To the Editor:
Patients with heart failure (HF) require frequent medical contact and are at high risk of hospitalization.1 The rapid transmissibility of coronavirus disease 19 (COVID-19), associated mortality, and anticipated burden on the health care system forced dramatic changes in health care delivery for HF.2 , 3 The immediate need to incorporate telemedicine prompted recent publication of a Heart Failure Society of America expert consensus statement on use of telehealth in HF.4 We thus describe our initial COVID-19–era experience of a telemedicine-based strategy to manage an at-risk ambulatory HF patient cohort in our HF disease management and ambulatory diuresis clinic.
Methods
Patients are referred to the Johns Hopkins Heart Failure Bridge Clinic after hospital discharge or by outpatient providers. Clinic services include assessment by HF certified nurse practitioners, HF medication optimization, intravenous (IV) diuretic administration, laboratories, education, and care coordination. Patients may be seen same day and as frequently as needed. In response to the first Maryland COVID-19 cases and state-issued stay-at-home orders, we implemented a COVID-specific clinic workflow incorporating telemedicine. In-person visits occurred per provider discretion. Weekly clinic volumes and hospital HF discharges (using all patient refined diagnosis related group) were tabulated. Patient and visit characteristics, and need for hospitalization were collected for the initial COVID-19 response study period from March 16 to April 24, 2020. All patients were screened for COVID-19 symptoms5 and referred for testing as indicated. For comparison, clinic volumes and outcomes from March 18 to April 26, 2019, were tabulated. The study was approved by the Institutional Review Board.
Results
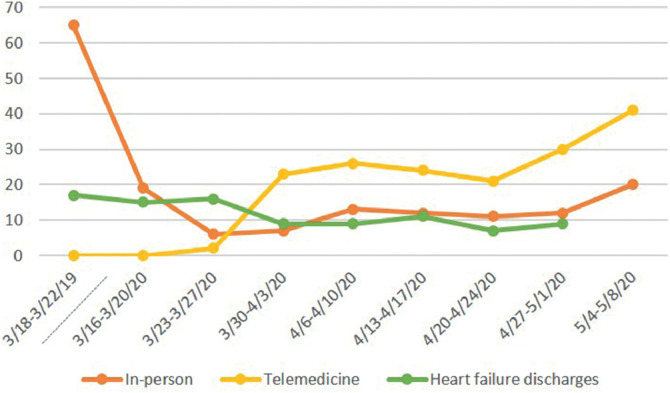
There were 116 patients (61 ± 14 years, 50% female, 70% black, with a left ventricular ejection fraction of 25 ± 21%) seen 164 times (Supplementary Table S1). Visit characteristics, including visit type, referral reason, diuretic interventions and disposition are depicted via flow diagram (Supplementary Fig. S1). Two-thirds of patients were seen after recent hospital discharge or for worsening HF. Weekly clinic volume trends by visit type are depicted in Fig. 1 . During the initial COVID-19 response period, telemedicine accounted for 96 visits (58.5%): 70 tele-audio, 26 tele-video.
Fig. 1.
Weekly telemedicine and in-person Johns Hopkins Heart Failure Bridge Clinic volumes and Johns Hopkins Hospital heart failure discharges before and during the COVID-19 pandemic.
Home oral diuretic dose was increased at 16.7% of telemedicine visits and decreased at 6.3%. All patients remained at home after telemedicine visit except for 6 referred for in-person clinic assessment. Of 68 in-person visits, 50% resulted in IV diuretic administration. Home oral diuretic dose was increased at 48% of in-person visits. Eight patients were referred from clinic for inpatient management (Supplementary Fig. S1). Sixteen patients were tested for COVID-19; 2 tested positive. There were 27 patients hospitalized within 30 days after clinic visit; 3 were referred to hospice by clinic team.
In the 2019 comparison group, 221 patients were seen 326 times, with 62 (19%) IV diuretic visits and 34 (15.4%) hospitalized within 30 days of the visit.
Discussion
We demonstrate the role of telemedicine integrated into a HF disease management clinic evaluating at-risk HF patients during the COVID-19 pandemic. Additionally, we found continued access to in-person assessment and ambulatory IV diuresis paramount to keeping HF patients out of the hospital.
Although telemedicine has been previously successfully used in HF,6 the urgency with which its implementation occurred during the COVID-19 pandemic is unprecedented. We initially had delayed but ultimately successful conversion from in-person to virtual visits, with visit rates increasing over time. Initially, the majority were conducted via tele-audio, reflective of early barriers in accessing videoconferencing that was compliant with the Health Insurance Portability and Accountability Act. These and other barriers to telemedicine access remain a challenge and may further widen the socioeconomic health care disparities that already exist in HF.7
Despite in-person visits commonly prompted by worsening HF, acute hospitalization was rare, likely owing to our ability to administer IV diuretics in the outpatient setting.8 Complete physical examination and laboratory studies are also possible, unlike with telemedicine, and allow safe and timely HF medication optimization and HF hospitalization prevention. Thus, the role of in-person assessment is invaluable and should be emphasized to HF patients, who we found were often hesitant to come to clinic. Additionally, hospitalization rate seemed to be higher during COVID-19 period compared with 2019; however, clinic volumes were one-half of those in 2019, possibly owing to more stable HF patients deferring clinic appointments.
From this initial experience, we recommend the following strategies be incorporated to optimize telemedicine in HF care. (1) Use hospitalization to educate and prepare patients for postdischarge virtual visits. (2) Empower and equip patients to perform self-care management and supply vital signs. (3) Use clinical infrastructure to receive, interpret, and act on data from increasingly available physiologic monitoring technologies. These initial experiences during COVID-19 lend insights to optimization of future outpatient HF care delivery, beyond the current global health emergency.
Declaration of Competing Interest
No relevant disclosures.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.cardfail.2020.06.003.
Appendix. Supplementary materials
References
- 1.Krumholz H.M., Merrill A.R., Schone E.M., Schreiner G.C., Chen J., Bradley E.H. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 2.Hendren N.S., Drazner M.H., Bozkurt B., Cooper L.T., Jr Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141:1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendren N.S., Grodin J.L., Drazner M.H. Unique patterns of cardiovascular involvement in COVID-19. J Card Fail. 2020 May 14 doi: 10.1016/j.cardfail.2020.05.006. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorodeski E.Z., Goyal P., Cox Z.L., Thibodeau J.T., Reay R.E., Rasmusson K. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020 Apr 18 doi: 10.1016/j.cardfail.2020.04.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel A., Jernigan D.B, 2019-nCoV CDC Response Team Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak - United States, December 31, 2019-February 4, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:140–146. doi: 10.15585/mmwr.mm6905e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kashem A., Droogan M.T., Santamore W.P. Web-based Internet telemedicine management of patients with heart failure. Telemed J E Health. 2006;12:439–447. doi: 10.1089/tmj.2006.12.439. [DOI] [PubMed] [Google Scholar]
- 7.Chaudhry S.I., Herrin J., Phillips C. Racial disparities in health literacy and access to care among patients with heart failure. J Card Fail. 2011;17:122–127. doi: 10.1016/j.cardfail.2010.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brinkley D.M., Jr., Burpee L.J., Chaudhry S.P. Spot urine sodium as triage for effective diuretic infusion in an ambulatory heart failure unit. J Card Fail. 2018;24:349–354. doi: 10.1016/j.cardfail.2018.01.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.