Abstract
Impairments in family functioning are associated with more severe depressive and manic symptoms, earlier recurrences, and more suicidal behaviors in early-onset bipolar disorder. This study examined whether family-focused treatment for adolescents (FFT-A) with BD I or II disorder led to greater increases in family cohesion and adaptability and decreases in conflict over 2 years compared to a briefer psychoeducational treatment (enhanced care, EC). Participants were 144 adolescents (mean age:15.6 ± 1.4 years) with BD I or II with a mood episode in the previous 3 months. Adolescents and parents were randomized to either FFT-A (21 sessions) or EC (three sessions). Patients received guideline-based pharmacotherapy throughout the 2-year study. Trajectories of adolescent- and parent-rated family cohesion, adaptability, and conflict were analyzed over 2 years. FFT-A had greater effects on adolescent-rated family cohesion compared to EC over 2 years. Participants in FFT-A and EC reported similar improvements in family conflict across the 2 years. In the FFT-A group, low-conflict families had greater adolescent-rated family cohesion throughout the study compared to high-conflict families. High-conflict families in both treatment groups tended to show larger reductions in conflict over 2 years than low-conflict families. Family psychoeducation and skills training may improve family cohesion in the early stages of BD. Measuring levels of family conflict at the start of treatment may inform treatment responsiveness among those receiving FFT-A.
Keywords: Bipolar Disorder, Cohesion, Adaptability, Family Functioning, Family-Focused Therapy, Adolescence, Mood Disorder
Family functioning is a critical prognostic variable for the course of major psychiatric disorders, such as bipolar disorder (BD), major depressive disorder, and schizophrenia. Impairments in family functioning, including low family cohesion (bonding and closeness), low adaptability (flexibility in response to change), and high levels of conflict (disagreements, arguments, fights), are associated with earlier illness onset, persistence and recurrence of mood and psychotic disorders, and suicidal behaviors among adults with schizophrenia, major depressive disorder, and BD (Keitner & Miller, 1990; Koutra et al., 2016; Miklowitz & Johnson, 2009).
For children and adolescents with BD, parent–child relationships are associated with less cohesion and adaptability, more conflict, and greater hostility compared to parent- child relationships in children with ADHD or healthy controls (Geller et al., 2000; Schenkel, West, Harral, Patel, & Pavuluri, 2008). These impairments in family functioning (e.g., parent- or adolescent-rated adaptability) are associated with a worse course of illness for early-onset BD including sustained depressive symptoms, earlier recurrences, more severe manic symptoms, and more suicidal ideation and behaviors (Ellis et al., 2014; Keenan-Miller, Peris, Axelson, Kowatch, & Miklowitz, 2012; Kim, Miklowitz, Biuckians, & Mullen, 2007; Schenkel et al., 2008; Sullivan, Judd, Axelson, & Miklowitz, 2012). More specifically, in children with BD, a measure of family conflict (i.e., power assertion) was associated with higher mania scores in a cross-sectional study (Schenkel et al., 2008). In a study of adolescents with BD, chronic stress in family relationships had stronger 1-year longitudinal associations with severity of mood symptoms (particularly depression) than either peer or academic stressors (Kim et al., 2007).
Conversely, adaptive family functioning has been shown to have a positive effect on outcomes for adolescents either at risk or already living with severe mental illness. Among adolescents at high risk for psychosis, positive communication and warmth from care-givers are associated with reductions in negative symptoms and improvements in social functioning (O’Brien et al., 2008). Children and adolescents with manic or mixed episodes who rate mothers as high in warmth were at lower risk of relapse over 24 months (Geller et al., 2002).
Interventions that reduce disturbances in cohesion, adaptability, and conflict, and increase the frequency of positive communication between adolescents and parents may have a beneficial impact on the course of psychiatric disorders in adolescents. Family-focused treatment for adolescents (FFT-A) is a manual-based, 9-month, 21-session treatment focusing on psychoeducation of BD, communication training, and problem-solving skills training. Primary analyses from the current trial examined whether pharmacotherapy plus FFT-A was more effective than pharmacotherapy plus EC in decreasing time to recovery from a mood episode (depressed, manic, mixed), increasing time to recurrence, and reducing symptom severity over the 2 years of the study. Results showed no differences between FFT-A and EC on time to recovery or recurrence, but found secondary effects of FFT-A on manic symptoms (Miklowitz et al., 2014). A follow-up study among these same adolescents with BD and their families found that parent-reported conflict prior to treatment moderated the treatment responses of families such that high-conflict families receiving FFT-A showed greater reductions in conflict over time compared to low-conflict families in FFT-A (Sullivan et al., 2012). Lastly, compared to a briefer psychoeducational treatment (enhanced care, EC), FFT was associated with an improvement in constructive communication and decreased conflictual behaviors during family interactions among adolescents and young adults at clinical high risk for psychosis (O’Brien et al., 2014). Thus, baseline levels of conflict may clarify which families are likely to benefit most from FFT-A.
The present study examines whether FFT-A, given in conjunction with guideline-based pharmacotherapy, is associated with increased levels of family cohesion and adaptability and lower levels of family conflict over 2 years in adolescents with bipolar I or II disorder and parents. We hypothesized that: (1) adolescents in FFT-A would report better family functioning over time than those in EC in cohesion, adaptability, and conflict; and (2) baseline family conflict would moderate the effects of FFT-A, with families reporting the highest levels of conflict showing the greatest changes in cohesion, adaptability, and conflict over time. We examined family functioning from the perspective of the adolescent and their primary caregiver.
METHODS
Overview
This randomized controlled trial was conducted in outpatient clinics in three locations: University of Colorado, Boulder, CO; University of Pittsburgh School of Medicine, Pittsburgh, PA; and the University of Cincinnati/Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA. Recruitment included inpatient and outpatient sources, print and online advertisement, public presentations, and referrals from community practitioners. This study was approved by the institutional review boards of all three universities. Parents, adolescent patients, and siblings gave written consent or assent to participate after receiving full explanations of the trial procedures.
Participants
Participants ranged from 12 years, 0 months, to 18 years, 1 month. All met DSM-IVTR criteria for a diagnosis of bipolar I or II disorder. The “Kiddie” Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime version (K-SADS-PL; Chambers, 1985; Kaufman et al., 1997) was the main diagnostic assessment used to determine diagnosis using consensus reports of the adolescent and at least one parent. In addition, participants had to meet DSM-IV-TR criteria for a mood episode in the previous 3 months (at least 2 weeks of syndromal depressive symptoms or one week of syndromal manic, hypomanic, or mixed symptoms, with significant impairment). Symptoms had to be of at least moderate severity for mania (≥17 on the K-SADS Mania Rating Scale; Axelson et al., 2003) or depression (≥16 on the K-SADS Depression Rating Scale; Chambers, 1985).
