Abstract
Purpose
To report changes in outcomes for these 3 treatment options for meniscal root tears.
Methods
We systematically searched databases including PubMed, SCOPUS, and ScienceDirect for relevant articles. Criteria from the National Heart, Lung, and Blood Institute was used for a quality assessment of the included studies. A meta-analysis was performed to analyze changes in outcomes for meniscal repair.
Results
Nineteen studies, 12 level III and 7 level IV, were included in this systematic review, with a total of 1086 patients. Conversion to total knee arthroplasty (TKA) following partial meniscectomy ranged from 11% to 54%, 31% to 35% for nonoperative, conservative treatment, and 0% to 1% for meniscal repair. Studies comparing repair with either meniscectomy or conservative treatment found greater improvement and slower progression of Kellgren–Lawrence grade with meniscal repair. A meta-analysis of the studies included in the systematic review using forest plots showed repair to have the greatest mean difference for functional outcomes (International Knee Documentation Committee and Lysholm Activity Scale) and the lowest change in follow-up joint space.
Conclusions
In patients who experience meniscal root tears, meniscal repair may provide the greatest improvement in function and lowest risk of conversion to TKA when compared with partial meniscectomy or conservative methods. Partial meniscectomy appears to provide no benefit over conservative treatment, placing patients at a high risk of requiring TKA in the near future. However, future high-quality studies—both comparative studies and randomized trials—are needed to draw further conclusions and better impact treatment decision-making.
Level of Evidence
Level IV, systematic review of level III and level IV evidence
Tears or avulsions of the meniscal root, whether occurring acutely or as a result of chronic degeneration of the meniscus, have been shown to occur less frequently than tears of the meniscal body or meniscal horns and are often more difficult to diagnose. Nevertheless, early diagnosis and treatment of meniscal root tears (MRTs) are crucial in minimizing meniscal extrusion, which can disrupt normal biomechanics in the knee, result in increased instability and tibiofemoral contact pressure, and increase cartilage degeneration.1,2
Although many developments in orthopaedic surgery have broadened treatment options, data regarding the clinical indications for one treatment over another are limited. A recent classification system for MRTs was developed by LaPrade et al.,3 which is based on the morphology and location of the tear. By this system, tears are grouped into 1 of 5 types, with type 2, complete radial tears, having 3 subtypes based on the distance between the tear and root attachment. While such a classification system is certainly a useful aid when describing meniscal tears, the utility of such a system, especially in determining the prognosis of a root tear and in guiding treatment, is not yet known.4
It has been recommended that the decision regarding treatment modality should be based on the degree of pre-existing osteoarthritis and the chronicity of the tear.5 However, the paucity of literature guiding surgeons toward one treatment over another has proved it difficult to create a set algorithm for the treatment of MRTs. Moreover, several comparative studies have drawn contradictory conclusions about the superiority or noninferiority of the aforementioned nonoperative, operative, and repair treatment options with regards to frequently used outcome scores.4,6, 7, 8 While 2 relatively recent systematic reviews focused on reporting outcomes of meniscal repair, the goal and novelty of this study is to systematically compare a broader range of treatment options for MRTs, including repair, partial meniscectomy, and conservative treatment.9 The primary focus of this study was to report changes in functional outcome scores between these 3 treatment options for MRTs. We hypothesized that meniscal repair would result in the greatest improvement in these outcomes measures.
Methods
Search Strategy
A systematic literature review was performed under the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement to identify and select studies in this review. A systematic search was conducted in PubMed, SCOPUS, and ScienceDirect databases on December 10, 2018 for all English-language literature using the following terms and Boolean operators in the title and abstract: [Meniscus] AND [“root tear”] OR [avulsion]; [meniscus] AND [“root tear” meniscectomy]; [meniscus] AND [“root tear” transtibial suture repair]; [meniscus] AND [“root tear”] AND [“suture anchor repair”]; [meniscus] AND [“root tear”] AND [non-operative] OR [Non-surgical].
Studies were systematically reviewed if they met the following inclusion criteria: (1) English-language studies and (2) level I through IV clinical studies of operative and nonoperative treatment options for MRT and avulsion. The exclusion criteria included (1) level V studies, including technique articles, biomechanical studies, and narrative review articles; (2) studies lacking data on clinical outcomes, failure, or reoperation rate; (3) non-English language; and (4) publication before 2010.
Data Extraction
Two reviewers independently screened all titles and abstracts to determine suitability for a full-text review. Search criteria and filtering was completed in line with a checklist of inclusion and exclusion criteria. Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org) was used for study review and data extraction. Data extracted from the studies included year of publication, study design, study population demographics, interventions, and all clinical and radiographic data.
