Abstract
Background
Olfactory dysfunction (OD) has been reported in coronavirus disease 2019 (COVID-19). However, there are knowledge gaps about the severity, prevalence, etiology, and duration of OD in COVID-19 patients.
Methods
Olfactory function was assessed in all participants using questionnaires and the butanol threshold test (BTT). Patients with COVID-19 and abnormal olfaction were further evaluated using the smell identification test (SIT), sinus imaging, and nasoendoscopy. Selected patients received nasal biopsies. Systematic review was performed according to PRISMA guidelines. PubMed items from January 1, 2020 to April 23, 2020 were searched. Studies that reported clinical data on olfactory disturbances in COVID-19 patients were analyzed.
Results
We included 18 COVID-19 patients and 18 controls. Among COVID-19 patients, 12 of 18 (67%) reported olfactory symptoms and OD was confirmed in 6 patients by BTT and SIT. Olfactory dysfunction was the only symptom in 2 patients. Mean BTT score of patients was worse than controls (P = .004, difference in means = 1.8; 95% confidence interval, 0.6–2.9). Sinusitis and olfactory cleft obstruction were absent in most patients. Immunohistochemical analysis of nasal biopsy revealed the presence of infiltrative CD68+ macrophages harboring severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antigen in the stroma. Olfactory dysfunction persisted in 2 patients despite clinical recovery. Systematic review showed that the prevalence of olfactory disturbances in COVID-19 ranged from 5% to 98%. Most studies did not assess olfaction quantitatively.
Conclusions
Olfactory dysfunction is common in COVID-19 and may be the only symptom. Coronavirus disease 2019-related OD can be severe and prolonged. Mucosal infiltration by CD68+ macrophages expressing SARS-CoV-2 viral antigen may contribute to COVID-19-related OD.
Keywords: anosmia, COVID-19, olfactory dysfunction, SARS-CoV-2, smell impairment
COVID-19-related olfactory dysfunction is common (67%, 12/18 patients). Recovery can be slow (>3 weeks). Sinusitis and olfactory cleft obstruction were absent in most patients. Immunohistochemical analysis of nasal biopsy specimens demonstrated infiltrative CD68+ macrophages expressing SARS-CoV-2 antigen in the stroma.
Coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization on March 11, 2020. Coronavirus disease 2019 is caused by a novel betacoronavirus: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 is highly adapted to humans and is capable of efficient person-to-person transmission [1]. As of May 31, 2020, COVID-19 has infected over 5.9 million people worldwide, with over 360 000 associated deaths [2]. Due to inadequacies in testing programs and large proportions of mild infections, the exact community burden of COVID-19 is unknown and will require population-wide seroepidemiological studies for definitive elucidation.
The common symptoms of COVID-19 include fever, cough, dyspnea, malaise, myalgia, and gastrointestinal disturbances [3]. In addition, olfactory dysfunction (OD) or anosmia has been reported in COVID-19 patients [4–6]. The majority of studies investigating OD in COVID-19 have used retrospective questionnaires or self-reported symptoms by patients [7–9]. These methods of assessment are prone to reporting bias and might fail to identify subtle OD. Therefore, objective measurements of olfactory function in COVID-19 patients are required. Furthermore, olfactory function in COVID-19 patients has not been compared to healthy controls, which is necessary to prove that olfaction in COVID-19 patients is compromised. A systematic assessment of the severity, prevalence, etiology, and duration of OD in COVID-19 patients is also lacking.
In this study, we quantitated olfactory function in COVID-19 patients and compared them to healthy controls. We also evaluated the severity, prevalence, etiology, and duration of OD in COVID-19 patients. In addition, a systematic review of the existing literature on olfactory disturbances in COVID-19 patients was performed.
METHODS
Study Setting
The study was conducted in Queen Mary Hospital and Pamela Youde Nethersole Eastern Hospital in Hong Kong. Both institutions are designated referral centers providing acute care to COVID-19 patients. Ethics approval for this study was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 20-310).
Patients and Controls
Patients between 18 and 60 years of age with mild COVID-19 infection (defined as not requiring supplemental oxygen therapy) who were consecutively admitted to either institutions between April 6 and April 9, 2020 were eligible for inclusion. All patients received standard care during hospitalization. Their demographic characteristics, clinical features, and laboratory results were retrieved from the electronic patient records. Patients with COVID-19 were compared to a control group in a 1:1 ratio. The control group comprised of healthy volunteers who were students or healthcare workers who reported no recent symptoms of upper respiratory tract infection and were age-matched to the patient group ±5 years to control for the potential effect of age on olfaction. Patients with COVID-19 and controls were excluded if they had an underlying history of allergic rhinitis or nasal polyps, which might confound the results of olfactory assessment. All participants completed a detailed questionnaire relating to olfaction (see Supplementary Material) as previously described with modifications [10]. This was followed by functional olfactory assessment.
