Abstract
As of April 17th, 2020, more than 2,190,010 COVID-19 cases with 147,010 deaths have been recorded worldwide. It has been suggested that a high mortality rate occurs in patients with severe disease and is associated with advanced age and underlying comorbidities, such as malignancies. To the best of our knowledge, no study has been conducted to evaluate chest CT features in patients with malignancy and concomitant COVID-19 infection. In fact, the imaging findings can be challenging and have not yet been fully understood in this setting. In this manuscript, we go over imaging findings in chest CT of patients with COVID-19 and known cancer. With the ongoing COVID-19 pandemic and exponentially increasing incidence throughout the world, in at-risk and vulnerable populations such as patients with known malignancies, infection with SARS-CoV-2 should be included in the differential considerations even with atypical image pictures. Detection of superimposed infection in patients with cancers who present with pulmonary infiltrations warrant correlation with clinical picture, contact history, and RT-PCR confirmatory testing.
Keywords: COVID-19, SARS-CoV-2, Malignancy, Pneumonia, Leukemia, Lymphoma, Cancer, Computed tomography, Radiology
Highlights
-
•
Patients with underlying malignancies might be at a higher risk of COVID-19 infection and its complications.
-
•
Pulmonary infiltrations in patients with malignancies can be caused by many infectious which pose a clinical challenge
-
•
Atypical, rare, or subtle CT patterns, may be among the presenting radiological features of COVID-19 infection in patients with pre-existing cancers.
1. Introduction
In late December 2019, an outbreak of novel coronavirus disease (known as COVID-19) was first reported in the city of Wuhan (China). With new cases emerging rapidly across the other regions of China and worldwide, COVID-19 has been stated as a global pandemic by the World Health Organization (WHO). As of April 17th, 2020, more than 2,190,010 COVID-19 cases with 147,010 deaths have been recorded worldwide [1].
Although most patients with COVID-19 initially present with fever and mild to moderate respiratory symptoms [2], various degrees of pulmonary manifestations develop later on chest computed tomography (CT) studies. It has been suggested that a high mortality rate occurs in patients with severe disease and is associated with advanced age and underlying comorbidities, such as malignancies [[3], [4], [5]]. The study by Liang et al. [6] on 1590 patients with COVID-19 in China has asserted that pre-existing conditions (including malignant neoplastic disease) correlate positively with poorer clinical outcomes, similar to previous findings in other severe acute respiratory diseases, such as SARS and MERS [7]. Eighteen patients with a history of cancer were found among 1590 patients with confirmed coronavirus disease 2019 (COVID-19), which was higher than the general population, probably indicating a higher risk of viral infection in this population. On the other hand, patients with concomitant COVID-19 and cancer were noted to have a higher risk of severe events.
Despite some uncertainties due to lack of sufficient data in this field [8,9], patients with cancer should be considered susceptible to infection due to their immunocompromised status caused by the malignancy and chemoradiotherapy. Therefore, during the present widespread community transmission of COVID-19 pneumonia, some practical steps regarding diagnosis and management of the infection in patients with pre-existing malignancies should be taken.
Due to the limited availability of viral testing kits and growing concern for test sensitivity from earlier reports [10], chest CT has been considered to be a fundamental element of the evaluation of patients with suspected or known COVID-19 infection. Indeed, CT has been found to be useful as a fast and sensitive diagnostic tool for COVID-19 infection to improve patients' management. The spectrum of radiological findings seen in COVID-19 has been widely discussed in literature [[11], [12], [13], [14]]; Multifocal bilateral ground-glass opacities (GGOs) with a peripheral distribution and later superimposition of consolidation and possible vascular ectasia have been reported as the main imaging features. However, most of these publications have been merely focused on acute respiratory COVID-19 infection occurring in general population, mainly previous-healthy patients without underlying diseases. Only a few studies have described CT patterns of COVID-19 pneumonia in individuals with the pre-existing pulmonary disease [15,16]. To the best of our knowledge, no study has been conducted to evaluate chest CT features in patients with malignancy and concomitant COVID-19 infection and the specific imaging findings have not yet been fully understood in this setting. In this manuscript, we go over imaging findings in chest CT of patients with COVID-19 and known cancer.
2. Lung cancer
The spread of COVID-19 pneumonia has affected the routine diagnosis and management of most chronic diseases, including malignancies [[17], [18], [19], [20], [21]]. As mentioned before, patients with pre-existing cancer are not only more susceptible to the disease, but also pose a poorer clinical prognosis [6]. Specifically, patients with lung cancer require particular attention due to the higher mortality rate [18]. However, accurate diagnosis and optimal treatment of COVID-19 in patients with lung cancer can present a real challenge to clinicians. Many symptoms of pneumonia may resemble the symptoms or complications of lung malignancies. Even the radiologic findings of lung cancer, such as parenchymal consolidation, spiculation, and microlobulations are not specific, and infections can present similar features [22]. To carefully identify COVID-19 infection in patients with lung cancer who develop respiratory symptoms, epidemiologic data, and detailed clinical history combined with chest CT seem to be of great value.
Imaging findings of COVID-19 infection in patients with lung cancer consist of multiple patchy GGOs and consolidations [18], which can be hardly separable from the primary lung tumor (Fig. 1 ). However, although peripheral GGOs and consolidations are usually highly suggestive of superimposed COVID-19 pneumonia, these findings can be hardly distinguishable from an underlying lung malignancy or other opportunistic infections in patients with known lung cancer and warrant clinical, epidemic and laboratory correlation with PCR testing.
