Abstract
Transcatheter interventions for structural heart disease (SHD) now represent an effective alternative to surgery in selected patients. A clear premise is that delay in or neglect of treating patients in need of SHD intervention is associated with unavoidable morbidity and mortality because many of them have life-threatening conditions. However, the recent outbreak of coronavirus-associated disease-2019 (COVID-19) is placing an unprecedented strain on patients, physicians and world healthcare systems that resulted in deferral of elective and semi-elective procedures, such as SHD, and delay in the treatment of patients with acute coronary syndrome (ACS). We hereby present the case for a focused resumption of transcatheter SHD interventions in selected centers, in order to preserve patient safety and avoid that death rate will extend far beyond that directly associated with COVID-19. A similar approach should be applied to the invasive management of ACS. Indeed, a proactive and vigilant stance on managing SHD and ACS is crucial, especially in the context of the COVID-19 pandemic, when the risk of overlooking severely sick patients or postponing life-saving treatments is high. If such corrective measures are not put into effect, we may expect in the near future an excess of avoidable fatalities indirectly due to COVID-19 but truly caused by cardiovascular diseases, as well as an exceedingly large number of patients with severe heart failure leading to shorter life expectancy, reduced quality of life and increased healthcare cost.
Keywords: Acute coronary syndrome, COVID-19, Aortic stenosis, Mitral regurgitation, Transcatheter aortic valve implantation
Delay always breeds danger; and to protract a great design is often to ruin it.
Miguel de Cervantes
Transcatheter interventions for structural heart disease (SHD), in particular aortic stenosis and mitral regurgitation, have come a long way in less than two decades and now represent an effective alternative to surgery in selected patients [1, 2]. Accordingly, several centers worldwide have established SHD programs with substantial case load yearly. A clear premise is that delay in or neglect of treating patients in need of SHD intervention is associated with unavoidable morbidity and mortality because many of them have life-threatening conditions. However, the recent outbreak of coronavirus-associated disease 2019 (COVID-19) is placing an unprecedented strain on patients, physicians, and world healthcare systems resulting in deferral of elective and semi-elective procedures, such as those for subjects with SHD, and delay in the treatment of patients with acute coronary syndrome (ACS) [3–6]. We hereby present the case for a focused resumption of transcatheter SHD interventions in selected centers, in order to preserve patient safety and avoid that death rates will extend far beyond that directly associated with COVID-19. A similar approach should be applied to the invasive management of ACS (Table 1).
Table 1.
Highlights of life-saving interventions for structural heart disease and coronary artery disease
| Setting | Incidence per year | Treatment | Comparator | Outcome | Results | Number needed to treat to prevent one death | Reference |
|---|---|---|---|---|---|---|---|
| Aortic stenosis | 150/106 | Transcatheter aortic valve implantation | Balloon aortic valvuloplasty | Risk of death at 12 months | 31% vs 50% | 5 | [7] |
| Secondary mitral regurgitation | 300/106 | Transcatheter mitral valve repair | Conservative management | Risk of death at 12 months | 19% vs 23% | 25 | [8] |
| ST-elevation myocardial infarction | 800/106 | Streptokinase and aspirin | Conservative management | Risk of vascular death at 5 weeks | 8% vs 13% | 20 | [9] |
| ST-elevation myocardial infarction | 800/106 | Primary percutaneous coronary intervention | Thrombolysis | Risk of death at 4–6 weeks | 7% vs 8% | 50 | [10]. |
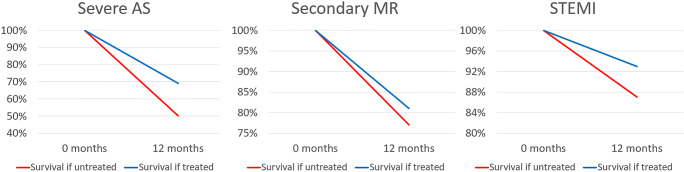
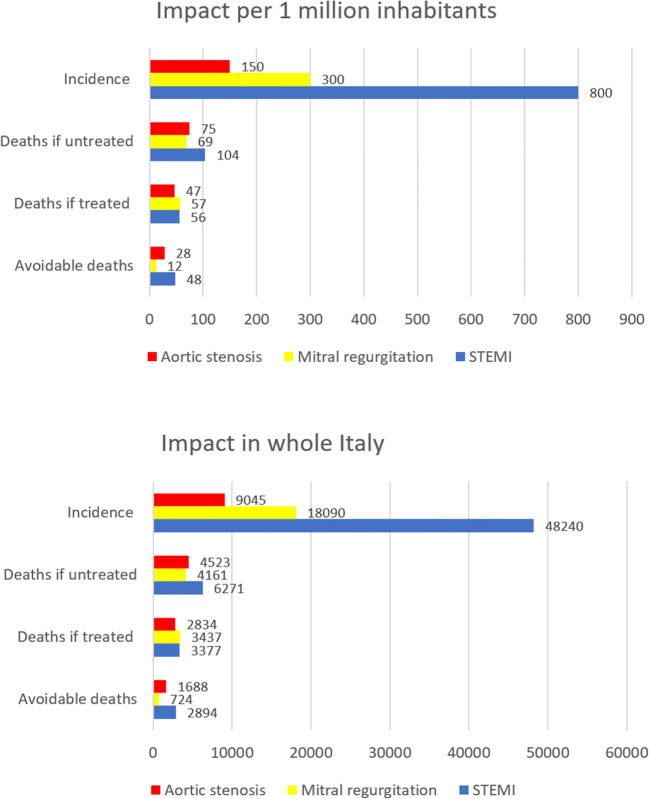
As previously mentioned, there is ample evidence that transcatheter aortic valve implantation (TAVI) is significantly more beneficial than medical therapy (even when valvuloplasty is considered) in patients with severe aortic stenosis at prohibitive risk of surgery [7]. Similar favorable results have been reported in patients who have high, intermediate, or low operative risk [11]. Indeed, we should not ignore that the 1-year all-cause mortality in inoperable patients enrolled in the Placement of AoRTic TraNscathetER Valve Trial (PARTNER) and treated with medical therapy reached 50%. This translates into a monthly death rate of 4% (Fig. 1) [7]. In other words, for each month of interventional treatment delay, we may expect that roughly 1 out of 20 inoperable patients with symptomatic severe aortic stenosis dies while waiting due treatment (Fig. 2). This risk is significantly reduced with timely TAVI. Although mortality of asymptomatic aortic stenosis is lower, recent data suggest that early intervention is similarly beneficial if timely and systematically adopted [12].
