Abstract
Purpose
Limited research has examined maternal experiences of racial/ethnic discrimination in relation to child cardiometabolic health. In this study, we investigated whether maternal experiences of ethnic discrimination were associated with cardiometabolic risk in Hispanic/Latino youth several years later.
Methods
Our sample included 1,146 youth (8 to 16 years) from the Study of Latino (SOL) Youth (2012–2014), who were children of the Hispanic Community Health Study/Study of Latinos participants (HCHS/SOL; 2008–2011). We used regression models to examine the prospective associations between maternal-report of ethnic discrimination in relation to her child’s body mass index (BMI) z-score, metabolic syndrome score (MetS), and C-reactive protein (hsCRP) levels two years later.
Results
Maternal ethnic discrimination was associated with youth hsCRP, but not BMI or MetS (p-values>.05). Adjusting for age, nativity, and national background, maternal ethnic discrimination was associated with higher (log) hsCRP levels (β=0.18, 95% CI=0.04—0.32) in children. This association was robust to adjustment for maternal and household characteristics (β=0.17, 95% CI=0.04—0.31), as well as maternal depression and maternal BMI.
Conclusions
Maternal ethnic discrimination is associated with inflammation among Hispanic/Latino youth, and not BMI z-score or MetS. Studies are needed to address temporality and pathways.
Cardiometabolic disorders begin in childhood (1) and are among the leading causes of death among adults in the US (2). The American Heart Association has acknowledged the large public health burden of cardiometabolic disorders in Hispanic/Latinos in the US (3), a large and rapidly growing minority group (3). There are persistent racial/ethnic and socioeconomic disparities in the incidence, treatment, and outcomes of cardiometabolic disorders that are shaped by social determinants (4). Racial/ethnic discrimination, defined as differential or unfair treatment based on actual or perceived membership in a racial/ethnic group, is now recognized as a social determinant of health for both children and adults (5, 6). Research with Hispanic/Latino adolescents shows that discrimination is associated with mental health and behavioral problems (5, 7). In the present study, we extend this work to examine the association between maternal experiences of ethnic discrimination and youth cardiometabolic risk factors in a diverse Hispanic/Latino population. This study builds on the integrative model for minority youth (8), which emphasizes the role of discriminatory experiences in the health of minority youth, and the concept of “linked lives” (9). This model directs researchers to consider the connectedness among individuals within families and across generations (i.e., discriminatory experiences in parents’ lives would be expected to have implications for the health of their children, and vice versa).
A substantial body of research has documented that stressful environments are associated with poorer child outcomes (10), including a variety of physiological factors related to the development of cardiometabolic disorders (11, 12). Maternal experiences of racial/ethnic discrimination may be an important, yet under-explored, form of childhood adversity (13) which could influence development via a number of pathways, including elevated stress in the household that could erode capacity for supportive and sensitive parenting (5). Furthermore, by definition, maternal experiences of discrimination are likely to be associated with difficulties that follow from unfair experiences, including restricted access to high quality healthcare, housing, or employment. Prior studies that have examined a parent’s experiences of discrimination (14–19), including the related construct of acculturative stress (20, 21), have documented strong associations with child socioemotional and behavioral outcomes and overall family functioning..
Only a few prior studies have examined parental experiences of racial/ethnic discrimination in relation to non-mental health outcomes (e.g., (22, 23)), and most of these studies have relied on parent-reported BMI or history of illness, have largely examined young children (16, 18, 22, 23), and have rarely focused on Hispanic/Latinos (see (16, 17) for exceptions). To our knowledge, there are no prior studies of parental experiences of racial/ethnic discrimination in relation to cardiovascular risk outcomes among youth in the US or elsewhere.
Using data from the Study of Latino (SOL) Youth, we examined the association between maternal experiences of ethnic discrimination and Hispanic/Latino youth cardiometabolic risk outcomes approximately two years later, including body mass index (BMI), metabolic syndrome (MetS) score, and inflammation (indicated by high sensitivity C-reactive protein level (hsCRP)). Given the sex and age differences documented in SOL for a range of CVD risk outcomes (24), and the potential for sex or age differences in response to maternal experiences of ethnic discrimination, we also examined whether associations differed by sex or age. The results from this investigation may be used to 1) generate hypotheses for future prospective studies on factors that influence the emergence of racial/ethnic health disparities in cardiometabolic outcomes, 2) illustrate the importance of gathering data on discriminatory experiences of parents to better understand and devise strategies to improve cardiometabolic health among racial/ethnic minority youth over the life course, and 3) support structural-level strategies to reduce discrimination agains Hispanics/Latinos in the U.S.
METHODS
Study design and data collection
The Study of Latino Youth (SOL-Youth) is a population-based study of youth ages 8 to 16 years recruited between 2012 to 2014 from 4 communities in the US (Bronx, NY; Chicago, IL; Miami, FL; San Diego, CA). Details of recruitment and study design have been previously published (24, 25). Briefly, SOL-Youth enrolled a subset of the offspring of participants in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a comprehensive multicenter community-based cohort study of Hispanics/Latinos in the United States. HCHS/SOL participants (n=16,415 from 9,872 households) were recruited through a 2-stage area probability sampling design, as described previously (26). The HCHS/SOL baseline interviews and clinical evaluation were conducted in English or Spanish at in-person clinic visits during 2008–2011.
Of 6,741 screened households of HCHS/SOL participants, 1,777 eligible children age 8–16 were identified and 1,466 were enrolled in SOL-Youth, representing a participation rate of 82%. Participants were instructed to fast for 10 hours prior to the SOL-Youth baseline visit, which was conducted in 2012–2014 and included in-person interviews of youth participants and their accompanying parent or caregiver, height and weight measurements of the parent/caregiver, and a clinical examination that included a blood draw. Both studies were approved at the institutional review boards for each participating center. All HCHS/SOL participants gave written informed consent, and all youth and adults in SOL-Youth provided written informed assent and consent, respectively.
