Abstract
Patients with cleft lip and palate could develop dentofacial deformity characterized by malocclusion, midface retrusion, midline discrepancy and asymmetry. Cleft orthognathic surgery has evolved from the simple maxillary LeFort I advancement with correction of dental malocclusion to the current model of patient-centered approach focusing on skeletofacial reconstruction using computer-assisted diagnosis and planning. Three-dimensional imaging and surgical simulation have provided valuable information for facial aesthetics and surgical feasibility. Surgery-first approach and two-jaw orthognathic surgery have gradually become prevalent replacing the conventional method. A better dentofacial outcome is achieved with reduction of the burden of care.
Keywords: Unilateral cleft lip and palate, Dental occlusion, Facial aesthetics, Orthognathic surgery, Skeletofacial reconstruction, Midline
Skeletal mature patients with unilateral cleft lip and palate (UCLP) commonly present with dentofacial deformity requiring life-changing orthognathic surgery (OGS) [[1], [2], [3]]. These patients display a distinctive clinical pattern characterized by the combination of abnormalities in the dental occlusion, i.e. arch irregularities and tooth anomalies, and in the face, including different degrees of vertical, transverse, and anteroposterior disharmony and rotational asymmetry [[1], [2], [3], [4], [5]]. The potential combination of these cleft-related factors in a same patient poses additional challenges for OGS planning, as any misdiagnosis or mistreatment of the dento-skeletofacial deformity may limit the accomplishment of a successful functional occlusion and facial appearance outcome. Additionally, even minimal residual asymmetries would result in unsatisfied patients with the requirement for revisionary surgical management. This increases the number of surgeries and treatment time and also intensifies the burden of care, i.e., psychosocial and direct and indirect costs, in a population already marked by a high burden since the first months of life [1,6]. Therefore, the ideal cleft OGS treatment would be one that fundamentally corrects all possible occlusion and facial skeleton issues in a single intervention.
In this setting, the possibilities of OGS-related diagnosis and planning have meaningfully been strengthened by the ever-improving three-dimensional medical imaging [3,[7], [8], [9]]. However, some cleft-specific topics remain target of ongoing debates in the literature, with no universal consensus about an ideal cleft-OGS planning being reached to date. One practical example is the traditional teaching related to the accomplishment of alignment between the upper and lower incisors and facial midline during planning [10,11]. For patients with cleft-related absent maxillary lateral incisor associated with facial asymmetry of midline in nasal dorsum and tip, columella base, upper and lower lips, and chin areas, as well as contour in paranasal, cheek, mandibular, and chin regions, the combined adoption of this traditional surgical occlusion set up with the virtual movements of the maxillomandibular complex in six potential directions may result in an technically unfeasible surgery. To resolve this problem, the occlusion set up requires modifications or the facial deformity could only be partially corrected. Based on the delivery of three-dimensional computer-guided OGS care to a high volume of patients with UCLP in recent years, our team has perceived that patients could accept the possible discordance of upper and lower dental midlines or dental and facial midlines as a tactical measure to obtain a harmonic, proportional, symmetrical, and aesthetically pleasing facial outcome. This midline-based planning approach is part of strategic lessons learned over the years that takes a holistic view on the full cleft-related dento-skeletofacial deformities which have permitted this team to achieve satisfactory cleft OGS outcome, not only from a professional standpoint but also from the patients’ perspectives.
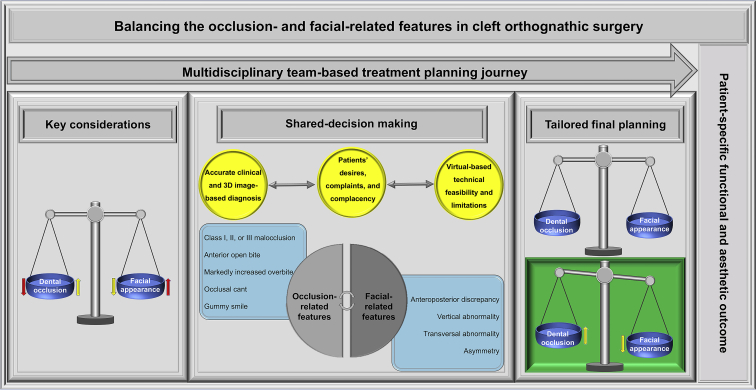
In this center, the patient-centered care principle [12] has been incorporated into the OGS care, with a shared decision-making process [13] between patients, families, and members of the team acting as a guide for essential discussions and judgments during the preoperative workup (Fig. 1). Three components, i.e., diagnosis, patients' opinions, and virtual surgery, were considered as crucial to formulate a personalized planning to meet patients' needs. A thorough and accurate diagnosis was established, encompassing the representative cleft-related malocclusion with anteroposterior discrepancy as well as further occlusion and facial features that likewise matter for patients. The patients' values, beliefs, and preferences regarding the occlusion and facial aspects were interactively considered to set realistic expectations about OGS and to define the degree of patients' satisfaction in accepting and dealing with specific limitations of orthodontic and surgical treatments. Considering the components of the diagnosis and patient's opinions, a focused-problem list was formulated to guide the virtual surgery. The bony segments were repositioned to the desired position by the surgeon and orthodontist, and a tailored planning was generated to assist the surgical execution based on the single-splint two-jaw surgery technique [3,[7], [8], [9],12,14].
