Abstract
Marijuana use among older adults is on an unprecedented rise, yet little is known about its effects on cognition in this population where, due to advanced age, risk for cognitive decline is high. Thus, we investigated whether marijuana use and use characteristics were associated with self-reported cognition among older adults ages ≥ 50 years using the National Epidemiologic Survey on Alcohol and Related Conditions-III. Respondents either had never used marijuana (“never”: n=10,976), used but not in the past 12 months (“former”: n=2,990), or used in the past 12 months (“current”: n=712). Self-reported cognition was measured using the Executive Function Index. Marijuana and substance use characteristics were obtained using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5. Covariates included demographics, mental health and disability, and comorbid mental and substance use disorder. Using general linear models of cross-sectional data, we found that current users, particularly those with cannabis use disorder, reported worse cognition than never or former users, but these effects were small in magnitude. Among both former and current users, greater duration of past use was associated with worse cognition. Frequent use within the past 12 months was associated worse cognition among current users, but daily users reported better cognition compared to monthly or weekly users. Thus, marijuana use may impact self-reported cognition in older adulthood, although these effects may be subtle, specific to particular use characteristics, and possibly affected by self-awareness of deficits. Future work using objective measures such as neuropsychological testing or neuroimaging may better elucidate these effects.
Keywords: Older adults, aging, cognition, executive function, marijuana, cannabis
1. INTRODUCTION
Marijuana use among persons ages 50 and older is on an unprecedented rise (Colliver et al., 2006). From 2006 to 2013, past-year marijuana use increased by 57.8% in adults ages 50–64 and by 250% in those aged 65 and older (Han et al., 2017). More recently, survey data from 2015 to 2016 estimates that 9.0% of adults ages 50–64 and 2.9% of adults ages 65 and older have used marijuana in the past year (Han & Palamar, 2018), making older adults one of the fastest growing usage groups upon which to focus further research (Burggren et al., 2019). Various explanations have been offered to account for these trends, primarily cohort effects, legalization, and perceived safety and tolerability of marijuana for recreational use or as a treatment for a variety of conditions in lieu of, or as an adjunct to, prescription medications (Abuhasira et al., 2018; Salas-Wright et al., 2017).
Despite these trends, there is limited data on the impact of marijuana use in older adults (Briscoe & Casarett, 2018; van den Elsen et al., 2014). It is unknown whether the potential benefits outweigh the risks of addiction, incident disease, or exacerbations of the disease for which marijuana presumably provides symptom relief. One particular risk for which older adults are especially vulnerable is cognitive decline (Alzheimer’s Association, 2019). In adolescence/young adulthood, marijuana use has been associated with adverse effects on cognition and brain structure (Broyd et al., 2016; Cohen & Weinstein, 2018; Gonzalez et al., 2017; Nader & Sanchez, 2018). However, there is some inconsistent evidence (Gillespie et al., 2018; Thayer et al., 2017), including findings of small effects when deficits are found as well as deficit resolution following abstinence (Scott et al., 2018). It is therefore unsurprising that preliminary findings in older adults are also mixed. Compared to controls, abstinent older adults with heavy cannabis use histories exhibited thinner hippocampal subfields in one study (Burggren et al., 2018) whereas in another study current users demonstrated no adverse loss in brain volumes (Thayer et al., 2019). Both studies showed no significant differences in cognition between the marijuana users and non-users. In contrast, studies using rodent models of aging and Alzheimer’s disease have shown the restorative effects of tetrahydrocannabinol, the principal psychoactive constituent of cannabis, on cognition (Aso et al., 2016; Bilkei-Gorzo et al., 2017; Sarne et al., 2018).
Despite these intriguing, albeit mixed, findings, there have been no prior population-based investigations of the relationship between marijuana use and cognition in aging with which to inform more systematic investigations. Thus, the goal of this study was to test whether marijuana use was associated with self-reported cognition in adults ages ≥ 50 using data from a nationally representative survey. We hypothesized that current users would report more cognitive difficulties than individuals who had never used or who had used marijuana only prior to the last 12 months. Furthermore, we expected that self-reported cognition would be associated with marijuana use characteristics among current and former users, over and above variables that influence self-reported cognition such as demographics, concurrent mental health, disability, or disorder, and other substance use. These findings are anticipated to have implications for public policy and subsequent investigations of causality.
2. MATERIALS AND METHODS
2.1. Design and Participants
This cross-sectional study uses data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) whose target population is the noninstitutionalized, civilian population 18 years or older living in the US, including persons residing in noninstitutionalized group quarters. Subjects provided written informed consent after receiving a complete description of the study. As detailed elsewhere (Grant et al., 2014; Grant, Goldstein, Saha, et al., 2015), multistage probability sampling was used to randomly select persons within sampling units from April 2012 to June 2013. Data were adjusted for oversampling and non-response, then weighted to represent the US civilian population.
Data were requested, received, and analyzed by the authors from October 2017 to February 2020. Respondents were asked about medical marijuana use and recreational marijuana use separately. For the former, only whether or not the respondent had ever used medical marijuana within the past 12 months or prior was queried, whereas for the latter much more extensive follow-up questions regarding marijuana use patterns were asked. The vast majority of respondents ages ≥ 50 who had ever used marijuana did not endorse ever having used medical marijuana (i.e. 3,505 of 3,702 ever users or 95.5%). However, we included all marijuana users in our analyses given that there is little NESARC-III data to distinguish medical from marijuana use in addition to recent evidence indicating that more than half of medical marijuana users also use marijuana recreationally (Morean & Lederman, 2019). These data therefore include 14,678 respondents ages who endorsed: a) no lifetime marijuana use (“never”, n=10,976), b) past recreational or medical marijuana use but no use in the past 12 months (“former”, n=2,990, including 2,934 who had only used recreationally, 35 who reported both recreational and medical marijuana use, and 21 who used medical marijuana only), and c) current use within the past 12 months (“current”, n=712, including 597 who report recreational use only within the past 12 months and prior, 94 who report both recreational and marijuana use within the past 12 months and prior, 12 who report medical marijuana use only within the past 12 months and prior, 5 who report medical marijuana use only within the past 12 months and not prior, and 4 who report recreational use only in the past 12 months and not prior).