The present study excluded 270 youth (18.42%) for whom the SOL participant living in their household was not their mother (in order to improve homogeneity of the exposure variable), and an additional 48 youth were excluded because their mother did not respond to the item on ethnic discrimination (n excluded=318; n elgible for inclusion=1,148). Of the remaining 1,148 youth, A total of 1085 children had valid data for all components required to create the MetS score (59 children were missing a required measurement, 18 did not fast at least 8 hours before the clinic visit), and 1,144 children had a valid BMI value. There were 1,093 children with a valid hsCRP value (41 children had missing hsCRP, and 14 children were excluded due to hsCRP levels greater than 10 mg/L). A total of 1,146 youth had at least one of the three outcomes.
Maternal ethnic discrimination
At the HCHS/SOL parent exam in 2008–2011, which was on average 2.6 (SD=0.9) years prior to the SOL-Youth visit, parents/guardians were asked “How often do people treat you unfairly because you are Hispanic/Latino?”, taken from the Perceived Ethnic Discrimination Questionnaire–Community Version (PED-CV) (27). The response options included ‘often’, ‘always’, ‘sometimes’ and ‘never’ and this item was treated as a continuous variable.
Youth cardiometabolic risk
Youth body composition was assessed using standardized protocols. Weight was measured to the nearest 0.1 kilogram with a digital scale (Tanita Body Composition Analyzer, model TBF300; Tanita, Tokyo, Japan). Standing height was measured to the nearest centimeter in triplicate by stadiometer (Seca model 222; Seca, Hamburg, Germany). BMI was calculated as weight divided by mean height squared. Youth BMI z-scores according to 2000 growth charts were computed using the SAS Macro provided by the Centers for Disease Control and Prevention.
High sensitivity C-reactive protein (hsCRP) was measured on either a Roche/Modular P (prior to January 1, 2014) or Roche COBAS 6000 chemistry analyzer (starting January 1, 2014; Roche Diagnostics Corporation) using the same methodology, calibration and control for all samples. Details for measurement of triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), and fasting plasma glucose (FPG) have been described previously (24). Seated systolic blood pressure (SBP) was measured in triplicate by sphygmomanometer after 5 minutes rest, with the average of the last 2 measures used in analyses. The metabolic syndrome z-score (MetS-z) was calculated using validated gender-specific equations for Hispanic youth (28, 29) (Appendix 1). This score advances on the traditional approach to calculating MetS by avoiding use of thresholds and assumptions that each MetS component has an equal weight, and accounts for how MetS may manifest differently across sex and racial/ethnic groups (30).
Covariates
Other covariates were assessed through interviews with mothers at the SOL-Youth study visit, including youth’s age, sex, and caregiver/household characteristics (age, language preference, educational attainment, annual household income, employment/student status, nativity and marital status). Youth reported their place of birth as within or outside the 50 US states, and reported their Hispanic/Latino background. All covariates were treated as categorical variables; please see Table 1 for the categories for each covariate. Maternal depression and maternal BMI were included as a covariates in secondary models given that each could function as a confounder (i.e., a temporally prior cause of reported discrimination and child cardiometabolic outcomes) or pathway variable.. Maternal BMI was assessed following the same protocol followed for youth, described above, and maternal depressive symptoms were assessed using a 10-item version of the Center for Epidemiologic Studies Depression (CES-D) scale (31). We used a cut-point of ≥ 10 which is a common cut-point for probable depression using this version of the CES-D (32).
Table 1.
Mother’s reported level of discrimination at the SOL/HCHS interview (2008–2011) and Characteristics of SOL youth participants (n=1146 adolescents, 2012–2014)
| By mother’s reported discrimination (SOL/HCHS 2008–2011) | |||||
|---|---|---|---|---|---|
| Overall | Never (n=514) | Sometimes (n=515) | Often/Always (n=117) | ||
| n (weighted %)1 | Weighted column percent (95% CI) | p-value2 | |||
| Adolescent Characteristics | |||||
| Body mass index, z-score3 | 1144 | 0.69 (0.56, 0.82) | 0.80 (0.63, 0.97) | 0.89 (0.64, 1.15) | 0.26 |
| MetS Score, z-score3 | 1085 | −0.13 (−0.23, −0.04) | −0.06 (−0.18, 0.07) | −0.20 (−0.36, −0.04) | 0.34 |
| hsCRP, mg/dL3 | 1093 | 0.45 (0.40, 0.51) | 0.48 (0.42, 0.55) | 0.73 (0.55, 0.96) | 0.008 |
| Sex | 0.96 | ||||
| Male | 585 (50%) | 258 (50%) | 261 (50%) | 66 (51%) | |
| Female | 561 (50%) | 256 (50%) | 254 (50%) | 51 (49%) | |
| Age group (years) | 0.66 | ||||
| 8–9 | 259 (21%) | 107 (20%) | 125 (23%) | 27 (22%) | |
| 10–11 | 269 (22%) | 127 (22%) | 116 (21%) | 26 (21%) | |