Fig. 1.
Survival benefits of appropriate invasive management in patients with severe aortic stenosis (AS), secondary mitral regurgitation (MR), and ST-elevation myocardial infarction (STEMI)
Fig. 2.
Incidence and yearly deaths, including avoidable ones, in patients with severe aortic stenosis, secondary mitral regurgitation, and ST-elevation myocardial infarction (STEMI), per million inhabitants (top panel), and in Italy as a whole (bottom panel)
Analogous evidence in favor of transcatheter repair of functional mitral regurgitation has been reported by the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) trial [8]. Although estimates of absolute risk clearly differ in this patient population, a 50% all-cause death rate has been reported at 24-month follow-up in the conservative management arm. This translates into a 2% monthly fatality rate unless percutaneous edge-to-edge mitral repair is early instituted in patients with severe regurgitation.
While more challenging given the potential interaction between the prothrombotic milieu of COVID-19 and the natural history of atherothrombosis, we cannot neglect the importance of the invasive and timely management of ACS. Unfortunately, growing data show that the number of ACS patients presenting for emergent care is not in line with pre-pandemic levels. This may indicate that people are reluctant to go to the hospital because of COVID-19 fear. Indeed, STEMI admissions have apparently dropped in many countries, and patients hospitalized often have substantially longer symptom-to-balloon times, leading to poor reperfusion and higher rate of cardiogenic shock and in-hospital cardiac mortality [13–15]. Although lytic therapy may be considered an option in selected cases, timely percutaneous coronary intervention is still the standard of care in terms of effective reperfusion and risk of intracranial hemorrhage [9, 10, 16].
Thus, how can we safely navigate between the Scylla of COVID-19 and the Charybdis of SHD and ACS? Many strategies might be envisioned, and several have been already implemented and recommended [17]. First, the concept of creating or adapting some hospitals to the care of COVID-19 patients only is reasonable and appropriate. However, this should not impede the ongoing activity of other institutions that may play a referral role in a hub and spoke system. Second, multi-institutional online registries should be implemented to track all patients with evident indications, in order to appropriately and timely prioritize, allocate, and treat them. Similarly, safe and high-quality management of SHD and ACS in the COVID-19 era requires careful planning and centralization of cases and procedures, using dedicated catheterization laboratories for suspected, probable, or confirmed COVID-19 patients. Of utmost importance to minimize exposure to coronavirus is also the systematic use of appropriate personal protection equipment while ensuring that all patients, relatives, and healthcare providers are preliminarily and periodically screened for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection. Nowadays, this may be easily accomplished with point-of-care instantaneous tests, most of which are based on inexpensive and sensitive polymerase chain reaction methods or measurement of antibody levels.
However, the simplest and most important recommendation should be made to patients and primary care physicians.: do not underestimate SHD and ACS risk, do not overlook symptoms, and consider appropriate and safe work-up of any patient with suspicious symptoms or sign of cardiovascular disease. Accordingly, enforce all measures that can increase appropriate diagnosis and management, including medical therapy, as pharmacology treatments are also being underused during the COVID-19 emergency. Indeed, given the current COVID-19 outbreak and the recognized high prevalence of SHD and ACS, patients may have both diseases. Conversely, considering them “simply” COVID-19 patients carries the risk of delivering inappropriate care, by not only overlooking cardiovascular diseases but also providing suboptimal COVID-19 management, given the established prognostic impact of cardiovascular and other comorbidities on COVID-19 outcome.