Quantitative Assessment of Olfactory Function
The butanol threshold test (BTT) was used as the screening method for quantitation of olfactory function in all participants. The BTT was performed as previously described with modifications [11]. In brief, 99.9% 1-butanol AnalaR NORMAPUR (VWR International Limited, Briare, France) was diluted in deionized water to produce a range of 10 serial dilutions (see Supplementary Table 1), from 0.00002% (step 10) to 4% (step 1). Identical bottles containing deionized water were used as controls. All solutions were colorless. During the assessment, the test subjects were blindfolded. Each nostril was tested independently, starting from the lowest concentration (0.00002% 1-butanol [step 10]). Each concentration was tested along with a control in a forced-choice paradigm, in which the participant was required to differentiate between the test solution and control. The concentration step at which the participant was able to correctly differentiate between the test solutions and controls over 4 consecutive trials was the BTT score. The averaged scores of both nostrils was the participant’s final BTT score. If the participant failed to identify the highest concentration (4% 1-butanol [step 1]), a BTT score of zero was given. Mean BTT scores of COVID-19 patient and control groups were compared.
For COVID-19 patients who reported impaired olfaction at the time of study entry and received a BTT score of less than 4, the Smell Identification Test ([SIT] Sensonics International, Haddon Heights, NJ) was performed as a confirmatory and discriminatory test of olfactory function [12]. The SIT consisted of 40 test odorants. The test score was the total of all correct answers. The SIT results were compared against an age-matched and gender-matched normative SIT score, which were further categorized according to severity.Patients were defined as having OD if they met the following criteria: (1) self-reported ongoing olfactory impairment, (2) a BTT score of less than 4, and (3) an abnormal SIT result.
Virologic Assessment and Diagnosis
Coronavirus disease 2019 was diagnosed by real-time reverse-transcriptase polymerase chain reaction (RT-PCR) of pooled nasopharyngeal and throat swab specimens targeting the E-gene (TIB Molbiol, Berlin, Germany) of SARS-CoV-2. Serial cycle threshold (Ct) values of SARS-CoV-2 RT-PCR were assessed from diagnosis to discharge. Other respiratory viral infections including influenza A, influenza B, respiratory syncytial virus, adenovirus, and rhinovirus/enterovirus were excluded by commercial multiplex and in-house PCR assays.
Computed Tomography Scans
Patients with COVID-19 fulfilling the definition of OD received plain computed tomography scans of the sinuses and thorax. All scans were reviewed by a radiologist. The degree of rhinosinusitis was evaluated using the Lund-Mackay (LM) score, which is a 3-point scoring system used to describe the degree of sinus opacification (no opacification = 0, partial opacification = 1, or total opacification = 2) [13]. A combined LM score of 0 (no sinus opacification) to 24 (total opacification of all sinuses) is possible.
Nasoendoscopy and Nasal Biopsy
Nasoendoscopy was performed for COVID-19 patients with OD. The examination was performed at a seated and upright position at bedside. Local anaesthetic, Co-phenylcaine Forte (Mayne Pharma, Greenville, NC) was applied to both nostrils by spray. The nasal anatomy was assessed using a 4-mm diameter 30° rigid nasal endoscope (Karl Storz SE & Co., Tuttlingen, Germany) with tele-system (TELE PACK; Karl Storz SE & Co., Tuttlingen, Germany). Nasal biopsy was obtained at the discretion of the operating surgeon. A cotton pledget soaked with Co-phenylcaine Forte was inserted under endoscopic guidance for vasoconstriction and regional anesthesia. Nasal biopsies were obtained at the high anterior septum, just superior to the level of the axilla of the middle turbinate, using a 2.7-mm diameter biopsy forceps (Type 8150.00; Richard Wolf GmbH, Knittlingen, Germany).
Histological Assessment and Immunofluorescence Staining
Nasal biopsy specimens were fixed in 10% formalin and embedded in paraffin blocks. Four-micrometer tissue sections were stained with standard hematoxylin and eosin (H&E). The presence of macrophages was confirmed by immunohistofluorescence staining with mouse antihuman CD68 (clone KP-1) (LifeSpan Biosciences, Seattle, WA) and fluorescein isothiocyanate-conjugated donkey antimouse immunoglobulin (Ig)G (Jackson ImmunoResearch, West Grove, PA). The SARS-CoV-2 nucleoprotein (NP) was detected by immunofluorescence staining using rabbit anti-SARS-CoV NP antibody or mouse anti-SARS-CoV-2 NP antibody as previously described [14, 15].
