Abstract
As the world accommodates to the coronavirus disease 2019 (COVID‐19) pandemic, routine in‐person medical services are resuming. The resumption of non urgent electrodiagnostic (EDX) testing faces unique challenges due to the long duration of the procedure and direct close contact with patients, including studies with risk of exposure to oropharyngeal secretions. We provide consensus guidance for resumption of EDX testing, addressing scheduling, patient arrival and registration, use of personal protective equipment, COVID‐19 screening and testing, the performance of EDX testing in outpatient and inpatient settings, cleaning and maintenance of the EDX equipment and laboratory, balancing trainee safety and training requirements, and patient care issues. These are broad recommendations that need to be adapted to local COVID‐19 risks, institutional guidelines and policies, and changing federal, state, and local regulations, and to changes in the pandemic over time.
Keywords: AANEM, COVID‐19, electrodiagnosis, electrodiagnostic testing, nerve conduction study, pandemic
Abbreviations
- AANEM
American Association of Neuromuscular & Electrodiagnostic Medicine
- CDC
Centers for Disease Control and Prevention
- COVID‐19
coronavirus disease 2019
- EDX
electrodiagnostic
- EMG
electromyography
- FDA
Food and Drug Administration
- HCP
healthcare personnel
- PCR
polymerase chain reaction
- PPE
personal protective equipment
- QPSC
Quality and Patient Safety Committee
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has necessitated several measures to contain or limit spread of the disease. Social distancing and the use of personal protective equipment (PPE) are two frequently used measures. In health care, balancing the risk of infection and the demand for healthcare resources to treat COVID‐19 affected patients has resulted in a significant reduction of nonurgent in‐person healthcare delivery. Alternative modes of healthcare delivery such as telephone visits or video platforms (“telemedicine”) are being increasingly used to provide health care. 1 , 2 However, nonurgent health care cannot be delayed indefinitely. Unique challenges with electrodiagnostic (EDX) testing in this context include the long duration of testing, close, direct patient contact (including studies with risk of exposure to oropharyngeal secretions), and potential for contamination of the EDX equipment.
The goals of this consensus guidance are to minimize disease transmission in patients and healthcare personnel (HCP), to identify and appropriately triage persons with possible COVID‐19 infections, and to balance efficient use of PPE with protecting HCP, while providing EDX services to patients. 3
2. METHODS
In response to member requests, the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) Quality and Patient Safety Committee (QPSC) developed this practice guidance for resumption of routine EDX services in the COVID‐19 pandemic. At an initial video‐call of the QPSC members and AANEM staff on May 8, 2020, we considered the document scope and identified a writing group. We reviewed available institutional guidance and Centers for Disease Control and Prevention (CDC) recommendations and drafted a document. We held video‐calls on May 14 and May 15, 2020, and finalized the document with input from QPSC members and AANEM staff. The draft was approved by the AANEM Board of Directors on May 17, 2020.
3. RESULTS
3.1. General operations
3.1.1. Patient scheduling
Patient scheduling modifications are as follows.
(1) Lengthening intervals between EDX appointments, staggering appointments, and reducing the number of appointments should be considered based on availability of space for social distancing, time required for appropriate cleaning of EDX equipment/laboratories between visits, and accommodation of a potentially reduced workforce. A reduction in initial volume of routine EDX studies with gradual escalation of the number of scheduled visits per day may be required.
(2) Extended hours (evenings and weekends) may be required to adjust for changes in scheduling.
(3) The EDX clinician should consider evaluating all EDX requests to prioritize the scheduling of patients. 4
(4) When scheduling EDX appointments, patients should be instructed to call if they develop symptoms of COVID‐19 before the appointment.
(5) Consider collecting co‐payments over the telephone or using contactless methods.
3.1.2. Patient arrival and registration
Modifications to patient arrival and registration processes should be aimed at avoiding overcrowding and facilitating social distancing.
(1) Points of entry to the testing facility should be monitored to limit entry and enforce social distancing.
(2) Patients can be asked to wait in their cars upon arrival and present for registration at their appointment time. Alternatively, the patient may check in by telephone from the parking lot and be escorted by staff to the EDX laboratory or called to report for check‐in just before their appointment time.
(3) If clinic waiting areas are used, the chairs should be rearranged at 6‐foot intervals. Social distancing markers 6 feet apart should be placed in the waiting room and around the registration area. There should be clear signage to instruct patients.
(4) Discrete entrances and exits should be designated and clearly marked, with the option of using escorts to guide patients in and out of the facility.
(5) Accompanying persons should be asked to wait outside the institution unless their presence is necessary to perform EDX testing (eg, in young children, patients with cognitive impairment).