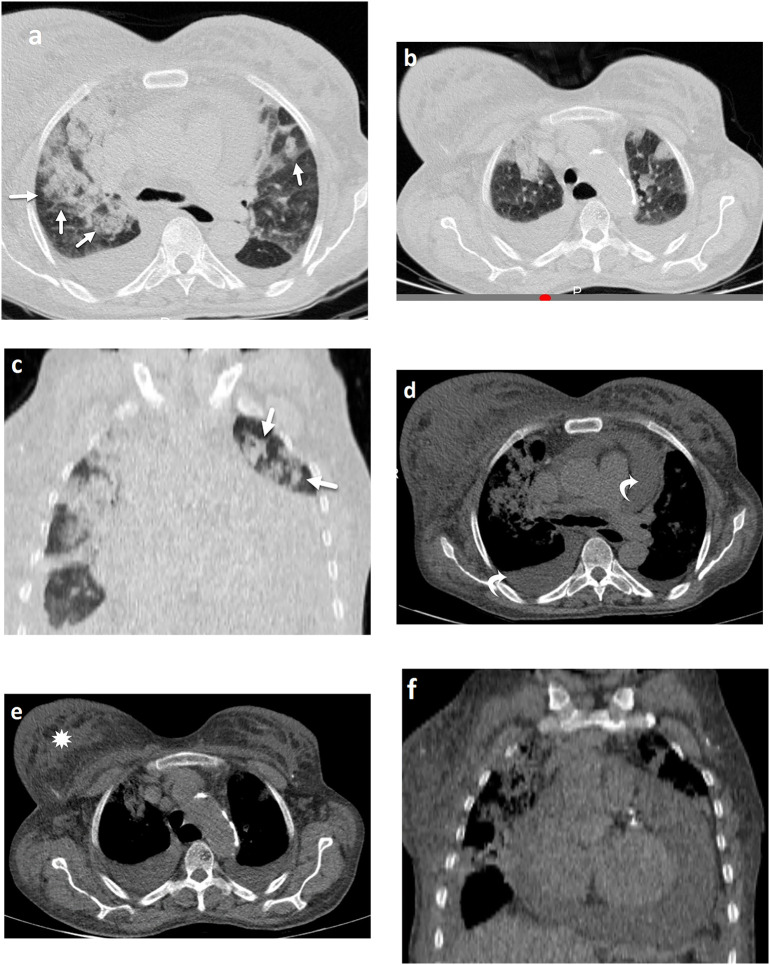
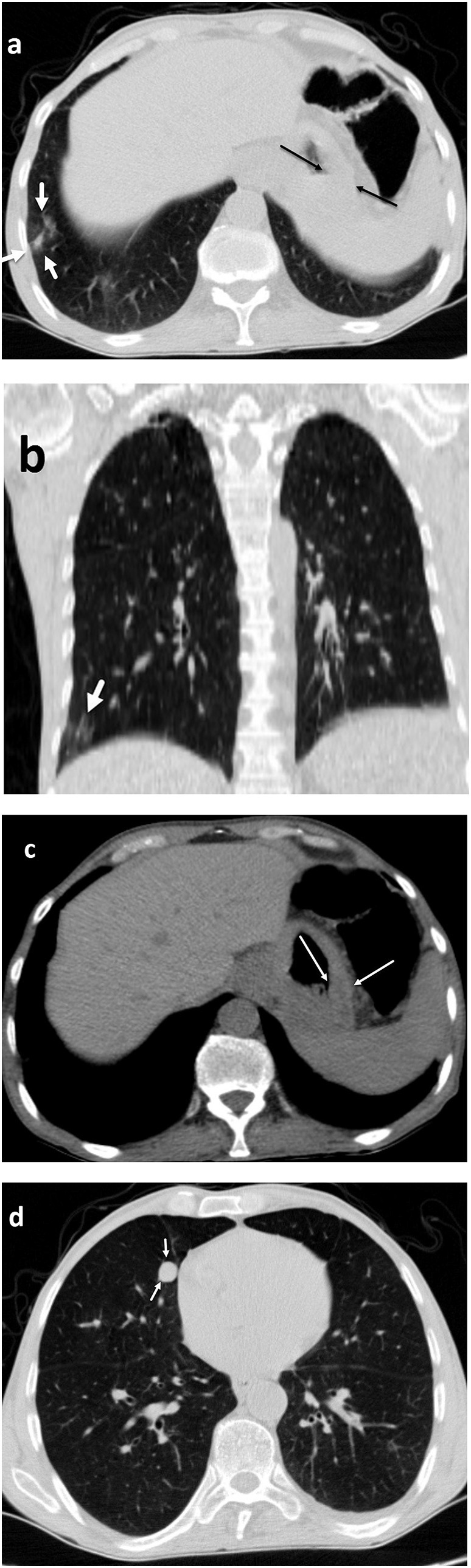
Fig. 1.
COVID-19 in lung cancer. A fifty-year-old patient with history of lung cancer presented with new-onset fever. Axial images of chest CT reveal lobulated right para-hilar mass (a; black arrows), resulting in post-obstructive collapse and consolidation, consistent with the patient's known lung cancer. Associated ground-glass opacity involving the right upper lung (a, b; white arrows) is also noted, concerning for superimposed atypical infection, such as COVID-19, a diagnosis which was subsequently confirmed with RT-PCR. The narrowing of right main bronchus (c; curved arrow) is also observed. Furthermore, soft tissue window images of the chest reveal prominent right para-tracheal and internal mammary lymphadenopathy (d;☆), which can be metastatic in etiology or reactive to concomitant infectious/inflammatory process.
3. Hematologic malignancies
3.1. Acute myeloid leukemia (AML)
As per the early published reports from China, patients with cancer infected with SARS-CoV-2 are at a higher risk of complications, ICU admission, mechanical ventilation, and death (6). Active hematologic cancers such as non-Hodgkin lymphoma, chronic lymphocytic leukemia, acute myeloid leukemia, acute lymphoblastic leukemia, and multiple myeloma [23,24] are believed to have a significant risk for developing COVID-19 infection, due to their profound immune deficits. Patients on chemotherapy or with a history of marrow transplant constitute the most vulnerable population [[25], [26], [27], [28], [29]].
Due to this high vulnerability, all patients with neutropenic fever might be considered undergoing CT-scan to determine to exclude parenchymal abnormalities. Generally, CT findings of COVID-19 pneumonia in patients with underlying hematologic malignancies include interstitial or alveolar infiltrations, resulting in reticulations or ground-glass opacities (Fig. 2, Fig. 3, Fig. 4 ). However, in leukemic patients, non-infectious diseases (such as hemorrhage and adult acute respiratory distress syndrome [ARDS] may also present with similar features [29]. Hence, a definitive diagnosis cannot always be made based on imaging features alone.