| 12–13 | 287 (22%) | 125 (21%) | 137 (25%) | 25 (17%) | |
| 14–16 | 331 (35%) | 155 (37%) | 137 (31%) | 39 (40%) | |
| Born outside of U.S. mainland | 0.21 | ||||
| Yes | 235 (20%) | 111 (19%) | 97 (18%) | 27 (29%) | |
| No | 903 (80%) | 400 (81%) | 413 (82%) | 90 (71%) | |
| Hispanic/Latino background | 0.61 | ||||
| Mexican | 518 (48%) | 226 (51%) | 236 (46%) | 56 (44%) | |
| Central American | 92 (6%) | 33 (4%) | 46 (7%) | 13 (10%) | |
| Cuban | 72 (5%) | 45 (5%) | 24 (4%) | 3 (3%) | |
| Dominican | 125 (13%) | 58 (12%) | 52 (13%) | 15 (18%) | |
| Puerto Rican | 103 (10%) | 47 (11%) | 48 (10%) | 8 (7%) | |
| South American | 56 (4%) | 26 (4%) | 26 (4%) | 4 (4%) | |
| Other/>1 | 149 (14%) | 64 (12%) | 68 (16%) | 17 (14%) | |
| Household & maternal characteristics | |||||
| Highest parental education | 0.25 | ||||
| No H.S. Diploma/GED | 421 (38%) | 168 (36%) | 202 (38%) | 51 (48%) | |
| High school diploma/GED | 358 (31%) | 168 (32%) | 154 (28%) | 36 (33%) | |
| > H.S. diploma/GED | 367 (31%) | 178 (32%) | 159 (33%) | 30 (19%) | |
| Total household income | 0.009 | ||||
| ≤$20,000 | 556 (52%) | 247 (50%) | 244 (49%) | 65 (69%) | |
| $20,001–$40,000 | 377 (32%) | 161 (33%) | 177 (33%) | 39 (27%) | |
| >$40,000 | 144 (16%) | 66 (17%) | 71 (18%) | 7 (4%) | |
| Maternal depressive symptoms | 0.007 | ||||
| CES-D <10 | 702 (65%) | 359 (72%) | 288 (63%) | 55 (43%) | |
| CES-D ≥10 | 424 (35%) | 145 (28%) | 218 (37%) | 61 (57%) | |
| Maternal BMI, mean (95% CI) | 1144 | 30.0 (29.0, 31.0) | 29.8 (28.9, 30.8) | 32.0 (29.7, 34.3) | 0.22 |
| Mother’s age (years) | 0.31 | ||||
| 24–34 | 353 (34%) | 148 (32%) | 162 (36%) | 43 (39%) | |
| 35–49 | 733 (63%) | 346 (66%) | 317 (60%) | 70 (60%) | |
| 50–73 | 60 (3%) | 20 (2%) | 36 (4%) | 4 (1%) | |
| Mother’s language preference | 0.71 | ||||
| Spanish | 975 (84%) | 441 (86%) | 432 (83%) | 102 (85%) | |
| English | 171 (16%) | 73 (15%) | 83 (17%) | 15 (15%) | |
| Maternal employment status | 0.68 | ||||
| Not employed or in school or retired | 592 (56%) | 272 (58%) | 265 (55%) | 55 (51%) | |
| Employed or in school | 535 (44%) | 230 (42%) | 244 (45%) | 61 (49%) | |
| Maternal marital status | 0.61 | ||||
| Single | 243 (23%) | 99 (20%) | 114 (24%) | 30 (29%) | |
| Married or living with a partner | 715 (62%) | 326 (65%) | 325 (62%) | 64 (53%) | |
| Widowed, divorced or separated | 187 (15%) | 89 (15%) | 75 (14%) | 23 (18%) | |
| Born outside of U.S. mainland | 0.77 | ||||
| Yes | 979 (86%) | 448 (87%) | 431 (85%) | 100 (83%) | |
| No | 166 (15%) | 66 (13%) | 83 (15%) | 17 (17%) | |
May not sum to sample total due to missing data
P-values indicate any difference between groups
N’s for BMI z-score, metabolic symptom (MetS) score and high sensitivity C-reactive protein are smaller than total N due to missing values or abnormal values.
Percentages may not sum to 100 due to rounding.
Note: BMI=body mass index; MetS = metabolic syndrome score; hsCRP=high sensitivity C-reactive protein.
Statistical analysis
All analyses, accounting for household clustering, study site, other design effects and sampling weights, were performed using SAS version 9.3 (SAS Institute, Cary, NC) and SUDAAN release 11.0.1 (RTI International, Research Triangle Park, NC). Descriptive statistics for the overall sample and across levels of maternal ethnic discrimination were computed; differences in distributions of classification variables were assessed using Rao-Scott chi-squared tests and differences in means were evaluated using Wald F statistics from survey linear regression models.
Prior to conducting our multiple variable models, we tested for effect modification by sex and age to examine whether stratified models were appropriate. No age or sex interactions were identified at p<.10 (see Appendix 2 for interaction tests) so all models used data pooled across age and sex.
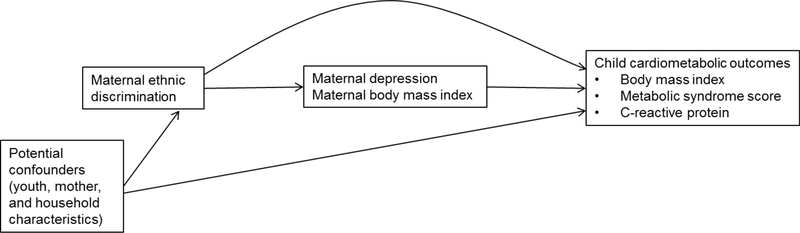
The conceptual model that we used to develop our analyses is presented in Appendix 3. Multiple variable survey linear regression models were constructed for each dependent variable of interest: BMI-z, MetS-z, and hsCRP. Initial models adjusted for youth sex, age, nativity, and Hispanic/Latino background. Subsequent models adjusted for maternal and household characteristics, including educational attainment, annual household income, mother’s age, language preference, employment/student status, nativity and marital status. We selected this set of potential confounders based on the existing literature. We did not use a priori criteria for a variable to be considered a confounder. We present results for the minimally- and fully-adjusted models. Beta estimates were derived from models treating maternal ethnic discrimination as a continuous variable. If associations were observed at p<.05, we evaluated the degree to which maternal depressive symptoms and maternal BMI explained the association by including these variables in subsequent models. We did not conduct formal mediation analyses given the cross-sectional design.