Fig. 1.
Planning journey for cleft-OGS treatment. (Left box) Dental occlusion and facial appearance parameters are the key features to consider during planning, with the opposite arrows (yellow versus yellow and red versus red arrows) representing the possibilities of adjustments based on the shared decision-making process. (Central box) This “adjustable balance” should be “calibrated” for each patient through diagnosis of real dental occlusal, skeletal, and soft tissue deformities, characterization of patients' opinions (delineation of tolerance for limitations in occlusion- or facial-specific changes), and the establishment of virtual-based translational and rotational surgical movements (judgment of practicability and limitations of surgical execution). Unlike the traditional cleft-OGS treatment, a wide spectrum criterion of indication for OGS has been adopted in this patient-centered model, encompassing the cleft-related Class III malocclusion as well as several other occlusion and facial elements. (Right box) The final planning is tailored to meet patients' needs and opinions, pursuing the satisfactory equalization between dental occlusion and facial appearance status. (Green box) For a myriad of clinical instances, the yellow type of balance would be suitable to guide the planning, since this tactical modality will address the patients' facial appearance-related features (desires and complaints) with less (or not equal) relevance for his/her dental occlusion factor (complacency). The upper and lower dental midline element, for example, can be compromised to achieve a patient-specific outcome based on the balance between functional occlusion (mouth opening, biting, and chewing parameters) and facial appearance (aesthetic, harmony, proportion, and symmetry factors) but with no perfect positioning of all dental, nasal, lip, and chin midlines at the same alignment level.
The adoption of this customized planning based on the equilibrium between the actual diagnosis-specific needs, the particular patient's requests, and the virtual-based surgical feasibility and limitations has successfully and consistently resulted in balanced occlusion and facial outcomes. This has been revealed by the very low requisite for revisionary bone surgeries in patients with UCLP, even in challenging scenarios composed by cleft-related dental and arch abnormality and facial asymmetry. The increasing application of surgery-first model [12,[15], [16], [17]] in these patients has improved the OGS-related endpoints of treatment, with immediate enhancement of dental function and facial esthetics and overall treatment time reduction.
The therapeutic concept-related reflections derived from this perspective article provide a data-driven hypothesis generation to be tested in future investigations encompassing patient-reported and objective-based outcome measures [18,19]. This may form the basis to deliver optimized patient-centered care based on individualized patient-specific approaches around the globe.
In conclusion, the paradigm shift in the cleft orthognathic surgery has occurred focusing both on dental occlusion and facial appearance. The new model involves 3-dimensional planning, surgery-first approach and two-jaw procedure. Better surgical outcome with reduction of burden of care have been achieved.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Pai B.C.J., Hung Y.T., Wang R.S.H., Lo L.J. Outcome of patients with complete unilateral cleft lip and palate: 20-year follow-up of a treatment protocol. Plast Reconstr Surg. 2019;143:359e–367e. doi: 10.1097/PRS.0000000000005216. [DOI] [PubMed] [Google Scholar]
- 2.Cheong Y.W., Lo L.J. Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 2011;34:341–351. [PubMed] [Google Scholar]
- 3.Lonic D., Pai B.C., Yamaguchi K., Chortrakarnkij P., Lin H.H., Lo L.J. Computer-assisted orthognathic surgery for patients with cleft lip/palate: from traditional planning to three-dimensional surgical simulation. PLoS One. 2016;11 doi: 10.1371/journal.pone.0152014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu T.T., Chen P.K., Lo L.J., Cheng M.C., Ko E.W. The characteristics and distribution of dental anomalies in patients with cleft. Chang Gung Med J. 2011;34:306–314. [PubMed] [Google Scholar]