Study Procedures
Treatments
After the initial K-SADS-PL evaluation and a separate medical evaluation by a child psychiatrist, participants were randomly assigned in a 1:1 proportion to either pharmacotherapy plus FFT-A or pharmacotherapy plus EC, using a modified version of Efron’s biased coin toss, as administered by a data manager at the Pittsburgh site (Begg & Iglewicz, 1980). The groups were balanced at each study site by bipolar subtype (I and II) and mood state at study entry (depressed, manic/hypomanic, mixed).
All participants in both treatment conditions (FFT-A and EC) received pharmacotherapy throughout the 2-year course of the study. Pharmacotherapy was managed by board-certified psychiatrists using the algorithms of the Child Psychiatric Workgroup on Bipolar Disorder (Kowatch & DelBello, 2005) as supervised by expert child pharmacologists. All clinicians were trained in both FFT-A and EC during a 2-day pretrial workshop and received monthly group teleconference supervision during the trial. Treatment fidelity in both conditions was monitored using the Therapist Competency and Adherence Scales, Revised (TCAS-R; Marvin, Miklowitz, O’Brien, & Cannon, 2016). Interrater reliability for the TCAS was 0.84; mean overall fidelity scores did not differ significantly across sites, treatment conditions, or the interaction of sites with treatment conditions. Further study design details are given in a paper reporting the primary analyses from this trial (Miklowitz et al., 2014).
Family-focused therapy for adolescents
Family-focused treatment for adolescents included 21, 1-hour sessions over 9 months (12 weekly, 6 biweekly, and 3 monthly) with adolescents, their parents, and siblings. Clinicians administered the treatment in three phases: psychoeducation, communication training, and problem-solving skills training. During the psychoeducation component, clinicians acquainted adolescent patients and their family members with the signs and symptoms of BD most relevant to the adolescent such as depressive, manic, anxiety, and/or psychotic symptoms. The clinician reviewed the causes of BD (e.g., vulnerability–stress model) and illness management strategies most fitting for the adolescent including mood charting, medication adherence, sleep/wake cycle monitoring, identifying risk/protective factors, stress and coping strategies, and developing consistent sleep habits. Lastly, the psychoeducation component focused on identifying early warning signs of relapse and prevention planning (e.g., how and when to contact the physician for a medication change). The next component focused on communication training in which family members were encouraged to rehearse active listening with each other, request changes in one another’s behavior, provide positive feedback to each other, and offer constructive criticism about specific behaviors. This positive communication between family members (e.g., expressing positive feelings, making positive requests, active listening) promotes a sense of closeness and warmth (i.e., cohesion) between family members. In problem-solving training, clinicians helped families focus on defining specific problems (e.g., conflicts within the school or social environment), identifying and evaluating possible solutions, selecting preferred solutions, and developing plans to implement the selected solutions. While working together to resolve family conflicts, family members are encouraged to be flexible in their roles and responsibilities (adaptability) allowing for a more successful problem-solving within the family system. For more details on FFT-A, please see Miklowitz et al., 2014.
Enhanced care
Enhanced care consisted of 3-weekly, 1-hour sessions for the adolescent, parents, and siblings, conducted in the first month after randomization. This brief psychoeducation included several topics from the full FFT-A treatment (i.e., mood monitoring, identifying early warning signs of recurrence, developing strategies to prevent recurrence) presented in abbreviated form (see above for fidelity measurement).
Mood Measures
Mood severity
The Mania Rating Scale (MRS; Chambers, 1985) and Depression Rating Scale (Axelson et al., 2003) of the K-SADS-PL were used to assess mood severity. These clinician-rated measures consist of symptom items rated on 1–6 or 1–7 scales of severity, allowing for a fine-grained assessment of mood symptom severity and diagnostic clarification. Interrater reliabilities in the present study (intraclass rs), calculated across the three sites (12 K-SADS tapes rated by an average of 12 raters), were 0.89 for K-SADS Depression Rating Scale Scores and 0.81 for Mania Rating Scale scores.
To assess mood severity, an independent evaluator unaware of treatment assignments interviewed participants and at least one parent every 3 months during year 1 (with FFT-A sessions occurring between months 1–9 and EC sessions occurring during month 1) and every 6 months during year 2. Evaluators did not attend clinic meetings in which participants were discussed. If an evaluator became aware of a participant’s treatment condition, a new independent evaluator replaced him/her.
Family Functioning Measures
Family adaptability and cohesion evaluation scales
The Family Adaptability and Cohesion Evaluation Scale (FACES-II; Olson & Tiesel, 1991) is a 30-item, self-report measure completed by youths and their parents. Family behaviors are rated on a Likert scale from 1 (almost never) to 5 (almost always). The cohesion and adaptability subscales range from 15 to 70. Higher scores for each subscale reflect better family functioning. An example item from the cohesion subscale is “Family members feel very close to each other,” and an example item on the adaptability subscale is “When problems arise, we compromise.” The two subscales of cohesion and adaptability were computed for each participant and analyzed as separate dependent variables. Prior research has found that each subscale assesses a separate and important construct of family functioning (Place, Hulsmeier, Brownrigg, & Soulsby, 2005). In order to remain consistent with prior research reconciling single and dual-parent homes, the parent score was determined using the higher of the two scores. The mother was the primary reporter in 97% of the cases (Ellis et al., 2014). Higher scores indicate greater reported cohesion and adaptability. Therefore, the higher of the two scores represented the families’ best parent-rated score. For this study, Cronbach’s alpha was .77 for the FACES-II adolescent report and .74 for the parent report.
Conflict Behavior Questionnaire
The Conflict Behavior Questionnaire (CBQ) is a well-validated, 20-item, adolescent and parent self-report questionnaire that assesses the degree of negative communication and conflict within a family (Prinz, Foster, Kent, & O’Leary, 1979). Items on this instrument assessed argumentativeness, frustration in communication, degree of empathy for the child (or parent), and general relationship between the child and parent. The adolescent filled out a questionnaire regarding conflict with their primary caregiver, and one parent filled out the questionnaire regarding conflict with the adolescent. In two-parent families, we used the questionnaires completed by the parent who had the most daily contact with the child. For each scale item, participants indicated whether the statement is true or false. Sample items include “My mom screams a lot” and “My teenager often seems angry at me.” Responses are assigned a score of 0 or 1, dependent on whether or not the response reflects conflict; items are summed to generate a total conflict score (range: 0–20; higher scores indicate greater conflict). In this study, Cronbach’s alpha for the CBQ was 0.93 for parent scores and 0.93 for child (adolescent) scores.
Statistical Analyses
Analyses were conducted using IBM Statistical Package for the Social Sciences (SPSS22). Baseline descriptive statistics were calculated for demographic and illness history variables and compared across treatment groups. Family functioning scores from the adolescent and parent perspectives were examined separately. The Pearson correlations and t-tests were used to assess the relationships between baseline demographic/symptom variables (e.g., age, sex, and baseline Depression Rating Scale and Mania Rating Scale scores) and family functioning variables as measured by adolescent and parent report (i.e., FACES cohesion, FACES adaptability, and CBQ scores) over 24 months. Variables that were associated with family functioning scores were included as covariates in overall mixed-effect regression models.
We analyzed the 2-year trajectory of all family functioning scores (i.e., FACES cohesion, FACES adaptability, and the CBQ) in parents and separately adolescents as a function of treatment condition, time, and baseline levels of family conflict, using full-factorial mixed-effect regression models. Subject-level random intercepts were included to account for within-subject correlations induced by repeated measurements. Time was treated categorically across the study to allow for any higher-order, nonlinear trends throughout the 24-month period. The baseline assessment and every 6-month follow-up were included in the models (i.e., months 0, 6, 12, 18, and 24). For ease of interpretation, we dichotomized scores for baseline family conflict into high/low scores by using the mean split of the average of the adolescent-rated and parent-rated CBQ scores, such that each family was classified as high or low in conflict. Baseline family conflict was examined as a moderator of the effect of treatment, time, and their interaction on family functioning (e.g., the 2-way and 3-way interactions between baseline CBQ, time, and treatment group on family adaptability, cohesion, and conflict). Treatment site and baseline Depression Rating Scale and Mania Rating Scale scores were covaried in each model. When we observed significant effects of treatment, time, or their interaction, post hoc least square comparisons were conducted to determine the direction of effects.
To evaluate whether differential participant attrition between the treatment groups explained group differences in family functioning, we conducted ANOVAs comparing treatment groups subdivided by completer (24 months of participation) versus noncompleter (exited study prior to 24 months) status on baseline family functioning scores (FACES cohesion, FACES adaptability, and the CBQ). Chi-square tests were conducted to evaluate differential participant attrition between treatment groups during the active treatment phase (first 9 months) and at the last follow-up session. A chi-square test was also conducted to evaluate whether there were treatment group differences (FFT versus EC) in family adaptability, cohesion, and conflict between completers and noncompleters.
RESULTS
Baseline Demographics
A total of 145 adolescents and families participated in the trial (54 at Colorado, 44 at Pittsburgh, and 47 at Cincinnati). Of the 145, 1 did not complete any baseline or follow-up FACES-II or CBQ questionnaires (Figure 1). Of the 144, 76 met DSM-IV criteria for bipolar I disorder and 68 met criteria for bipolar II disorder (Table 1). The mean age was 15.6 (SD = 1.4) with 79 females and 65 males. There were no significant differences between treatment groups (FFT-A, EC) on baseline demographic variables (i.e., age, sex, race, ethnicity, SES), FACES-II adaptability scores (child and parent reports), cohesion scores (child and parent reports), or CBQ scores. None of the baseline demographic variables (i.e., sex, age, race, ethnicity, SES) nor baseline mood scores (DRS and MRS scores) were related to baseline family functioning variables.
Figure 1.
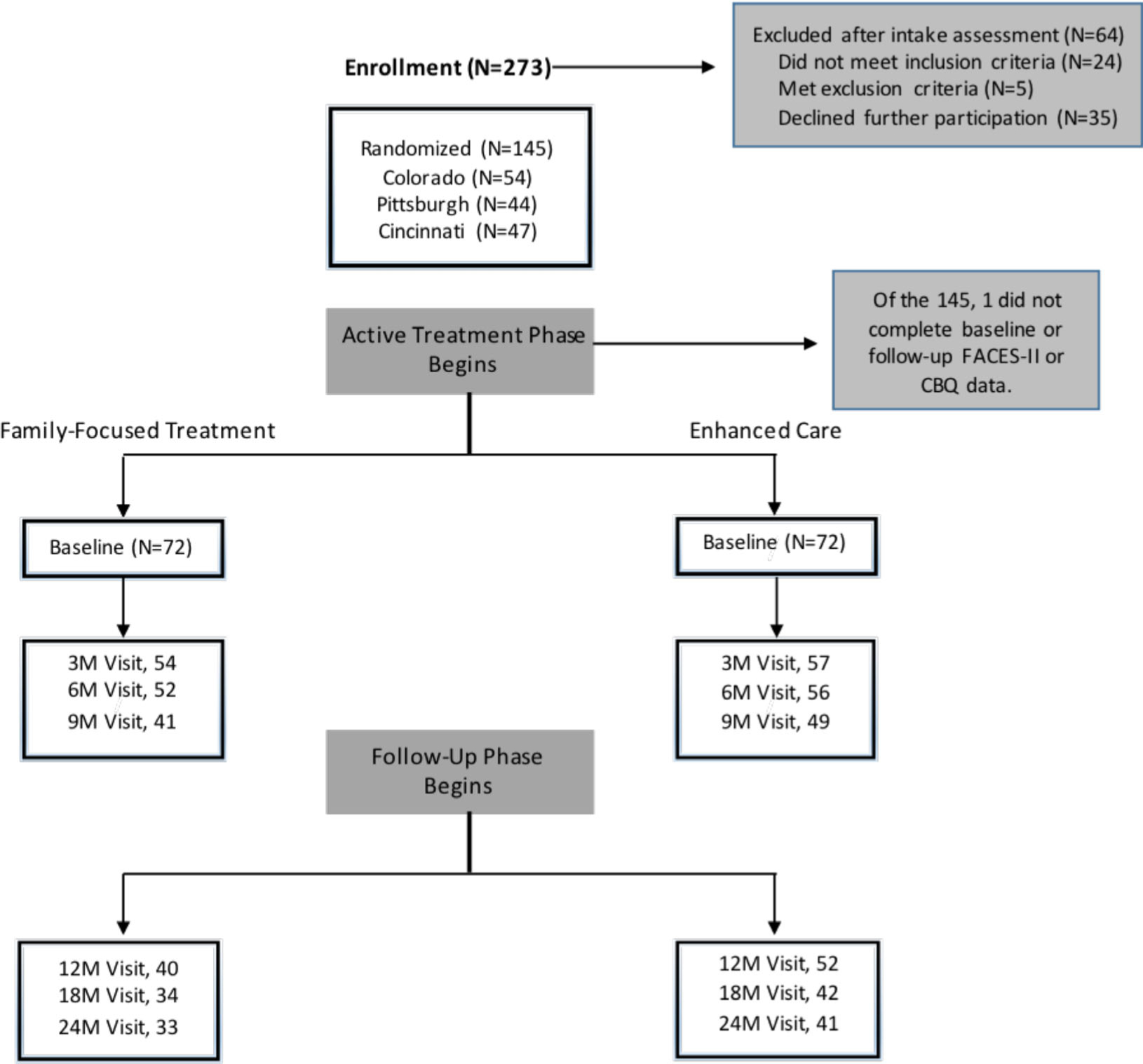
CONSORT Diagram. Two-Year Randomized Trial of Pharmacotherapy with Either Family-Focused Treatment (21 Sessions) or Enhanced Care (Three Sessions) in Adolescents with Bipolar I or II Disorder.