Quality Assessment
Two reviewers independently assessed the quality of each included study according to the 14 criteria outlined for observational studies and 9 criteria for case series studies by the National Heart, Lung, and Blood Institute for study quality assessment.10 If ratings differed between reviewers, then the article was discussed to reach consensus. The questions asked in the quality assessment cover a variety of biases, including selection bias, detection bias, attrition bias, and reporting bias, as well as other questions to judge the quality and methodology of the included studies. The scores have been totaled for both the comparative studies and case series in Table 14,6,7,11, 12, 13, 14, 15, 16, 17, 18, 19 and Table 2,20, 21, 22, 23, 24, 25, 26 respectively, and can be used both qualitatively and quantitatively as a measure of bias within this systematic review.
Table 1.
Quality Assessment of Comparative Studies
| Question No. | Ahn et al., 201511 | LaPrade et al., 201712 | Krych et al., 20177 | Ma 201513 | Lee et al., 201414 | Kim et al., 201115 | Keyhani et al., 201816 | Chung et al., 201717 | Chung et al., 20156 | Kim et al., 20114 | Furumatsu et al., 201918 | Lee et al., 201919 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 3 | NA | NA | NA | NA | NA | Y | NA | Y | NA | NA | NA | NA |
| 4 | Y | Y | Y | Y | N | Y | N | Y | Y | Y | N | Y |
| 5 | N | N | Y | N | N | Y | N | Y | Y | Y | Y | Y |
| 6 | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 7 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 8 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 9 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 10 | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 11 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 12 | N | N | N | N | N | N | N | N | N | N | N | N |
| 13 | Y | Y | Y | Y | Y | Y | N | Y | N | Y | Y | Y |
| 14 | Y | N | N | N | Y | N | N | N | N | N | N | N |
| Total | 11 | 10 | 9 | 10 | 10 | 12 | 8 | 12 | 10 | 11 | 10 | 11 |
1. Was the research question or objective in this paper clearly stated? 2. Was the study population clearly specified and defined? 3. Was the participation rate of eligible persons at least 50%? 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? 5. Was a sample size justification, power description, or variance and effect estimates provided? 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? 7. Was the time frame sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as a continuous variable)? 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 10. Was the exposure(s) assessed more than once over time? 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 12. Were the outcome assessors blinded to the exposure status of participants? 13. Was loss to follow-up after baseline 20% or less? 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
N, no; NA, not available; Y, yes.
Table 2.
Quality Assessment of Case Series
| Question No. | Han et al., 201020 | Ahn et al., 201021 | Lee et al., 201822 | Krych et al., 201723 | Chung et al., 201824 | Tjoumakaris et al., 201525 | Alaia et al., 201726 |
|---|---|---|---|---|---|---|---|
| 1 | Y | Y | Y | Y | Y | Y | Y |
| 2 | Y | Y | Y | Y | Y | N | N |
| 3 | Y | Y | Y | Y | Y | CD | CD |
| 4 | Y | N | Y | N | Y | CD | CD |
| 5 | Y | Y | Y | Y | Y | Y | Y |
| 6 | Y | Y | Y | Y | Y | Y | Y |
| 7 | Y | N | Y | Y | Y | Y | Y |
| 8 | Y | Y | Y | Y | Y | N | N |
| 9 | Y | Y | Y | Y | Y | Y | Y |
| Total | 9 | 7 | 9 | 8 | 9 | 5 | 5 |
1. Was the research question or objective in this paper clearly stated? 2. Was the study population clearly and fully described, including a case definition? 3. Were the cases consecutive? 4. Were the subjects comparable? 5. Was the intervention clearly described? 6. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants? 7. Was the length of follow-up adequate? 8. Were the statistical methods well-described? 9. Were the results well-described?
CD, cannot determine; N, no; Y, yes.
