Abstract
Primary cardiac lymphoma (PCL) involves the heart and pericardium. Symptoms may vary according to the cardiac site involved. The most frequent cardiac manifestations associated with PCL are pericardial effusion, heart failure, and atrioventricular block. PCL can be diagnosed using transesophageal echocardiography, computed tomography (CT), or magnetic resonance imaging. We herein discuss a 67-year-old male patient who presented with sick sinus syndrome. CT demonstrated a tumor in the right atrium obstructing the superior vena cava. The patient underwent a diagnostic lateral thoracotomy with concomitant epicardial pacemaker insertion. Histological examination revealed a diffuse large B cell lymphoma, and chemotherapy, including rituximab, was begun. A diagnostic thoracotomy is crucial for a definitive diagnosis of PCL, and the most effective treatment is chemotherapy.
<Learning objective: Primary cardiac lymphoma may cause sick sinus syndrome. The choice of epicardial lead precludes the risk of peripheral embolisms during transvenous endocardial pacemaker insertion.>
Keywords: Primary cardiac lymphoma, Sick sinus syndrome, Epicardial lead, Epicardial pacemaker
Introduction
Primary cardiac lymphoma (PCL) involves the heart and pericardium, with symptoms sometimes varying according to the cardiac site involved. The most frequent cardiac manifestations associated with PCL are pericardial effusion, heart failure, and atrioventricular block (AV block) [1]. PCL is a rare disease comprising only 1.3% of all cardiac tumors [2]. The majority of cases are diffuse large B-cell lymphomas. PCL is fatal unless diagnosed and treated in time [3]. We report herein a patient with PCL who showed unusual cardiac manifestations. The patient was treated successfully by thoracotomy with a concomitant epicardial pacemaker insertion and chemotherapy.
Case report
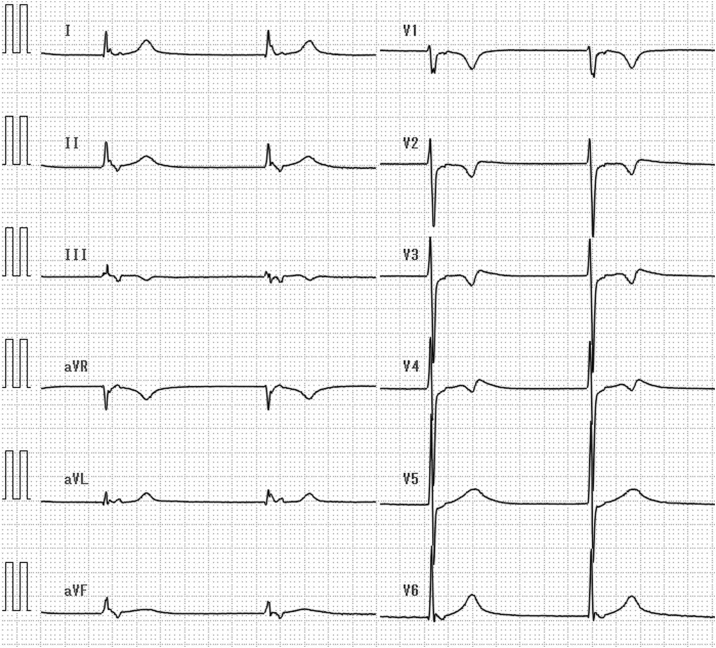
A 67-year-old male patient was admitted with worsening dyspnea and loss of strength of two weeks’ duration. A clinical examination denied lymphadenopathy, intermittent fever, and loss of weight. However, he had sick sinus syndrome with a junctional escape rhythm which was refractory to atropine and necessitated temporary pacing (Fig. 1).
Fig. 1.
Sick sinus syndrome with a junctional escape rhythm (49 bpm).
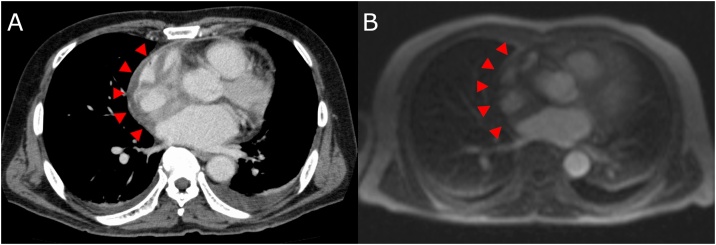
Laboratory tests showed an elevated lactate dehydrogenase level of 364 U/L, soluble interleukin-2 receptor level of 982 U/mL, and an N-terminal pro hormone B-type natriuretic peptide level of 1517 pg/mL. The complete blood count and coagulation profile test were within normal limits. A transthoracic echocardiogram revealed pericardial effusion and thickening of the atrial free wall. Computed tomography (CT) demonstrated extensive pericardial tumor masses invading the right atrium and superior vena cava (SVC) (Fig. 2A), and magnetic resonance imaging (MRI) demonstrated a tumor in the right atrium obstructing the SVC (Fig. 2B). Cardiac effusion was reduced by medication, including diuretics. For a definitive diagnosis, the patient underwent a diagnostic thoracotomy with epicardial pacemaker insertion. A small biopsy specimen of the right atrial wall was obtained by thoracotomy, and an epicardial screw-in electrode was placed in the right ventricle, inserted into the subcutaneous tissue, and connected to a VVI pacemaker.
