Abstract
The new pandemic of SARS-CoV-2 has shown stark differences in number of affected patients between countries in the tropics and those with temperate environments. Though there have been many theories on reasons for these differences, we hypothesise that this could be due to differences in the fate of respiratory droplets in the two environments. A simple understanding of the mechanics of droplet size, dispersion and displacement could help infection control and public health measures to minimize spread and mitigate the risk of people getting infected especially in hotspots like hospital environments or other closed spaces. This paper discusses the possibility of differences in number of infections and spread between different countries based on the spread of droplets.
Keywords: SARS-CoV-2, COVID-19, Respiratory droplets, Transmission, Pandemic
Introduction
The situation with respect of COVID-19 globally is very grim with 3,939,119 cases and 274,917 deaths as on May 9th [1]. Interestingly, resource rich countries like US, Germany, UK, Italy, Spain seem to have been much more affected than many of the tropical countries in South and South East Asia and Africa. For example, Vietnam, which shares a long border with China has only 288 cases and no deaths though 2 cases were detected as early as 23rd January. Laos, sharing border with China had 19 cases with no deaths, Myanmar, sharing border with China had 177 cases with 6 deaths. Thailand had cases detected in January, but in April, the case count is only 3,004 with 56 deaths. In contrast, in US, cases started appearing only early March, but in a span of a month, the numbers have increased dramatically to 1,322,154 and 78,616 deaths. In Italy, the cases started showing up during the last week of February, but escalated to 217,185 with 30,201 deaths. In Spain, cases started appearing early March, but soon increased to 260,117with 26,299 deaths, while in Germany, cases began appearing late February, but increased to 170,588 with 7,510 deaths. The explosive increase in cases in resource rich countries with well-established public health system compared to a very slow increase in countries in South East Asia, which are resource limited and having weak public health system is perplexing. Though inadequate testing contributes to lower numbers in some countries, the difference is indeed stark and calls for other explanations based on transmission of this virus.
Respiratory droplet size and settlement influenced by temperature and relative humidity
The predominant mode of virus spread is said to be through droplets generated by infected individuals during coughing, talking or sneezing and contact transmission [2]. The droplets may range in size from sub-micrometers to hundred of micrometers. From “Stoke’s Drag force equation”, the terminal settling velocity of a particle of known diameter and density can be calculated. The settling velocity of the particle would be directly proportional to the density of the particle and to the square of the particle diameter. Owing to their size, larger particles settle down at a much faster speed than smaller particles. For instance, the settling velocity of a 10 µm water droplet will be approximately 88 times greater than a 1 µm water droplet. Thus smaller particles will stay airborne for a longer time, while larger particles will settle down on surfaces more quickly.
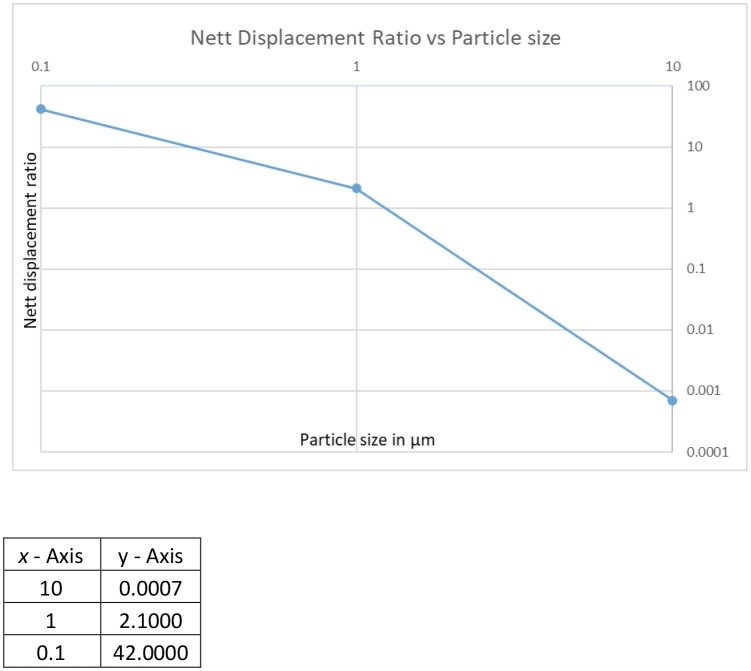
According to Law of Brownian motion, which is applicable to smaller particles, the diffusive forces would transport the particles in random directions. The Diffusion co-efficient of a particle as given by “Stokes-Einstein Equation” is inversely proportional to the diameter of the particle. So, smaller the particle, higher the diffusivity. Higher diffusivity helps smaller particles to travel through the room at a faster speed than larger particles. For instance, a 1 µm particle will have a net diffusion displacement that is 3 times more than that for a 10 µm particle (Fig. 1 ). Thus a smaller particle will spread throughout the room at a much faster rate than a large particle.
