Abstract
Objective
To ensure that a standardized method of continuous symptom monitoring was available to hospice patients enrolled at our institution.
Patients and Methods
The Palliative/End-of-Life/Assessment/Care Coordination/Evidence-Based Program (PEACE) seeks to enhance the provision of hospice care through symptom control and patient support. We conducted a quality improvement initiative between November 1, 2015, and March 31, 2017, following Define-Measure-Analyze-Improve-Control methodology to improve hospice care at a rural hospice. The gap in our current hospice model was a standardized method of continuous symptom monitoring. We aimed to explore ways in which technology-assisted care coordination could enhance end-of-life and hospice care. We measured continuous symptom assessments through co-developed condition management protocols (CMPs), technology-assisted care pathways (TACPs), nursing visits, length of stay, respite days, and satisfaction survey data from patients, caregivers, and hospice staff. At baseline, no continuous symptom monitoring was being performed. Baseline data for our enrolled population was compared with data from patients who were eligible, but opted out.
Results
We monitored 50 patients using CMP and TACP. The mean ± SD number of skilled nursing visits per patient in the enrolled population compared with those who were eligible but opted out was 13.7±7.6 vs 14.2±10.5, respectively. In response to the survey question, “Because of the overall program, I felt supported and confident at home,” 74% (37 of 50) of patients and caregivers answered, “always.”
Conclusion
PEACE enhanced hospice care through symptom control and patient support through CMP and TACP. PEACE is a unique and feasible care platform for hospice patients, with high patient and caregiver satisfaction.
Abbreviations and Acronyms: CMP, condition management protocol; PDSA, Plan-Do-Study-Act; PEACE, Palliative/End of Life/Assessment/Care Coordination/Evidence Based Program; QI, quality improvement; TACP, technology-assisted care pathway; WI, Wisconsin
There is a growing interest in the way that care is provided for the 1.43 million US patients using hospice care1 and 6 million Americans who could benefit from accessing palliative care services.2 Facilitating care transitions, the preferred location of care, and designating the primary objective of care delivery as palliative or end of life, as appropriate to an individual patient’s clinical circumstances, can reduce unnecessary intensive care unit admission, avoid other in-patient hospital stays, and diminish high rates of emergency department visits3, 4, 5 for the purpose of assessing and managing symptoms.
Of the 2.5 million people who die annually in the United States,6 most would prefer to die in their own homes.7 However, one-third of these people die in short-stay general hospitals.8 In addition, death in the hospital is associated with poorer quality of life and increased risk for psychiatric illness among bereaved caregivers.9 These data suggest that there are significant opportunities to improve the humanity of end-of-life care and reduce its costs by educating patients and caregivers about palliative care and hospice services, offering strategies for self-management of symptoms,10 and increasing accessibility to palliative care and hospice at the end of life,11 preferably from nonhospital settings.
Telehealth involves the use of information and telecommunication technologies to provide care in situations in which the clinician and patient are separated by geographic distance.9 A systematic review of the evidence for providing elements of hospice care through information and telecommunication technologies (telehospice) highlights the relevance of exploring this mode of hospice care provision, a medium-strength level for the scientific evidence to support this approach, and the need for additional outcome-focused clinical research in this area.12 In November 2015, Mayo Clinic, a leading medical institution,13 and Medtronic, a leader in its field for engineering innovation,14 entered into a collaborative agreement to explore ways in which technology-assisted care coordination can enhance palliative and hospice care.
The vision of this collaboration is one of combining leading medical and engineering institutions to create a unique technology-assisted care coordination platform that ensures eligible patients and caregivers access to high-quality care. Actualizing this vision requires creating evidence-based clinical care pathways that connect patients and clinical teams across the continuum of care, supporting patient self-management, and making care available in the least restrictive and most convenient settings for patients and staff. Having provided the background and rationale for this quality improvement (QI) program, we describe its implementation at the Mayo Clinic Health System in Eau Claire, Wisconsin (WI), between November 1, 2015, and March 31, 2017; its subsequent evaluation; and applicable recommendations.