Outcome Measures
The primary outcomes of our study were clinical and radiologic improvement or progression of MRTs between the various treatments of MRTs. Assessment of clinical improvement or worsening associated with operative or nonoperative treatment of MRTs used International Knee Documentation Committee (IKDC) score and Lysholm Activity Scale. Radiologic improvement or worsening of MRTs was quantified by changes in medial meniscus extrusion and changes in the width of medial joint space using magnetic resonance imaging and Kellgren–Lawrence (K-L) grade on plain radiographs. Progression of the tear site gap and need for subsequent arthroplasty also were included for an assessment of treatment success. A meta-analysis using forest plots was performed for functional outcomes of MRT repair: IKDC, Lysholm Activity Scale, meniscal extrusion, and joint space. Statistical analysis was performed using R (R Foundation for Statistical Computing, Vienna, Austria). Results were reported as standardized mean difference and 95% confidence interval. Statistical significance was set at P < .05
Results
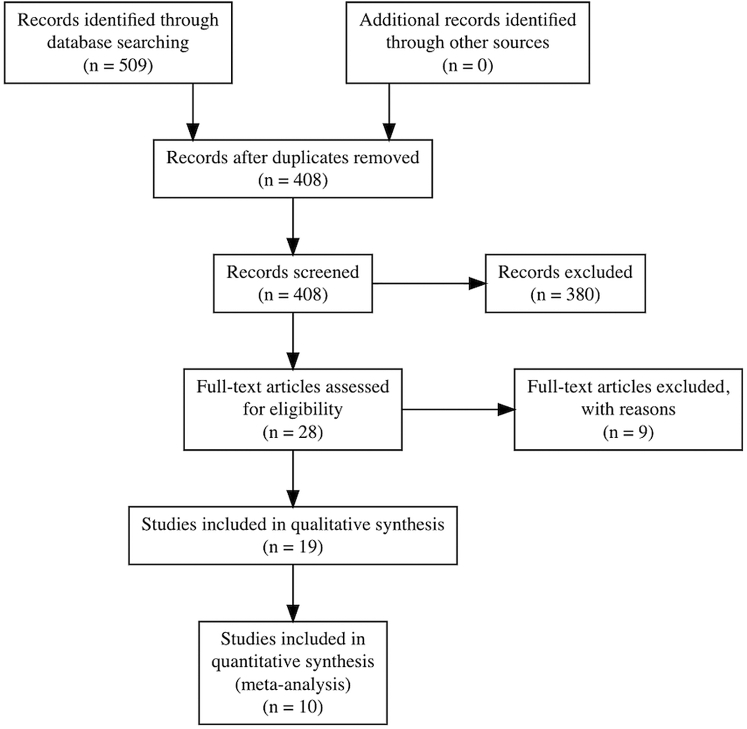
Our literature search identified 406 unique studies for review. Nineteen studies were selected for full-text review, all of which satisfied our inclusion and exclusion criteria (Fig 1); 5 studies included conservative groups, 5 studies included partial meniscectomy groups, and 15 studies included meniscal repair groups. Of the 19 included studies, 12 had a level III evidence (1 prospective case-control, 2 prospective comparative, 9 retrospective) (Table 3),4,6,7,11, 12, 13, 14, 15, 16, 17, 18, 19,27 and 7 had a level IV evidence (one prospective therapeutic case series, 6 retrospective case series) (Table 4).20, 21, 22, 23, 24, 25, 26
Fig 1.
Systematic review algorithm using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Table 3.
Level III Studies
| Study | Intervention | Mean Follow-up | Laterality | Radiographic Outcomes | Clinical Outcomes | Comments |
|---|---|---|---|---|---|---|
| Ahn et al., 201511 | Pull-out repair (25) vs Conservative (13) | 18 mo | Medial | Severe varus alignment and Outerbridge 3 or 4 associated with poorer outcomes in patients undergoing meniscal repair | Significantly greater IKDC, Tegner, and Lysholm scores at final follow-up with meniscal repair | Increased MA angle, tibia vara angle cartilage grade correlated with poor IKDC, Tegner, and Lysholm scores |
| LaPrade et al., 201712 | Pull-out repair of lateral (14) vs medial (31) | 24 mo (minimum) | Both | Not reported | Significant improvement in Lysholm, WOMAC, SF-12, and Tegner with both groups No significant difference between groups |
Lateral tear had 8 times the odds of undergoing concomitant ACL reconstruction All failures (6.7%) occurred with medial meniscal tears and in patients <50 years old |
| Krych et al., 20177 | Meniscectomy (26) vs conservative (26) | 66 mo | Medial | No significant difference in progression of K-L grade between groups | No significant difference in follow-up Tegner or IKDC scores | Female sex, BMI >30, and meniscal extrusion greater than 3mm associated with worse outcomes |
| Ma et al., 201513 | Pull-out repair (31) vs conservative (31) | Lateral | Significantly worse ICRS score with conservative treatment | —Significant improvement in Lysholm and IKDC scores in both groups —No significant difference between groups |
All patients underwent concomitant ACL reconstruction | |
| Lee et al., 201414 | Mason-Allen stitch repair (25) vs simple stitch repair (25) | 25 mo | Medial | —Significantly greater progression of joint space narrowing, progression of K-L grade, and arthrosis grade with simple stitch but not Mason-Allen stitch | Significant improvement in IKDC, Lysholm, and Tegner scores in both groups No significant difference between groups |
—Significant improvement in effusion, range of motion, joint line tenderness, pain of flexion, locking, giving way, and McMurray test in both groups —No significant difference between groups |
| Kim et al., 201115 | Suture anchor repair (22) vs pull-out suture repair (23) | 25.9 mo | Medial | Suture anchor repair associated with greater progression to grade 3 K-L grade, cartilage degeneration, and incomplete healing | —Significant improvement in IKDC, Lysholm, and HSS scores in both groups —No significant difference between groups |
Incomplete healing associated with progression of cartilage degeneration |
| Keyhani et al., 201816 | Suture anchor repair (40) vs conservative (33) | 24 mo (minimum) | Lateral | No significant difference in Lachman test | —No significant difference in s-IKDC or Lysholm score —Significantly greater proportion returned to previous level of activity following repair |