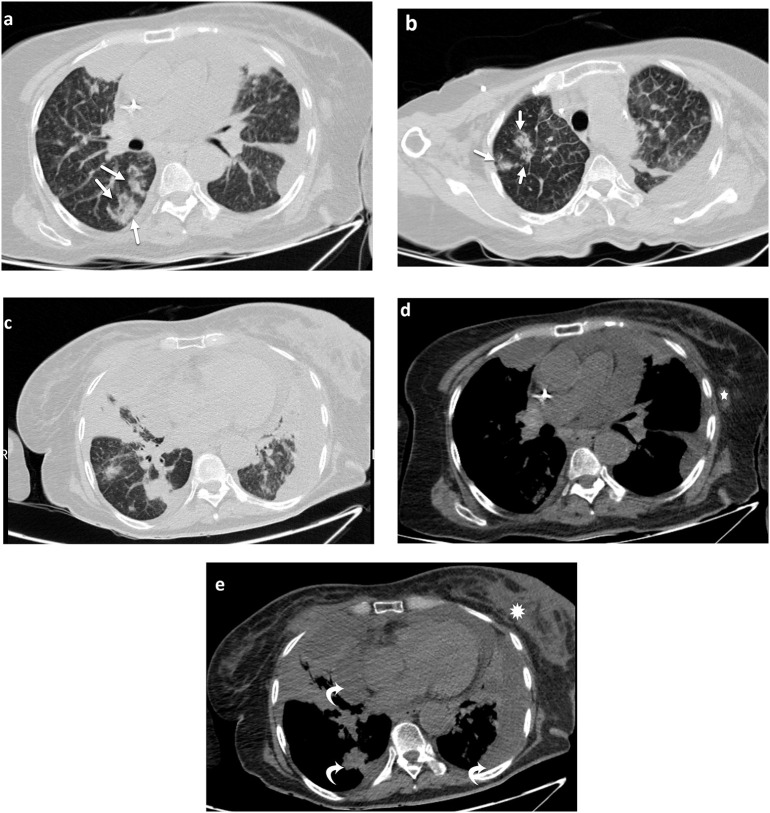
Fig. 2.
Subtle findings of COVID-19 infection in AML. A twenty-five-year-old man with a history of AML for over a year, presented with fever. Axial CT images (a) and (b) demonstrate small faint nodular ground-glass opacity in posterolateral aspect of right upper lobe. Although this finding is not typical for COVID-19, due to the underlying immunodeficiency from chemotherapy, and extensive local spread of the disease in the community (Iran), RT-PCR testing was performed, which was positive for COVID-19.
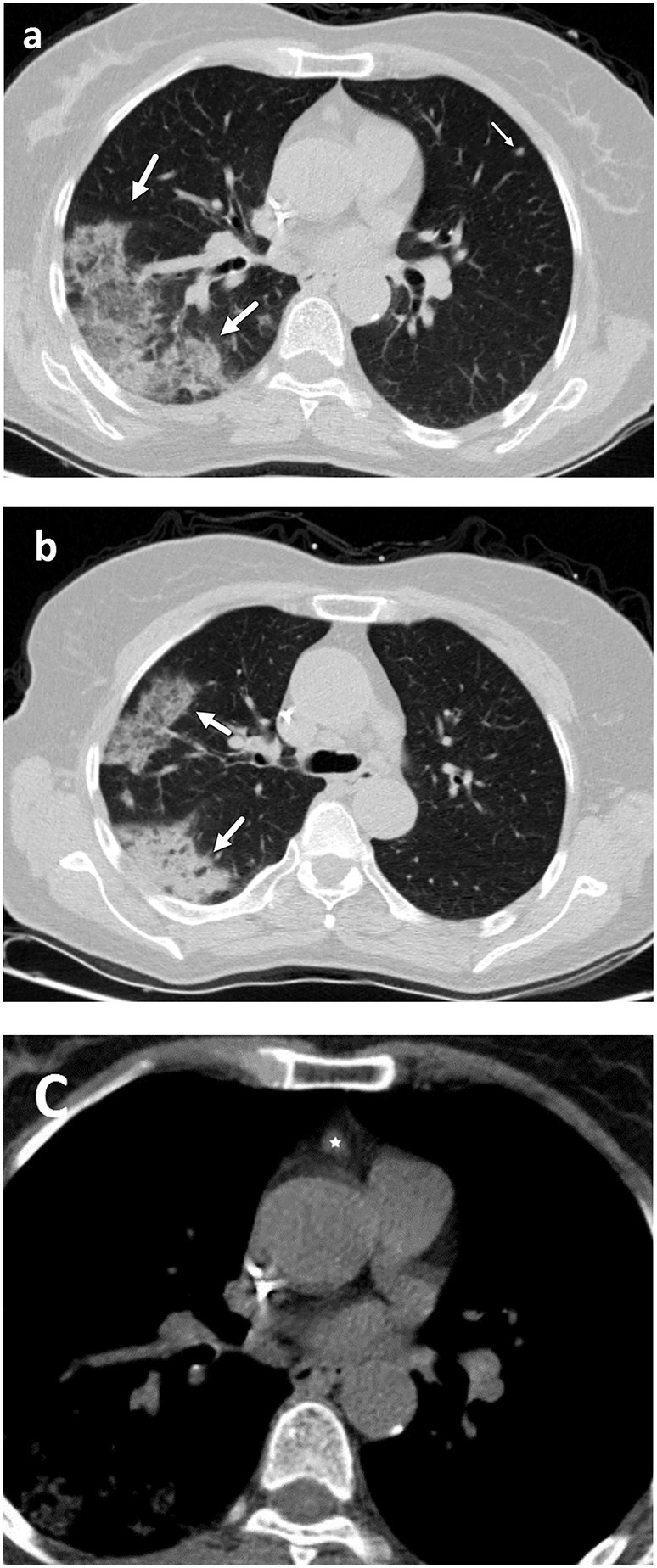
Fig. 3.