3.2. Safety and PPE
(1) All patients should wear face masks.
(2) All patients should perform hand hygiene before EDX testing with alcohol‐based hand sanitizers (containing 80% ethanol or 75% isopropanol) or soap and water.
(3) All HCP in contact with patients should wear PPE.
(4) In persons not suspected of having COVID‐19 infection, the recommended PPE includes clean nonsterile gloves, surgical masks, and goggles or face shields. Disposable N95 filtering facepiece respirators (“N95 masks”) or an approved equivalent mask are alternative options.
(5) For high‐risk EDX studies (eg, facial studies, laryngeal electromyography [EMG]) isolation gowns and N95 masks or an approved equivalent are additionally recommended (Figure 1). 5
FIGURE 1.
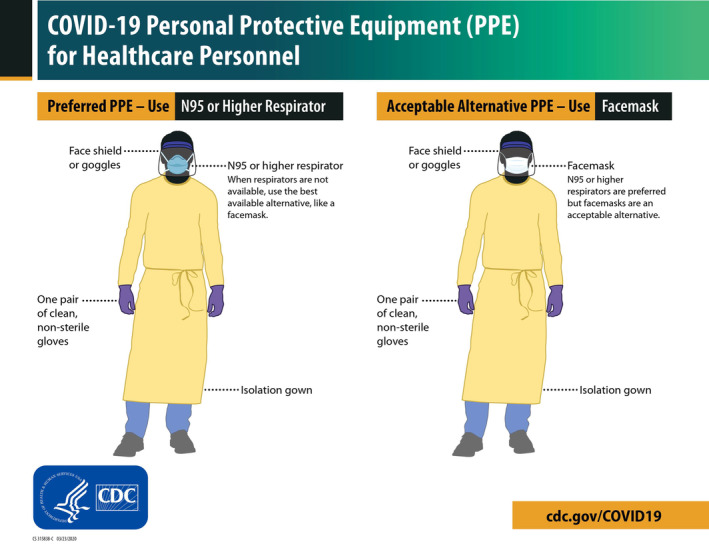
Personal protective equipment. COVID‐19 personal protective equipment (PPE) for healthcare personnel 5
(6) The same surgical mask may be worn throughout the workday but should be changed if it is visibly soiled.
(7) HCP must be educated about proper procedure and sequence for donning and doffing of PPE. Guidance regarding this is available from the CDC. 6
3.3. Patient and HCP screening
(1) All HCP with direct patient contact should be screened daily for COVID‐19. At present, most institutions in the United States use a symptom checklist to identify personnel who require COVID‐19 testing. Table 1 provides a suggested checklist.
TABLE 1.
Example of screening checklist for COVID‐19
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(2) All patients should be screened the day before their appointment using a symptom checklist. The check‐list responses should be documented in the medical records.
(3) Because of potential inaccuracies in the responses to the screening checklist, temperature screening at the entrance to the hospital or clinic may also be used.
(4) There is no CDC or other federal guidance at this time for preprocedure COVID‐19 testing. State and local mandates are broad, leaving testing decisions to the treating clinician. Institutional policies vary, with some institutions in the United States leaning toward presurgical and preprocedural testing for COVID‐19. Because of the risk of asymptomatic transmission, COVID‐19 testing using Food and Drug Administration (FDA) Emergency Use Authorized polymerase chain reaction (PCR) assays of nasopharyngeal or oropharyngeal swabs should be considered in all patients 24 to 48 h before EDX testing and strongly considered before high risk EDX studies. 7
(5) A protocol for urgent management of patients who report symptoms on screening or have a positive test for COVID‐19 should be readily available, and EDX testing should be postponed in these patients.
(6) Scheduling of EDX testing in patients who have tested positive for COVID‐19 or have a history of symptoms that are suggestive of COVID‐19 in the recent past requires evidence that the infective phase has passed. Replication‐competent virus is usually not present by 10 days after the onset of illness, even if PCR is positive. 8 General recommendations to discontinue isolation include all of the following: an afebrile period of at least 72 h without anti‐pyretic medications, improving respiratory symptoms, and at least 10 days since the first appearance of symptoms. 9 For immunocompromised and hospitalized patients, two consecutive FDA Emergency Use Authorized assays on upper respiratory swabs collected at least 24 h apart should be negative. 10
3.4. Outpatient EDX studies
(1) Limit the number of HCP in the EDX laboratory. Observers (eg, medical students or visiting trainees/faculty) should be avoided.
(2) Plan the study to obtain data efficiently and minimize study duration. Avoid studies that may not add meaningful diagnostic information.
