A few weeks after the first Italian case of person‐to‐person transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), 1 the Italian government promulgated a Decree Law imposing a general lockdown, aimed at reducing the spread of coronavirus disease 2019 (COVID‐19). Among the restrictions affecting the healthcare system, outpatient clinics and day services were suspended, and in‐ward access was granted only for urgent procedures. On the one hand, this reduced the risk of in‐hospital COVID‐19 spread, but on the other hand this led to a marked decrease in the assistance for chronic diseases – i.e. heart failure (HF).
The aims of the present report were to investigate whether a telemedicine service (TMS), expressly set up by our HF university tertiary referral centre 2 during the COVID‐19 outbreak, impacts on HF outcomes (i.e. composite of HF hospitalization/death), and to compare outcomes with the same period (11 March–4 May) of the previous year, when a TMS was not available.
Our TMS included two phone numbers, active 24/7, with the possibility of chat and video‐conference services available with the most popular smartphone applications; an email address was available too. Telemedicine visits were not scheduled, and access to the TMS was done on a voluntary basis by the patients, who were advised to use the TMS for any clinical necessity. However, if the attending physician deemed a further access necessary, patients were encouraged to contact us again. All patients were advised to follow all recommended measures to prevent COVID‐19 transmission (e.g. social distance, frequent handwashing, use of face masks in public places, self‐isolation). With regard to HF treatment, the maintenance of all prescribed medications was recommended. 3 Notably, after a few days, the European Society of Cardiology (ESC) published a statement against the discontinuation of angiotensin‐converting enzyme inhibitors (ACEi)/angiotensin receptor blockers (ARBs)/angiotensin receptor–neprilysin inhibitors (ARNI) 4 ; further, recent evidence from the literature showed the lack of negative effects of ACEi/ARBs/ARNI on COVID‐19 infection and severity. 5 At the end of the study period, all patients were contacted to get information about outcome.
Overall, 103 patients participated in the present study; outcomes were compared with data from 104 HF patients attending our unit in the same period in 2019 (Table 1 ). From 11 March to 4 May 2020, 58% of patients made at least one TMS access, mostly by phone call (64.2%), followed by chat service (33.6%). Overall, 51% of contacts led to a clinical decision (adjustment of diuretic doses, change in blood pressure‐lowering drugs, rate controls, anticoagulation management, and other) (Figure 1 ). Five patients experienced the primary endpoint; specifically, three patients were hospitalized (one for non‐ST‐elevation acute coronary syndrome, one for pulmonary oedema, and one for defibrillator battery replacement), and two patients died [both in end‐stage HF before the lockdown (New York Heart Association class IV) who died from sudden cardiac death]. Notably, none of our HF patients got COVID‐19. Pearson's chi‐square and Fisher's exact tests showed that patients in the 2019 cohort (when the TMS was not available) were more likely to experience the primary outcome compared with the cohort having access to the TMS [n = 207; X2 (degree of freedom 1) 10.699, P = 0.001]. A significant difference was observed in HF hospitalizations (P = 0.001) whereas no differences were observed in mortality.
Table 1.