2.2. Measures
2.2.1. Primary Outcomes: The Executive Function Index (EFI) scales
The EFI is composed of 12 items querying self-reported cognitive functioning for use in community surveys (Spinella, 2005). Respondents were asked to rate each self-statement as not at all, a little, somewhat, a lot, or very much descriptive of him or herself. Responses were coded 0 to 4, with higher values indicating better functioning. Collected as part of NESARC-III (Aharonovich et al., 2017), the EFI has acceptable reliability and validity, with two subscales (executive functions [4 items] and attention [5 items] and a total score.
2.2.2. Predictors: Marijuana Use Characteristics
Marijuana use prior to the past 12 months was characterized by: age at first use, age began using most frequently, frequency of most use (binned to approximate yearly, monthly, weekly, and daily use), duration of period of most frequent use (in years), and number of joints usually smoked in a single day during period of most frequent use. Current marijuana use was characterized by: frequency of use over the past year (binned as above), last time used, number of joints usually smoked in a single day, and meeting criteria for cannabis use disorder (CUD).
2.2.3. Covariates
Demographics.
Four variables were selected as covariates given their influence on assessments of cognitive functioning: age, sex, race/ethnicity, and education (Alzheimer’s Association, 2019; Early et al., 2013).
The 12-item Short-Form Health Survey (SF-12).
The SF-12, version 2, is a measure of current disability including mental health and disability (Ware et al., 1996). Each norm-based score is expressed as T-scores (i.e., Mean=50, SD=±10), with lower scores indicating greater disability.
Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5).
The AUDADIS-5 is a diagnostic interview of drug and alcohol use, DSM-5 drug, alcohol, and nicotine use disorders, and selected psychiatric disorders in the last 12 months and prior. The AUDADIS-5 demonstrates acceptable concordance with the Psychiatric Research Interview for Substance and Mental Disorders, DSM-5 version (Grant, Goldstein, Smith, et al., 2015; Hasin et al., 2015), verifying its utility in epidemiologic studies. The presence of any past year mental health disorder and/or substance use disorder as determined by the AUDADIS-5 were combined into a variable of any co-occurring past year mental or substance use disorder.
2.3. Analyses
All variables were examined and reported for the never, former, and current users. Analyses were conducted using SAS v9.4 (SAS Institute, Inc., Cary, NC) and accounted for NESARC-III’s complex sampling design using relevant cluster variables and survey weights. Between-group differences were tested using chi-square tests for categorical measures and general linear models (GLMs) for continuous measures. For Cohen’s d effect sizes, population standard deviations were estimated by using the relevant survey weights and pooling within and across sampling strata. In terms of missing data on the EFI, subjects with ≥ 3 missing items within EFI scales were excluded per scale guidelines (Aharonovich et al., 2017) (i.e. 0.6% and 0.8% of former and current users, respectively). P-values < 0.05 were interpreted as statistically significant; no correction was made for multiple hypothesis testing given that all tests involving marijuana use characteristics and EFI scores were pre-specified.
We performed two sets of primary analyses. First, we constructed GLMs to test differences in EFI scales between never, former, and current users, and between current users who did or did not meet criteria for CUD. Second, we examined associations between self-reported cognition and marijuana use characteristics among former and current users separately. Within the former users sub-sample, 3 GLMs were constructed to test the association between each EFI score and marijuana use characteristics prior to the past 12 months. Within the current users sub-sample, 3 GLMs were constructed to test the association between each EFI score and marijuana use characteristics prior to and within the past 12 months. All GLMs included the seven covariates as prespecified above. To meet the statistical assumptions of GLMs, a skewed variable (i.e. duration of marijuana use) was log-transformed. When multicollinearity between two variables resulted in model instability, one variable was selected based on the magnitude of association with the outcome measure. As described in section 2.1, respondents who only reported medical marijuana without recreational marijuana use were not queried about marijuana use characteristics. As such, these analyses only include 2,969 former and 695 current recreational marijuana users.
3. RESULTS
3.1. Sample Characteristics
3.1.1. Demographics
With the exception of urban/rural residence, the groups significantly differed with respect to all variables (Table 1.A). Compared to never users, former and current users were younger and more likely to be male. Irrespective of use, the majority of respondents were Non-Hispanic Whites. Current users were less likely to be married/cohabiting and more likely to be widowed/separated/divorced or never married compared to never and former users. Most former users were employed, while fewer of the never and current users were employed. Most former users had some college education or higher, whereas the never and current users had comparable proportions of respondents with and without college experience.
Table 1.
Demographic, mental, and physical health characteristics by marijuana use history.a
| Never users (n=10,976) | Former users (n=2,990) | Current users (n=712) | p-value | ||
|---|---|---|---|---|---|
| A. Demographic Characteristics | |||||
| Age (%) | <0.001 | ||||
| 50–64 years | 51.4 | 82.9 | 85.9 | ||
| 65+ years | 48.6 | 17.1 | 14.1 | ||
| Male (%) | 42.5 | 57.4 | 66.8 | <0.001 | |
| Race/ethnicity (%) | <0.001 | ||||
| Non-Hispanic White | 73.1 | 81.9 | 73.8 | ||
| Non-Hispanic Black | 10.0 | 9.3 | 15.3 | ||
| Hispanic | 10.2 | 5.6 | 6.2 | ||
| Non-Hispanic Asian | 5.5 | 1.6 | 0.8 | ||
| American Indian | 1.2 | 1.6 | 3.9 | ||
| Marital Status (%) | <0.001 | ||||
| Married/cohabiting | 64.2 | 64.5 | 43.7 | ||
| Widowed/separated/divorced | 30.2 | 27.4 | 43.7 | ||
| Never married | 5.6 | 8.1 | 12.6 | ||
| Education (%) | <0.001 | ||||
| Less than high school | 16.1 | 7.4 | 13.7 | ||
| High school or GED | 28.2 | 22.3 | 33.2 | ||
| Some college or higher | 55.7 | 70.3 | 53.2 | ||
| Family Income (%) | <0.001 | ||||
| $0–19,999 | 43.6 | 31.4 | 51.0 | ||
| $20,000—34,999 | 21.7 | 18.3 | 20.0 | ||
| $35,000—69,999 | 22.2 | 28.9 | 20.8 | ||
| >=$70,000 | 12.6 | 21.4 | 8.3 | ||
| Urban Residence (%) | 73.4 | 76.4 | 75.4 | 0.132 | |
| Geographic Region (%) | <0.001 | ||||
| Northeast | 18.1 | 21.7 | 18.1 | ||
| Midwest | 22.2 | 23.2 | 16.6 | ||
| South | 38.6 | 31.7 | 28.6 | ||
| West | 21.1 | 23.6 | 36.7 | ||
| Employed full-/part-time (%) | 38.0 | 58.3 | 42.1 | <0.001 | |
| B. Mental and Physical Health Characteristics | |||||
| Short-Form Health Survey [mean (SD)] | |||||
| Mental Health Scale | 52.7 (10.5) | 50.5 (10.8) | 47.3 (12.3) | <0.001 | |
| Mental Disability Scale | 52.0 (10.0) | 50.0 (10.4) | 47.3 (12.0) | <0.001 | |
| Past Year Mental Health (%) | |||||
| Depressive disorder | 7.8 | 13.5 | 20.0 | <0.001 | |
| Bipolar 1 or any hypomania | 0.9 | 2.0 | 3.7 | <0.001 | |
| Anxiety disorder | 10.7 | 16.0 | 23.2 | <0.001 | |
| Post-traumatic stress disorder | 2.6 | 5.2 | 9.4 | <0.001 | |
| Any of the above | 17.1 | 27.5 | 34.8 | <0.001 | |
| Past Year Substance Use (%) | |||||
| Other drug use disorder* | 0.3 | 0.7 | 5.3 | <0.001 | |
| Alcohol use disorder | 3.8 | 11.1 | 28.3 | <0.001 | |
| Opioid use disorder | 0.4 | 0.9 | 4.3 | <0.001 | |
| Nicotine use disorder | 11.5 | 23.5 | 47.8 | <0.001 | |
| Any of the above | 14.5 | 31.8 | 59.8 | <0.001 | |
| Co-occurring Mental and Substance Disorder (%) | 4.0 | 11.0 | 24.2 | <0.001 | |
| Number of diseases [mean (SD)] | |||||
| Neurological diseases | 0.2 (0.4) | 0.2 (0.5) | 0.3 (0.5) | <0.001 | |
| Cardiovascular diseases | 1.5 (1.5) | 1.3 (1.5) | 1.4 (1.6) | <0.001 | |
| Infectious diseases | 0.01 (0.1) | 0.02 (0.1) | 0.03 (0.2) | <0.001 | |
| Pain conditions | 0.1 (0.3) | 0.1 (0.3) | 0.1 (0.3) | 0.599 | |
| Any of the above | 1.8 (1.8) | 1.6 (1.8) | 1.8 (2.0) | 0.024 | |
Results are weighted and account for the complex survey design of the NESARC-III, precluding the report of raw numbers. Percentages have been rounded and may not total 100.0%.
3.1.2. Mental and Medical Conditions
Compared to never and former users, current users reported worse mental health and disability, and met criteria for more mental health and substance use disorders within the past year (Table 1.B). There were consistent stepwise differences in these variables; never users demonstrated better mental health than former users, and former users demonstrated better mental health than current users. All respondents reported few neurological, cardiovascular, or infectious diseases, or pain conditions.
3.1.3. Marijuana Use Characteristics
Both former and current users tended to begin to use marijuana during late adolescence (Table 2); however, current users began using marijuana most frequently at a younger age. Compared to former users, most current users (i.e. 83.5%) used weekly to daily, for over twice as many weeks and using more joints, during the period of most frequent use. Within the past 12 months, 47.6% of the current users used marijuana weekly to daily, using fewer than two joints a day. Among current users, 17.5% met criteria for CUD.
Table 2.
Marijuana use characteristics among former and current users.a
| Former users (n=2,969) | Current users (n=695) | p-value | |
|---|---|---|---|
| Use prior to the past 12 months | |||
| Age at first use [in years; mean (SD)] | 19.5 (6.3) | 19.0 (8.1) | 0.154 |
| Age when began using marijuana most [in years; mean (SD)] | 21.2 (7.2) | 19.0 (8.1) | <0.001 |
| Frequency of most use (%) | <0.001 | ||
| 1–11 times in a year | 35.2 | 6.8 | |
| 1–3 times a month | 17.6 | 8.8 | |
| 1–4 times a week | 25.8 | 27.1 | |
| Every day or nearly every day | 20.7 | 56.4 | |
| Duration used marijuana the most [in weeks, median (IQR)] | 156.0 (260.0) | 364.0 (1300) | <0.001 |
| Number of joints usually smoked in a day when using marijuana the most [mean (SD)] | 1.9 (2.5) | 3.2 (4.0) | <0.001 |
| Use within the past 12 months | |||
| Frequency of use in the last 12 months (%) | |||
| 1–11 times in the last year | − | 33.8 | |
| 1–3 times a month | − | 18.2 | |
| 1–4 times a week | − | 21.6 | |
| Every day or nearly every day | − | 26.0 | |
| Number of days since most recent marijuana use [Median (IQR)] | − | 7.0 (29.0) | |
| Number of joints usually smoked in a day in the last 12 months [mean (SD)] | − | 1.7 (1.8) | |
| Met criteria for CUD (%) | − | 17.5 |
Results are weighted and account for the complex survey design of the NESARC-III, precluding the report of raw numbers. Percentages have been rounded and may not total 100.0%.
3.2. EFI Scores by Marijuana Use History
Figure 1 presents the non-covariate adjusted EFI scores for each sub-group, with scores adjusted using survey weights. Figure 1.A illustrates the EFI scores of the three groups on the executive function (never: M=10.2, SE=0.1; former: M=10.4, SE=0.1; current: M=9.4, SE=0.1), attention (never: M=15.9, SE=0.0; former: M=15.9, SE=0.1; current: M=14.8, SE=0.2), and total scale (never: M=32.9, SE=0.1; former: M=32.7, SE=0.1; current: M=29.9, SE=0.4). Differences in all three scales were significant (p < 0.001) after adjusting for all covariates. All pairwise differences were statistically significant except for the comparisons between the never and former users’ executive functioning subscale (p = 0.197). Overall, current users reported lower EFI scores than never and former users with small-to-medium differences in all scales (d = −0.23 to −0.42), while these effects were absent between never and former users (d < 0.1). Figure 1.B illustrates the EFI scores of the current users with CUD (executive function: M=9.3, SE=0.4; attention: M=14.1, SE=0.5; total: M=28.8, SE=0.9) and without CUD (executive function: M=9.4, SE=0.2; attention: M=14.9, SE=0.3; total: M=30.1, SE=0.4). After covariate adjustment, current users with CUD had significantly lower attention (p = 0.018, d = 0.24) and total EFI scores (p = 0.039, d = 0.19) than current users without CUD.
Figure 1. Executive Function Index Subscale and Total Scores by Marijuana Use History and Cannabis Use Disorder (CUD) Diagnosis.
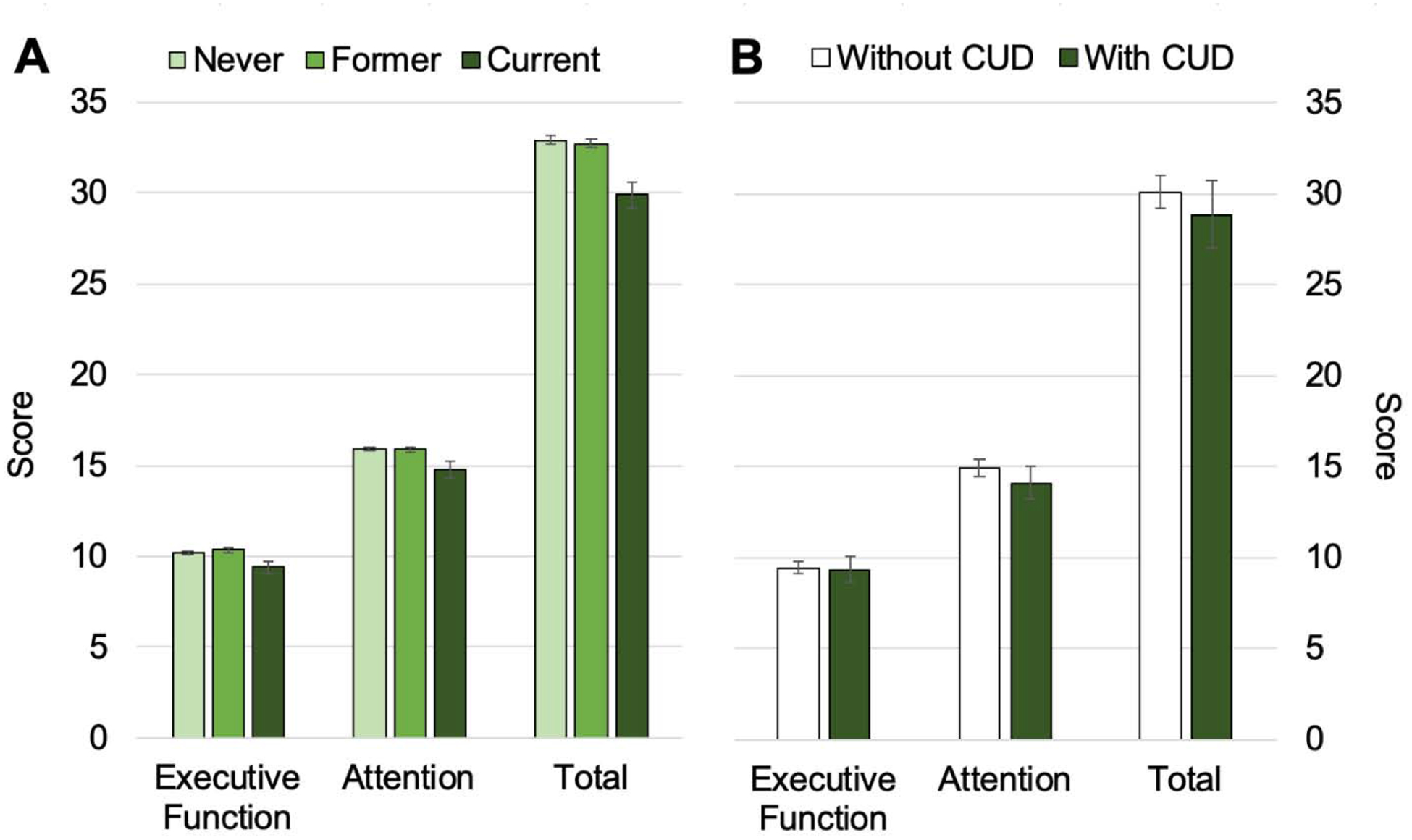
A. Bar chart of the mean Executive Function Index scores of never (n=10,976), former (n=2,990), and current users (n=712), where error bars indicate 95% confidence intervals. B. Bar chart of the mean Executive Function Index scores of the current users with (n=122) or without (n=573) CUD, where error bars indicate 95% confidence intervals. The Executive Function Index executive function, attention, and total scores have maximum scores of 16, 20, and 48, respectively. Values presented here were adjusted using NESARC-III survey weights but not for covariates.
3.3. Associations Between EFI Scores and Marijuana Use Characteristics
Among former users, greater duration of marijuana use during the period of most use was associated with lower scores on the executive function (p = 0.008), attention (p = 0.026), and total scales (p = 0.009; Table 3.A). Frequency of most use and age when began using marijuana the most were not significantly associated with EFI scales. Neither age at first use nor number of joints usually smoked in a day when using marijuana the most was included in these models due to multicollinearity.
Table 3.
Results from general linear models associating marijuana use characteristics with EFI scores.
| Executive Function Subscale | Attention Subscale | Total Scale | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | p-value | Est. | SE | p-value | Est. | SE | p-value | |
| A. Former Users (n=2,969) | |||||||||
| Intercept | 11.64 | 0.76 | <0.001 | 13.99 | 0.82 | <0.001 | 30.78 | 1.69 | <0.001 |
| Use prior to the past 12 months | |||||||||
| Age when began using marijuana most | −0.01 | 0.01 | 0.24 | −0.02 | 0.01 | 0.08 | −0.03 | 0.02 | 0.17 |
| Frequency of most use | 0.08 | 0.15 | 0.57 | ||||||
| 1–11 times in a year | Ref. | Ref. | Ref. | ||||||
| 1–3 times a month | −0.44 | 0.20 | 0.24 | 0.18 | −0.12 | 0.40 | |||
| 1–4 times a week | −0.34 | 0.18 | 0.30 | 0.14 | −0.29 | 0.34 | |||
| Every day or nearly every day | −0.45 | 0.22 | 0.07 | 0.19 | −0.59 | 0.44 | |||
| Duration used marijuana the most (years, on log scale) | −0.09 | 0.03 | 0.008 | −0.09 | 0.04 | 0.026 | −0.21 | 0.08 | 0.009 |
| R2 | p-value | R2 | p-value | R2 | p-value | ||||
| 0.10 | <0.001 | 0.18 | <0.001 | 0.19 | <0.001 | ||||
| B. Current Users (n=695) | |||||||||
| Intercept | 6.25 | 0.44 | <0.001 | 13.29 | 0.28 | <0.001 | 22.80 | 0.83 | <0.001 |
| Use prior to the past 12 months | |||||||||
| Age when began using marijuana most | 0.01 | 0.00 | 0.04 | 0.00 | 0.02 | 0.83 | 0.03 | 0.03 | 0.24 |
| Duration used marijuana the most (years, on log scale) | −0.16 | 0.03 | <0.001 | −0.02 | 0.01 | 0.13 | −0.30 | 0.08 | <0.001 |
| Use within the past 12 months | |||||||||
| Frequency of use in the last 12 months | 0.002 | <0.001 | <0.001 | ||||||
| 1–11 times in the last year | Ref. | Ref. | Ref. | ||||||
| 1–3 times a month | −0.22 | 0.10 | −0.73 | 0.14 | −1.64 | 0.16 | |||
| 1–4 times a week | −0.35 | 0.12 | −0.47 | 0.19 | −1.10 | 0.28 | |||
| Every day or nearly every day | −0.35 | 0.13 | −0.06 | 0.18 | −0.67 | 0.35 | |||
| R2 | p-value | R2 | p-value | R2 | p-value | ||||
| 0.11 | <0.001 | 0.22 | <0.001 | 0.24 | <0.001 | ||||
Note: All regression models included the following covariates: age, sex, race/ethnicity, education, SF-12 mental disability scale, SF-12 mental health scale, and co-occurring mental and substance use disorder per AUDADIS-5. The estimates provided reflect the difference in EFI scores associated with a 1-unit increase in the use characteristic (for continuous variables) or the difference when one group is compared to a referent group (for categorical variables). Est.=Estimate, Ref.=Reference group, SE=Standard Error.
Among current users, greater duration of use during the period of most use was also associated with lower scores on the executive function subscale and the total scale (p’s < 0.001; Table 3.B) but not the attention subscale. Age when began using the most was also associated with the executive function subscale (p = 0.043) but not with any other EFI scale, although the magnitude of this effect was very small. Frequency of use within the past 12 months was significantly associated with the EFI scales, but in varying ways according to frequency and EFI scale. As expected, more frequent use was associated with lower executive function (p = 0.002), in that former users who smoked monthly, weekly, or daily scored 0.2 to 0.4 points lower on the subscale compared to those who smoked infrequently (i.e. 1–11 times per year). More frequent use was also associated with worse attention and total scale scores compared to those who smoked infrequently, yet daily to near daily users endorsed higher scores than monthly or weekly users. Age at first use, number of joints smoked in a day when using the most, number of days since most recent use, and number of joints usually smoked in a day in the last 12 months were excluded due to multicollinearity. We also excluded the predictor of cannabis use disorder as it was highly associated with the comorbid mental and substance disorder covariate.
4. DISCUSSION
Using data from a nationally representative survey, we queried whether marijuana use was associated with self-reported cognitive function in older adults, adjusting for pertinent covariates. First, we tested differences in EFI scores between never, former, and current users. Consistent with our hypothesis, current users reported worse self-reported cognition than never and former users, although these effects were modest. Current users with CUD similarly reported worse cognition than current users without CUD. Second, we examined associations between marijuana use characteristics and EFI scores within each user group. We found that among both former and current users, greater duration of past marijuana use was associated with lower present-day EFI scores. We also found that although frequency of use (during their period of most use) was not associated with EFI scales among former users, for current users greater frequency of use during the past 12 months was associated with worse EFI scores. Interestingly, daily or near daily users reported better attention and executive function overall than monthly or weekly users. Taken together, these results suggest that current marijuana use and certain use characteristics (both recent and remote) may adversely affect self-reported cognition in older adults, over and above pertinent explanatory variables such as demographics and mental health.
Several factors likely contribute to current users’ endorsement of worse cognition compared to never and former users. Noteworthy among these are that almost half of current users were using weekly to daily, had greater rates of comorbid mental and substance use disorders, and had used marijuana at a younger age, more frequently, for longer, and with more joints than former users during their period of most use. Furthermore, current users with CUD also reported worse cognition, albeit the magnitude of this effect was small. It is possible that performance-based measures of cognition may identify more significant deficits that subjective self-report methodology cannot. Indeed, subjective and objective measures of cognitive function are often poorly correlated, particularly among older adults (Herreen & Zajac, 2017; Mendes et al., 2008; Reid & MacLullich, 2006).