Fig. 1.
Settling time for 1 m height vs particle size.
The relative humidity of the environment influences the density of the particle as well as the size of the particle (Fig. 2 ). Upon release, the droplets may be subject to partial or total evaporation, depending on environmental conditions and would reduce in size. The environmental Relative Humidity (RH) will influence the extent of evaporation and final equilibrium size of the droplet. Thus lower RH reduces the size of the particle as the particle desiccates. Furthermore, relative humidity could affect the particle density too, as the particle desiccates. The combined effect of change in size of the droplet as well as the density amplifies the influence that environmental relative humidity would have on the particle settling velocity. Marr et al. [3] studied the effect of RH on droplet equilibrium using droplets containing 9 mg/ml NaCl, 3 or 76 mg/ml protein and 0.5 mg/L surfactant. They noted that a droplet of 10 μm shrinks to 2.8 μm at 90%RH and to 1.9 μm at less than 64%RH. The droplet size would greatly affect settling times, with 10 μm droplet remaining suspended for only 8 min at 100% RH while the 1.9 μm droplet at 64% RH remaining suspended for more than 3 h.
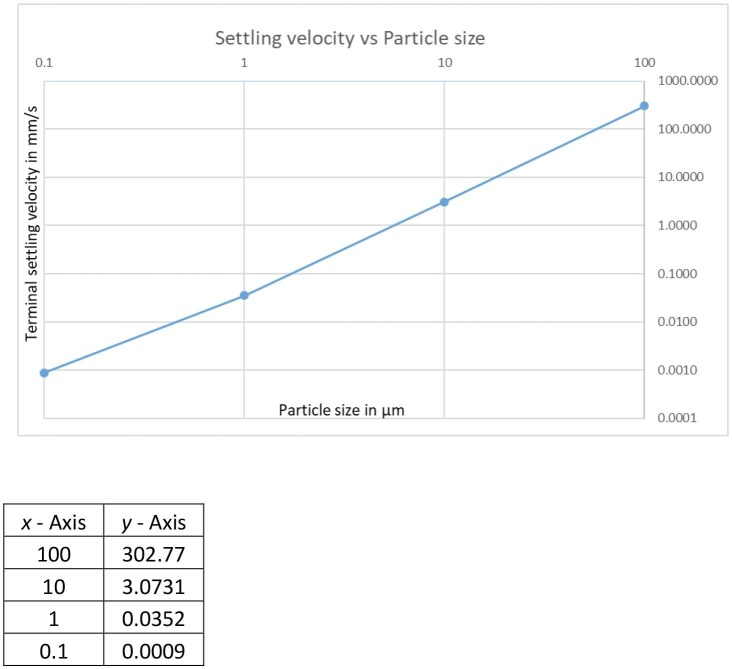
Fig. 2.
Showing settling velocity vs particle size.
All the above apply to the dynamics of particles in still air, with no air currents. However, in real life scenario, air currents and turbulences are unavoidable. These would further affect the settling patterns of particles. Therefore a significant portion of the particles are likely to be airborne indefinitely, drifting around freely. The expelled aerosol by a person on account of exhaling, talking, coughing, sneezing, etc would have a poly dispersed particle size distribution. The mean, median, mode and standard deviation of the distribution would vary based on expulsion characteristics. A significant portion of this cocktail of particles expelled by a person could hence stay airborne, influenced by environmental conditions and perhaps even get transported out of the source room, when provided with suitable conditions.
Respiratory droplets in tropical and temperate environments
Our hypothesis suggests that mechanistically, in tropical conditions of high temperature and high humidity, droplets settle quickly, while in temperate conditions of low temperature and low humidity, droplets tend to remain suspended in air. In the case of respiratory droplets, these would dramatically affect airborne transmission of viruses in the droplets. It is possible that droplets discharged from infected individuals in places like New York City could shrink in size quickly and remain airborne for considerable period of time. A droplet size of 1 μm could be airborne for 8 hrs. The humidity in New York City which is experiencing a serious COVID situation is around 64%, and in Berlin, the humidity is around 60%. On the other hand, in Hanoi, Vietnam, the humidity is above 80%. Under conditions of temperature and humidity in cities like Hanoi and Hochi Minn City in Vietnam, the droplets would settle quickly. This might explain higher transmission rates observed in temperate environments compared to tropical ones. The same argument holds good for air conditioned spaces, where the temperatures and relative humidity levels could be low. This may influence the measures needed to prevent infections. Hand hygiene and social distancing could be the most important step in tropical settings, since transmission could be predominantly through droplets settling on various surfaces, while, use of masks, hand hygiene and social distancing would be important in temperate places, since virus could remain airborne for considerably longer period of time. For air conditioned environments, suitable modifications and adjustments would be required to the air conditioning system to control the spread of infections.
Implications for transmission of SARS-CoV-2
In addition to differences in mode of dispersion, there could be differences in infectivity of virus due to survival under conditions of temperature and sensitivity. Chan et al [4] studied survival of SARS Coronavirus on various surfaces at different temperature and humidity conditions. Virus viability was retained up to 5 days on plastic surface at temperature of 22–25 °C and humidity of 40–50% with only one log reduction in titre. Temperature range of 28–33 °C and humidity of greater than 95% did not make much difference, but temperature of 38 °C at 80–90% RH led to up to 2 log reduction in titres in 24 h. Studies with porcine coronavirus (Transmissible Gastroenteritis Virus, TGEV) showed that they remain viable longer at low Relative Humidity (RH) than at high humidity [5]. TGEV is also an enveloped virus like SARS-CoV-2. The persistence of influenza virus in the environment has been studied by a number of investigators. Using systematic review methodology, Irwin et al. [6] surmised that increasing temperature (2–12 °C vs ≥27 °C) resulted in shorter virus half life. Published studies indicate that virus half life was 16.5 times longer at temperatures between 7 and 12 °C as compared to ≥27 °C. Harper [7] studied influenza survival at three temperatures (7–8 °C, 20.5–24 °C and 32 °C) and five RH ranges (20–25%, 34–36%, 49–51%, 64–65% and 81.82%) and noted that virus survival was highest at lowest temperature and lowest RH studied. Using enveloped virus Phi6 in droplets as surrogate for influenza and coronaviruses, Prussin II et al. [8] noted significant decrease in infectivity at RH range 60–85%. Infectivity decreased two orders of magnitude between 19 and 25 °C at humidity level of 75%. It can be expected that SARS-CoV-2 virus behaves on similar lines as SARS-CoV-1 and influenza virus. Infectivity could be reduced under environmental conditions prevailing in cities like Hanoi in Vietnam compared with New York City in US. Therefore, reduced infectivity and shorter airborne transmission could explain lower number of cases observed in South East Asia.
Funding
The research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.JHU SSE (John Hopkins University, Center for Systems Science and Engineering), 2020 COVID-19 dashboard https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. [DOI] [PMC free article] [PubMed]
- 2.Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., Duan G. Virology, epidemiology, pathogenesis and control of COVID-19. Viruses. 2020;12:372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marr L.C., Tang T.W., Muellekom J.V., Lakdawala S.S. Mechanistic insights into the effect of humidity on airborne influenza survival, transmission and incidence. J Roy Soc Interface. 2019;16 doi: 10.1098/rsif.2018.0298. 20180298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan K.H., Malik Peiris J.S., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. Effect of temperature and relative humidity on the viability of SARS coronavirus. Adv Virol. 2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim S.W., Ramakrishnan M.A., Raynor P.C., Goyal S.M. Effects of humidity and other factors on the generation and sampling of coronavirus aerosol. Aerobiologia. 2007;23:239–248. doi: 10.1007/s10453-007-9068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irwin C.K., Yoon K.J., Wang C., Hoff S.J., Zimmerman J.J., Denagamage T. Using the systematic review methodology to evaluate factors that influence the persistence of influenza virus in environmental matrices. Appl Environ Microbiol. 2011;77:1049–1066. doi: 10.1128/AEM.02733-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper G.J. Airborne microorganisms: survival tests with four viruses. J Hyg Cambridge. 1961;59:479–486. doi: 10.1017/s0022172400039176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PrussinII A.J., Schwake D.O., Lin K., Gallaghar D.L., Buttling L., Marr L.C. Survival of the enveloped virus Phi6 in droplets as a function of relative humidity, absolute humidity and temperature. Appl Environ Microbiol. 2018;84:e00551–18. doi: 10.1128/AEM.00551-18. [DOI] [PMC free article] [PubMed] [Google Scholar]