In conclusion, a proactive and vigilant stance on managing SHD and ACS is crucial, especially in the context of the COVID-19 pandemic, when the risk of overlooking severely sick patients or postponing life-saving treatments is high. If such corrective measures are not put into effect, we may expect in the near future an excess of avoidable fatalities indirectly due to COVID-19 but truly caused by cardiovascular diseases, as well as an exceedingly large number of patients with severe heart failure leading to shorter life expectancy, reduced quality of life, and increased healthcare cost.
Compliance with Ethical Standards
Conflict of Interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Giordano A, Biondi-Zoccai G, Frati G, editors. Transcatheter aortic valve implantation: clinical, interventional, and surgical perspectives. Cham: Springer Nature Publishing; 2019. [Google Scholar]
- 2.Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, ESC Scientific Document Group 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–2791. doi: 10.1093/eurheartj/ehx391. [DOI] [PubMed] [Google Scholar]
- 3.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–71. [DOI] [PMC free article] [PubMed]
- 4.Marullo AG, Cavarretta E, Biondi-Zoccai G, Mancone M, Peruzzi M, Piscioneri F, et al. Extracorporeal membrane oxygenation for critically ill patients with coronavirus-associated disease 2019: an updated perspective of the European experience. Minerva Cardioangiol. 2020. 10.23736/S0026-4725.20.05328-1. [DOI] [PubMed]
- 5.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323:1545. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 6.Biondi-Zoccai G, Landoni G, Carnevale R, Cavarretta E, Sciarretta S, Frati G. SARS-CoV-2 and COVID-19: facing the pandemic together as citizens and cardiovascular practitioners. Minerva Cardioangiol. 2020;68:61–4. [DOI] [PubMed]
- 7.Makkar RR, Fontana GP, Jilaihawi H, Kapadia S, Pichard AD, Douglas PS, Thourani VH, Babaliaros VC, Webb JG, Herrmann HC, Bavaria JE, Kodali S, Brown DL, Bowers B, Dewey TM, Svensson LG, Tuzcu M, Moses JW, Williams MR, Siegel RJ, Akin JJ, Anderson WN, Pocock S, Smith CR, Leon MB, Trial Investigators PARTNER. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med. 2012;366:1696–1704. doi: 10.1056/NEJMoa1202277. [DOI] [PubMed] [Google Scholar]
- 8.Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, Whisenant B, Grayburn PA, Rinaldi M, Kapadia SR, Rajagopal V, Sarembock IJ, Brieke A, Marx SO, Cohen DJ, Weissman NJ, Mack MJ, Investigators COAPT. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379:2307–2318. doi: 10.1056/NEJMoa1806640. [DOI] [PubMed] [Google Scholar]
- 9.ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988;2:349–360 [PubMed]
- 10.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 11.Biondi-Zoccai G, Peruzzi M, Abbate A, Gertz ZM, Benedetto U, Tonelli E, D'Ascenzo F, Giordano A, Agostoni P, Frati G. Network meta-analysis on the comparative effectiveness and safety of transcatheter aortic valve implantation with CoreValve or Sapien devices versus surgical replacement. Heart Lung Vessel. 2014;6:232–243. [PMC free article] [PubMed] [Google Scholar]
- 12.Kang DH, Park SJ, Lee SA, Lee S, Kim DH, Kim HK, Yun SC, Hong GR, Song JM, Chung CH, Song JK, Lee JW, Park SW. Early surgery or conservative care for asymptomatic aortic stenosis. N Engl J Med. 2020;382:111–119. doi: 10.1056/NEJMoa1912846. [DOI] [PubMed] [Google Scholar]
- 13.Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, et al. Disruptive modifications to cardiac critical care delivery during the COVID-19 pandemic: an international perspective. J Am Coll Cardiol. 2020 pii: S0735–1097(20)35002–6. 10.1016/j.jacc.2020.04.029. [DOI] [PMC free article] [PubMed]
- 14.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Rumoroso JR, López-Palop R, et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020. 10.24875/RECIC.M20000120.
- 15.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020 pii: S0735–1097(20)34913–5. 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed]
- 16.Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med. 2020 Mar 11. 10.1007/s00134-020-05993-9. [DOI] [PMC free article] [PubMed]
- 17.Welt FGP, Shah PB, Aronow HD, Bortnick AE, Henry TD, Sherwood MW, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC's Interventional Council and SCAI. J Am Coll Cardiol. 2020 pii: S0735–1097(20)34566–6. 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed]