that a “quality not quantity” maxim may apply. More work needs to be done to clarify whether specific types of social roles (e.g., those outside the immediate family) put older adults at increased risk for FE and other types of elder mistreatment. In addition, are there particular subsets of older adults for whom larger social networks are more or less protective? Future research on the relationship between social embeddedness and risk for elder abuse should include assessments of both perceptual/functional and objective/structural aspects of social support.
In terms of practice and policy implications, family members, caregivers, and health care/service providers should encourage older adults to develop and nurture high quality, close, supportive interpersonal ties. Encouragement to widen the social network by “making new friends” should be stressed less than making sure these new network members will truly be supportive of the older adult. For example, older adults’ use of social networking technologies and online dating sites may put them at increased risk of FE. Similarly, frequent visits to senior centers or participation in group activities with strangers may also increase risk. These risks for FE may be especially heightened in the context of living alone or other forms of social isolation. In the most frequently cited national prevalence study of elder abuse, Acierno and colleagues (2010) noted the central role played by low social support in risk for neglect and physical, sexual, and emotional abuse—but not financial mistreatment by family. They suggested a variety of ways to potentially enhance social support for older adults, including reconnection with community resources, improved housing designs for older adults that maximize communal interaction, funding for familial and community programs that bring together the elderly and their neighbors or family members, and affordable transportation. This study suggests that these policies may be a double-edged sword when attempting to reduce risk of FE. Policies aimed at enhancing network size and access to potentially “weak ties” should be balanced with a focus on enhancing supportive relationships with family and intimate friends.
Acknowledgments
This study was approved by the University of Pittsburgh Institutional Review Board (IRB #0606011).
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Preparation of this manuscript was supported by the National Institute on Aging (5R21AG028-15-01).
Biographies
Author Biographies
Scott R. Beach is associate director and director of the Survey Research Program at the University Center for Social and Urban Research at the University of Pittsburgh. He received his PhD in social psychology from the University of Pittsburgh in 1993. His research interests include survey methods, caregiver stress, elder abuse, and technology and aging.
Richard Schulz is distinguished service professor of psychiatry and director of the University Center for Social and Urban Research at the University of Pittsburgh. He earned his PhD in social psychology from Duke University in 1974. His research interests include adult development and aging, and technology-based approaches designed to enhance patient functioning and quality of life (QoL) of both patients and their relatives.
Rodlescia Sneed is a post-doctoral researcher at the University Center for Social and Urban Research at the University of Pittsburgh. She received her PhD in psychology from Carnegie Mellon University in 2014. Her research interests include the role of social factors in mental and physical health outcomes among older adults.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Acierno R, Hernandez M, Amstadter A, Resnick H, Steve K, Muzzy W, & Kilpatrick DG (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100, 292–297. doi: 10.2105/AJPH.2009.163089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L, & West S (1991). Multiple regression: Testing and interpreting interacttions. Newbury Park, CA: SAGE. [Google Scholar]
- Beach S, Schulz R, Castle N, & Rosen J (2010). Financial exploitation and psychological mistreatment among older adults: Differences between African Americans and non-African Americans in a population-based survey. The Gerontologist, 50, 744–757. doi: 10.1093/geront/gnq053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach S, Schulz R, Degenholtz H, Castle N, Rosen J, Fox A, & Morycz RK (2010). Using audio computer-assisted self-interviewing and interactive voice response to measure elder mistreatment in older adults: Feasibility and effects on prevalence estimates. Journal of Official Statistics, 26, 507–533. [PMC free article] [PubMed] [Google Scholar]