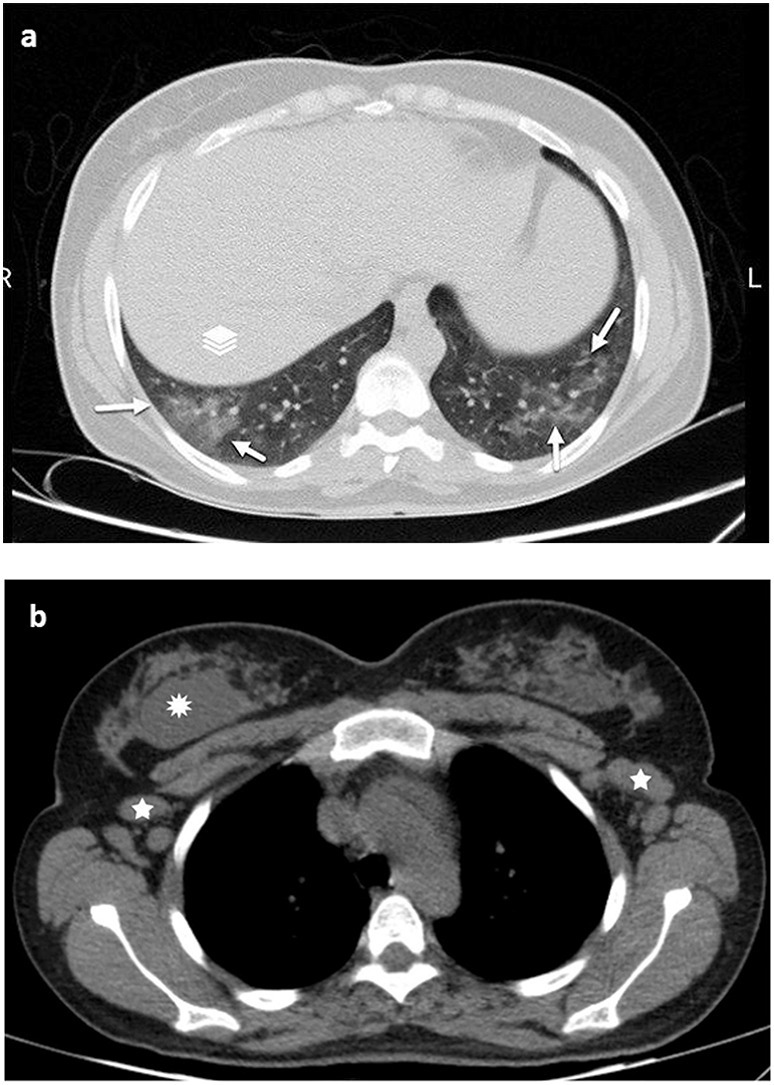
COVID-19 infection in a known case of AML. A thirty-three-year-old woman, a new case of AML since three months ago, admitted with cough and fever. (a) Axial CT image reveal ground-glass opacities (thick arrows) in basal segments of both lower lungs, in favor of COVID-19 infection. Also, large bilateral axillary lymphadenopathies (white stars) are observed (b), likely secondary to the underlying hematologic disease or less likely reactive to the superimposed infectious process. Incidental note is made of a soft tissue mass within posterior depth of the right breast (*), concerning for primary breast neoplasm versus leukemic infiltration.
Fig. 4.
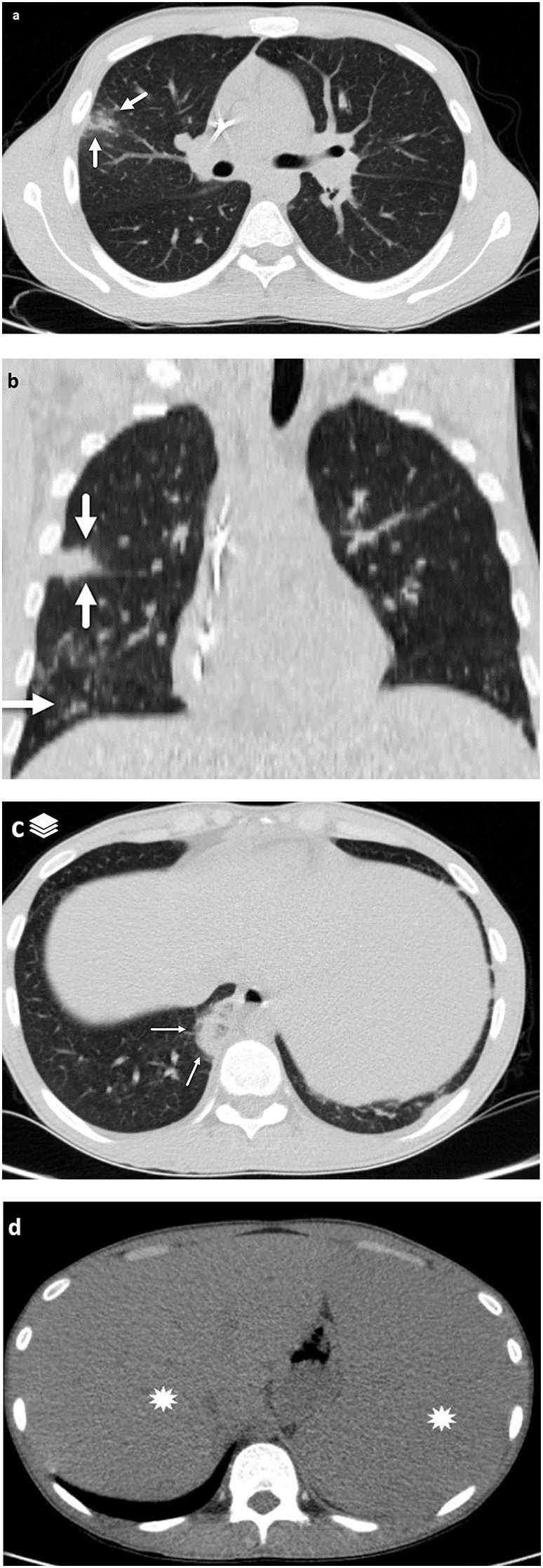
COVID-19 in AML. A twenty-two-year-old man with a history of AML for nine months was referred with fever and cough. Axial and coronal CT images demonstrate GGO (a) and consolidation (thick arrows) in right upper (b) and para-mediastinal right lower lobe (c), suspicious for SARS-CoV-2 pneumonia. Subsequent PCR testing confirmed COVID-19. Hepatosplenomegaly (*) is also identified in the soft tissue window images of the upper abdomen.
