Dear Editor,
We recently reviewed papers on discharged COVID-19 patients with positive RT-PCR re-test [1], and we would like to discuss a role of low-dose CT in discharge decision based on our recent experience regarding the positive conversion of COVID-19 after two consecutive negative RT-PCR results.
Since the initial outbreak of coronavirus disease 19 (COVID-19) in December 2019, increasing numbers of patients have recovered and been discharged. Now is the time to turn our attention not only to diagnosis and treatment, but also to prevention of reactivation. In order to discharge patients from the hospital, most guidelines include no fever for more than 3 days, improvement of symptoms, and two consecutive negative real-time polymerase chain reaction (RT-PCR) test results [2]. However, there have been reports of false-negative RT-PCR results or reconfirmed cases after discontinuation of quarantine [3,4], highlighting the need to re-evaluate the guidelines for discharge. Also, Dou et al. [1] recently published an article describes serial CT features in discharged COVID-19 patients with positive RT-PCR re-tests, giving us a lesson that follow-up CT after discharge is essential. Accordingly, we would like to introduce a recent case from our hospital.
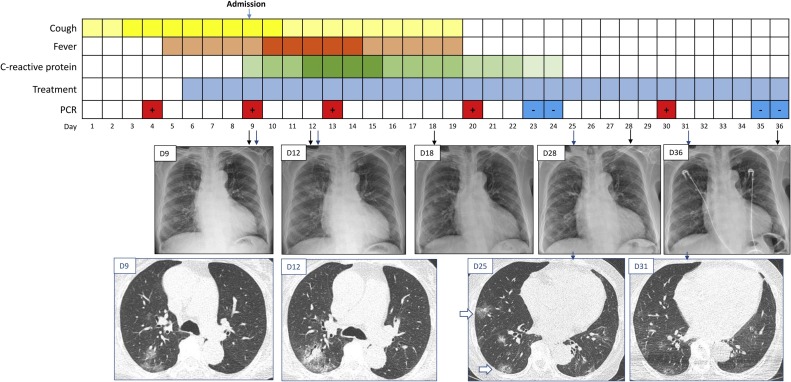
A 72-year-old woman was diagnosed with COVID-19 using an RT-PCR assay for the severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) via naso- and oropharyngeal swab and was admitted to our hospital. At admission (Day 9 from the initial symptom), low-dose chest CT (LDCT) revealed patchy peripheral ground-glass opacities (GGOs) in the right upper lobe. The patient had a high fever (> 38.3°C) for five days after hospitalization, and follow-up LDCT revealed progression of the lung lesions. After treatment, the patient’s fever and respiratory symptoms resolved. After 3 days without symptoms, two consecutive naso- and oropharyngeal swabs were negative for viral RNA, and opacities on chest radiographs were improving. The patient therefore met the criteria for hospital discharge (absence of fever or symptoms and two negative RT-PCR results) established by the Korea Centers for Disease Control and Prevention [5]; however, follow-up LDCT prior to discharge revealed newly developed multifocal GGOs in the lower lobes, which led to cancelation of discharge. After an additional 6 days, repeat naso- and oropharyngeal swab testing showed positive conversion. With continued treatment, the patient was discharged after two consecutive negative RT-PCR results and near complete resolution of her previous pneumonia without new lesions on LDCT (Fig. 1 ).
Fig. 1.
Clinical and radiologic courses of a 72-year-old patient with COVID-19 with positive conversion of RT-PCR. The patient’s low-dose chest CT identified newly developed lesions after two consecutive negative PCR results (Day 23, 24), which may have indicated reactivation of the disease. Repetition of the PCR test on Day 30 indicated positive conversion. After continued treatment, both radiologic and PCR results were negative on Days 35 and 36.
The depth of shading in the squares indicates the severity of fever and C-reactive protein concentration as follows: fever was categorized as low-grade fever (37.5–38.2℃), or high-grade fever (> 38.3℃); C-reactive protein elevation was categorized as < 1, 1–4.9, 5–9.9, ≥ 10 mg/dL. Lopinavir/ritonavir and hydroxychloroquine were used as treatments. PCR = polymerase chain reaction.
This case indicates that it is advisable to reconsider discharging patients with COVID-19 pneumonia whose radiologic manifestations and PCR results are mismatched. With regard to recently identified reactivation of COVID-19, use of LDCT as an ancillary diagnostic tool may reduce possible disease spread and improve our understanding of the pathophysiology of conversion of previously negative RT-PCR results to positive after discontinuation of quarantine.
Transparency document
References
- 1.Dou P., Zhang S., Wang C. Serial CT features in discharged COVID-19 patients with positive RT-PCR re-test. Eur. J. Radiol. 2020;127(June) doi: 10.1016/j.ejrad.2020.109010. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Centre for Disease Prevention and Control . 2020. Novel Coronavirus (SARS-CoV-2) - Discharge Criteria for Confirmed COVID-19 Cases.https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-Discharge-criteria.pdf [Google Scholar]
- 3.Han H., Luo Q., Mo F., Long L., Zheng W. SARS-CoV-2 RNA more readily detected in induced sputum than in throat swabs of convalescent COVID-19 patients. Lancet Infect. Dis. 2020;12(March) doi: 10.1016/s1473-3099(20)30174-2. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;27(February) doi: 10.1001/jama.2020.2783. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korea Center for Disease Control & Prevention . 2020. Updates on 2019 Novel Coronavirus: for Press Release.https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.