Statistical Analysis
Means of BTT scores between patient and control groups were compared using Student’s t test. The BTT follow-up results for COVID-19 patients with OD were compared using paired t test. Categorical variables were compared using the Fisher’s exact test. Correlation between BTT scores and Ct values were assessed using Spearman’s rank test. Statistical analysis was performed using XLSTAT (Addinsoft, New York, NY) and Prism 8 (GraphPad, San Diego, CA).
Systematic Review
Systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [16]. PubMed items from January 1, 2020 to April 23, 2020 were searched using the following keywords: COVID-19, SARS-CoV-2, 2019-nCoV, or novel coronavirus. Duplicates were removed. Records were screened by the title and abstract. Two authors, T.W.-H.C. and H.-L.L., carried out screening and determined the eligibility of studies independently. Disagreements were resolved by another author (S.S.). The inclusion criteria included the following: (1) study population - adult patients diagnosed with COVID-19; (2) study design - (randomized) controlled trials, case-control studies, prospective or retrospective cohort studies, case series, and case reports; and (3) publications written in English. The exclusion criteria included (1) records that did not report anosmia or hyposmia or smell disturbances as symptoms and (2) correspondences, editorials, review articles that did not contain new clinical data. For included articles, we collected basic information (authors, country, sample size, and primary outcomes), patient demographics (age and sex), the method(s) used to assess olfaction, the prevalence of abnormal olfaction reported in the article, relevant imaging and endoscopic findings, and proposed etiology of impaired olfaction.
RESULTS
Patient Characteristics
A total of 20 patients and 21 controls were assessed for study inclusion. Two COVID-19 patients and 3 controls were excluded due to known history of nasal polyps and allergic rhinitis, respectively. Overall, 18 patients and 18 controls were included in the study. Patients with COVID-19 and controls did not differ significantly in terms of age, sex, smoking status, drinking history, and medical comorbidities (Table 1). One (1 of 18, 6%) COVID-19 patient was diagnosed with adenovirus coinfection. Other common respiratory viruses were excluded. The blood sodium levels were normal in COVID-19 patients on admission.
Table 1.
Demographic and Clinical Characteristics of COVID-19 Patients and Controls
| Characteristics | COVID-19 Patients (n = 18) | Controls (n = 18) | P Value |
|---|---|---|---|
| Age (years)a | 28 ± 19 (18–59) | 31 ± 17.5 (18–59) | .98 |
| 18–21 | 5 (28%) | 5 (28%) | |
| 22–31 | 5 (28%) | 7 (39%) | |
| 32–41 | 4 (22%) | 2 (11%) | |
| 42–60 | 4 (22%) | 4 (22%) | |
| Gender | |||
| Female | 11 (61%) | 13 (72%) | .725 |
| Male | 7 (39%) | 5 (28%) | |
| Smoking Status | |||
| Smoker | 1 (6%) | 0 (0%) | 1 |
| Nonsmoker | 17 (94%) | 18 (100%) | |
| Drinking Status | |||
| Nondrinker | 11 (61%) | 14 (78%) | .471 |
| Regular drinker | 1 (6%)b | 0 (0%) | 1 |
| Social drinker | 6 (33%) | 4 (22%) | .711 |
| Past Surgical History | |||
| Head injuries | 2 (11%) | 0 (0%) | .486 |
| Neurosurgery | 0 (0%) | 0 (0%) | |
| Maxillofacial surgery | 1 (6%)c | 0 (0%) | 1 |
| Good past health | 16 (89%) | 14 (78%) | .658 |
| Medical Comorbidities | |||
| Hypertension | 2 (11%) | 2 (11%) | |
| Diabetes mellitus | 0 (0%) | 0 (0%) | |
| Hyperlipidemia | 0 (0%) | 0 (0%) | |
| Malignancy | 0 (0%) | 1 (6%)d | 1 |
| Others | 0 (0%) | 1 (6%)e | 1 |
| History of zoster reactivation | 0 (0%) | 1 (6%) | 1 |
Abbreviations: COVID-19, coronavirus disease 2019.
aAge are median (interquartile range), n (%).
bPatient works as a wine merchant.
cHistory of tonsillectomy.
dHistory of breast cancer.
eCase of chronic hepatitis B carrier.