On the other hand, it cannot be overemphasized that COVID-19 in AML patients may present with atypical or subtle findings, which presents an important challenge in their diagnosis and timely treatment. In this setting, CT-scan may demonstrate only minimal small ground-glass lesions in the lungs, disproportionate to the patient's symptomatology (Fig. 2). This suggests that during the pandemic, in patients with hematologic malignancies, COVID-19 should be considered among the differential considerations even with mild or atypical clinical presentations and subtle and atypical radiologic findings. In this specific patient population, the threshold for RT-PCR testing should be significantly lower, particularly for those who live in the endemic regions. Also, atypical radiologic presentations cannot necessarily exclude COVID-19 infection in the presence of an underlying hematologic disease.
3.2. Lymphoma
Similar to leukemia, pulmonary infiltrative lesions in CT-scan of patients with lymphoma can be representative of various pathologies [30]. Acute respiratory SARS-CoV-2 infection may sometimes complicate the underlying pulmonary lymphomatous infiltration (Fig. 5 ). In this setting, GGOs and patchy consolidation patterns could be suggestive of superimposed COVID-19, which needs confirmation by RT-PCR. However, differentiation between the various causes of radiologic pulmonary lesions in these patients is not always straightforward and may lead to diagnostic difficulties.
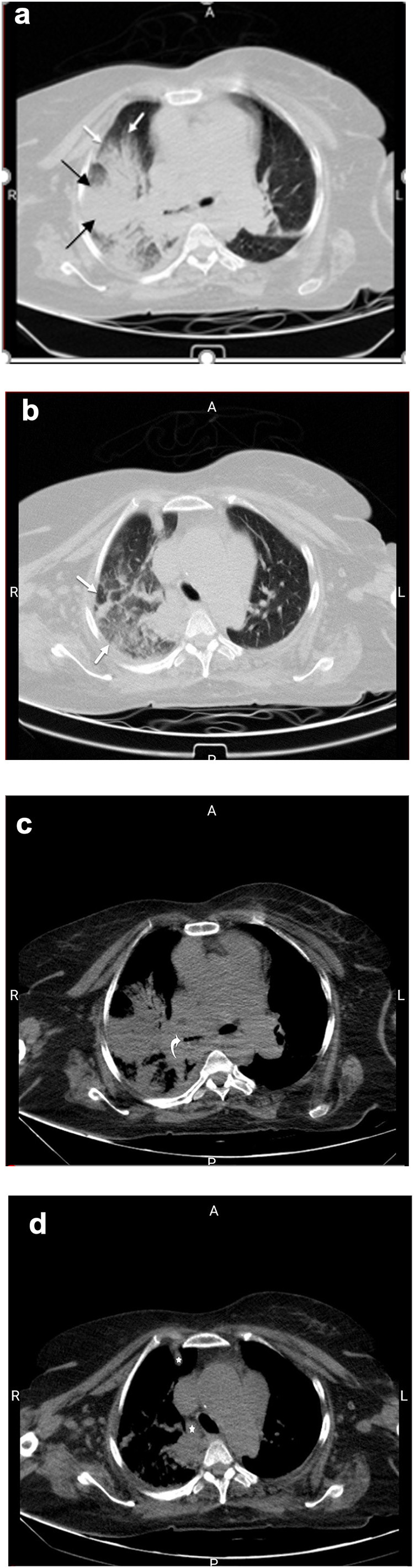
Fig. 5.
COVID-19 infection in lymphoma. A forty-five-year-old female with non-Hodgkin's lymphoma for few years developed COVID-19. Axial CT images reveal multiple lobulated-border masses involving bilateral lungs (a and b), in favor of lymphomatous infiltration (short thick arrows). Superimposed GGOs and consolidations are identified involving the left lung, concerning for acute respiratory SARS-CoV-2 infection (long thin arrows).