Incomplete data for adjustment variables ranged from 1 participant for parent marital status to 3.6% of the analytic sample for maternal BMI, and based on Little’s MCAR test, the missing covariates were not missing at random (χ2 = 110.76, df=66, p<.001). Misssing values on covariates were multiply imputed with logistic regression for binary and ordinal variables, predictive mean matching for continuous variables, and discriminant function methods for Hispanic/Latino background. Imputation models included all covariates noted above, as well as the design variables sampling strata and weight, and all dependent variables. Primary analyses were performed on 10 imputed data sets. Parallel analyses were also conducted in which only participants with complete data for all variables were included, and results were substantively the same. In addition, all analyses were repeated with the sample expanded to include youth with non-mother caregiver respondents.
RESULTS
Our sample of youth included an equal proportion of females and males, with 20% born outside of the US. Nearly half of the sample (48%) identified as having Mexican background, and over half of the sample lived in a household earning less than $20,000 a year (52%). Over a third of the youth’s mothers reported depression symptom scores above a threshold indicative of risk for a clinical depression disorder (35%), and the majority of the youth’s mothers were married or living with a partner (62%) (Table 1). At the HCHS/SOL interview,45 percent of the mothers reported that they were never treated unfairly, whereas 44 reported that they were sometimes treated unfairly, and the remaining 10% reported that they often or always treated unfairly due to their ethnicity. Reports of maternal ethnic discrimination were more common for mothers with lower household incomes (p−=0.009) and for mothers with elevated depressive symptoms (p =0.007).
In bivariate analyses (Table 1), maternal ethnic discrimination showed a dose-response relationship with hsCRP, with reports of more frequent discrimination associated with higher level of hsCRP (p =0.008), whereas the bivariate trends for maternal ethnic discrimination and BMI and MetS were not significant (p=0.26 and 0.34, respectively). Consistent with the bivariate results, in multiple variable linear regression models reports of maternal ethnic discrimination were not associated with youth BMI and MetS score at p<.05, although for the effect estimate for the association between maternal ethnic discrimination and BMI z-score was in the hypothesized direction (Table 2).In models adjusted for youth’s age, nativity, and national background,maternal ethnic discrimination was associated with elevated levels of (log) hsCRP (Model 1, β=0.18, 95% CI=0.0.04—0.32). The association remained similar with sequential adjustment for additional covariates including maternal and household characteristics (Model 2, β=0.17, 95% CI=0.04—0.31). Full model results to display associations for all covariates are presented in Appendix 4. There are only a few notable associations between the covariates and outcomes, including a protective (i.e., inverse) association between U.S. mainland birth and MetS score (Model 2, β=−0.18, 95% CI=−0.36—−0.01). Similarly, youth of parents with a college education or more had lower BMI z-score (Model 2, β=0.28, 95% CI=−0.54—−0.02) and MetS score (β=−0.20, 95% CI=−0.38—−0.03) relative to youth with parents who had less than a high school education.
Table 2.
Multiple variable adjusted associations between maternal ethnic discrimination1 and youth cardiometabolic outcomes
| BMI | MetS z-score | Log hsCRP | ||||
|---|---|---|---|---|---|---|
| Beta (95% CI) | p-value | Beta (95% CI) | p-value | Beta (95% CI) | p-value | |
| Model 1: | ||||||
| Maternal discrimination | 0.11(−0.01, 0.23) | 0.08 | 0.01(−0.09, 0.10) | 0.89 | 0.18( 0.04, 0.32) | 0.01 |
| Model 2 | ||||||
| Maternal discrimination | 0.10(−0.03, 0.22) | 0.14 | −0.01(−0.10, 0.09) | 0.91 | 0.17( 0.04, 0.31) | 0.01 |
HSHC/SOL maternal-report discrimination (2008–2011).
Model 1: adjusted for youth’s sex, age, nativity, and national background.
Model 2: Model 1 + mother and household characteristics, including highest parental education, total household income, and mother’s age, language preference, employment/student status, nativity and marital status.
Note: BMI=body mass index; MetS = metabolic syndrome score; hsCRP=high sensitivity C-reactive protein.
Finally, we considered several additional models with variables that could be on the causal pathway linking maternal ethnic discrimination to levels of hsCRP in youth, including maternal depression and maternal BMI. When maternal depression was added to the adjusted model (i.e., Model 2), the coefficient for maternal ethnic discrimination was unchanged (β=0.17, 95% CI=0.04—0.31) and maternal depression was not associated with youth hsCRP (β=−0.02, 95% CI=−0.20—0.17). When maternal BMI was additionally included in the adjusted model, the coefficient for maternal ethnic discrimination was slightly attenuated (β=0.16, 95% CI=0.02—0.29) although maternal BMI was not associated with youth hsCRP (β=0.04, 95% CI=−0.03—0.05). Given that maternal ethnic discrimination was not associated with youth BMI, youth BMI was not considered as a potential pathway linking maternal ethnic discrimination and youth hsCRP.
As a sensitivity analysis, we replicated our analyses with the sample expanded to additionally include youth with non-mother caregiver respondents (data not shown); results were similar.
DISCUSSION
Summary
Drawing on data from a large sample of Hispanic/Latino youth of diverse national backgrounds, we documented elevated levels of hsCRP among children whose mothers had experienced higher levels of ethnic discrimination. However, we did not observe a relationship between maternal ethnic discrimination and youth BMI or metabolic syndrome severity score. The association between maternal ethnic discrimination and hsCRP levels in youth was robust to adjustment for maternal depression and maternal BMI.
A growing body of research has linked adverse social conditions, including low socioeconomic status and maltreatment, to elevated inflammation among youth (11); our study extends this literature to include maternal ethnic discrimination. The current findings are of public health significance, as inflammation is known to track from childhood into adulthood (33), is associated with other cardiovascular risk factors among youth (e.g., disturbed endothelial function, intima media thickening (34)) and is correlated with subsequent diabetes and CVD in adults (35). Prior studies suggest that maternal ethnic discrimination could impact adolescent wellbeing through a variety of intermediate pathways that were not directly tested in our study, including stress in the household, health behaviors (e.g., diet, sleep), and activation of arousal and vigilance (36). These processesmay influence hypothalamic pituitary adrenal axis or sympathetic nervous system dysregulation (37) and contribute to low-grade chronic inflammation (38, 39).