All patients underwent concomitant ACL reconstruction |
| Chung et al., 201717 | Meniscus repair- increased extrusion (23) vs decreased extrusion (16) | Medial | —No significant progression of K-L grade in patients with decreased extrusion —Significantly greater progression of OA in patients with increased extrusion |
Significantly higher postop Lysholm and IKDC score in patients with decreased extrusion | No significant difference in meniscal healing between groups | |
| Chung et al., 20156 | Partial meniscectomy (20) vs pull-out repair (37) | 60 months (minimum) | Medial | Significantly greater progression of joint space narrowing and K-L grade with partial meniscectomy over repair | Significantly greater Lysholm, IKDC, and Tegner scores at final follow-up with meniscal repair than meniscectomy | Significantly greater conversion to TKA rate with partial meniscectomy (35% vs 0%) |
| Kim et al., 20114 | Partial meniscectomy (28) vs pull-out repair (30) | 46.1-48.5 mo | Medial | Significantly less joint space narrowing and progression of K-L grade in repair group | Significant improvement in IKDC and Lysholm for both groups, repair more than meniscectomy | 3/28 progressed to TKA in meniscectomy group while none progressed to TKA in repair group |
| Furumatsu et al., 201918 | Repair, FasT-Fix vs FasT-Fix Modified Mason Allen (F-MMA) | 12 mo | Medial | F-MMA had better second-look arthroscopic score (7.2 vs 6.0) | Significant improvement in Lysholm, IKDC, and VAS for both groups. F-MMA group had better postoperative (VAS) pain score, KOOS pain, and sports/rec scores | Second-look arthroscopic score defined by same authors in alternate study27 |
| Lee, 201919 | Progression to TKA post-meniscectomy vs no progression to TKA post-meniscectomy | 60 mo (minimum) | Medial | Varus alignment, presence of radiographic arthritis, and greater K-L grade at baseline (2-3) significantly more associated with progression to TKA post-meniscectomy | Older age and greater BMI associated with significantly greater progression to TKA | Patients with no TKA still had significant progression of radiographic arthritis 2 years and at last follow-up (mean 8.9 y) |
ACL, anterior cruciate ligament; BMI, body mass index; HSS, Hospital for Special Surgery; ICRS, International Cartilage Repair Society; IKDC, International Knee Documentation Committee; K-L, Kellgren–Lawrence; KOOS, Knee Injury and Osteoarthritis Outcome Score; MA, mechanical axis; OA, osteoarthritis; SF-12, Short Form-12; TKA, total knee arthroplasty; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Table 4.
Level IV Studies
| Study | Intervention | Mean Follow-up | Laterality | Radiographic Outcomes | Clinical Outcomes | Comments |
|---|---|---|---|---|---|---|
| Han et al., 201020 | Partial meniscectomy (46) | 78 mo | Medial | 35% showed progression of K-L grade | Significant improvement in modified Lysholm score | 56% improvement in pain 67% patient satisfaction 19% underwent reoperation |
| Ahn et al., 201021 | Repair, all inside (27) | 18 mo | Lateral | Significant improvement in extrusion in sagittal plane only | Improvement in IKDC and Lysholm scores | —All patients underwent concomitant ACL reconstruction —8 of 9 patients showed complete healing on second-look arthroscopy |
| Lee et al., 201822 | Repair, pull-out (56) | 40.6 mo | Medial | –23% Progression of K-L grade —Narrowed medial joint space: 3.52 to 3.17 mm |
Improved Lysholm, IKDC, and HSS functional scores | Significant prognostic factors were age, BMI, K-L grade, medial joint space width, meniscal extrusion, type of tear, grade 3 or greater chondral lesion |
| Krych et al., 201723 | Conservative (52) | 62 mo | Medial | Significant progression of K-L grade | 13% with abnormal IKDC, 56% had severely abnormal score | Female sex associated with worse outcomes |
| Chung et al., 201824 | Repair, pull-out (91) | 84.8 mo | Medial | All failures were K-L grade I and Outerbridge grade 2 or 3 | Significant improvement in Lysholm score | All failures were female |
| Tjoumakaris et al., 2015∗,25 | Repair, pull-out (9) | Unknown | Medial | Mean meniscal extrusion: 1.5 mm | Mean Lysholm: 81.6 Mean WOMAC: 11.2 |
—Recurrence of tear in 4 patients |
| Alaia et al., 2017∗,26 | Repair, transtibial (18) | 24.9 mo | Medial | —Significantly worsened ICRS grades —Meniscal extrusion increased: 4.74 to 5.98 |
Significant improvement in IKDC (45.9-76.8) and Lysholm (50.9-87.1) | Only 1/18 achieved complete healing |
ACL, anterior cruciate ligament; BMI, body mass index; HSS, Hospital for Special Surgery; ICRS, International Cartilage Repair Society; IKDC, International Knee Documentation Committee; K-L, Kellgren–Lawrence; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Abstract presentation.