Patients and Methods
Define Project
Our QI project was reviewed using direct verbal communications and e-mail with key stakeholders, including hospice, palliative care, nurse administrators, administrators, remote monitoring experts, and leadership from Mayo Clinic and Medtronic. Their suggestions and feedback were included in the development of the project and protocols. Our target population was hospice patients admitted to the Mayo Clinic Health System hospice in Eau Claire, WI.
Our initial assessment through listening sessions with hospice stakeholders revealed that many stakeholders were interested in incorporating proactive symptom monitoring for hospice patients. Hospice patients and their caregivers have complex and time-sensitive needs in often progressively worsening clinical situations over days to weeks. These patients and caregivers often reside at home, sometimes far removed from readily available access to a professional from the hospice team.
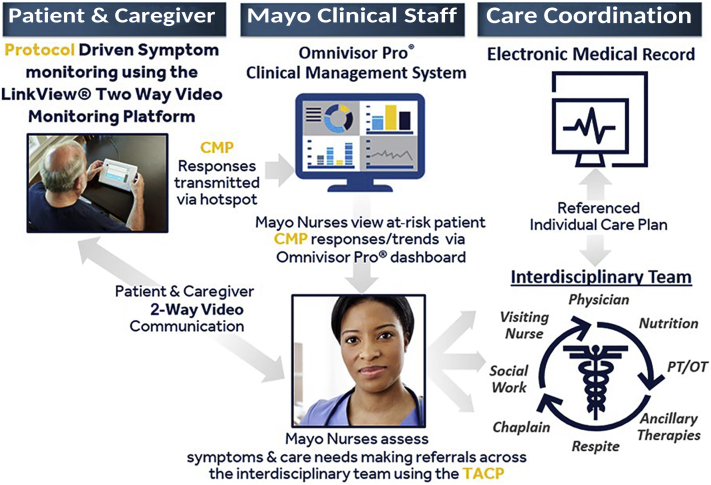
The gap in our current hospice care model is the lack of a standardized method of proactive continuous symptom monitoring. Our project team from Medtronic and Mayo Clinic, consisting of hospice nurses, hospice physicians, administrators, and experts in technology-assisted care pathways, developed a condition management protocol (CMP) and technology-assisted care pathway (TACP) on an existing US Food and Drug Administration–approved Medtronic remote patient monitoring platform, LinkView, and cloud-based software application, Omnivisor Pro, to provide proactive continuous symptom monitoring. The CMP is an algorithmic series of questions and education to assess and support the patient’s condition. CMP is a way of proactively seeking information about symptoms to intervene early. TACP is an algorithmic approach to guide nursing assessment and interventions based on alerts from the CMP.
Our partnership included the rural area in and surrounding our regional hospice in Eau Claire, WI. Our project team from Mayo Clinic and Medtronic worked to define common interests, develop working teams and framework, and develop the CMP and TACP with the associated staff education, training, and implementation strategy from November 1, 2015, to March 31, 2017.
The development led to an interactive platform to proactively assess patients’ symptoms and notify the hospice care team if symptoms require intervention. The CMP and TACP were symptom focused and were neither disease-specific nor dependent on patient functional status. The program was designed to support home hospice teams to proactively recognize (CMP) and address (TACP) end-of-life care concerns, thereby enhancing care coordination and ensuring timely compassionate care in the home. The platform allowed for video visits with a nurse at the hospice office. Telephone interaction was also possible following notification through the CMP. The entire platform is called PEACE (Palliative/End of Life/Assessment/Care Coordination/Evidence Based Program; Figure 1).
Figure 1.
Palliative/End-of-Life/Assessment/Care Coordination/Evidence-Based Program (PEACE) model overview. CMP = condition management protocol; PT/OT = physical therapy/occupational therapy; TACP = technology-assisted care pathway.
Our aim was to improve symptom monitoring in a cohort of up to 50 patients from November 1, 2015, to March 31, 2017, without increasing nursing visits as a counterbalance measure. At baseline, no proactive continuous symptom monitoring was being performed.