(3) There is a risk of contamination of EMG supplies if handled during the procedure (eg, when replacing the ground electrode with a new one). This may be reduced by using a pre‐assembled single‐use kit for each study. The kit should contain alcohol wipes, electrode paste if required, disposable electrodes, a measuring tape, adhesive tape, a small pack of gauze, one EMG needle, and a marker pen.
(4) Because supplies may need to be replenished during the procedure, a “secondary kit” with an extra needle and electrodes may be useful, while keeping the bulk of supplies outside of the EDX room.
(5) Strongly consider using disposable electrodes.
(6) Use disposable markers or clean and disinfect the markers after each use.
(7) Use disposable tape measures or clean and disinfect measuring tapes after each use.
(8) Use disposable heating packs or an alternative method of warming such as heat lamps.
(9) Cover the patient with a sheet/blanket to minimize direct contact.
3.5. Inpatient EDX studies
(1) For inpatient EDX studies on patients who are not suspected of having COVID‐19 infection, we recommend following the procedures in the Outpatient EDX Studies section.
(2) Inpatient EDX studies on COVID‐19 positive patients, patients on ventilators, and patients using noninvasive positive pressure ventilation (NIPPV):
(i) The critical need for the study and the potential utility of EDX results in changing management should be discussed with the ordering clinician. 4 In some instances, the information may be obtained by other testing modalities such as imaging, and in others, the study may be postponed until patient is not infectious. In patients on ventilators or using NIPPV, the study should be postponed until two consecutive FDA Emergency Use Authorized assays on upper respiratory swabs collected at least 24 h apart are negative.
(ii) If the EDX study is deemed necessary, the following additional steps are recommended:
(a) PPE should include isolation gowns; N95 masks or an approved equivalent mask, face shields, or goggles; and gloves. 5
(b) If possible, perform the study at the patient’s bedside to avoid patient transport.
(c) Only essential EDX personnel should be physically present during the study.
(d) Consider performing the study at the end of the day so that there is sufficient time to thoroughly clean and disinfect the EDX equipment without immediate need to re‐use it.
3.6. EDX equipment/laboratory cleaning/disinfection and maintenance 11 , 12
3.6.1. EDX equipment
(1) Clean and disinfect the EDX machine, reusable cables, and electrodes thoroughly after each procedure per manufacturer guidance. Solutions containing bleach may damage sensitive equipment. The equipment may be cleaned with a cloth moistened with water and detergent, followed by disinfection with 80% ethanol or 75% isopropanol wipes, allowing the alcohol to evaporate.
(2) Consider using protective plastic covers that can be wiped for the keyboard, computer mouse, and protective plastic barriers between the patient and machine.
(3) Minimize furniture and other nonessential objects in the laboratory.
(4) Remove furniture that is upholstered with fabric or other material that cannot be disinfected.
3.6.2. Cleaning of the EDX laboratory
(1) Custodial services may not be available to clean EDX laboratories between procedures, and EDX laboratory staff will have to perform room cleaning. Use soap and water to clean surfaces where feasible before disinfection.
(2) Wipe down all hard surfaces including, but not limited to doorknobs, kiosks, elevator buttons, handrails, light switches, chairs, stools, beds, computer keyboards, mouse, screens, telephones, sinks/faucets, counter spaces with disinfecting wipes following product label instructions for duration of surface contact, etc.
(3) Place “Cleaned and Sanitized Room” signs on the door after cleaning.
3.7. Training of fellows and residents
The training of fellows and residents is a balance between fulfilling training program requirements and trainee safety.
(1) EDX in‐person training should continue with modifications to minimize exposure risk to trainees.
(2) All recommended PPE must be available to trainees, who must be educated about their proper use.
(3) Review of trainee reports should maintain social distancing between the attending and trainees. Alternatively, virtual technologies can be used.
(4) Other formats of EDX training such as virtual EDX case discussions should be used to supplement hands‐on training.
3.8. Patient care
(1) Reassure patients that stringent cleaning and disinfecting procedures are followed to minimize their risk of COVID‐19.
(2) It may be useful to prominently display the cleaning and disinfecting protocols in the EDX laboratory.
(3) Consider a specific discussion of the benefits of EDX testing versus the potential risks of COVID‐19 infection when obtaining informed consent for EDX testing.
4. CONCLUSIONS
The above recommendations should be used in conjunction with changing CDC and other federal, state, and local regulations. The recommendations may require modifications in the context of local infection rates, institutional policies and guidelines, and the availability of workforce, equipment, and other resources. The landscape of the pandemic is changing rapidly, and these recommendations should be adapted to meet those changes.