Demographic characteristics at baseline, telemedicine data, and outcomes
| Variables | 2020 Cohort (n = 103) | 2019 Cohort (n = 104) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 68 ± 12.7 | 68 ± 11.4 | NS |
| Sex (male/female) | 84/19 | 84/20 | NS |
| NYHA class (I–II/III–IV) | 66/37 | 65/39 | NS |
| Aetiology (ischaemic) (%) | 53 | 51 | NS |
| Years of disease | 6 [1–12] | 5 [1–13] | NS |
| Systolic blood pressure (mmHg) | 123 ± 15.6 | 122 ± 6.4 | NS |
| Diastolic blood pressure (mmHg) | 78 ± 9.8 | 79 ± 7.5 | NS |
| BMI (kg/m2) | 29.8 ± 6.3 | 29.7 ± 5.2 | NS |
| eGFR (mL/min) | 80 [53–118] | 81[49–112] | NS |
| ICD (%) | 45.8 | 43.9 | NS |
| CRT (%) | 14.6 | 13.4 | NS |
| LVEF (%) | 34.1 [28.8–39.3] | 34.8 [29.2–39.8] | NS |
| LVEDVi (mL/m2) | 88.5 [74.3–114.1] | 87.6 [72.8–111.9] | NS |
| LVESVi (mL/m2) | 57.9 [46.9–79.5] | 57.3 [46.7–77.3] | NS |
| NT‐proBNP (pg/mL) | 536 [180–1621] | 600 [201–1815] | NS |
| Medication (%) | |||
| Beta‐blockers | 92.3 | 91.7 | NS |
| ACEi/ARB/ARNI | 89 | 88 | NS |
| MRA | 49 | 50 | NS |
| Loop diuretics | 74.7 | 75.1 | NS |
| Telemedicine | |||
| Total no. of accesses | 127 | – | – |
| Patients with at least 1 access, n (%) | 60 (58) | – | – |
| Type of access, n (%) | |||
| Phone call | 82 (64.2) | – | – |
| Chat service | 43 (33.6) | – | – |
| Video | 3 (2.2) | – | – |
| 0 (0) | – | – | |
| Patients needing at least one clinical intervention, n (%) | 31 (52) | – | – |
| No. of clinical interventions, n (%) | 65 (51) | ||
| Type of clinical intervention, n | |||
| Loop diuretic dose change | 23 | – | – |
| Blood pressure management | 10 | – | – |
| Rate control | 6 | – | – |
| Anticoagulation management | 6 | – | – |
| Other a | 20 | – | – |
| Outcome, n | |||
| Composite HF hospitalization/death | 5 | 21 | 0.001* |
| HF hospitalizations | 3 | 18 | 0.001* |
| Deaths | 2 | 3 | NS |
Data are expressed as mean ± standard deviation, or median [interquartile range] unless otherwise specified.
ACEi, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; ARNI, angiotensin receptor–neprilysin inhibitor; BMI, body mass index; CRT, cardiac resynchronization therapy; eGFR, estimated glomerular filtration rate (Chronic Kidney Disease Epidemiology Collaboration formula); HF, heart failure; ICD, implantable cardioverter‐defibrillator; LVEDVi, left ventricular end‐diastolic volume index; LVEF, left ventricular ejection fraction; LVESVi, left ventricular end‐systolic volume index; MRA, mineralocorticoid receptor antagonist; NT‐proBNP, N‐terminal pro B‐type natriuretic peptide; NYHA, New York Heart Association.
P < 0.01.
Other interventions: antibiotics management, pain management, general advise.
Figure 1.
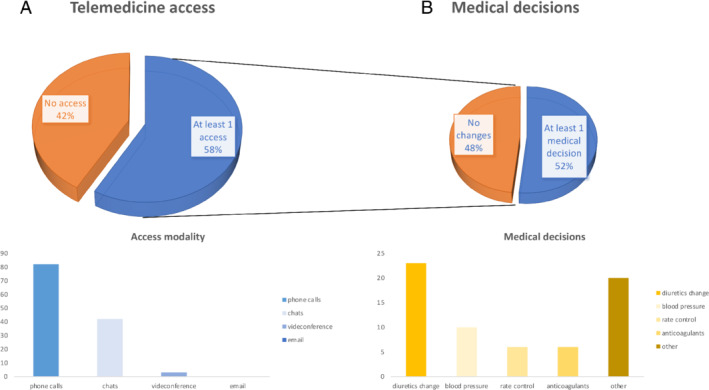
(A) Patients who accessed to the telemedicine service and access modality. (B) Outcome of the accesses performed and medical decisions.
This investigation represents the first study evaluating the utility of a TMS during the lockdown due to the COVID‐19 outbreak in Italy; using commonly available technologies (analogic phones, smartphones, apps) our team was able to offer a continuous service to all our HF patients.