Project Measurement
We monitored and documented the number of patients enrolled in PEACE weekly during Plan-Do-Study-Act (PDSA) cycles.15 A tally sheet was used to capture weekly and running enrollment status, reasons for discontinuation of PEACE, days enrolled in PEACE, CMP alerts, communications, TACP interventions, hospice length of stay, and interdisciplinary team member visits. We also describe secondary outcomes of patient demographics, nursing visits, length of stay, and satisfaction survey data from patients, caregivers, and hospice staff. We compared baseline data from our enrolled population with data from patients who were eligible but opted out.
Our counterbalance measure was monitoring of nursing visits to ensure that the PEACE process did not increase the nursing workload. Additionally, we surveyed our patients and staff on their experience using PEACE and held a focus group with our staff to better understand areas of improvement for the refinement of PEACE.
Results
Analyze the Project
The QI method primarily used was the PDSA cycle method. We created a plan by obtaining data and listening to key stakeholders. The plan was carried out through the implementation of the project. We used PDSA cycles weekly throughout the implementation of the project to refine our processes. These PDSA cycles were documented in a PEACE Pilot PDSA chart with elements: count, data element, measure methodology, data source, review frequency, and approach. This chart was completed weekly by the PEACE pilot team. We used PDSA cycles weekly throughout the implementation of the project to refine our processes. This proved to be the most important aspect of our project and informed the improvement process and our most key lessons learned while proactively monitoring symptoms in hospice patients at home.
Improvement Intervention
Our project team conducted an on-site formal didactic session that all stakeholders attended. Baseline measurement of proactive continuous symptom monitoring was 0. Because PEACE required equipment, connectivity, and an extra layer of support in the home, patients were given an option to participate or not. Two hundred thirty-two patients were enrolled in hospice during the improvement phase. One hundred eighty-two were not eligible for intervention or declined or were in non PEACE conducive situations for the following reasons: residing in a facility, 108 (59.3%); death, 25 (13.7%); caregiver or patient declination, 19 (10.4%); and other, 30 (16.5%). A total of 99 patients were therefore eligible for the PEACE protocol. To avoid the burden of training multiple nursing facility staff, patients residing in health care institutions were not able to participate in this initial improvement effort. Other reasons for ineligibility included inability to use the device, no cellular coverage, or current conditions not conducive to the use of PEACE . Fourteen of 50 (28.0%) patients used the program through the end of life.
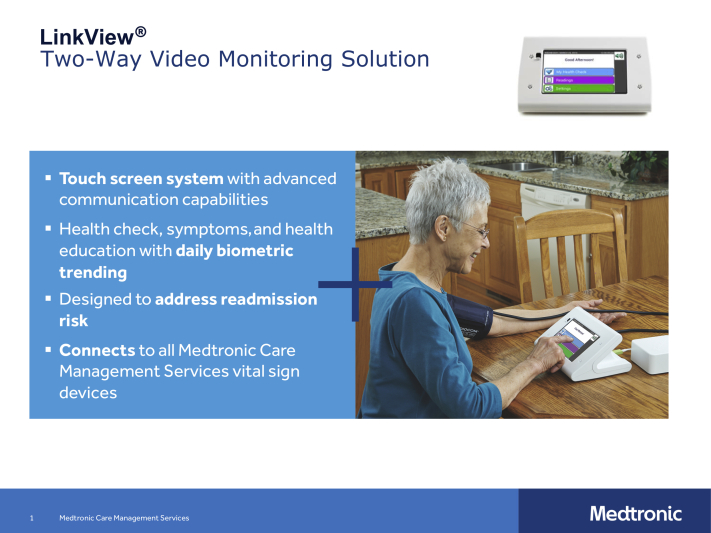
During the course of the intervention, we conducted regular staff check-ins in the manner of PDSA cycles, gathering real-time continuous feedback. We then incorporated those suggestions into the next week and reevaluated. The identified patients received a tablet-type device that allowed them to answer questions based on the length of time they had been using the device (Figure 2). For example, day 1 questions differed slightly from day 2 or day 3 questions. The clinical team determined the cadence of the questions based on experience of frequency of patient issues. Questions regarding pain were asked daily, and questions regarding financial difficulty were asked less frequently. Questions asked regarded pain, dyspnea, cough, nausea, vomiting, oral intake, elimination, anxiety, depression, stress/coping, activity, weakness, activities of daily living, delirium, caregiver capacity, spiritual concerns, advance directive, finance concerns, and I need a call from a nurse. Symptom scoring for the system was set to alert for a symptom score of 6 points or higher, symptoms tagged as acute, and biometric out of range (temperature ≥101°F). Answers to the questions on the system fed a triage system, which indicated times when follow-up from the clinical team was necessary. Positive response to pain or other physical symptom questions resulted in nurse follow-up, and positive responses to other types of questions triggered other team member follow-up (spiritual care or social work).