- 5.Lo L.J., Wong F.H., Chen Y.R., Wong H.F. Mandibular dysmorphology in patients with unilateral cleft lip and cleft palate. Chang Gung Med J. 2002;25:502–508. [PubMed] [Google Scholar]
- 6.Meazzini M.C., Capello A.V., Ventrini F., Autelitano L., Morabito A., Garattini G. Long-Term follow-up of UCLP patients: surgical and orthodontic burden of care during growth and final orthognathic surgery need. Cleft Palate Craniofac J. 2015;52:688–697. doi: 10.1597/12-211. [DOI] [PubMed] [Google Scholar]
- 7.Wu T.Y., Denadai R., Lin H.H., Ho C.T., Lo L.J. The outcome of skeletofacial reconstruction with mandibular rotation for management of asymmetric skeletal class III deformity: a three-dimensional computer-assisted investigation. Sci Rep. 2019;9:13337. doi: 10.1038/s41598-019-49946-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ho C.T., Lin H.H., Liou E.J., Lo L.J. Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: a qualitative and quantitative study. Sci Rep. 2017;7:40423. doi: 10.1038/srep40423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin H.H., Chang H.W., Wang C.H., Kim S.G., Lo L.J. Three-dimensional computer-assisted orthognathic surgery: experience of 37 patients. Ann Plast Surg. 2015;74:S118–S126. doi: 10.1097/SAP.0000000000000455. [DOI] [PubMed] [Google Scholar]
- 10.Arnett G.W., Bergman R.T. Facial keys to orthodontic diagnosis and treatment planning-Part II. Am J Orthod Dentofacial Orthop. 1993;103:395–411. doi: 10.1016/s0889-5406(05)81791-3. [DOI] [PubMed] [Google Scholar]
- 11.Jerrold L., Lowenstein L.J. The midline: diagnosis and treatment. Am J Orthod Dentofacial Orthop. 1990;97:453–462. doi: 10.1016/S0889-5406(05)80025-3. [DOI] [PubMed] [Google Scholar]
- 12.Denadai R., Lo L.J. Paradigm shift in skeletofacial reconstruction: changing traditional cleft care. Plast Reconstr Surg. 2020;145:886e–889e. doi: 10.1097/PRS.0000000000006692. [DOI] [PubMed] [Google Scholar]
- 13.Berger Z.D., Brito J.P., Ospina N.S., Kannan S., Hinson J.S., Hess E.P. Patient centred diagnosis: sharing diagnostic decisions with patients in clinical practice. BMJ. 2017;359:j4218. doi: 10.1136/bmj.j4218. [DOI] [PubMed] [Google Scholar]
- 14.Chortrakarnkij P., Lonic D., Lin H.H., Yamaguchi K., Kim S.G., Lo L.J. A modified technique of mandibular ramus sagittal split osteotomy for prevention of inferior alveolar nerve injury: a prospective cohort study and outcome assessment. Ann Plast Surg. 2017;78:S108–S116. doi: 10.1097/SAP.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 15.Huang C.S., Hsu S.S., Chen Y.R. Systematic review of the surgery-first approach in orthognathic surgery. Biomed J. 2014;37:184–190. doi: 10.4103/2319-4170.126863. [DOI] [PubMed] [Google Scholar]
- 16.Yu C.C., Chen P.H., Liou E.J., Huang C.S., Chen Y.R. A Surgery-first approach in surgical-orthodontic treatment of mandibular prognathism-a case report. Chang Gung Med J. 2010;33:699–705. [PubMed] [Google Scholar]
- 17.Seo H.J., Denadai R., Pai B.C.J., Lo L.J. Digital occlusion setup is quantitatively comparable to the conventional dental model approach: characteristics and guidelines for orthognathic surgery in patients with unilateral cleft lip and palate. Ann Plast Surg. 2019 doi: 10.1097/SAP.0000000000002079. [in press] [DOI] [PubMed] [Google Scholar]
- 18.Su Y.Y., Denadai R., Ho C.T., Lai B.R., Lo L.J. Measuring patient-reported outcomes in orthognathic surgery: linguistic and psychometric validation of the Mandarin Chinese version of FACE-Q instrument. Biomed J. 2020;43:62–73. doi: 10.1016/j.bj.2019.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denadai R., Chou P.Y., Su Y.Y., Lo C.C., Lin H.H., Ho C.T. Facial appearance and psychosocial features in orthognathic surgery: a FACE-Q- and 3D facial image-based comparative study of patient-, clinician-, and lay-observer-reported outcomes. J Clin Med. 2019;8 doi: 10.3390/jcm8060909. [DOI] [PMC free article] [PubMed] [Google Scholar]