Consistent with other reports using this and similar datasets (Choi et al., 2016, 2017; Han et al., 2017), current users in this study had highly prevalent co-occurring mental health (34.8%) or substance use (59.8%) disorders which may also confer independent or synergistic effects on cognition. That is, these comorbidities may highly influence the emergence of cognitive difficulties in addition to marijuana use in ways that cannot be fully captured or accounted for by incorporating these comorbidities as covariates, as we have done here. For instance, among the current users in this study, 28.3% had concurrent alcohol use disorder (AUD), and these individuals also had significantly lower EFI scores compared to those without AUD (see Supplementary Material). There is some evidence, at least in adolescents, that accounting for alcohol use may mitigate the association between cannabis use and cognition (Curran et al., 2016), but AUD is only one of the many comorbidities that may impact self-reported cognitive functioning; other conditions such as depression, anxiety, and nicotine use are also present at high rates among the current users in this study and are also associated with self-reported cognition (Carrigan & Barkus, 2016; Sachs-Ericsson et al., 2008; Shi et al., 2019; Valentine & Sofuoglu, 2018). As such, these results remain limited as disentangling the unique and shared variance among mental and substance use variables is not fully possible when using survey data that is observational (i.e. not subject to experimental control) and subjective (e.g. without corroborative biomarkers of substance use, performance-based measures of cognition, etc.). While population-based analyses provide power to characterize these phenomena in broad strokes, more carefully controlled clinical studies, ideally longitudinal ones, may offer a more nuanced understanding of how these factors interact to affect cognition in older adults. Future work should also verify these findings based on self-report with performance-based measures of cognition and corollary indices of brain health (e.g. neuroimaging), in addition to carefully characterizing psychiatric, substance use, and other medical comorbidities that may impact cognition (Vassilaki et al., 2015; Wolff et al., 2002).
This study also identified marijuana use characteristics, both recent and remote, that are worth probing further when examining their associations with cognition. Of these, duration of past use may be most influential, as this was consistently associated with worse cognition among both former and current users. However, inherent to survey research is the noise introduced by recall bias, so this finding bears further replication. Frequency of current use also appears to impact present-day cognition, although our findings suggest that more frequent (i.e. daily) users may under-report cognitive problems compared to less frequent (i.e. weekly to monthly) users. This effect is aligned with previous observations that drug use may impair meta-cognition (i.e. awareness of deficits), which has been observed among adolescent marijuana users (McClure et al., 2015) and adults taking benzodiazepines (Kleykamp et al., 2010). These nuanced findings reinforce the need for further corroboration with performance-based and other corollary measures of cognitive function.
That age during period of most use was not associated with self-reported cognition was unexpected, given previous reports suggesting marijuana use during a vulnerable time of brain development can be impactful (Gruber et al., 2012; Sagar & Gruber, 2018). It is possible that while both former and current users in this sample reported first using most heavily during late adolescence/early adulthood, intervening events such as periods of abstinence or other restorative factors may attenuate this possible effect throughout the lifespan. There may also be other important factors such as pre-existing executive or cognitive control problems that drive self-initiation of substance use in general that may influence the emergence of these problems in older adulthood, irrespective of the substance/s used. Thus, modeling dynamic changes in these exposures or differences in predisposing factors becomes especially important when studying older adults, which was not possible with the current study. We had to exclude other use characteristics in our models to adhere to statistical assumptions, but these factors should still be thoroughly characterized and be factored into metrics of overall disease burden when statistically modeling these potential associations. Furthermore, with the increasing legalization of marijuana, it will be even more necessary to collect data on use characteristics with which to approximate causal associations, such as motivations for use (i.e. recreational vs. medical use and its indication/s), product type (i.e. plant, concentrate, etc.), method of delivery or route of administration (i.e. edible, combustible, non-combustible), cannabis constituents and potency (THC:CBD ratio).
This study is a significant contribution to the literature in that it is, to our knowledge, the first population-based study to explicitly examine cognition in older marijuana users and to provide evidence that current users may have worse self-reported cognition than former and non-users. Nonetheless, we were unable to address other important questions, such as whether marijuana use affects other cognitive domains (notably memory and processing speed (Sagar & Gruber, 2018)), or whether the onset of marijuana use in later life or the use of medical marijuana affects cognition. We also could not account for medical comorbidities given that the available data only indicated the number of diseases and not their severity or potential influence on cognition. The presence of cognitive disorders was neither ascertained nor were individuals with bona fide cognitive deficits excluded in this study. Thus, other factors may account for self-reported cognition in addition to marijuana use. Moreover, we cannot infer causality as cognitive deficits may predispose an individual to substance use and impact use trajectory. Mitigating these limitations is the large sample size with data that are optimized for accurate characterization of mental health and substance use on a population level. As such, we were able to control for many variables that might influence self-reported cognition.
5. CONCLUSIONS
Given the shifting legal landscape and increased use among older adults, a better understanding of the impact of marijuana use on cognition is critical. This paper represents an important first step in understanding these associations on a population level. While the results suggest that lifetime marijuana use may impact self-reported cognition in older adulthood, the methodological limitations in this study necessitate cautious interpretation of these findings. Future studies can clarify these associations by including objective cognitive assessments or neuroimaging, as well as longitudinal studies examining individual-level changes in cognitive functioning.
Supplementary Material
HIGHLIGHTS.
Older marijuana users reported worse cognition compared to never and former users
Greater duration and frequency of past use were associated with worse cognition
Effects may be subtle and specific to particular marijuana use characteristics
Results must be interpreted with caution given the limitations of self-report
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
The authors report no conflicts of interest or financial relationships with commercial interests.