Figure 2.
LinkView®: 2-way video monitoring solution.
We enrolled 50 of 99 (50.5%) patients during this QI initiative. Participants had a mean ± SD age of 75.7±14.2 years, 45.9% (34 of 99) were men, and 35.1% (26 of 99) were women (Table). Data pulled from Omnivisor Pro demonstrated that participants complied daily with the protocol use on average 45.7% of the time. The mean ± SD number of communications per patient was 3.6±6.2. These ranged from 2 to 76 alerts per week. Almost 14% of alerts were acute; 61.1%, a symptom score alert; and 24.9%, a symptom variance alert. The mean ± SD number of alerts per patient during an enrollment period was 7.5±15.7. There were 1 to 29 TACP interventions per week, and on average 4.1±9.0 per patient. The most common reason for a TACP intervention was nausea and vomiting (19.5%), followed by dyspnea (13.2%) and pain (10.8%). Every patient we admitted onto hospice services during the time frame of the project was entered/enrolled in Omnivisor Pro. If they did not meet the inclusion criteria (listed previously) and/or they refused to participate in the project, we “disenrolled” them immediately and identified the reason for disenrollment. This data set formed the comparator data set of eligible patients who opted out of the PEACE process.
Table.
Clinical Characteristics
| Characteristic | Eligible, Enrolled | Eligible, Declined |
|---|---|---|
| Sample size, no. | 50 | 24 |
| Age (y), mean ± SD | 75.7±14.2 | 74.6±12.0 |
| Hospice length of stay routine days | ||
| Mean ± SD | 55.2±40.3 | 44.0±35.5 |
| Median (range) | 42.5 (3.0-157.0) | 35.5 (3.0-127.0) |
| Hospice location of care, mean ± SD | ||
| Respite days | 0.3±1.1 | 0.2±0.7 |
| In-patient days | 0.0±0.2 | 0.5±1.9 |
| Skilled nurse visits, mean ± SD | ||
| Total visits | 13.7±7.6 | 14.2±10.5 |
| 7 am-3 pm visits | 12.0±7.3 | 11.8±8.9 |
| 3 pm -11 pm visits | 1.5±1.9 | 1.9±2.3 |
| 11 pm-7 am visits | 0.4±0.6 | 0.5±0.7 |
| Interdisciplinary team visits, mean ± SD | ||
| Total visits | 31.3±21.4 | 26.1±20.9 |
| 7 am-3 pm visits | 28.9±20.6 | 23.1±18.9 |
| 3 pm-11 pm visits | 2.1±2.5 | 2.5±2.7 |
| 11 pm-7 am visits | 0.4±0.7 | 0.6±0.8 |
The mean ± SD days that participants participated in the protocol was 31.9±27.8, median of 24, and range of 4 to 147 days. The mean ± SD number of skilled nurse visits per patient in the enrolled population was 13.7±7.6 compared with 14.2±10.5 for those who opted out. Nursing visits did not increase during our QI program.