For the primary outcome of identifying differences in various quantitative variables between treatment options for MRT, 1142 tears were included: 968 were medial and 174 were lateral; 155 were in the conservative treatment group, 408 were in the meniscectomy group, and 579 were in the repair group. The study population had an average reported age range of 15 to 85 years and was more likely to be female (55%).
Results of quality assessment are summarized in Tables 1 and 2. Of the 14 questions assessing the quality of the 12 included comparative studies, the average score was 10.3 of 14 (73.8%) with a standard deviation of 1.15. Sources of bias in these studies included: outcome assessors not being blinded to the participants’ exposure status (question 12), lack of power description or sample size justification (question 5), and the potential for confounding variables (question 14). Of the 9 questions assessing the quality of the 7 included studies that were case series, the average quality assessment score was 7.43 of 9 (82.5%) with a standard deviation of 1.81. The largest sources of bias came from the subjects not being comparable (question 4) and the statistical methods within the studies not being well described (question 8). Overall, we believe the bias in this systematic review is due to the availability of low-level studies and the reliance on level III and level IV studies to draw conclusions.
Of the 12 level III studies included in this review, 3 compared meniscal repair with conservative treatment, 1 compared meniscectomy with conservative treatment, 2 compared repair with meniscectomy, and 4 compared distinct repair groups, such as medial versus lateral tears or repair techniques.4,6,7,11, 12, 13, 14, 15, 16, 17, 18, 19 One study compared patients with primary meniscectomy and conversion to total knee arthroplasty (TKA) with patients who did not need subsequent TKA.19 Meniscal repair resulted in significant improvement in functional outcomes scores in all studies. Functional improvement with repair was significantly greater in the 1 study comparing it with conservative treatment of medial MRTs, but no difference in improvement was noted in the 2 studies comparing repair with conservative treatment of lateral meniscal tears.11,13,16 The 1 study comparing partial meniscectomy with repair of medial root tears suggests that repair results in better outcomes with a slower progression of osteoarthritis.8 Meniscectomy appears to provide no benefit over conservative treatment in medial MRTs.
Of the 7 level IV studies included in this systematic review, 6 looked at medial MRT (1 meniscectomy, 1 conservative, and 4 repair) and 1 looked at lateral MRT (repair).20, 21, 22, 23, 24, 25, 26 Six of the studies showed improvement in clinical outcomes for MRT, whereas Krych et al.23 found 13% abnormal and 56% severely abnormal IKDC scores in patients who underwent conservative treatment of MRT, as well as an 87% failure rate. Thirty-one percent of patients underwent TKA at mean 30 months’ postdiagnosis. In patients undergoing treatment of a lateral MRT repair with concomitant anterior cruciate ligament reconstruction, Ahn et al.21 showed significant improvement in both radiographic and clinical outcomes with 8 of 9 patients, displaying complete healing on second-look arthroscopy. Lee et al.24 identified age, body mass index, K-L grade, medial joint space width, meniscal extrusion, and degree of cartilage damage as worse prognostic factors for medial MRT repair.24 Krych et al. and Chung et al. showed a greater degree of failure and worse functional outcomes in women for conservative treatment and repair, respectively.23,24 Alaia et al.26 and Tjoumakaris et al.25 showed that worsening in radiographic outcomes (such as meniscal extrusion and K-L grade) was not always correlated with functional outcome scores.
Nine studies reported incidence of K-L grade progression, 27.8% for conservative, 34.8%-100% for meniscectomy, and 8.7%-67.6% for repair. Six studies reported rates of conversion to TKA (Table 5). Three of these studies included patients treated by partial meniscectomy with failure rates ranging from 10.77% and 53.85% with mean time to failure ranging from 17.8 to 84.0 months.4,6,7,17,19,23 For the 2 groups who were treated conservatively, there were similar rates of conversion of 30.77% and 34.62% with similar mean time to failure of 30 months.10,25 However, in the 3 groups who underwent repair, rates of failure were considerably lower, with only 1 of the 158 total patients (0.6%) requiring conversion to TKA.4,6,17
Table 5.