It has been described a decrease of acute coronary syndrome‐related hospitalization rates in Italy during the COVID‐19 outbreak, 6 , 7 suggesting that several patients experienced a poor outcome because they did not access to the healthcare system. We provided a TMS that allows our patients to have direct access to the healthcare system, observing a significant reduction of the primary endpoint if compared to the same period of the previous year, supporting its use to increase the value of health care. 8 Further, our findings support the recent statement from the Heart Failure Society of America that strongly suggests the use of telemedicine for HF management during the COVID‐19 outbreak, 9 in line with the ESC advice. 4 Notably, it has recently been stated that ‘it is a great shame that home telemonitoring was not already routine before the pandemic struck’. 10
In order to avoid any social disparities (e.g. TMS accessibility only to people with available technologies and/or capacities to use the service), on purpose we based our telemedicine system mostly on phone calls.
In conclusion, our TMS allows follow‐up of HF patients also during the COVID‐19 lockdown, with a positive impact on HF outcome; the present report confirms telemedicine as a valuable tool in HF management and shows for the first time its feasibility during the COVID‐19 outbreak.
Funding
Dr Salzano receives research grant support from CardioPath, Department of Advanced Biomedical Sciences, Federico II University, Naples, Italy, and UniNA and Compagnia di San Paolo in the frame of the STAR (Sostegno Teritoriale alla Attività di Ricerca) programme.
Conflict of interest: none declared.
References
- 1. Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R. The response of Milan's emergency medical system to the COVID‐19 outbreak in Italy. Lancet 2020;395:e49–e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bossone E, Arcopinto M, Iacoviello M, Triggiani V, Cacciatore F, Maiello C, Limongelli G, Masarone D, Perticone F, Sciacqua A, Perrone‐Filardi P, Mancini A, Volterrani M, Vriz O, Castello R, Passantino A, Campo M, Modesti PA, De Giorgi A, Monte I, Puzzo A, Ballotta A, Caliendo L, D'Assante R, Marra AM, Salzano A, Suzuki T, Cittadini A; TOSCA Investigators . Multiple hormonal and metabolic deficiency syndrome in chronic heart failure: rationale, design, and demographic characteristics of the T.O.S.CA. Registry. Intern Emerg Med 2018;13:661–671. [DOI] [PubMed] [Google Scholar]
- 3. Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JG, Boer RA, Drexel H, Ben Gal T, Hill L, Jaarsma T, Jankowska EA, Anker MS, Lainscak M, Lewis BS, McDonagh T, Metra M, Milicic D, Mullens W, Piepoli MF, Rosano G, Ruschitzka F, Volterrani M, Voors AA, Filippatos G, Coats AJ. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2019;21:1169–1186. [DOI] [PubMed] [Google Scholar]
- 4.European Society of Cardiology (ESC). Guidance for the Diagnosis and Management of CV Disease during the COVID‐19 Pandemic. 21 April 2020. https://www.escardio.org/Education/COVID‐19‐and‐Cardiology/ESC‐COVID‐19‐Guidance (27 May 2020).
- 5. Tomasoni D, Italia L, Adamo M, Inciardi RM, Lombardi CM, Solomon SD, Metra M. COVID‐19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail 2020;22:957–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in Northern Italy. N Engl J Med 2020;383:88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Piccolo R, Bruzzese D, Mauro C, Aloia A, Baldi C, Boccalatte M, Bottiglieri G, Briguori C, Caiazzo G, Calabrò P, Cappelli‐Bigazzi M, de Simone C, di Lorenzo E, Golino P, Monda V, Perrotta R, Quaranta G, Russolillo E, Scherillo M, Tesorio T, Tuccillo B, Valva G, Villari B, Tarantini G, Varricchio A, Esposito G. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID‐19 outbreak. Circulation 2020;141:2035–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fraiche AM, Eapen ZJ, McClellan MB. Moving beyond the walls of the clinic: opportunities and challenges to the future of telehealth in heart failure. JACC Heart Fail 2017;5:297–304. [DOI] [PubMed] [Google Scholar]
- 9. Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay RE, Rasmusson K, Rogers JG, Starling RC. Virtual visits for care of patients with heart failure in the era of COVID‐19: a statement from the Heart Failure Society of America. J Card Fail 2020;26:448–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cleland JG, Clark RA, Pellicori P, Inglis SC. Caring for people with heart failure and many other medical problems through and beyond the COVID‐19 pandemic; the advantages of universal‐access to home telemonitoring. Eur J Heart Fail 2020;22:995–998. [DOI] [PMC free article] [PubMed] [Google Scholar]