Table 1.
Demographics and Clinical Characteristics of Adolescents with Bipolar I and II Disorder
| Family-Focused Treatment (n = 72) | Enhanced Care (n = 72) | |
|---|---|---|
| Characteristics | n (%) | n (%) |
| Female | 36 (50) | 43 (59.7) |
| Bipolar subtype (bipolar II disorder) | 32 (44.4) | 36 (50) |
| Non-white | 12 (16.7) | 12 (16.7) |
| Hispanic | 7 (9.7) | 5 (6.9) |
| Lives with both biological parents | 23 (31.9) | 27 (37.5) |
| Current comorbid disorders | ||
| Anxiety disorder | 27 (37.5) | 30 (41.7) |
| Attention-deficit/hyperactivity disorder | 25 (34.7) | 23 (31.9) |
| Oppositional defiant or conduct disorder | 22 (30.6) | 20 (27.8) |
| Medications prescribed | ||
| Lithium | 13 (18.1) | 11 (15.3) |
| Anticonvulsants | 19 (26.4) | 14 (19.4) |
| Second-generation antipsychotics | 47 (65.3) | 44 (61.1) |
| Antidepressants | 17 (23.6) | 10 (13.9) |
| Mean ± SD | Mean ± SD | |
| Age | 15.5 ± 1.4 | 15.7 ± 1.5 |
| Socioeconomic status (class 1–5)a | 3.6 ± 1.3 | 3.7 ± 1.1 |
| Baseline Depression Rating Scale | 24.2 ± 10.7 | 26.9 ± 10.9 |
| Baseline mania rating score | 29.1 ± 12.0 | 28.1 ± 10.7 |
| CGAS most severe past | 40.6 ± 8.0 | 40.6 ± 7.8 |
| CGAS current | 47.8 ± 16.3 | 50 ± 4.9 |
Higher values indicate higher education and occupation; a value of three indicates middle class.
Treatment Sessions
There was not a significant difference between treatment groups for the number of pharmacotherapy visits during the trial (mean = 11.6, SD = 6.9). Across sites, participants in FFT-A attended a mean of 15.4-hour-long sessions (SD = 7.3), out of 21 expected protocol sessions. In the EC group, participants attended a mean of 2.5-hour-long sessions (SD = 1.1) of 3 protocol sessions. Of the participants randomized to FFT-A, 40% received ≥18 sessions, 18% received 10–17 sessions, 20% received one to nine sessions, and 22% received no sessions (dropped out following baseline interview). Among participants in the EC group, 79% received three sessions, 8% received one to two sessions, and 13% received no sessions.
Participant Attrition
The FFT-A and EC groups did not differ in the proportion of participants who dropped out of the study during the active treatment phase (first 9 months; 43% and 32%, respectively; χ2(1) = 2.25, p = .13). At the two-year follow-up, 54% of the FFT-A group remained in the study compared to 43% of the EC group, a nonsignificant difference (χ2(1) = 2.49, p = .12). There were no significant differences between participants completing the study (n = 71) versus exiting the study (n = 73) on FACES-II adaptability scores (child and parent reports), cohesion scores (child and parent reports), or CBQ scores (child and parent reports) obtained at baseline. However, participants who terminated early had higher baseline K-SADS Mania Rating Scale scores than those who were followed across the 2 years, F(1,143) = 5.57, p = .02. Participants who lived with one biological parent or in another living situation were more likely to terminate the study earlier (M = 77.0 weeks, SD = 35.9) than participants who lived with both biological parents (M = 92.2 weeks, SD = 28.3; F(1,121) = 6.07, p = .02).
Effects of Treatment on Family Functioning Scores over Time
Cohesion
There was no main effect of treatment group or time on adolescent-rated cohesion scores; however, there was a significant interaction between treatment group and time on adolescent-rated cohesion, F(4,223) = 2.53, p = .04. Follow-up pairwise analyses revealed adolescents’ cohesion in the FFT group improved to significantly higher levels during the 12- to 18-month trajectory compared to adolescents in the EC group, F(1,265) = 4.80, p = .03. There were no significant differences between treatment groups during the 18- to 24-month trajectory.
Baseline conflict also moderated the effect of treatment group on adolescent-rated cohesion scores, F(1,107) = 6.38, p = .01. In the FFT-A group, the low-conflict families had greater adolescent-rated family cohesion throughout the study compared to the high-conflict families, F(1,112) = 4.61, p = .03. In the EC group, there was no difference between high- versus low-conflict families on adolescent-rated family cohesion. Baseline conflict did not interact with time, nor was there a three-way interaction between treatment condition, time, and baseline conflict on adolescent-rated cohesion.
There were no main effects or interactive effects of treatment group or time on parent-rated cohesion. Baseline conflict negatively predicted parent-rated cohesion throughout the course of the study, F(1,100) = 5.87, p = .02; however, baseline conflict did not interact with treatment group or time on parent-rated cohesion (see Figure 2).
Figure 2.