REFERENCES
- Abuhasira R, Schleider LB-L, Mechoulam R, & Novack V (2018). Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. European Journal of Internal Medicine, 49, 44–50. 10.1016/j.ejim.2018.01.019 [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Shmulewitz D, Wall MM, Grant BF, & Hasin DS (2017). Self-reported cognitive scales in a US National Survey: reliability, validity, and preliminary evidence for associations with alcohol and drug use: Substance use and cognition in a US survey. Addiction. 10.1111/add.13911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2019). 2019 Alzheimer’s disease facts and figures. 15(3), 321–387. [Google Scholar]
- Aso E, Andrés-Benito P, & Ferrer I (2016). Delineating the Efficacy of a Cannabis-Based Medicine at Advanced Stages of Dementia in a Murine Model. Journal of Alzheimer’s Disease: JAD, 54(3), 903–912. 10.3233/JAD-160533 [DOI] [PubMed] [Google Scholar]
- Bilkei-Gorzo A, Albayram O, Draffehn A, Michel K, Piyanova A, Oppenheimer H, Dvir-Ginzberg M, Rácz I, Ulas T, Imbeault S, Bab I, Schultze JL, & Zimmer A (2017). A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nature Medicine, 23(6), 782–787. 10.1038/nm.4311 [DOI] [PubMed] [Google Scholar]
- Briscoe J, & Casarett D (2018). Medical Marijuana Use in Older Adults. Journal of the American Geriatrics Society, 66(5), 859–863. 10.1111/jgs.15346 [DOI] [PubMed] [Google Scholar]
- Broyd SJ, van Hell HH, Beale C, Yücel M, & Solowij N (2016). Acute and Chronic Effects of Cannabinoids on Human Cognition-A Systematic Review. Biological Psychiatry, 79(7), 557–567. 10.1016/j.biopsych.2015.12.002 [DOI] [PubMed] [Google Scholar]
- Burggren AC, Shirazi A, Ginder N, & London ED (2019). Cannabis effects on brain structure, function, and cognition: considerations for medical uses of cannabis and its derivatives. The American Journal of Drug and Alcohol Abuse, 1–17. 10.1080/00952990.2019.1634086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burggren AC, Siddarth P, Mahmood Z, London ED, Harrison TM, Merrill DA, Small GW, & Bookheimer SY (2018). Subregional Hippocampal Thickness Abnormalities in Older Adults with a History of Heavy Cannabis Use. Cannabis and Cannabinoid Research, 3(1), 242–251. 10.1089/can.2018.0035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrigan N, & Barkus E (2016). A systematic review of the relationship between psychological disorders or substance use and self-reported cognitive failures. Cognitive Neuropsychiatry, 21(6), 539–564. 10.1080/13546805.2016.1250620 [DOI] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, & Marti CN (2016). Older marijuana users: Life stressors and perceived social support. Drug and Alcohol Dependence, 169, 56–63. 10.1016/j.drugalcdep.2016.10.012 [DOI] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, & Marti CN (2017). Older adults who use or have used marijuana: Help-seeking for marijuana and other substance use problems. Journal of Substance Abuse Treatment, 77, 185–192. 10.1016/j.jsat.2017.02.005 [DOI] [PubMed] [Google Scholar]
- Cohen K, & Weinstein A (2018). The Effects of Cannabinoids on Executive Functions: Evidence from Cannabis and Synthetic Cannabinoids-A Systematic Review. Brain Sciences, 8(3). 10.3390/brainsci8030040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colliver J, Compton W, Gfroerer J, & Condon T (2006). Projecting Drug Use Among Aging Baby Boomers in 2020. Annals of Epidemiology, 16(4), 257–265. 10.1016/j.annepidem.2005.08.003 [DOI] [PubMed] [Google Scholar]
- Curran HV, Freeman TP, Mokrysz C, Lewis DA, Morgan CJA, & Parsons LH (2016). Keep off the grass? Cannabis, cognition and addiction. Nature Reviews. Neuroscience, 17(5), 293–306. 10.1038/nrn.2016.28 [DOI] [PubMed] [Google Scholar]
- Early DR, Widaman KF, Harvey D, Beckett L, Park LQ, Farias ST, Reed BR, DeCarli C, & Mungas D (2013). Demographic predictors of cognitive change in ethnically diverse older persons. Psychology and Aging, 28(3), 633–645. 10.1037/a0031645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie NA, Neale MC, Bates TC, Eyler LT, Fennema-Notestine C, Vassileva J, Lyons MJ, Prom-Wormley EC, McMahon KL, Thompson PM, de Zubicaray G, Hickie IB, McGrath JJ, Strike LT, Rentería ME, Panizzon MS, Martin NG, Franz CE, Kremen WS, & Wright MJ (2018). Testing associations between cannabis use and subcortical volumes in two large population-based samples. Addiction, 113(9), 1661–1672. 10.1111/add.14252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez R, Pacheco-Colón I, Duperrouzel JC, & Hawes SW (2017). Does Cannabis Use Cause Declines in Neuropsychological Functioning? A Review of Longitudinal Studies. Journal of the International Neuropsychological Society: JINS, 23(9–10), 893–902. 10.1017/S1355617717000789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Jiao R, Ren W, & Goldstein R (2014). Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Grant Bridget F., Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant Bridget F., Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP, Ruan WJ, Huang B, Saha TD, Aivadyan C, Greenstein E, & Hasin DS (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. Drug and Alcohol Dependence, 148, 27–33. 10.1016/j.drugalcdep.2014.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber SA, Sagar KA, Dahlgren MK, Racine M, & Lukas SE (2012). Age of onset of marijuana use and executive function. Psychology of Addictive Behaviors, 26(3), 496–506. 10.1037/a0026269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, & Palamar JJ (2018). Marijuana use by middle-aged and older adults in the United States, 2015–2016. Drug and Alcohol Dependence, 191, 374–381. 10.1016/j.drugalcdep.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, Sherman S, Mauro PM, Martins SS, Rotenberg J, & Palamar JJ (2017). Demographic trends among older cannabis users in the United States, 2006–13: Cannabis use among older adults. Addiction, 112(3), 516–525. 