Studies Reporting Conversion to TKA Grouped by Intervention
| Intervention | Authors | Study Type | Level of Evidence | No. of Tears | Mean Age, y | Mean Time to Failure, mo | Conversion to TKA (%) |
|---|---|---|---|---|---|---|---|
| Partial meniscectomy | Krych et al., 20177 | Retrospective comparative | III | 26 | 54.7 | 54.3 | 53.85% |
| Chung et al., 20156 | Retrospective comparative | III | 20 | 55.0 | NR | 35.00% | |
| Kim et al., 20114 | Retrospective comparative | III | 28 | 57.4 | 17.8 | 10.71% | |
| Lee et al., 201919 | Retrospective comparative | III | 60 | 60.8 | 84.0 | 20.83% | |
| Repair | Chung et al., 20156 | Retrospective comparative | III | 37 | 55.5 | – | 0.00% |
| Chung et al., 201717 | Retrospective case series | IV | 91 | 66 | 47 | 1.10% | |
| Kim et al., 20114 | Retrospective comparative | III | 30 | 55.2 | – | 0.00% | |
| Conservative | Krych et al., 201723 | Retrospective case series | IV | 52 | 58 | 30 | 30.77% |
| Krych et al., 20177 | Retrospective comparative | III | 26 | 55.8 | 30.2 | 34.62% |
NR, not reported; TKA, total knee arthroplasty.
Repair of the meniscal root significantly increased functional outcomes scores in 14 of 14 studies and the rate of conversion to TKA was considerably less than those observed following conservative treatment or partial meniscectomy. Studies comparing repair with either meniscectomy or conservative treatment found greater improvement and slower progression of K-L grade with meniscal root repair. A single study compared partial meniscectomy with conservative treatment and found no significant difference in outcomes.
Meta-Analysis of Meniscal Repair Groups
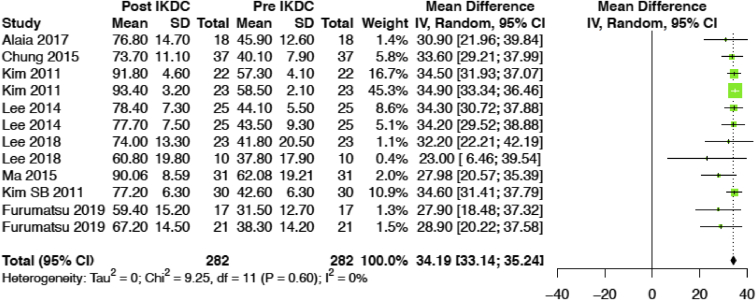
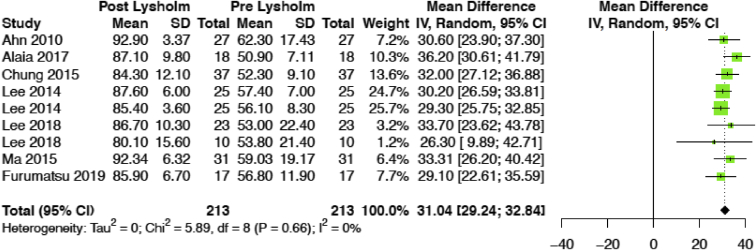
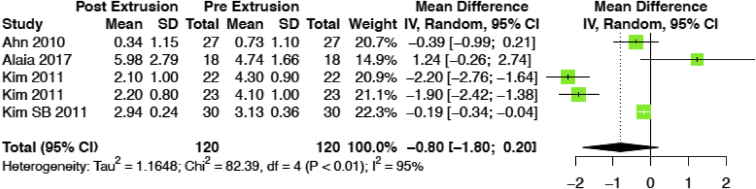
Meniscal repair resulted in a significant and consistent improvement in IKDC scores (mean difference [MD] = 34.19, 95% confidence interval [CI] 33.14-35.24, P ≤ .001; Fig 2). Similar findings were found for Lysholm scores (MD 31.04, 95% CI 29.24-32.84, P ≤ .001; Fig 3). Changes in meniscal extrusion were not as consistent however, with an MD of –0.80 mm (95% CI –1.80 to 0.20, P = .117; Fig 4).
Fig 2.
IKDC forest plot of meniscal repair studies. (CI, confidence interval; IKDC, International Knee Documentation Committee; IV, inverse variance; SD, standard deviation.)
Fig 3.
Lysholm Score forest plot of meniscal repair studies (CI, confidence interval; IV, inverse variance; SD, standard deviation.)
Fig 4.
Meniscal extrusion forest plot of meniscal repair studies. (CI, confidence interval; IV, inverse variance; SD, standard deviation.)