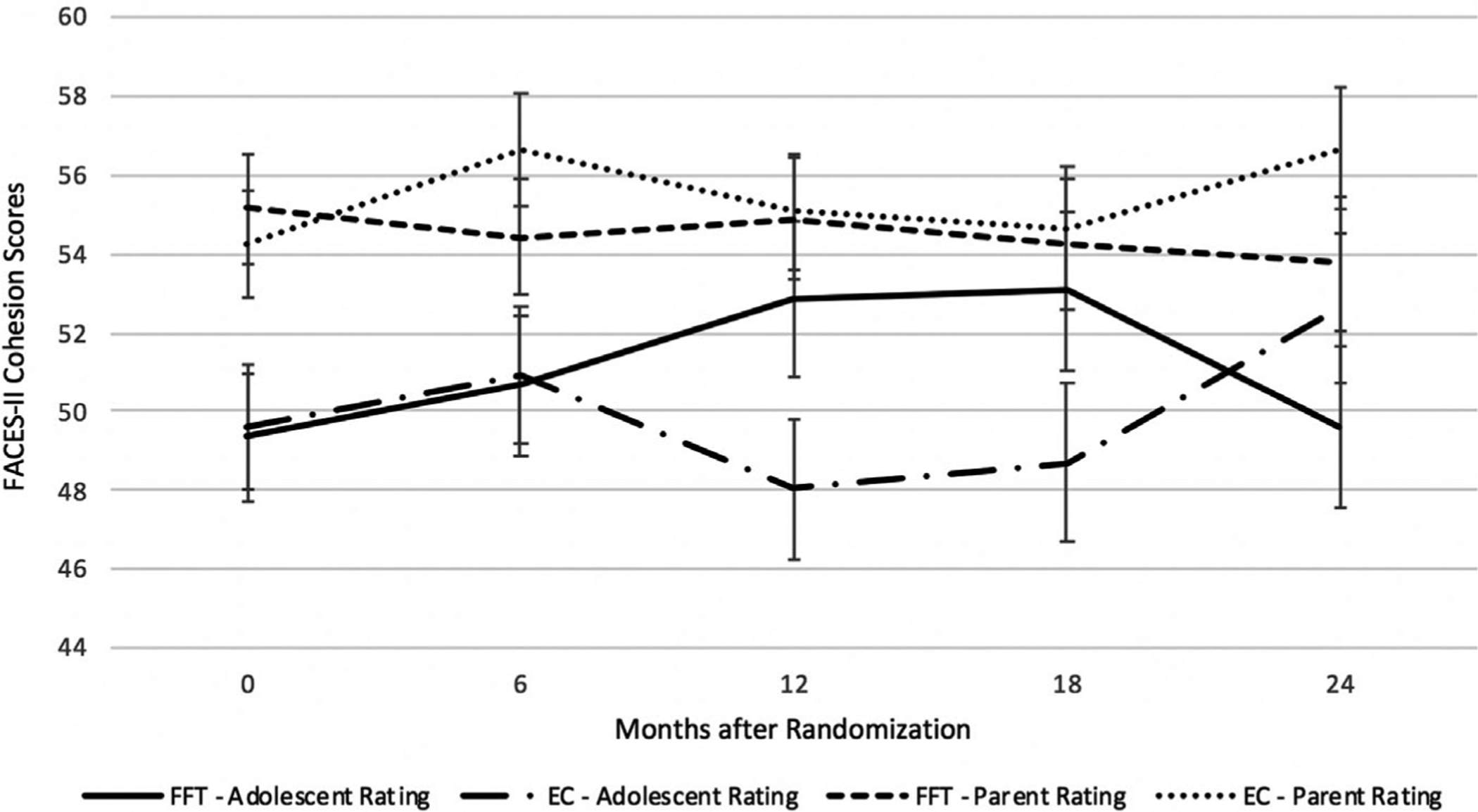
Comparing Family-Focused Treatment and Enhanced Care on Mean Cohesion Scores Across 2 Years. FACES-II Cohesion Scores: Estimated Predicted Means and Standard Errors of the Estimated Means. Months After Randomization.
Adaptability
There was no effect of treatment condition, time, or their interaction on adolescent-rated adaptability. However, there was a 3-way interaction between baseline family conflict, treatment condition, and time on adolescent-rated adaptability scores, F(1,109) = 5.28, p = .02. In the FFT-A group, low-conflict families had higher adolescent-rated adaptability scores over 24 months compared to high-conflict families, F(1,112) = 5.74, p = .018. In the EC group, there was no difference between high- versus low-conflict families in adaptability scores. Baseline conflict did not interact with time or with treatment and time on adolescent-rated adaptability scores.
There was no effect of treatment group on parent-rated family adaptability scores. However, parent-rated adaptability scores increased (indicating greater adaptability) over the course of the study in both treatment groups, F(4,230) = 3.55, p = .008. Baseline conflict was negatively related to parent-rated adaptability scores, indicating that high baseline conflict predicted reduced adaptability throughout the study, F(1,100) = 11.70, p = .001. There were no interactions between predictors of parent-rated adaptability (see Figure 3).
Figure 3.
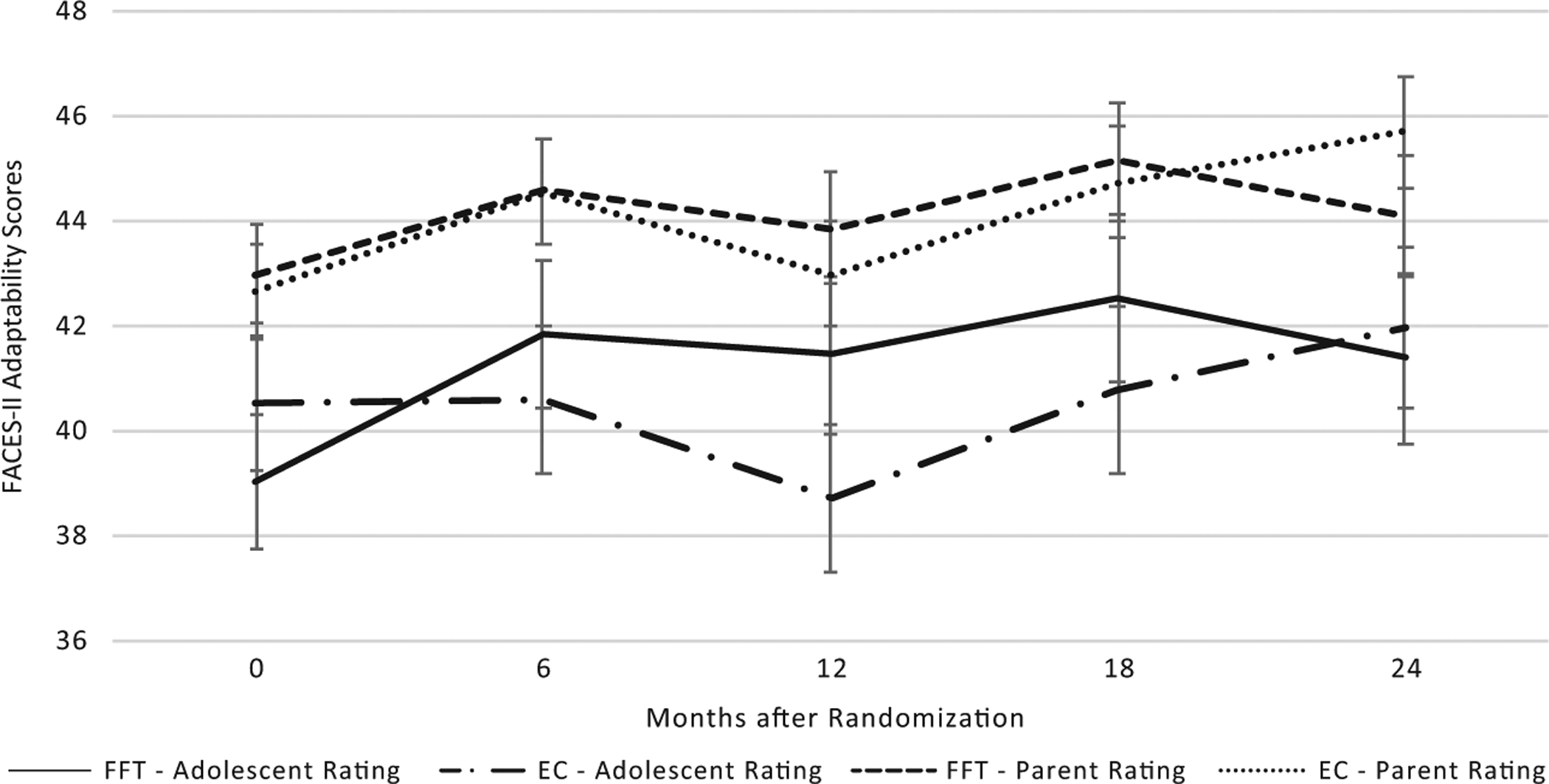
Comparing Family-Focused Treatment and Enhanced Care on Mean Adaptability Scores Across 2 Years.