10.1111/add.13670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Greenstein E, Aivadyan C, Stohl M, Aharonovich E, Saha T, Goldstein R, Nunes EV, Jung J, Zhang H, & Grant BF (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug and Alcohol Dependence, 148, 40–46. 10.1016/j.drugalcdep.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herreen D, & Zajac I (2017). The Reliability and Validity of a Self-Report Measure of Cognitive Abilities in Older Adults: More Personality than Cognitive Function. Journal of Intelligence, 6(1), 1 10.3390/jintelligence6010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleykamp BA, Griffiths RR, & Mintzer MZ (2010). Dose effects of triazolam and alcohol on cognitive performance in healthy volunteers. Experimental and Clinical Psychopharmacology, 18(1), 1–16. 10.1037/a0018407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure EA, Lydiard JB, Goddard SD, & Gray KM (2015). Objective and subjective memory ratings in cannabis-dependent adolescents: Memory in Cannabis-Dependent Adolescents. The American Journal on Addictions, 24(1), 47–52. 10.1111/ajad.12171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes T, Ginó S, Ribeiro F, Guerreiro M, Sousa G. de, Ritchie K, & de Mendonça A (2008). Memory complaints in healthy young and elderly adults: Reliability of memory reporting. Aging & Mental Health, 12(2), 177–182. 10.1080/13607860701797281 [DOI] [PubMed] [Google Scholar]
- Morean ME, & Lederman IR (2019). Prevalence and correlates of medical cannabis patients’ use of cannabis for recreational purposes. Addictive Behaviors, 93, 233–239. 10.1016/j.addbeh.2019.02.003 [DOI] [PubMed] [Google Scholar]
- Nader DA, & Sanchez ZM (2018). Effects of regular cannabis use on neurocognition, brain structure, and function: a systematic review of findings in adults. The American Journal of Drug and Alcohol Abuse, 44(1), 4–18. 10.1080/00952990.2017.1306746 [DOI] [PubMed] [Google Scholar]
- Reid LM, & MacLullich AMJ (2006). Subjective Memory Complaints and Cognitive Impairment in Older People. Dementia and Geriatric Cognitive Disorders, 22(5–6), 471–485. 10.1159/000096295 [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Joiner T, & Blazer DG (2008). The influence of lifetime depression on self-reported memory and cognitive problems: results from the National Comorbidity Survey-Replication. Aging & Mental Health, 12(2), 183–192. 10.1080/13607860801951739 [DOI] [PubMed] [Google Scholar]
- Sagar KA, & Gruber SA (2018). Marijuana matters: reviewing the impact of marijuana on cognition, brain structure and function, & exploring policy implications and barriers to research. International Review of Psychiatry, 30(3), 251–267. 10.1080/09540261.2018.1460334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Cummings-Vaughn LA, Holzer KJ, Nelson EJ, AbiNader M, & Oh S (2017). Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002–2014. Drug and Alcohol Dependence, 171, 97–106. 10.1016/j.drugalcdep.2016.11.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarne Y, Toledano R, Rachmany L, Sasson E, & Doron R (2018). Reversal of age-related cognitive impairments in mice by an extremely low dose of tetrahydrocannabinol. Neurobiology of Aging, 61, 177–186. 10.1016/j.neurobiolaging.2017.09.025 [DOI] [PubMed] [Google Scholar]
- Scott JC, Slomiak ST, Jones JD, Rosen AFG, Moore TM, & Gur RC (2018). Association of Cannabis With Cognitive Functioning in Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Psychiatry, 75(6), 585 10.1001/jamapsychiatry.2018.0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi R, Sharpe L, & Abbott M (2019). A meta-analysis of the relationship between anxiety and attentional control. Clinical Psychology Review, 72, 101754 10.1016/j.cpr.2019.101754 [DOI] [PubMed] [Google Scholar]
- Spinella M (2005). SELF-RATED EXECUTIVE FUNCTION: DEVELOPMENT OF THE EXECUTIVE FUNCTION INDEX. International Journal of Neuroscience, 115(5), 649–667. 10.1080/00207450590524304 [DOI] [PubMed] [Google Scholar]
- Thayer RE, YorkWilliams S, Karoly HC, Sabbineni A, Ewing SF, Bryan AD, & Hutchison KE (2017). Structural neuroimaging correlates of alcohol and cannabis use in adolescents and adults: Neuroimaging of alcohol and cannabis use. Addiction, 112(12), 2144–2154. 10.1111/add.13923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer RE, YorkWilliams SL, Hutchison KE, & Bryan AD (2019). Preliminary results from a pilot study examining brain structure in older adult cannabis users and nonusers. Psychiatry Research. Neuroimaging, 285, 58–63. 10.1016/j.pscychresns.2019.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine G, & Sofuoglu M (2018). Cognitive Effects of Nicotine: Recent Progress. Current Neuropharmacology, 16(4), 403–414. 10.2174/1570159X15666171103152136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Elsen GAH, Ahmed AIA, Lammers M, Kramers C, Verkes RJ, van der Marck MA, & Rikkert MGMO (2014). Efficacy and safety of medical cannabinoids in older subjects: A systematic review. Ageing Research Reviews, 14, 56–64. 10.1016/j.arr.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Vassilaki M, Aakre JA, Cha RH, Kremers WK, St. Sauver JL, Mielke MM, Geda YE, Machulda MM, Knopman DS, Petersen RC, & Roberts RO (2015). Multimorbidity and Risk of Mild Cognitive Impairment. Journal of the American Geriatrics Society, 63(9), 1783–1790. 10.1111/jgs.13612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J, Kosinski M, & Keller SD (1996). A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Starfield B, & Anderson G (2002). Prevalence, Expenditures, and Complications of Multiple Chronic Conditions in the Elderly. Archives of Internal Medicine, 162(20), 2269 10.1001/archinte.162.20.2269 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