The findings from this study only partially align with prior research on parent’s experiences of discrimination and child physical (22, 23) and socioemotional outcomes (14–19), given that we did not observe associations for BMI or MetS. To our knowledge, no other studies have examined parent’s experiences of discrimination in relation to children’s inflammation levels; however, two prior studies of US Hispanic/Latino youth have documented associations between parent’s discrimination and youth mental health (16, 17). In a two-week daily-diary study of 138 parent-child dyads (children ages 3–5 years) in a Southeastern city, Mexican immigrant parents’ report of workplace discrimination was associated with children’s internalizing and externalizing behaviors (16). Similarly, in a one-year prospective study of 344 Mexican American high school students in Los Angeles, CA, parental experiences of discrimination was associated with lower self-esteem and higher internalizing symptoms (17). Similar to our study, a cross-sectional analysis of the UK Millennium Cohort Study data at age five documented a positive association between maternal experiences of racism and child obesity, but the effect estimate was not significant at p<.05 (23).
There are several limitations to consider. First, this is an observational design; accordingly, we are only able to demonstrate associations, and despite adjustment for potential individual- and family-level confounders, our results are susceptible to unmeasured confounding by either contemporary unmeasured variables or pre-/post-natal characteristics (e.g., depression symptoms or weight during pregnancy, birthweight, etc.). Related, missing data were not missing completely at random. However we controlled for variables associated with missingness, and also used multiple imputed data sets. Second, the sample is not representative of the Hispanic/Latino youth population in the US, which has implications for external validity of the findings. Notably, the sample originates from four communities that are among the 15 areas with the largest concentrations of Hispanic/Latinos in the US (24). Third, although maternal ethnic discrimination was assessed temporally prior to assessment of the offspring outcomes, which is a strength of the study, discrimination was measured using a single item which limited precision for the assessment of discrimination. In addition, this item relied on self-report which may have introduced bias, and the item did not include a timeframe. Fourth, the validation analysis for the MetS score (29) was based on data from adolescents 12–19 years old. We opted to use this score, based on research suggesting that this continuous approach is advantageous for identifying individuals at risk for developing CVD and type 2 diabetes, even when including children younger than 12 years (28). Finally, information on maternal ethnic discrimination was obtained exclusively from maternal-report, and we did not include information on paternal experiences of discrimination. Moving forward, it will be valuable to utilize longitudinal studies with repeated measures of discrimination, and to comprehensively assess and combine maternal and paternal reports with child reports (13).
This study makes a number of contributions to the literature on vicarious racism and child health and development, given that we utilized a large sample of youth from four metropolitan areas with large Hispanic/Latino populations, which enabled recruitment of youth from diverse national backgrounds, and tests of age and sex interactions. In addition, HCHS/SOL and SOL Youth included detailed assessments of maternal and household characteristics, which allowed us to adjust for an array of potential confounders. Of the existing studies on parental discrimination and child health, this is the first to consider multiple biomarker assessments of cardiometabolic risk rather than subjective reports of child health. In using biological measures of health as outcomes in this study, we avoid biases inherent to self- or parent-report that may depend on physician diagnoses, and gain insights on pre-clinical or pre-symptomatic processes implicated in the development of cardiometabolic disorders. Our study suggests that the impact of maternal discrimination may extend beyond psychological and behavioral health in youth, to levels of inflammation, prior to adulthood.
In conclusion, maternal experiences of ethnic discrimination were associated with higher hsCRP among Hispanic/Latino youth, and did not relate to BMI z-score or MetS score in this population. Although our results were not consistent across all outcomes that we examined, similar to studies from around the world, including the U.S. (14–18), Australia (22), the United Kingdom (23), and New Zealand (40), our results suggest that interventions to improve health outcomes for racial/ethnic minority youth, including cardiometabolic outcomes in adolescence and throughout life, should consider influences beyond individual health behaviors (19, 23). It may be beneficial for future interventions to attend to parental experiences of racism, at the individual and institutional levels (41). In light of the current national climate towards immigrants and racial/ethnic minorities in the U.S. and around the world (42), it is critical to improve our understanding of the association between parental discrimination and child cardiometabolic health in order to inform social policies as well as targeted interventions to prevent racism (43, 44) and improve outcomes for youth affected by vicarious racism (13).
Acknowledgments
Support:
The SOL Youth Study was supported by Grant Number R01HL102130 from the National Heart, Lung, And Blood Institute. The children in SOL Youth are drawn from the study of adults: The Hispanic Community Health Study/Study of Latinos, which was supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). NS was supported by a Research and Scholarship Award from the Graduate School, University of Maryland and Grant P3022586 from the W. K. Kellogg Foundation. MJG was supported by NHLBI grant R01HL120960
Appendix 1. Validated gender-specific equations to calculate metabolic syndrome z-score for Hispanic youth
Boys: MetS-z = 3.2971 + 0.2930*BMI-z 0.0315* HDL-c + 0.0109*SBP + 0.6137*log(TG) + 0.0095*FPG
Females: MetS-z = 4.7637 + 0.3520*BMI-z 0.0263* HDL-c + 0.0152*SBP + 0.6910*log(TG) + 0.0133*FPG
Appendix 2.
Sex- and age-specific associations between maternal ethnic discrimination and cardiovascular disease risk factors in youth
| Beta (95% CI) | P-interaction | |
|---|---|---|
| BMI Z-score | ||
| 8–12 years | 0.07(−0.13, 0.27) | |
| 13–16 years | 0.12(−0.04, 0.28) | 0.71 |
| Male | 0.07(−0.13, 0.27) | |
| Female | 0.12(−0.03, 0.28) | 0.68 |
| MetS Z-score | ||
| 8–12 years | −0.03(−0.18, 0.13) | |
| 13–16 years | 0.01(−0.13, 0.14) | 0.74 |
| Female | −0.02(−0.16, 0.13) | |
| Male | 0.01(−0.11, 0.12) | 0.82 |
| Log (hsCRP) | ||
| 8–12 years | 0.22( 0.02, 0.43) | |
| 13–16 years | 0.13(−0.04, 0.29) | 0.45 |
| Male | 0.26( 0.07, 0.46) | |
| Female | 0.08(−0.08, 0.24) | 0.12 |
Time 1= HSHC/SOL maternal-report discrimination (2008–2011).