Conflict
There was no effect of treatment group, time, or their interaction on adolescent-rated family conflict. Higher baseline levels of overall family conflict were associated with higher adolescent-rated conflict scores over the course of the study, F(1,107) = 7.15, p = .008. Baseline family conflict also moderated the effect of time on adolescent-rated cohesion at a marginally significant level, F(4,247) = 2.05, p = .09, which indicated that, despite having higher conflict throughout the study, the high-conflict families also showed greater improvements in adolescent-rated conflict over the course of the study compared to low-conflict families. Baseline conflict did not interact with treatment group or treatment group by time in predicting adolescent-rated conflict scores.
There was no effect of treatment group on parent-rated family conflict. However, in both groups, parent-rated conflict decreased at every time point compared to the baseline measurement over the course of the study, F(4,258) = 15.71, p < .001. There was no interaction between treatment group and time on parent-rated family conflict. Baseline family conflict was positively associated with parent-rated conflict throughout the course of the study such that high baseline conflict predicted greater conflict, F(1,107) = 7.15, p = .008. Additionally, baseline conflict moderated the effect of time on parent-rated conflict scores at a marginally significant level, F(4,259) = 2.23, p = .07, which indicated that the high-conflict families, although maintaining higher conflict throughout the study, also showed greater reductions in conflict over the course of the study compared to low-conflict families. Baseline conflict did not interact with treatment condition or treatment by time on parent-rated conflict scores (see Figure 4).
Figure 4.
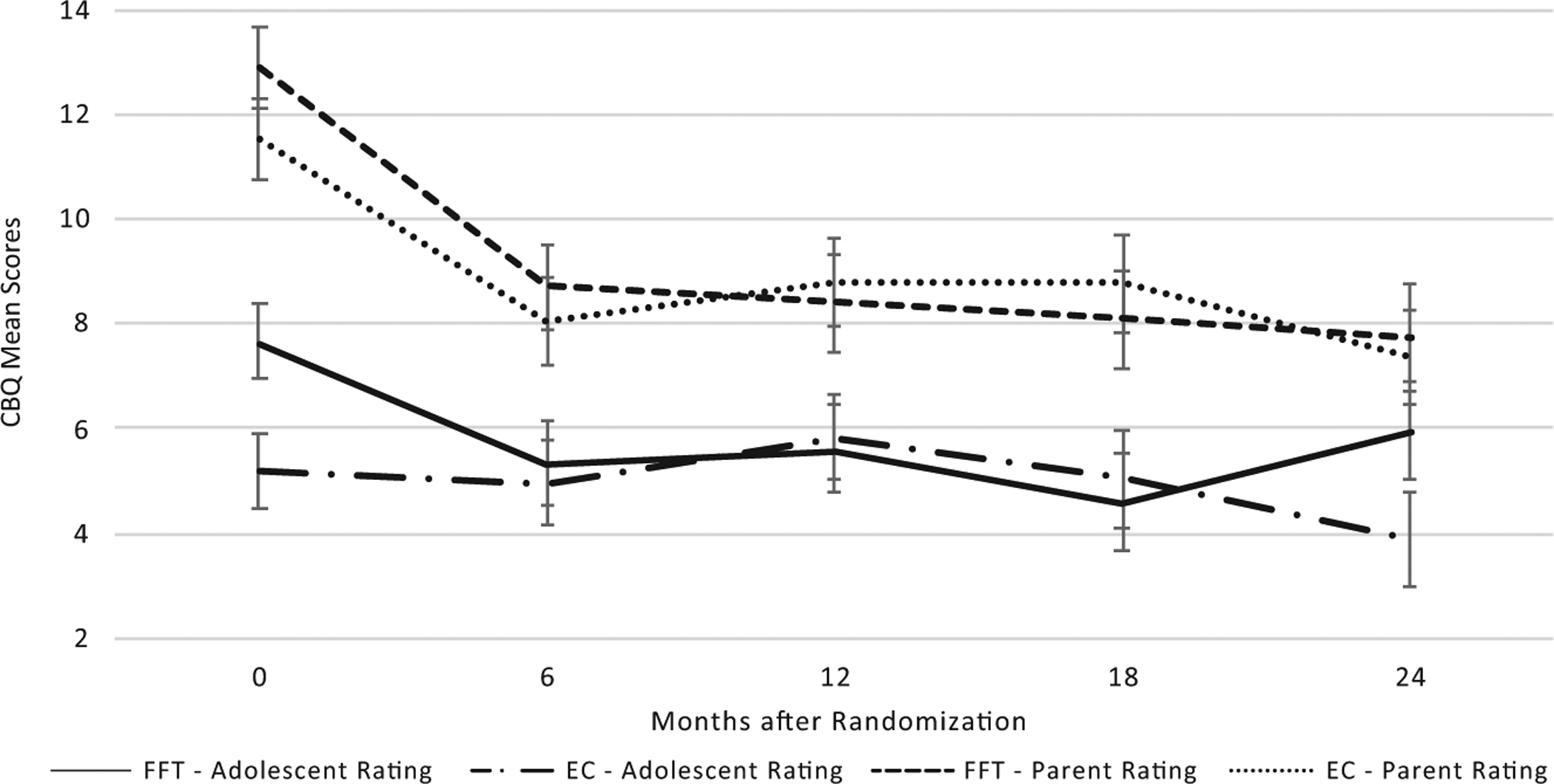
Comparing Family-Focused Treatment and Enhanced Care on Mean Conflict Scores Across 2 Years.
DISCUSSION
This study examined the effects of two psychosocial interventions on family functioning (cohesion, adaptability, conflict) among families of adolescents with bipolar I or II disorder, and the moderating effects of baseline conflict on these family outcomes. Both treatments targeted family environments and were psychoeducational in approach; however, the FFT-A was longer (21 sessions) and included skills training modules focused on communication and problem-solving. The EC condition was intended to reflect the level of educational input that families often receive in community clinic settings: three information-oriented sessions about mood symptoms, recognition of prodromal signs, and relapse prevention planning.