The mean ± SD length of stay in hospice was 50.5±40.2 days for PEACE participants vs 44.8±35.2 days for those who opted out; the median values were 42.5 and 35.5 days, respectively. Thirty-two of 232 (13.7%) patients died before participating in PEACE. PEACE participants spent 0.0±0.2 day in the hospital compared with 0.5±1.9 for those who opted out, with 0.3±1.1 and 0.2±0.7 respite days, respectively.
Twenty (40%) patients and caregivers decided to discontinue PEACE early, with median lengths of participation of 22 and 15 days, respectively. Caregiver and patient choice to discontinue was 11 (22%) and 9 (18%), respectively. Other reasons were death (14 [28%]), pilot discontinuation (11 [22%]), and facility placement (3 [6%]). In response to the survey question, "Because of the overall program, I felt supported and confident at home," 37 (73.3%) patients and caregivers answered, “Always.”
Control Summary
Baseline, implementation, and measurement data were communicated to the stakeholders during each PDSA cycle and following the intervention. Communication and regular meetings to discuss these data and QI continue to the present. Data monitoring continued during the intervention period, and ongoing conversations are determining process refinements based on PDSA and focus group findings to determine full-scale implementation and sustainability.
The operational control of the process could revolve around many of the intermediate outcomes that we have evaluated, and more than 1 would likely be useful. For example, the percentage of enrolled hospice patients making use of the technology, coupled with the number of alerts in relation to the control limits, could be monitored to ensure that the process is working and effective. This is all part of our ongoing process development.
Discussion
We proactively and continuously monitored symptoms in 50 enrolled hospice patients at home without increasing nursing visits with overall good patient, family, and staff satisfaction. PEACE participants also experienced longer median lengths of stay in hospice than the national average of 17 days,16 which may be attributable to selection bias or local identification practice standards. It may also reflect a selection bias toward patients who were not imminently about to die because many patients were referred at a late stage and may therefore have opted not to have the added burden of using technology. In the absence of an industry partner willing to refine the technology, the program has not progressed and is not likely to grow. We are looking for an industry partner to take this on.
Timing of Introduction
The first week of hospice enrollment is too busy to accommodate the introduction of a proactive continuous symptom-monitoring program. By about day 5, patients and caregivers have acclimated to the hospice program and may be ready to be introduced to the PEACE technology. From our experience, a well-trained nurse champion with a concise message is vital to managing the process. Educating staff with just-in-time methods may improve the use of new technologies. Some patients will die in the first days after hospice enrollment, and finding solutions to offer PEACE to them in their rapidly changing clinical condition remains a challenge.
Personalized CMP
The patients and families may benefit more from CMP algorithms, tailored to the specific disease state and functional status of the patient. Additionally, a nuanced range of answer options, rather than simply yes or no, and direct questioning regarding the need for a visit from a nurse may enhance the CMP. Patients were offered a call from a nurse each day. Our teams also see benefit in incorporating the patient’s medical chart into the monitoring system, with specific attention to medications and diagnoses. The standard algorithmic approach of the CMP was believed to be beneficial to the nurse triage lines.
Use Available Technology
The desire to access the CMP on existing mobile technology already used by the patient and family was a recurrent theme and an area of active development. This will allow for patients and their families to connect for video conference with TACP administration from any site. Additionally, this would provide the flexibility to use existing technologies in institutional settings.
Conclusion
Offering PEACE to patients as part of a comprehensive end-of-life care program demonstrated the feasibility of using a technology-assisted care coordination program to support end-of-life care in home settings, and although this quality initiative was not a controlled study, it suggests that patients had a longer median length of hospice care than the national hospice median; fewer days in the hospital; proactive continuous symptom assessment, with nausea, dyspnea, and pain as the main symptoms reported; and high levels of patient and caregiver satisfaction. Digital health technologies may therefore be a valuable adjunct to end-of-life care in community settings with a particular role in care coordination and providing continuous quality improvement data. Further controlled studies are recommended to determine the overall efficacy of this intervention and better define patient selection criteria because withdrawal of patients from the program when death was imminent suggests that use of such an interactive self-management tool may then be an unnecessary burden. In addition, use of patients' own technology platforms, such as tablets, televisions, and smart phones, may streamline this process and improve uptake.