Beta estimates derived from linear regression models including an interaction term between maternal-report discrimination and age or sex, while adjusting for age, sex, place of birth, national background, parent educational attainment, annual household income, parent age, parent language preference, parent marital status, nativity and an indicator for parent student and/or employment; age-interaction models additionally adjusted for age differences within age groups.
Note: hsCRP=high sensitivity C-reactive protein; BMI=body mass index; MetS=metabolic syndrome symptoms
Appendix 3.
Conceptual Model
Appendix 4.
Multiple variable adjusted associations between maternal ethnic discrimination1 and youth cardiometabolic outcomes
| BMI | MetS z-score | Log hsCRP | ||||
|---|---|---|---|---|---|---|
| Variable | Model 1 | Model 2 | Model 1 | Model 1 | Model 1 | Model 2 |
| Maternal discrimination | 0.11(−0.01, 0.23) | 0.10(−0.03, 0.22) | 0.01(−0.09, 0.10) | −0.01(−0.10, 0.09) | 0.18( 0.04, 0.32) | 0.17( 0.04, 0.31) |
| Youth’s sex (male vs female) | −0.13(−0.30, 0.05) | −0.13(−0.30, 0.05) | 0.06(−0.08, 0.20) | 0.05(−0.08, 0.19) | −0.03(−0.20, 0.14) | −0.03(−0.19, 0.14) |
| Youth’s age (years) | ||||||
| 10–11 vs 8–9 | 0.13(−0.09, 0.36) | 0.13(−0.09, 0.36) | 0.27( 0.11, 0.44) | 0.26( 0.09, 0.42) | −0.02(−0.27, 0.23) | −0.02(−0.26, 0.22) |
| 12–13 vs 8–9 | −0.03(−0.27, 0.21) | −0.07(−0.32, 0.18) | 0.12(−0.08, 0.31) | 0.08(−0.11, 0.27) | −0.09(−0.32, 0.14) | −0.14(−0.37, 0.09) |
| 14–16 vs 8–9 | 0.00(−0.23, 0.24) | −0.05(−0.28, 0.17) | 0.29( 0.14, 0.45) | 0.21( 0.05, 0.37) | −0.08(−0.32, 0.16) | −0.15(−0.39, 0.09) |
| US mainland born (Yes vs No) | −0.10(−0.32, 0.12) | −0.11(−0.35, 0.13) | −0.21(−0.37,−0.04) | −0.18(−0.36,−0.01) | −0.09(−0.30, 0.11) | −0.10(−0.32, 0.11) |
| Hispanic/Latino background | ||||||
| Central American vs Mexican | −0.36(−1.04, 0.32) | −0.35(−0.90, 0.19) | −0.20(−0.53, 0.13) | −0.23(−0.53, 0.07) | −0.31(−0.65, 0.02) | −0.32(−0.65, 0.01) |
| Cuban vs Mexican | −0.10(−0.51, 0.32) | −0.04(−0.45, 0.37) | −0.24(−0.52, 0.04) | −0.21(−0.49, 0.07) | 0.04(−0.37, 0.44) | 0.06(−0.33, 0.46) |
| Dominican vs Mexican | 0.25(−0.01, 0.50) | 0.25(−0.01, 0.51) | −0.12(−0.30, 0.07) | −0.10(−0.29, 0.09) | 0.11(−0.15, 0.38) | 0.12(−0.15, 0.39) |
| Puerto Rican vs Mexican | 0.07(−0.22, 0.36) | 0.03(−0.30, 0.35) | −0.11(−0.29, 0.07) | −0.04(−0.22, 0.14) | 0.06(−0.22, 0.35) | 0.04(−0.26, 0.35) |
| South American vs Mexican | 0.00(−0.29, 0.29) | −0.01(−0.28, 0.26) | −0.18(−0.47, 0.10) | −0.23(−0.49, 0.03) | −0.17(−0.65, 0.30) | −0.19(−0.64, 0.27) |
| Mixed/other vs Mexican | 0.10(−0.16, 0.37) | 0.12(−0.14, 0.38) | −0.05(−0.26, 0.17) | 0.01(−0.22, 0.24) | 0.20(−0.06, 0.46) | 0.21(−0.06, 0.48) |
| Highest parental education | ||||||
| High school vs <high school | −0.19(−0.39, 0.01) | −0.09(−0.25, 0.07) | −0.16(−0.36, 0.05) | |||
| College or more vs <high school | −0.28(−0.54,−0.02) | −0.20(−0.38,−0.03) | −0.17(−0.40, 0.06) | |||
| Annual household income | ||||||
| >$20K-40K vs $20K or less | −0.03(−0.26, 0.19) | −0.01(−0.18, 0.15) | 0.01(−0.20, 0.21) | |||
| >$40K vs $20K or less | −0.08(−0.42, 0.25) | −0.22(−0.47, 0.03) | −0.08(−0.35, 0.19) | |||
| Mother’s age (years) | ||||||
| 35–49 vs 24–34 | 0.16(−0.02, 0.34) | 0.12(−0.02, 0.26) | 0.15(−0.04, 0.33) | |||
| 50–73 vs 24–34 | −0.12(−1.17, 0.93) | 0.16(−0.32, 0.65) | 0.16(−0.31, 0.63) | |||
| Mother’s language preference (English vs Spanish) | 0.04(−0.29, 0.37) | −0.05(−0.26, 0.15) | 0.10(−0.21, 0.41) | |||
| Maternal marital status | ||||||
| Married/living with a partner vs single | −0.03(−0.28, 0.22) | 0.06(−0.11, 0.24) | 0.01(−0.23, 0.25) | |||
| Widowed, divorced or separated vs single | 0.09(−0.18, 0.36) | 0.06(−0.14, 0.27) | 0.13(−0.15, 0.41) | |||
| Maternal employment status (Yes vs No) | −0.03(−0.20, 0.15) | 0.11(−0.02, 0.25) | −0.06(−0.23, 0.12) | |||
| Mother born in mainland US (No vs Yes) | −0.01(−0.30, 0.28) | 0.07(−0.12, 0.27) | 0.08(−0.24, 0.40) | |||
HSHC/SOL maternal-report discrimination (2008–2011).