Adolescents randomized to the FFT-A group reported greater improvements in family cohesion compared to the EC group. Although FFT-A was not designed to directly target cohesion and make family members more interdependent, certain skills introduced in this treatment may enhance this dimension of family functioning. Beyond psychoeducation, FFT-A introduces skills that encourage positive communication between family members (e.g., expressing positive feelings, making positive requests, active listening) and working together to resolve family conflicts. These skill training tasks in FFT-A may promote a sense of closeness and warmth (i.e., cohesion) between family members. Prior studies have found associations between greater family cohesion and illness course (i.e., shorter depressive episodes, lower relapse rates, better social functioning) in those with BD (Keenan-Miller et al., 2012; Kim et al., 2007; Schenkel et al., 2008; Sullivan et al., 2012). Research examining whether cohesion mediates the relationship between family intervention and key outcome variables (e.g., course of illness, quality of life) measured over time may suggest the importance of cohesion as a treatment target for adolescents with severe mental illness. Currently, no family psychoeducational interventions explicitly target cohesion.
Family-focused treatment for adolescents and EC did not differentially affect conflict, which decreased from pre- to post-treatment in both conditions. It is possible that the decrease in conflict observed in both treatment groups occurred independently of any effects of the interventions. We were also surprised that youth in the lengthier FFT-A did not differ from those in EC on symptomatic outcomes until the second year of study follow-up (Miklowitz et al., 2014). There are adolescents with BD who appear to respond very quickly once entering an integrated treatment program, possibly due to immediate medication effects or the reduction in distress about mood symptoms that may be a by-product of family education. Families may react positively to the patient’s improvement from being acutely symptomatic at baseline to remitted or only subthreshold at follow-up (Miklowitz et al., 2014). These early responders may show most of their clinical benefits early in the follow-up, and not during the lengthier interval of the full FFT treatment. Future studies may be able to characterize early responders who do equally well with these two treatments of different intensities.
Another possibility is that the three sessions of EC were just as effective in reducing levels of conflict as the 21 sessions of FFT-A, although this is not supported in studies that look at conflict in direct observation tasks (O’Brien et al., 2014; Sullivan et al., 2012). Finally, the CBQ, a self-report measure of conflict, may not adequately measure negative exchanges that persist even if they do not always lead to arguments. Additionally, capturing the frequency of positive communication in the context of negative exchanges may require direct observation of family interactions rather than self-report measures.
Families that began the study with high conflict trended toward greater reductions in conflict over time compared to those who began with low conflict, regardless of treatment assignment. Prior research examining adolescents with BD and their families also found that high-conflict families demonstrated significantly greater decreases in conflict over time compared to low-conflict families (Sullivan et al., 2012). Together, these results indicate that placing a greater emphasis on effectively resolving family conflicts during the treatment process may result in greater improvements in overall family functioning over time.
A secondary finding was that levels of baseline conflict moderated the effects of treatment group on adolescent-rated cohesion and adaptability scores. Families low in conflict may already possess strengths in communication and problem-solving skills that become further enhanced during FFT-A, resulting in a greater sense of emotional bonding and closeness between family members (cohesion) and greater flexibility of a family system (adaptability).
It is worth noting that variability in cohesion, adaptability, and conflict were not related to initial symptom states, as baseline mood was controlled in these analyses. Prior results from this trial also found that the effects of treatment on quality of life were independent of baseline mood symptoms (O’Donnell et al., 2017). The large-scale STEP-BD (Systematic Treatment Enhancement Program for Bipolar Disorder) study of adults with BD indicated that FFT, interpersonal and social rhythm therapy, and cognitive–behavioral therapy each had a greater effect on relationship functioning than brief psychoeducational therapy over 1 year, even when controlling for concurrent depressive symptoms (Keenan-Miller et al., 2012; Kim et al., 2007; Schenkel et al., 2008; Sullivan et al., 2012). Future research that allocates adolescents with BD and their families to treatment conditions based on their baseline mood episode (i.e., currently depressed, manic, or mixed) may clarify whether the effects of psychosocial interventions vary according to the polarity of the index study episode.
Limitations
All families in this study were seeking treatment for their adolescents with BD. Therefore, the results may not generalize to families who are less motivated for psychosocial treatment. In addition, the sample was primarily Caucasian and from middle- to upper-class homes. Results may not generalize to families that experience sociocultural challenges (e.g., transportation challenges, differences between generations in levels of acculturation) that affect perceptions of the family, treatment engagement, or treatment responsiveness.
Self-report measures are often chosen over observational, clinician-rated measures due to their ease of use and versatility in various environments (in-person, online). However, the self-report measures used in this study, FACES-II and CBQ, may not have been sensitive enough to capture important changes in family relationships. When using observational measures of family interactions, prior research has found that FFT is associated with improvements in constructive communication and decreases in conflict in families with adolescents or young adults at high risk for psychosis (O’Brien et al., 2014) and enhanced family or spousal communication in families with adults with bipolar disorder (Simoneau, Miklowitz, Richards, Saleem, & George, 1999).
This study did not standardize medication choices or dosage plans, and it is conceivable that medications influenced the family functioning scores (FACES-II, CBQ) from adolescents or parents in one treatment group more than the other. It is also possible that the observed improvements in family cohesion in the FFT-A group were related to the greater number of sessions offered to families compared to the EC group. Future studies comparing FFT-A to treatments of similar frequency and duration would help to clarify this concern.
The attrition rates in FFT-A (43%) and the EC group (32%) during the 9-month active treatment phase are consistent with prior rates observed in family therapy studies, which range from 40 to 60% in meta-analyses (Wierzbicki & Pekarik, 1993). Further research is needed to identify factors associated with attrition in FFT-A and similar family treatment models for adolescents with severe mental illness.
CONCLUSIONS
Results highlight the impact of offering family-focused psychoeducation and skills training in the early stages of BD to improve family functioning. Accounting for family characteristics such as conflict, cohesion, and adaptability at the start of psychosocial or medical treatments may inform treatment responsiveness.
Acknowledgments
Financial support was provided by the National Institute of Mental Health (NIMH) grants R01 MH073871 and R34MH077856 to Dr. Miklowitz, grant R01MH073817 to Dr. Axelson, and grant R01MH074033 to Dr. Kowatch. The sponsors named above did not have any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
The authors thank Adrine Biuckians, Ph.D., University of Colorado, Boulder; Jedediah Bopp, Ph.D., University of Colorado, Boulder; Victoria Cosgrove, Ph.D., Stanford University School of Medicine; L. Miriam Dickinson, Ph.D., University of Colorado, Boulder; Dana Elkun, M.A., M.F.A., University of Colorado, Boulder; Elizabeth George, Ph.D., University of Colorado, Boulder; Jessica Lunsford-Avery, Ph.D., Duke University School of Medicine; Chris Hawkey, M.A., University of Colorado, Boulder; Zachary Millman, B.A., University of Maryland, Baltimore Country; Aimee Sullivan, Ph.D., University of Colorado, Boulder; Dawn Taylor, Ph.D., University of Colorado, Boulder; Marianne Wamboldt, M.D., University of Colorado; Boris Birmaher, M.D., University of Pittsburgh School of Medicine; and Melissa DelBello, M.D., University of Cincinnati Academic Health Center for their assistance.