CONTENT DISCLAIMER
This Clinical Guidance (“Guidance”) is provided for informational and educational purposes only. It is intended to offer physicians guidance regarding best practices in caring for and treating patients during the COVID‐19 pandemic. Adherence to any recommendations included in this Guidance will not ensure successful treatment and/or prevention of transmission in every situation. Furthermore, the recommendations contained in this Guidance should not be interpreted as setting a standard of care, or be deemed inclusive of all proper methods of care nor exclusive of other methods of care reasonably directed to obtaining the same results.
The ultimate judgment regarding the propriety of any specific therapy must be made by the physician and the patient in light of all the circumstances presented by the individual patient, and the known variability and biological behavior of the medical condition.
This Guidance and its conclusions and recommendations reflect the best available information at the time the Guidance was prepared. The results of future studies may require revisions to the recommendations in this Guidance to reflect new data.
AANEM does not warrant the accuracy or completeness of the Guidance and assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this Guidance or for any errors or omissions. This guidance is not intended to provide legal or medical advice and should not be relied upon as such.
CONFLICT OF INTEREST
Urvi Desai has received honoraria for speaker bureau or advisory board participation from Alexion, Akcea, Stealth Biotherapeutics, and CSL Behring. Charles Kassardjian has received honoraria or serve on an advisory board for Alexion, Akcea, Takeda, and Sanofi Genzyme. David Del Toro reports no disclosures. Nida Gleveckas‐Martens reports no disclosures. Jayashri Srinivasan reports no disclosures. Deborah Venesy reports no disclosures. Pushpa Narayanaswami has received grant support from the Patient Centered Outcomes Research Institute, Momenta Pharmaceuticals, and provided consultation for Alexion, Momenta and Argenx.
ETHICAL PUBLICATION STATEMENT
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
ACKNOWLEDGMENTS
We thank AANEM staff Carrie Winter and Millie Suk, Executive Director Shirlyn Adkins, and the Board of Directors for their input.
Desai U, Kassardjian CD, Del Toro D, et al. Guidance for resumption of routine electrodiagnostic testing during the COVID‐19 pandemic. Muscle & Nerve. 2020;62:176–181. 10.1002/mus.26990
REFERENCES
- 1.Telemdicine transforms response to COVID‐19 pandemic in disease epicenter. https://www.sciencedaily.com/releases/2020/04/200430150220.htm. Accessed May 14, 2020.
- 2. Klein BC, Busis NA. COVID‐19 is catalyzing the adoption of teleneurology. Neurology. 2020;94(21):903‐904. 10.1212/WNL.0000000000009494. [DOI] [PubMed] [Google Scholar]
- 3. CDC . Outpatient and ambulatory care settings: responding to community transmission of COVID‐19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html. Accessed May 14, 2020. [Google Scholar]
- 4. Kassardjian CD, Desai U, Narayanaswami P. The AANEM Quality And Patient Safety Committee. Practical guidance for managing EMG requests and testing during the COVID‐19 pandemic. Muscle Nerve. 2020. 10.1002/Mus.26891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. CDC . COVID‐19 personal protective equipment (PPE) for healthcare personnel. https://www.cdc.gov/coronavirus/2019-ncov/downloads/COVID-19_PPE_illustrations-p.pdf. Accessed May 14, 2020.
- 6. CDC . Sequence for putting on and removing personal protective equipment. https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf. Accessed May 14, 2020.
- 7. Al‐Muharraqi MA. Testing recommendation for COVID‐19 (SARS‐Cov‐2) in patients planned for surgery ‐ continuing the service and 'suppressing’ the pandemic. Br J Oral Maxillofac Surg. 2020;58(5):503‐505. 10.1016/J.Bjoms.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CDC . Symptom‐based strategy to discontinue isolation for persons with COVID‐19. https://www.cdc.gov/coronavirus/2019-ncov/community/strategy-discontinue-isolation.html. Accessed May 15, 2020.
- 9.CDC. Discontinuation of isolation for persons with COVID −19 not in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html. Accessed May 15, 2020.
- 10.CDC. Ending home isolation for immunocompromised persons with COVID‐19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ending-isolation.html. Accessed May 15, 2020.
- 11. CDC . Reopening guidance for cleaning and disinfecting public spaces, workplaces, businesses, schools, and homes. https://www.cdc.gov/coronavirus/2019-ncov/community/reopen-guidance.html. Accessed May 15, 2020.
- 12.OSHA. COVID‐19 control and prevention. https://www.osha.gov/SLTC/covid-19/controlprevention.html. Accessed May 15, 2020.