Note: BMI=body mass index; MetS = metabòlic syndrome score; hsCRP=high sensitivity C-reactive protein.
Contributor Information
Natalie Slopen, University of Maryland, College Park.
Garrett Strizich, Albert Einstein College of Medicine.
Simin Hua, Albert Einstein College of Medicine.
Linda C. Gallo, San Diego State University.
David H. Chae, Auburn University.
Naomi Priest, Australian National University.
Matthew J. Gurka, University of Florida.
Shrikant I. Bangdiwala, University of North Carolina at Chapel Hill
Julia I. Bravin, San Diego State University.
Earle C. Chambers, Albert Einstein College of Medicine.
Martha L. Daviglus, University of Illinois, Chicago.
Maria M. Llabre, University of Miami.
Mercedes R. Carnethon, Northwestern University.
Carmen R. Isasi, Albert Einstein College of Medicine.
REFERENCES
- 1.Camhi SM, Katzmarzyk PT. Tracking of cardiometabolic risk factor clustering from childhood to adulthood. Int J Pediatr Obes. 2010;5:122–9. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després J-P, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart Disease and Stroke Statistics—2016 Update. A Report From the American Heart Association. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Piña IL, Ramirez SM, Rodriguez B, Sims M. Status of Cardiovascular Disease and Stroke in Hispanics/Latinos in the United States: A Science Advisory From the American Heart Association. Circulation. 2014;130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW. Social Determinants of Risk and Outcomes for Cardiovascular Disease. A Scientific Statement From the American Heart Association. 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 5.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine. 2013;95:115–27. [DOI] [PubMed] [Google Scholar]
- 6.Williams DR, Mohammed SA. Racism and Health I: Pathways and Scientific Evidence. American Behavioral Scientist. 2013;57:1152–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umana-Taylor AJ, Updegraff KA. Latino adolescents’ mental health: exploring the interrelations among discrimination, ethnic identity, cultural orientation, self-esteem, and depressive symptoms. J Adolesc. 2007;30:549–67. [DOI] [PubMed] [Google Scholar]
- 8.Coll CG, Crnic K, Lamberty G, Wasik BH, Jenkins R, Garcia HV, McAdoo HP. An integrative model for the study of developmental competencies in minority children. Child development. 1996;67:1891–914. [PubMed] [Google Scholar]
- 9.Elder GH Jr. Time, human agency, and social change: Perspectives on the life course. Social psychology quarterly. 1994:4–15. [Google Scholar]
- 10.Evans GW, Li D, Sepanski Whipple S. Cumulative Risk and Child Development. Psychological Bulletin. 2013. [DOI] [PubMed] [Google Scholar]
- 11.Slopen N, Kubzansky LD, Koenen KC. Childhood adversity and inflammatory and immune biomarkers associated with cardiovascular risk in youth: a systematic review. Brain, Behavior, and Immunity. 2011;26:239–50. [DOI] [PubMed] [Google Scholar]
- 12.Slopen N, Goodman E, Koenen KC, Kubzansky LD. Socioeconomic and Other Social Stressors and Biomarkers of Cardiometabolic Risk in Youth: A Systematic Review of Less Studied Risk Factors. Plos One. 2013;8:e64418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heard-Garris N, Cale M, Camaj L, Hamati M, Dominguez T. Transmitting Trauma: A systematic review of vicarious racism and child health. Social Science & Medicine. 2017. [DOI] [PubMed] [Google Scholar]
- 14.Tran AG. Family contexts: parental experiences of discrimination and child mental health. Am J Community Psychol. 2014;53:37–46. [DOI] [PubMed] [Google Scholar]
- 15.Ford KR, Hurd NM, Jagers RJ, Sellers RM. Caregiver Experiences of Discrimination and African American Adolescents’ Psychological Health Over Time. Child Development. 2013;84:485–99. [DOI] [PubMed] [Google Scholar]
- 16.Gassman-Pines A Effects of Mexican Immigrant Parents’ Daily Workplace Discrimination on Child Behavior and Family Functioning. Child Development. 2015;86:1175–90. [DOI] [PubMed] [Google Scholar]
- 17.Espinoza G, Gonzales NA, Fuligni AJ. Parent Discrimination Predicts Mexican-American Adolescent Psychological Adjustment 1 Year Later. Child Dev. 2016;87:1079–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caughy MOB, O’Campo PJ, Muntaner C. Experiences of Racism Among African American Parents and the Mental Health of Their Preschool-Aged Children. American Journal of Public Health. 2004;94:2118–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bécares L, Nazroo J, Kelly Y. A longitudinal examination of maternal, family, and area-level experiences of racism on children’s socioemotional development: Patterns and possible explanations. Social Science & Medicine. 2015;142:128–35. [DOI] [PubMed] [Google Scholar]
- 20.Lorenzo-Blanco EI, Meca A, Piña-Watson B, Zamboanga BL, Szapocznik J, Cano MA, Cordova D, Unger JB, Romero A, Des Rosiers SE. Longitudinal Trajectories of Family Functioning Among Recent Immigrant Adolescents and Parents: Links With Adolescent and Parent Cultural Stress, Emotional Well-Being, and Behavioral Health. Child development. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lorenzo-Blanco EI, Meca A, Unger JB, Romero A, Gonzales-Backen M, Piña-Watson B, Cano MÁ, Zamboanga BL, Des Rosiers SE, Soto DW. Latino parent acculturation stress: Longitudinal effects on family functioning and youth emotional and behavioral health. Journal of Family Psychology. 2016;30:966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Priest N, Paradies Y, Stevens M, Bailie R. Exploring relationships between racism, housing and child illness in remote indigenous communities. Journal of Epidemiology and Community Health. 2010. [DOI] [PubMed] [Google Scholar]