Fig. 2.
(A) Computed tomography scan demonstrating tumor masses invading both the atrial free wall and intra-atrial septum. Tumor masses extending around the superior vena cava (arrows). (B) Preoperative cardiac magnetic resonance imaging. Four-chamber view perfusion sequence. Perfusion is seen in the masses (arrows).
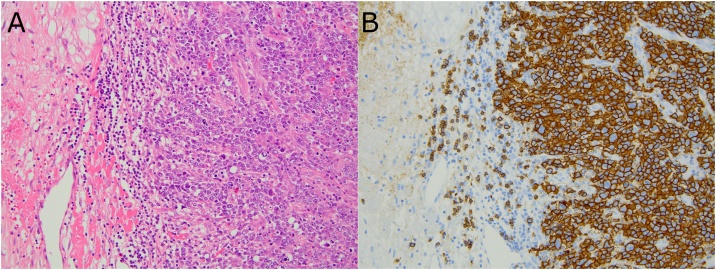
Detailed histological examination of the tumor revealed that it was a diffuse large B cell lymphoma (immuno-phenotype: non-germinal center, CD10-negative, CD19-positive, CD20-positive, CD25-positive, CD30-negative, CD45RO-negative, BCL2-negative, BCL6-negative, MUM1-positive, EBER-negative) (Fig. 3). A bone marrow biopsy revealed normocellular bone marrow infiltration of lymphomatous cells. The patient had a stage II diffuse large B cell lymphoma according to the Ann Arbor Classification and was started on a chemotherapy regimen including rituximab. A follow-up CT 12 weeks after finishing the third course of chemotherapy showed marked reduction of the tumor masses, but the sinus function had not recovered.
Fig. 3.
Histological section of the right atrium. Large, atypical, diffusely proliferating lymphoid cells with membranous expression of CD20. (A) Hematoxylin and eosin original magnification, ×200; (B) Membranous expression of CD20 (original magnification, ×200).
Discussion
The patient received the diagnosis of diffuse large B cell non-Hodgkin lymphoma (NHL) with cardiac involvement. Diffuse large cell lymphoma is the most common type of NHL, comprising 31% of cases, and is rapidly fatal if left untreated. In general, it occurs in middle-aged or older patients.
Cardiac tumors arising from the heart or the pericardium are normally benign. The most common primary malignant tumors are sarcomas and lymphomas. PCL is rare (1%), but secondary involvement of the heart is not uncommon in lymphoma (20%) [4]. PCL has been linked to immunosuppression, including that seen in human immunodeficiency virus infection, but is extremely rare in immunocompetent subjects where it is most frequently associated with rheumatoid arthritis [4]. Previously, a close relationship between Epstein–Barr virus infection and malignant lymphomas was discovered in immunodeficient patients [5]. Cardiac involvement as an initial presentation of malignant lymphoma is rare. At autopsy, cardiac involvement is evident in about 1% of patients with advanced cancer. Secondary involvement of the heart is seen in 7–27% of the documented, clinical cases of lymphoma [6].
The clinical presentation of cardiac metastases is determined by numerous factors, such as tumor location, size, growth rate, degree of invasion, and friability [6]. Electrocardiogram findings include atrial flutter, atrial fibrillation, and various degrees of AV block. The English-language literature has described about 20 cases presenting with AV block [7]. Sick sinus syndrome caused by tumoral disturbance of the pacing system is very rare. More common presentations associated with malignant cardiac tumors are congestive heart failure, pericardial effusion, and SVC obstruction [5].
A number of mechanisms have been suggested to explain heart involvement, such as direct pressure of the neighboring tumor in a mediastinal site, retrograde flow through the cardiac lymphatics, and hematogenous spread [8]. In the present case, we assumed that the lymphoma was directly interfering with the sinus node. The mechanism was unclear, but as the pathological examination revealed a direct invasion of the right atrial wall (Fig. 3), the lymphoma was assumed to have irreversibly invaded the sinus node. A small section was obtained from the upper lateral site of the atrium. Thus, the risk of surgical complications was low.