Discussion
The primary and secondary outcomes of this study were to review changes in functional outcomes and the rate of conversion to TKA for the various treatments of MRTs. Based on a systematic review of the literature on the treatment of medial and lateral MRTs, it is clear that although many prognostic factors may play a role, repair of an MRT has the best clinical and radiographic outcomes when compared with partial meniscectomy and conservative treatment. To our knowledge, this review is the first of its kind to pool and review outcomes and prognostic factors between the meniscal repair, meniscectomy, and nonoperative management in the hopes of determining which might be the most appropriate for a given patient.
Comparative analysis of clinical and radiologic outcomes for the treatment of medial and lateral MRTs revealed the best results with surgical repair over meniscectomy and conservative groups. For the medial meniscus, the available data showed improved functional outcome scores for patients undergoing surgical repair of medial MRT whereas the data for lateral MRT show similar results, although the limited data availability minimizes the generalizability of similar conclusions. A surface-level comparison of the treatment of medial MRT versus lateral MRT revealed the minimal use of surgical meniscectomy for the treatment of lateral MRT, and several studies have found that lateral meniscectomy has a greater risk of subsequent osteoarthritis when compared with medial meniscectomy.28,29 Despite the minimal number of studies directly comparing the treatment of lateral MRT by repair versus conservative options, the available data do not appear to show any significant difference in outcomes between the 2 approaches to lateral MRT management. One confounding variable may be that lateral MRTs almost exclusively occur in conjunction with anterior cruciate ligament tears. Therefore, this is likely a different demographic group that medial MRTs and their outcomes are not generalizable to the medial MRT group. In addition, the anatomy of the medial and lateral meniscal root complexes differ, and the degree to which they carry the compartment load of the knee differs.27 The medial attaches to the adjacent bone only, whereas the lateral attaches both to bone and via the posterior meniscofemoral ligaments, which are often preserved during injury and may confer some stability the avulsed lateral root.
This systematic review identified a number of prognostic factors associated with lower outcomes of the various procedures, as well as some insight into the specific prognostic factors favoring surgical repair over conservative treatment and meniscectomy. Overall, most studies concluded that the status of the articular cartilage, K-L grade, and meniscal extrusion were associated with worse clinical outcomes. For example, Chung et al.17 showed that increased meniscal extrusion on follow-up magnetic resonance imaging was associated with a greater progression of osteoarthritis and worse clinical outcomes for patients undergoing MRT repair than patients with decreased extrusion. It was also identified by Chung et al.24 that poor cartilage status at baseline (K-L grade I and Outerbridge grade 2 or 3) was associated with worse outcomes for repair of a medial MRT. For meniscectomy, poor cartilage status at baseline (K-L grade II or III), presence of radiographic arthritis, and varus alignment were show by Lee et al.19 to be poor prognostic factors and more likely to require subsequent TKA. When comparing meniscectomy and repair, Chung et al.6 showed the former to be more associated with joint space narrowing and K-L grade progression on follow-up imaging.
Other studies concluded that demographic and social factors, such as sex and body mass index, play a role in determining which treatment will have the best outcomes for a specific patient.7,19,23, 24, 25 Although many have associated older age with worsened outcomes of MRT repair, LaPrade et al.12 found no statistically significant difference in the clinical and radiologic improvements in patients older than 50 and younger than 50 years of age. Lastly, in analyzing patients with poor baseline cartilage status, Kim et al.15 discovered that the pullout suture repair technique had significantly worse progression of cartilage status —more follow-up K-L grade 3 or 5 and more incomplete healing—and a greater degree of cartilage degeneration (more patients with grade 3) at follow-up than suture anchor repair of the meniscus.
Limitations
There were several limitations to this study. First, this systematic review included only level III and level IV evidence studies. There was no high-quality evidence in the form of randomized controlled trials or controlled clinical trials, and this played a role in the level of bias within our systematic review as analyzed in our quality assessment (Tables 1 and 2). Second, varying techniques were used for meniscal root repair, which presents a potential source of confounding. Third, the measured outcomes and follow-up period were not consistent between studies, nor were statistical data universally reported by all studies, making direct comparison difficult and precluding us from using all studies in the meta-analysis of outcomes. Finally, the biggest limitation of the study was that the 3 treatment groups had significantly different numbers of patients, and both between the groups as well as within each group there were different indications for MRT treatment.
Conclusions
In patients who experience MRTs, meniscal repair may provide the greatest improvement in function and lowest risk of conversion to TKA when compared with partial meniscectomy or conservative methods. Partial meniscectomy appears to provide no benefit over conservative treatment, placing patients at a high risk of requiring TKA in the near future. However, future high-quality studies—both comparative studies and randomized trials—are needed to draw further conclusions and better impact treatment decision-making.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, Diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 2.Strauss E.J., Day M.S., Ryan M., Jazrawi L. Evaluation, treatment, and outcomes of meniscal root tears: A critical analysis review. JBJS Rev. 2016;4:1. doi: 10.2106/JBJS.RVW.15.00082. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 4.Kim S.B., Ha J.K., Lee S.W., et al. Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 6.Chung K.S., Ha J.K., Yeom C.H., et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy. 2015;31:1941–1950. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 7.Krych A.J., Johnson N.R., Mohan R., Dahm D.L., Levy B.A., Stuart M.J. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018;26:1117–1122. doi: 10.1007/s00167-017-4454-5. [DOI] [PubMed] [Google Scholar]
- 8.Ozkoc G., Circi E., Gonc U., Irgit K., Pourbagher A., Tandogan R.N. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 9.Feucht M.J., Kühle J., Bode G., et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI) https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 11.Ahn J.H., Jeong H.J., Lee Y.S., et al. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 2015;135:1265–1276. doi: 10.1007/s00402-015-2269-8. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 13.Ma Z. Surgical treatment of combined posterior root tears of the lateral meniscus and ACL tears. Medical Science Monitor. 2015;21:1345–1349. doi: 10.12659/MSM.892661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee D.W., Kim M.K., Jang H.S., Ha J.K., Kim J.G. Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: Comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30:1439–1446. doi: 10.1016/j.arthro.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 15.Kim J.-H., Chung J.-H., Lee D.-H., Lee Y.-S., Kim J.-R., Ryu K.-J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 16.Keyhani S., Mardani-Kivi M., Sharafat Vaziri A. Root avulsion and para-root tear of the posterolateral meniscus: Repair versus untreated. Curr Orthop Practice. January 2018:1. [Google Scholar]
- 17.Chung K.S., Ha J.K., Ra H.J., Nam G.W., Kim J.G. Pullout fixation of posterior medial meniscus root tears: Correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45:42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 18.Furumatsu T., Okazaki Y., Kodama Y., et al. Pullout repair using modified Mason-Allen suture induces better meniscal healing and superior clinical outcomes: A comparison between two surgical methods. Knee. 2019;26:653–659. doi: 10.1016/j.knee.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Lee B.-S., Bin S.-I., Kim J.-M., Park M.-H., Lee S.-M., Bae K.-H. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. Am J Sports Med. 2019;47:606–611. doi: 10.1177/0363546518819225. [DOI] [PubMed] [Google Scholar]
- 20.Han S.B., Shetty G.M., Lee D.H., et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: A 5- to 8-year follow-up study. Arthroscopy. 2010;26:1326–1332. doi: 10.1016/j.arthro.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 21.Ahn J.H., Lee Y.S., Yoo J.C., Chang M.J., Park S.J., Pae Y.R. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67–75. doi: 10.1016/j.arthro.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Lee S.-S., Ahn J.H., Kim J.H., Kyung B.S., Wang J.H. Evaluation of healing after medial meniscal root repair using second-look arthroscopy, clinical, and radiological criteria. Am J Sports Med. 2018;46:2661–2668. doi: 10.1177/0363546518788064. [DOI] [PubMed] [Google Scholar]
- 23.Krych A.J., Reardon P.J., Johnson N.R., et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25:383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 24.Chung K.S., Noh J.M., Ha J.K., et al. Survivorship analysis and clinical outcomes of transtibial pullout repair for medial meniscus posterior root tears: A 5- to 10-year follow-up study. Arthroscopy. 2018;34:530–535. doi: 10.1016/j.arthro.2017.08.266. [DOI] [PubMed] [Google Scholar]
- 25.Tjoumakaris F.P., Lombardi N.J., Tucker B.S., Levi D., Austin A., Pepe M.D. Medial meniscus root repair: Are we healing and how do we tell? Orthop J Sports Med. 2015;3 2325967115S0001(3 suppl) [Google Scholar]
- 26.Alaia M., Strauss E., Jazrawi L., Campbell K., Kaplan D. Discrepancy between radiographic and clinical outcomes at two year follow-up following transtibial medial meniscal root repair. Arthroscopy. 2017;33:e34. [Google Scholar]
- 27.Seedhom B.B., Dowson D., Wright V. Proceedings: Functions of the menisci. A preliminary study. Ann Rheumatic Dis. 1974;33 doi: 10.1136/ard.33.1.111. 111-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chatain F., Adeleine P., Chambat P., Neyret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842–849. doi: 10.1016/s0749-8063(03)00735-7. [DOI] [PubMed] [Google Scholar]
- 29.Bonneux I., Vandekerckhove B. Arthroscopic partial lateral meniscectomy long-term results in athletes. Acta Orthop Belg. 2002;68:356–361. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.