- 23.Kelly Y, Becares L, Nazroo J. Associations between maternal experiences of racism and early child health and development: findings from the UK Millennium Cohort Study. Journal of Epidemiology and Community Health. 2013;67:35–41. [DOI] [PubMed] [Google Scholar]
- 24.Isasi CR, Parrinello CM, Ayala GX, Delamater AM, Perreira KM, Daviglus ML, Elder JP, Marchante AN, Bangdiwala SI, Van Horn L, Carnethon MR. Sex Differences in Cardiometabolic Risk Factors among Hispanic/Latino Youth. The Journal of Pediatrics. 2016;176:121–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isasi CR, Carnethon MR, Ayala GX, Arredondo E, Bangdiwala SI, Daviglus ML, Delamater AM, Eckfeldt JH, Perreira K, Himes JH. The Hispanic Community Children’s Health Study/Study of Latino Youth (SOL Youth): design, objectives, and procedures. Annals of epidemiology. 2014;24:29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LaVange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2010;20:642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Cassells A, Tobin JN, Sweeney M, Contrada RJ. The perceived ethnic discrimination questionnaire: Development and preliminary validation of a community version1. Journal of Applied Social Psychology. 2005;35:335–65. [Google Scholar]
- 28.DeBoer MD, Gurka MJ, Woo JG, Morrison JA. Severity of Metabolic Syndrome as a Predictor of Cardiovascular Disease Between Childhood and Adulthood. J Am Coll Cardiol. 2015;66:755–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gurka MJ, Ice CL, Sun SS, DeBoer MD. A confirmatory factor analysis of the metabolic syndrome in adolescents: an examination of sex and racial/ethnic differences. Cardiovascular Diabetology. [journal article]. 2012;11:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walker SE, Gurka MJ, Oliver MN, Johns DW, DeBoer MD. Racial/ethnic discrepancies in the metabolic syndrome begin in childhood and persist after adjustment for environmental factors. Nutrition, Metabolism and Cardiovascular Diseases. 2012;22:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen E, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 32.Wassertheil-Smoller S, Arredondo EM, Cai J, Castaneda SF, Choca JP, Gallo LC, Jung M, LaVange LM, Lee-Rey ET, Mosley T Jr. Depression, anxiety, antidepressant use, and cardiovascular disease among Hispanic men and women of different national backgrounds: results from the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology. 2014;24:822–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Juonala M, Viikari JSA, Ronnemaa T, Taittonen L, Marniemi J, Raitakari OT. Childhood C-reactive protein in predicting CRP and carotid intima-media thickness in adulthood - The Cardiovascular Risk in Young Finns Study. Arteriosclerosis Thrombosis and Vascular Biology. [Article]. 2006;26:1883–8. [DOI] [PubMed] [Google Scholar]
- 34.Jarvisalo MJ, Harmoinen A, Hakanen M, Paakunainen U, Viikari J, Hartiala J, Lehtimaki T, Simell O, Raitakari OT. Elevated serum C-reactive protein levels and early arterial changes in healthy children. Arteriosclerosis Thrombosis and Vascular Biology. 2002;22:1323–8. [DOI] [PubMed] [Google Scholar]
- 35.Tabák AG, Kivimäki M, Brunner EJ, Lowe GD, Jokela M, Akbaraly TN, Singh-Manoux A, Ferrie JE, Witte DR. Changes in C-reactive protein levels before type 2 diabetes and cardiovascular death: the Whitehall II study. European Journal of Endocrinology. 2010;163:89–95. [DOI] [PubMed] [Google Scholar]
- 36.Harrell JP, Hall S, Taliaferro J. Physiological Responses to Racism and Discrimination: An Assessment of the Evidence. American Journal of Public Health. 2003;93:243–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buckley TM, Schatzberg AF. On the Interactions of the Hypothalamic-Pituitary-Adrenal (HPA) Axis and Sleep: Normal HPA Axis Activity and Circadian Rhythm, Exemplary Sleep Disorders. The Journal of Clinical Endocrinology & Metabolism. 2005;90:3106–14. [DOI] [PubMed] [Google Scholar]
- 38.Goosby BJ, Malone S, Richardson EA, Cheadle JE, Williams DT. Perceived discrimination and markers of cardiovascular risk among low-income African American youth. American Journal of Human Biology. 2015:n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slopen N, Koenen KC, Kubzansky LD. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: a systematic review. Brain Behav Immun. 2012;26. [DOI] [PubMed] [Google Scholar]
- 40.Thayer ZM, Kuzawa CW. Ethnic discrimination predicts poor self-rated health and cortisol in pregnancy: Insights from New Zealand. Social Science & Medicine. 2015;128:36–42. [DOI] [PubMed] [Google Scholar]
- 41.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. American Journal of Public Health. 2000;90:1212–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Macgregor-Bowles I, Bowles DC. Trump, Brexit, Right-wing Anti-globalisation, and An Uncertain Future for Public Health. AIMS public health. 2017;4:139–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paluck EL, Green DP. Prejudice reduction: What works? A review and assessment of research and practice. Annual review of psychology. 2009;60:339–67. [DOI] [PubMed] [Google Scholar]
- 44.Devine PG, Forscher PS, Austin AJ, Cox WTL. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology. 2012;48:1267–78. [DOI] [PMC free article] [PubMed] [Google Scholar]