This study is registered at http://clinicaltrials.gov identifier: NCT00332098.
Drs. O’Donnell, Ellis, Weintraub, and Axelson have none to declare. Dr. Kowatch is a consultant and faculty for the REACH Institute. He is a consultant for data safety committees for Forest and Pfizer. He is employed by the Ohio State Wexner Medical Center. Dr. Schneck has received research support from NIMH and the Ryan White HIV/AIDS Treatment Extension Act. Dr. Miklowitz has received research funding from the National Institute of Mental Health, Brain and Behavior Research Foundation, Attias Family Foundation, Danny Alberts Foundation, Carl and Roberta Deutsch Foundation, Kayne Family Foundation, Max Gray Foundation, and the American Foundation for Suicide Prevention, and book royalties from Guilford Press and John Wiley & Sons.
REFERENCES
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J et al. (2003). A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology, 13(4), 463–470. 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Begg CB, & Iglewicz B (1980). A treatment allocation procedure for sequential clinical trials. Biometrics, 36 (1), 81 10.2307/2530497. [DOI] [PubMed] [Google Scholar]
- Chambers WJ (1985). The assessment of affective disorders in children and adolescents by semistructured interview: Test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of General Psychiatry, 42(7), 696 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Ellis AJ, Portnoff LC, Axelson DA, Kowatch RA, Walshaw P, & Miklowitz DJ (2014). Parental expressed emotion and suicidal ideation in adolescents with bipolar disorder. Psychiatry Research, 216(2), 213–216. 10.1016/j.psychres.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Bolhofner K, Craney JL, Williams M, DelBello MP, & Gundersen K (2000). Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. Journal of the American Academy of Child & Adolescent Psychiatry, 39(12), 1543–1548. [DOI] [PubMed] [Google Scholar]
- Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, & Zimerman B (2002). Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. American Journal of Psychiatry, 159(6), 927–933. 10.1176/appi.ajp.159.6.927. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Peris T, Axelson D, Kowatch RA, & Miklowitz DJ (2012). Family functioning, social impairment, and symptoms among adolescents with bipolar disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(10), 1085–1094. 10.1016/j.jaac.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keitner GI, & Miller IW (1990). Family functioning and major depression: An overview. American Journal of Psychiatry, 147(9), 1128–1137. 10.1176/ajp.147.9.1128. [DOI] [PubMed] [Google Scholar]
- Kim EY, Miklowitz DJ, Biuckians A, & Mullen K (2007). Life stress and the course of early-onset bipolar disorder. Journal of Affective Disorders, 99(1–3), 37–44. 10.1016/j.jad.2006.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutra K, Triliva S, Roumeliotaki T, Basta M, Lionis C, & Vgontzas AN (2016). Family functioning in first-episode and chronic psychosis: The role of patient’s symptom severity and psychosocial functioning. Community Mental Health Journal, 52(6), 710–723. 10.1007/s10597-015-9916-y. [DOI] [PubMed] [Google Scholar]
- Kowatch RA, & DelBello MP (2005). Pharmacotherapy of children and adolescents with bipolar disorder. Psychiatric Clinics, 28(2), 385–397. 10.1016/j.psc.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Marvin SE, Miklowitz DJ, O’Brien MP et al. (2016). Family-focused therapy for individuals at clinical high risk for psychosis: Treatment fidelity within a multisite randomized trial. Early Intervention in Psychiatry, 10 (2), 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, & Johnson BSL (2009). Social and Familial factors in the course of bipolar disorder: Basic processes and relevant interventions. Clinical Psychology: Science and Practice, 16(2), 281–296. 10.1111/j.1468-2850.2009.01166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, George EL, Taylor DO, Sugar CA, Birmaher B et al. (2014). Pharmacotherapy and family-focused treatment for adolescents with bipolar I and II disorders: A 2-year randomized trial. The American Journal of Psychiatry, 171(6), 658–667. 10.1176/appi.ajp.2014.13081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, Candan KA, Marshall C, Domingues I, Walsh BC et al. (2014). A randomized trial of family focused therapy with populations at clinical high risk for psychosis: Effects on interactional behavior. Journal of Consulting and Clinical Psychology, 82(1), 90–101. 10.1037/a0034667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Zinberg JL, Bearden CE, Lopez SR, Kopelowicz A, Daley M et al. (2008). Parent attitudes and parent adolescent interaction in families of youth at risk for psychosis and with recent-onset psychotic symptoms: Parent adolescent interaction in family of at-risk youth. Early Intervention in Psychiatry, 2(4), 268–276. 10.1111/j.1751-7893.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- O’Donnell LA, Axelson DA, Schneck CD, Kowatch RA, Sugar CA, & Miklowitz DJ (2017). Enhancing quality of life among adolescents with bipolar disorder: A randomized trial of two psychosocial interventions. Journal of Affective Disorders, 219, 201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson DH, & Tiesel J (1991). FACES II: Linear Scoring and Interpretation. Minneapolis, MN: Life Innovations, Family Inventories Project. [Google Scholar]
- Place M, Hulsmeier J, Brownrigg A, & Soulsby A (2005). The family adaptability and cohesion evaluation scale (FACES): An instrument worthy of rehabilitation? Psychiatric Bulletin, 29(06), 215–218. 10.1192/pb.29.6.215. [DOI] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, & O’Leary KD (1979). Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis, 12(4), 691–700. 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenkel LS, West AE, Harral EM, Patel NB, & Pavuluri MN (2008). Parent–child interactions in pediatric bipolar disorder. Journal of Clinical Psychology, 64(4), 422–437. 10.1002/jclp.20470. [DOI] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Richards JA, Saleem R, & George EL (1999). Bipolar disorder and family communication: Effects of a psychoeducational treatment program. Journal of Abnormal Psychology, 108(4), 588. [DOI] [PubMed] [Google Scholar]
- Sullivan AE, Judd CM, Axelson DA, & Miklowitz DJ (2012). Family functioning and the course of adolescent bipolar disorder. Behavior Therapy, 43(4), 837–847. 10.1016/j.beth.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierzbicki M, & Pekarik G (1993). A meta-analysis of psychotherapy dropout. Professional Psychology: Research and Practice, 24(2), 190–195. 10.1037/0735-7028.24.2.190. [DOI] [Google Scholar]