3.3. Breast cancer
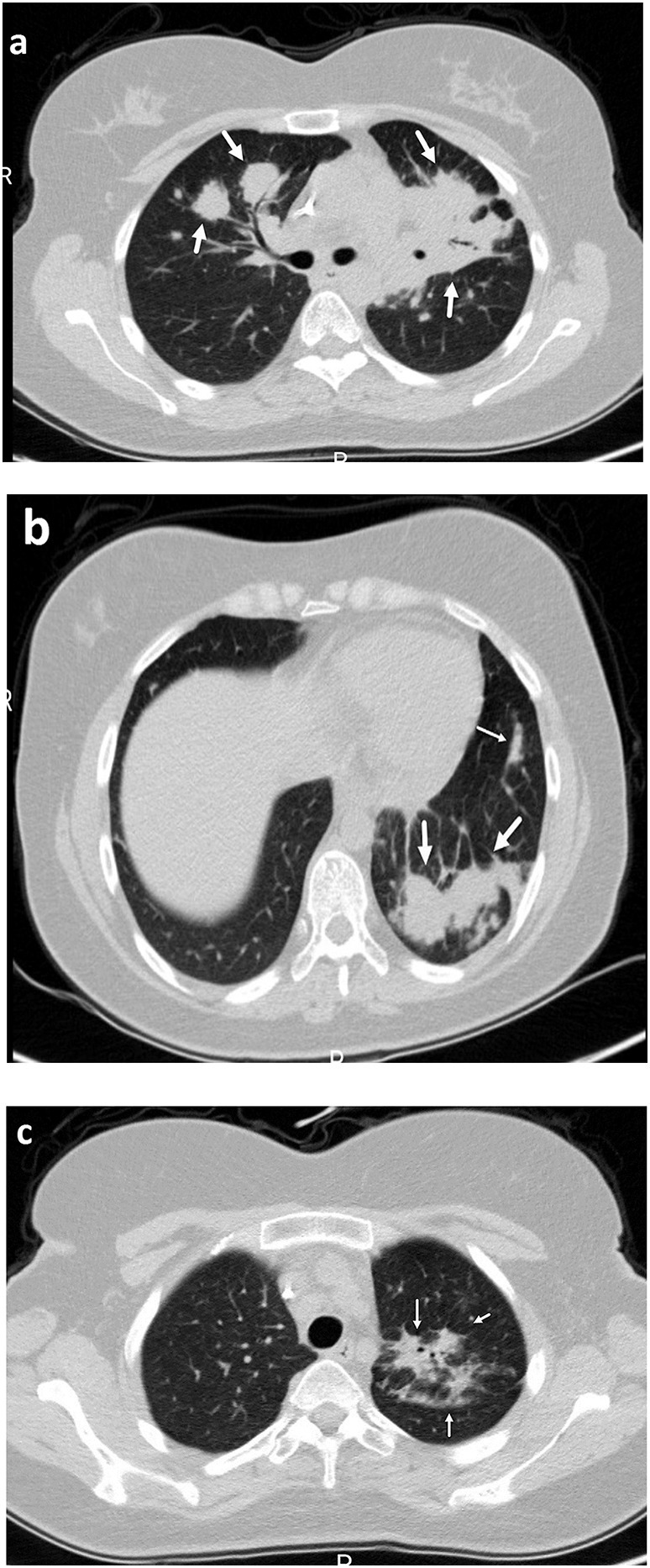
Like other malignancies, breast cancer patients are in lower immune status and prone to adverse reactions, such as leukopenia and other treatment-related complications during the course of chemotherapy. Therefore, they are considered to be at high risk for pneumonias and at a higher risk of developing severe events [31]. COVID-19 in patients with breast cancer demonstrates multifocal pulmonary GGOs (Fig. 6 ), which can be hard to be differentiated from the underlying pulmonary metastases (Fig. 7 ).
Fig. 6.
COVID-19 infection in breast cancer. A sixty-one-year-old female with a history of right breast cancer presented with progressive dyspnea and new onset fever. Axial and coronal CT images (a), (b), and (c) reveal diffuse GGOs and consolidations (thick arrows) in both lungs, highly suggestive of COVID-19 infection, that was confirmed with subsequent RT-PCR. Associated pleural effusion (a-d) is an atypical feature for COVID-19 and can be due to underlying metastatic disease. Right sided breast mass (*) with asymmetric right breast enlargement and cutaneous thickening and malignant pericardial effusion (curved arrow) are also noted.
Fig. 7.
COVID-19 infection in breast cancer. A fifty-year-old female with history of metastatic left breast cancer was referred for CT chest due to new-onset fever. Axial CT (a), (b), and (c) demonstrate scattered bilateral GGOs and consolidations (thick arrows) concerning for superimposed COVID-19 infection on pulmonary metastases. Also, there is pleural fluid in the left major fissure and interlobular septal thickening (a, b). Moreover, left axillary lymphadenopathy (d; ☆) the primary breast cancer (e; *), and parenchymal, pleural and pericardial metastases and effusion (e; curved arrows) are identified.
3.4. Gastrointestinal malignancies
It has not yet been fully explored as to whether patients with gastrointestinal cancers are more prone to SARS-CoV-2 infection compared to the rest of the population [32]. In a recent analysis from China [6], eighteen of 1590 COVID-19 cases (1%) had a history of cancer, among which, three patients had a history of colorectal cancer. It was found that patients with COVID-19 and cancer have a higher risk of severe complications. During the COVID-19 epidemic, patients with gastrointestinal tumors who develop respiratory symptoms should be closely monitored with clinical and epidemiologic data, chest CT-scan and, RT-PCR panel. Pulmonary infiltrative lesions, including GGOs, even in atypical distribution, should be considered highly suspicious for COVID-19 in this setting and warrant further evaluation by RT-PCR (Fig. 8, Fig. 9, Fig. 10 ). It should also be pointed out that a thorough investigation of chest CT-scan is mandatory in all cancer patients with suspect or known COVID-19 infection, in order to avoid missing significant accompanying pathologies, such as newly-appeared metastases (Fig. 9, Fig. 10).
Fig. 8.
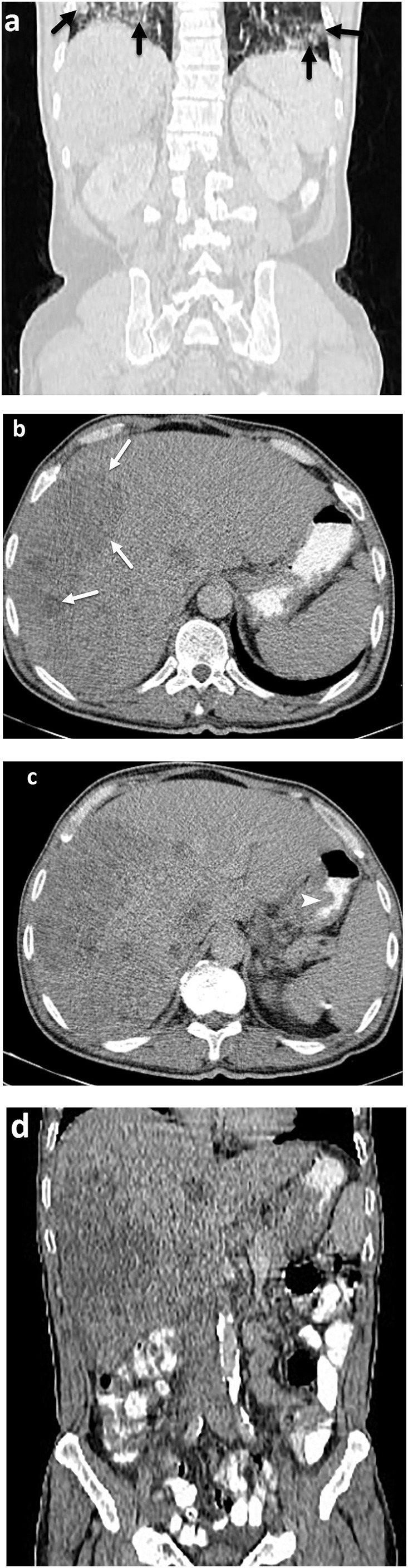
COVID-19 infection in metastatic gastric cancer. A sixty-year-old male with a history of metastatic gastric cancer presented with abdominal pain and fever. On coronal CT image of the abdomen and pelvis (a) incidental note is made of ground-glass opacity involving bilateral lung bases (black arrows), concerning for COVID-19 infection. Liver metastases (b; white arrows) and irregular wall thickening of stomach due to the known primary carcinoma (c; arrowhead) are also noted.