- Carstensen L, Isaacowitz D, & Charles S (1999). Taking time seriously: A theory of socioemotional selectivity. American Psychologist, 54, 165–181. doi: 10.1037/0003-066X.54.3.165 [DOI] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. American Psychologist, 59, 676–684. doi: 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle W, Skoner D, Rabin B, & Gwaltney J (1997). Social ties and susceptibility to the common cold. Journal of the American Medical Association, 277, 1940–1944. doi: 10.1001/jama.1997.03540480040036 [DOI] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, & Hoberman H (1985). Measuring the functional components of social support In Sarason IG & Sarason B (Eds.), Social support: Theory, research and applications (pp. 73–94). The Hague, The Netherlands: Martinus Nijhoff. [Google Scholar]
- Compton S, Flanagan P, & Gregg W (1997). Elder abuse in people with dementia in Northern Ireland: Prevalence and predictors in cases referred to a psychiatry old age service. International Journal of Geriatric Psychiatry, 12, 632–665. doi: 10.1002/(SICI)1099-1166(199706) [DOI] [PubMed] [Google Scholar]
- Herzog A, & Wallace R (1997). Measures of cognitive functioning in the AHEAD study. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 52(Special Issue), 37–48. doi: 10.1093/geronb/52B.Special_Issue.3 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine & National Research Council. (2014). Elder abuse and its prevention: Workshop summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Jackson S, & Hafemeister T (2014). How case characteristics differ across four types of elder maltreatment: Implications for tailoring interventions to increase victim safety. Journal of Applied Gerontology, 33, 982–997. doi: 10.1177/0733464812459370 [DOI] [PubMed] [Google Scholar]
- Lachs M, Berkman L, Fulmer T, & Horwitz R (1994). A prospective community-based pilot study of risk factors for the investigation of elder mistreatment. Journal of the American Geriatrics Society, 42, 169–173. doi: 10.1111/j.1532-5415.1994.tb04947.x [DOI] [PubMed] [Google Scholar]
- Lachs M, Williams C, O’Brien S, Hurst L, & Horwitz R (1997). Risk factors for reported elder abuse and neglect: A nine-year observational cohort study. The Gerontologist, 37, 469–474. doi: 10.1093/geront/37.4.469 [DOI] [PubMed] [Google Scholar]
- Laumann E, Leitsch S, & Waite L (2008). Elder mistreatment in the United States: Prevalence estimates from a nationally representative study. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 63(4), S248–S254. doi: 10.1093/geronb/63.4.S248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, & New York City Department for the Aging. (2011). Under the radar: New York State Elder Abuse Prevalence Study—Self-reported prevalence and documented case surveys. New York: New York State Office of Children and Family Services. [Google Scholar]
- Luo Y, & Waite LJ (2011). Mistreatment and psychological well-being among older adults: Exploring the role of psychosocial resources and deficits. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 66, 217–229. doi: 10.1093/geronb/gbq096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. (2003). Elder mistreatment: Abuse, neglect and exploitation in an aging America. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Paveza G, Cohen D, Eisdorfer C, Freels S, Semla T, Ashford W, … Levy P (1992). Severe family violence and Alzheimer’s disease: Prevalence and risk factors. The Gerontologist, 32, 493–497. doi: 10.1093/geront/32.4.493 [DOI] [PubMed] [Google Scholar]
- Pillemer K, & Finkelhor D (1988). The prevalence of elder abuse: A random sample survey. The Gerontologist, 28, 51–57. doi: 10.1093/geront/28.1.51 [DOI] [PubMed] [Google Scholar]
- Pillemer K, & Suitor JJ (1992). Violence and violent feelings: What causes them among family givers? Journal of Gerontology, 47(4), S165–S172. doi: 10.1093/geronj/47.4.S165 [DOI] [PubMed] [Google Scholar]
- Podnieks E (1993). National survey on abuse of the elderly in Canada. Journal of Elder Abuse & Neglect, 41, 5–58. doi: 10.1300/J084v04n01_02 [DOI] [Google Scholar]
- Quinn MJ, & Tomita SK (1986). Elder abuse and neglect: Causes, diagnosis, and intervention strategies. New York, NY: Springer. [Google Scholar]
- Radloff L (1977). The CES-D scale: A Self-Report Depression Scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Schafer MH, & Koltai J (2015). Does embeddedness protect? Personal network density and vulnerability to mistreatment among older adults. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 70, 597–606. doi: 10.1093/geronb/gbu071 [DOI] [PubMed] [Google Scholar]
- Seeman T (1996). Social ties and health: The benefits of social integration. Annals of Epidemiology, 6, 442–451. doi: 10.1016/S1047-2797(96)00095-6 [DOI] [PubMed] [Google Scholar]
- Shrout P, & Yager T (1989). Reliability and validity of screening scales: Effect of reducing scale length. Journal of Clinical Epidemiology, 42, 69–78. doi: 10.1016/0895-4356(89)90027-9 [DOI] [PubMed] [Google Scholar]
- Wills TA, & Ainette M (2012). Social networks and social support In Baum A, Revenson TA & Singer J (Eds.), Handbook of health psychology (2nd ed., pp. 465–492). New York, NY: Taylor & Francis. [Google Scholar]
- Wills TA, & Fegan M (2001). Social networks and social support In Baum A, Revenson TA & Singer J (Eds.), Handbook of health psychology (pp. 209–234). Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]