Acknowledgments
Editing, proofreading, and reference verification were provided by Scientific Publications, Mayo Clinic. Mayo Clinic does not endorse specific products or services included in this article.
Footnotes
Grant Support: The project was supported in part by Medtronic Care Management Services and Mayo Clinic. This was a Mayo/Medtronic collaboration project. The statistical analysis, data interpretation, and manuscript preparation were performed by Mayo researchers. Medtronic provided financial support to partially offset the cost to execute the project as well as resources and support for development and deployment of the project’s care pathways. Medtronic had no impact on the data analysis or decision to publish the findings.
Potential Competing Interests: The authors report no competing interests.
Data Previously Presented: These data were presented in abstract form: Ingram C, Bruce C, Shadbolt E, et al. Let There Be PEACE: Improving Continuous Symptom Monitoring in Hospice Patients. J Pain Symptom Manage. 2018;56(6):e103.
References
- 1.National Hospice and Palliative Care Organization Hospice Care Overview for Professionals. Hospice facts and figures. 2018. https://www.nhpco.org/research
- 2.Hallowell N. End-of-life palliative care. Today’s Geriatr Med. 2014;7(5):16. [Google Scholar]
- 3.Gade G., Venohr I., Conner D., et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190. doi: 10.1089/jpm.2007.0055. [DOI] [PubMed] [Google Scholar]
- 4.Dudgeon D.J., Knott C., Eichholz M., et al. Palliative Care Integration Project (PCIP) quality improvement strategy evaluation. J Pain Symptom Manage. 2008;35(6):573–582. doi: 10.1016/j.jpainsymman.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrison R.S., Dietrich J., Ladwig S., et al. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff (Millwood) 2011;30(3):454–463. doi: 10.1377/hlthaff.2010.0929. [DOI] [PubMed] [Google Scholar]
- 6.Murphy S.L., Xu J., Kochanek K.D., Division of Vital Statistics Deaths: preliminary data for 2010. Natl Vital Stat Rep. 2012;60(4):1–51. [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Service. Centers for Disease Control and Prevention. National Center for Health Statistics. Health, United States, 2010 . With Special Feature on Death and Dying. Government Printing Office; Hyattsville, MD: 2011. [Google Scholar]
- 8.Tang S.T. When death is imminent: where terminally ill patients with cancer prefer to die and why. Cancer Nurs. 2003;26(3):245–251. doi: 10.1097/00002820-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Wright A.A., Keating N.L., Balboni T.A., Matulonis U.A., Block S.D., Prigerson H.G. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol. 2010;28(29):4457–4464. doi: 10.1200/JCO.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorig K.R., Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 11.Bailey D.E., Jr., Steinhauser K., Hendrix C., Tulsky J.A. Pairing self-management with palliative care: intervening in life-limiting illness. J Nurs Healthc Chronic Illn. 2011;3(1):1–3. doi: 10.1111/j.1752-9824.2011.01083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliver D.P., Demiris G., Wittenberg-Lyles E., Washington K., Day T., Novak H. A systematic review of the evidence base for telehospice. Telemed J E Health. 2012;18(1):38–47. doi: 10.1089/tmj.2011.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nisen M. Mayo Clinic CEO: here's why we've been the leading brand in medicine for 100 years. 2013. https://finance.yahoo.com/news/mayo-clinic-ceo-heres-why-155300485.html
- 14.Bergstein B. 50 Smartest companies 2014. https://www.technologyreview.com/s/524671/50-smartest-companies-2014/
- 15.The W. Edwards Deming Institute PDSA cycle. https://deming.org/explore/p-d-s-a
- 16.Medicare Payment Advisory Commission Report to Congress: Medicare payment policy. 2016. http://www.medpac.gov/docs/default-source/reports/march-2016-report-to-the-congress-medicare-payment-policy.pdf