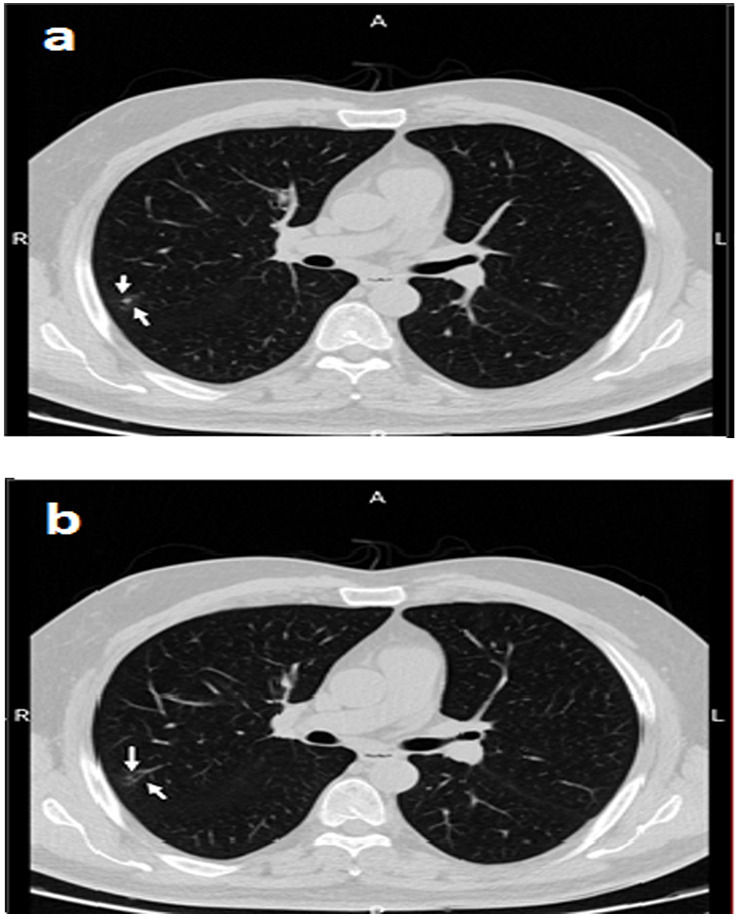
Fig. 9.
COVID-19 infection in metastatic gastric cancer. A fifty-two-year-old male was referred for CT chest because of recent respiratory symptoms (dyspnea and dry cough). Axial and coronal CT images (a) and (b) demonstrate peripheral GGO in the right lower lobe (short thick arrows), suggestive of COVID 19 infection, which was confirmed on PCR testing. Additional findings related to the underlying cancer, such as gastric wall thickening (c; thin arrows) and a solitary metastatic right paracardiac pulmonary nodule (d; thin arrows) are also identified.
Fig. 10.
COVID-19 infection in colon cancer. A seventy-year-old female, who was diagnosed with colon cancer more than ten months ago and was treated with surgery presented with new dyspnea and dry cough (without fever) two weeks after her last chemotherapy. Chest CT revealed peripheral consolidation and reverse halo sign involving the right lung (a, b; thick arrows) in favor of COVID-19. Also, small subcentimeter soft tissue density non-calcified pulmonary nodule is seen in left upper lobe (a; thin arrow), concerning for metastasis. Subcentimeter prevascular mediastinal lymph node (c; star) is also noted, which is non-specific and can be neoplastic or reactive in etiology.
4. Summary
Although there is insufficient information on how new COVID-19 infection affects cancer patients, the available evidence suggests that this population is at a higher risk of complications. However, the detection of COVID-19 in the setting of pulmonary infiltration in cancer patients can cause a real challenge. Pulmonary infiltration in patients with malignancies can be caused by many infectious and non-infectious etiologies [33]. However, the ongoing COVID-19 pandemic and exponentially increasing incidence throughout the world, in at-risk and vulnerable populations such as patients with known malignancies, infection with SARS-CoV-2 should be included in the differential considerations. Furthermore, given lower immune function, a substantial number of these patients may represent atypical clinical symptoms or imaging features, such as few or single pulmonary consolidations or GGOs, which makes the early diagnosis more challenging. Radiologists must be aware that atypical, rare, or subtle CT patterns may be among the presenting radiological features of COVID-19 infection in patients with pre-existing cancer, especially those with hematologic malignancies, history of multiple chemotherapies, and leukopenia. Therefore, raised clinical index of suspicion and low threshold for diagnostic testing, such as RT-PCR and chest CT is needed to allow earlier detection and treatment of this potentially life-threatening disease. Constant vigilance can help early diagnosis, not only for timely diagnosis, but also to ensure appropriate post-exposure precautions are implemented.
Financial disclosure
The author has no financial relationships relevant to this article to disclose.
Funding source
None.
Declaration of competing interest
The author has no conflicts of interest relevant to this article to disclose.