Echocardiography is the first-choice, non-invasive modality for examining the heart and pericardium, but the restricted acoustic window of the transthoracic approach remains a significant limitation. The larger imaging field afforded by transesophageal echocardiography makes this a more sensitive technique for these patients. CT adequately demonstrates the morphology, location, and extent of cardiac neoplasms while MRI with contrast enhancement produces superior images identifying the anatomy, blood flow, and cardiac function. CT and MRI have better contrast resolution than echocardiography and may help identify the tumor type. Although these different imaging modalities (ultrasound, CT, MRI) should be considered as complementary rather than competitive, if cardiac involvement is suspected, MRI is preferred [9].
The prognosis of lymphoma with cardiac involvement remains poor due to diagnostic delays and advanced organ infiltration [8]. The available literature suggests that systemic chemotherapy is the only effective therapy. Theoretically, there is a risk of cardiac wall perforation in response to chemotherapy. The majority of cases are treated with combination chemotherapy with varying results. However, nowadays, the addition of rituximab to the cyclophosphamide, doxorubicin, vincristine, and prednisone protocol increases the overall survival rate [8]. Rituximab is a monoclonal antibody directed against CD20 and frequently induces regression in a variety of B cell NHL. Its activity appears to involve the induction of antibody-dependent, cell-mediated cytotoxicity, complement-mediated lysis, phagocytosis of antibody-coupled tumor cells, and induction of apoptosis [10].
The present case demonstrated that a patient presenting with sick sinus syndrome and requiring a definitive diagnosis can successfully be treated by epicardial pacemaker lead insertion and obtaining a tissue sample from the right atrium. An epicardial lead avoids the risk of peripheral embolisms during transvenous endocardial pacemaker insertion.
All the authors have seen and approved the manuscript and have contributed significantly to the work. We confirm that the manuscript has not been published and is not being considered for publication elsewhere.
Potential conflicts of interest: All the authors report no conflicts of interest relevant to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
Acknowledgments
We are grateful to Dr Satoshi Miyahara for preparing the pathology figures.
References
- 1.Hsueh S.-C., Chung M.-T., Fang R., Hsiung M.-C., Young M.-S., Lu H.-F. Primary cardiac lymphoma. J Chin Med Assoc. 2006;69:169–174. doi: 10.1016/S1726-4901(09)70200-X. [DOI] [PubMed] [Google Scholar]
- 2.Johri A., Baetz T., Isotalo P.A., Nolan R.L., Sanfilippo A.J., Ropchan G. Primary cardiac diffuse large B cell lymphoma presenting with superior vena cava syndrome. Can J Cardiol. 2009;25:e210–e212. doi: 10.1016/s0828-282x(09)70110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rolla G., Bertero M.T., Pastena G., Tartaglia N., Corradi F., Casabona R. Primary lymphoma of the heart. A case report and review of the literature. Leuk Res. 2002;26:117–120. doi: 10.1016/s0145-2126(01)00092-3. [DOI] [PubMed] [Google Scholar]
- 4.Yavari A., El-Mahy H., McWilliams E.T. Right atrial mass in the context of recurrent non-Hodgkin's lymphoma: atrial myxoma presenting with atrial flutter. BMJ Case Rep. 2009 doi: 10.1136/bcr.10.2008.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagano M., Uike N., Suzumiya J., Muta K., Goto T., Suehiro Y. Successful treatment of a patient with cardiac lymphoma who presented with a complete atrioventricular block. Am J Hematol. 1998;59:171–174. doi: 10.1002/(sici)1096-8652(199810)59:2<171::aid-ajh12>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 6.Ban-Hoefen M., Zeglin M.A., Bisognano J.D. Diffuse large B cell lymphoma presenting as a cardiac mass and odynophagia. Cardiol J. 2008;15:471–474. [PubMed] [Google Scholar]
- 7.Cho S.W., Kang Y.J., Kim T.H., Cho S.K., Hwang M.W., Chang W. Primary cardiac lymphoma presenting with atrioventricular block. Korean Circ J. 2010;40:94–98. doi: 10.4070/kcj.2010.40.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Errihani H., Belbaraka R., Ismaili N., Cherti M. An unusual presentation of non-Hodgkin lymphoma: cardiac involvement. J Cancer Res Ther. 2010;6:401–402. doi: 10.4103/0973-1482.73329. [DOI] [PubMed] [Google Scholar]
- 9.Ryu S.J., Choi B.W., Choe K.O. CT and MR findings of primary cardiac lymphoma: report upon 2 cases and review. Yonsei Med J. 2001;42:451–456. doi: 10.3349/ymj.2001.42.4.451. [DOI] [PubMed] [Google Scholar]
- 10.Nakagawa Y., Ikeda U., Hirose M., Ubukata S., Katsuki T-a, Kaminishi Y. Successful treatment of primary cardiac lymphoma with monoclonal CD20 antibody (rituximab) Circ J. 2004;68:172–173. doi: 10.1253/circj.68.172. [DOI] [PubMed] [Google Scholar]