References
- 1.https://www.worldometers.info/coronavirus/
- 2.Huang C., Wang Y., Li X., Ren L. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [February] [DOI] [PubMed] [Google Scholar]
- 4.Mahase E. Covid-19: UK records first death, as world’s cases exceed 100 000. BMJ. 2020;368:m943. doi: 10.1136/bmj.m943. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) COVID-19 Response Team . 2020. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States. February 12–March 16. [Google Scholar]
- 6.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang Y.M., Hsu C.Y., Lai C.C. Impact of comorbidity on fatality rate of patients with Middle East respiratory syndrome. Sci Rep. 2017;7(1):1–9. doi: 10.1038/s41598-017-10402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang H., Zhang L. Risk of COVID-19 for patients with cancer. 2020;21(4):e181. doi: 10.1016/S1470-2045(20)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia Y., Jin R., Zhao J., Li W., Shen H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21(4):e180. doi: 10.1016/S1470-2045(20)30150-9. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang Y., Zhang H., Xie J. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng M.Y., Lee E.Y., Yang J. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1) doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kooraki S., Hosseiny M., Myers L., Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. (Feb 19) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseiny M., Kooraki S., Gholamrezanezhad A., Reddy S., Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. Am J Roentgenol. 2020;214(5):1 078–82. doi: 10.2214/AJR.20.22969. [DOI] [PubMed] [Google Scholar]
- 14.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 15.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020:1–9. doi: 10.1007/s00330-020-06801-0. Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao Y., Lu M., Liu Y., Cao B. The effects and management of viral pneumonia on lung cancer patients. Chin J Lung Cancer. 2020:23. doi: 10.3779/j.issn.1009-3419.2020.102.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu Y., Liu H., Hu K., Wang M., Wang Mengzhao. Clinical management of lung cancer patients during the outbreak of 2019 novel coronavirus disease (COVID-19) 2020;23(3):136–141. doi: 10.3779/j.issn.1009-3419.2020.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zieba M., Baranowska A., Krawczyk M. Pneumonia as a cause of death in patients with lung cancer. Radiol Oncol. 2003;37(3):167–174. (2003) [Google Scholar]
- 20.Nichols L., Saunders R., Knollmann F.D. Causes of death of patients with lung cancer. Arch Pathol Lab Med. 2012;136(12):1552–1557. doi: 10.5858/arpa.2011-0521-OA. [DOI] [PubMed] [Google Scholar]
- 21.Arjeyni Yaser, Goudarzi Hossein, Eslami Gita, Faghihloo Ebrahim. Viral respiratory infections in patients with cancer. Iran J Cancer Prev. 2017;10(2) [Google Scholar]
- 22.Madhusudhan K.S., Gamanagatti S., Seith A., Hari S. Pulmonary infections mimicking cancer: report of four cases. Singapore Med J. 2007;48(12):e327–e331. [PubMed] [Google Scholar]
- 23.Allison Inserro A. COVUD-19 and cancer: practices seek to protect patients, providers from growing pandemic. AJMC. 2020 [Google Scholar]
- 24.Ueda M., Martins R., Hendrie P.C. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020:1–4. doi: 10.6004/jnccn.2020.7560. [DOI] [PubMed] [Google Scholar]
- 25.Vilar-Compte D., Shah D.P., Vanichanan J. Influenza in patients with hematological malignancies: experience at two comprehensive cancer centers. J Med Virol. 2018;90(1):50–60. doi: 10.1002/jmv.24930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hirsch H.H., Martino R., Ward K.N., Boeckh M., Einsele H., Ljungman P. Fourth European Conference on Infections in Leukaemia (ECIL-4): guidelines for diagnosis and treatment of human respiratory syncytial virus, parainfluenza virus, metapneumovirus, rhinovirus, and coronavirus. Clin Infect Dis. 2013;56(2):258–266. doi: 10.1093/cid/cis844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tavil B., Azik F., Culha V. Pandemic H1N1 influenza infection in children with acute leukemia: a single-center experience. J Pediatr Hematol Oncol. 2012;34(1):48–50. doi: 10.1097/MPH.0b013e3182387d57. [DOI] [PubMed] [Google Scholar]
- 28.Lee G.E., Fisher B.T., Xiao R. Burden of influenza-related hospitalizations and attributable mortality in pediatric acute lymphoblastic leukemia. J Pediatr Infect Dis Soc. 2015;4(4):290–296. doi: 10.1093/jpids/piu066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Otenza L., Luppi M., Morselli M. Leukaemic pulmonary infiltrates in adult acute myeloid leukaemia: a high-resolution computerized tomography study. Br J Haematol. 2003;120:1058–1061. doi: 10.1046/j.1365-2141.2003.04192.x. [DOI] [PubMed] [Google Scholar]
- 30.Winer-Muram H.T., Arheart K.L., Jennings S.G. Pulmonary complication ns in children with hematologic malignancies: accuracy of diagnosis with chest radiography and CT. Radiology. 1997;204(3):643–649. doi: 10.1148/radiology.204.3.9280238. [DOI] [PubMed] [Google Scholar]
- 31.Liu B.L., Ma F., Wang J.N., Fan Y., Mo H.N., Xu B.H. Health management of breast cancer patients outside the hospital during the outbreak of 2019 novel coronavirus disease. Chin J Oncol. 2020;42(0):E002. doi: 10.3760/cma.j.cn112152-20200221-00110. 26. [DOI] [PubMed] [Google Scholar]
- 32.Chen Y.H., Peng J.S. Treatment strategy for gastrointestinal tumor under the outbreak of novel coronavirus pneumonia in China. Chin J Gastrointes Surg. 2020;23(2):I–IV. doi: 10.3760/cma.j.issn.1671-0274.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Zhu W.J., Wang J., He X.H. The differential diagnosis of pulmonary infiltrates in cancer patients during the outbreak of the 2019 novel coronavirus disease. Chin J Oncol. 2020;4 2(0):E008. doi: 10.3760/cma.j.cn112152-20200303-00166. 5. [DOI] [PubMed] [Google Scholar]