Self-Reported Olfactory Symptoms
Olfactory symptoms were reported by 12 of 18 (67%) COVID-19 patients compared with 0 of 18 controls (P < .001). Of the 12 patients with olfactory symptoms, 6 reported recovered olfaction at the time of study inclusion, including the patient who was diagnosed with adenovirus coinfection. The remaining 6 patients had never experienced olfactory symptoms. Age, gender distribution, and initial presenting symptoms of COVID-19 patients with (n = 12) and without (n = 6) olfactory symptoms were not significantly different. Of the 12 patients reporting olfactory symptoms, the median time from symptom onset to olfactory symptoms was 0.5 days (interquartile range [IQR], 0–4.75 days), whereas the time from onset of olfactory symptoms to study recruitment was 14 days (IQR, 10.5–16.25 days). Only 2 of 12 (17%) patients with olfactory symptoms reported concomitant rhinorrhea or nasal congestion, whereas 9 of 12 (75%) reported dysgeusia. Two patients were asymptomatic apart from the the impaired sense of smell.
Butanol Threshold Test
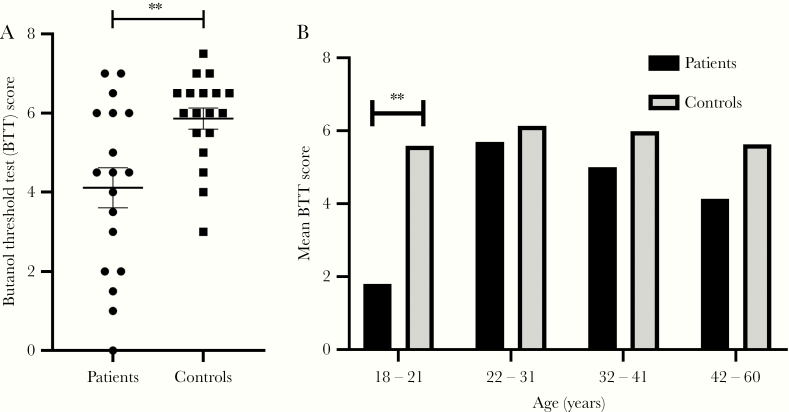
Quantitative olfactory function was screened for all 36 COVID-19 patients and controls by BTT. Mean BTT of COVID-19 patients was 4.1 (standard deviation [SD] = 2.2), whereas that of controls was 5.9 (SD = 1.1). The mean BTT scores were significantly higher for healthy controls compared with COVID-19 patients, indicating impaired olfactory function in the latter group (P = .004, difference in means = 1.8 with 95% confidence interval [CI]: 0.6–2.9) (Figure 1A). All 6 patients who reported ongoing olfactory disturbances at study entry had a BTT score <4. One COVID-19 patient had a BTT score of 0. Young COVID-19 patients (age <22) performed worse in the BTT; their mean score was lower when compared with COVID-19 patients from other age groups (P = .002) as well as controls (P < .001). However, there was a shorter mean duration between symptom onset and BTT in the younger age group of less than 22 years of age (P < .001, difference in means = 12.7 days with 95% CI: 7.5–17.9). Above age 22, the mean BTT score in the COVID-19 patient group also tended to be lower than in the control group but did not reach statistical significance (Figure 1B). Admission SARS-CoV-2 RT-PCR Ct values and BTT scores were not correlated (P = .882).
Figure 1.
Comparison of butanol threshold test (BTT) scores between coronavirus disease 2019 (COVID-19) patients and healthy controls. Bars represent mean and standard error of mean (A). Comparison of mean BTT scores of COVID-19 patients and healthy controls stratified by age group (B). ** indicates statistically significant difference between means of groups.
Smell Identification Test
From the BTT score and history taking, 6 COVID-19 patients met the criteria for SIT confirmatory assessment, which showed that 2 patients (33%) were anosmic, 2 patients (33%) suffered from severe microsmia, and 1 patient each had moderate and mild microsmia. Their demographic, clinical, and olfactory function profiles are described in Table 2.
Table 2.
Clinical, Olfactory Function, Nasoendoscopy, and Imaging Findings of COVID-19 Patients With Olfactory Dysfunction
| Patient 1 | Patient 2 | Patient 4 | Patient 5 | Patient 14 | Patient 15 | |
|---|---|---|---|---|---|---|
| Patient Characteristics | ||||||
| Sex | F | F | M | F | F | F |
| Age | 18 | 18 | 20 | 21 | 41 | 42 |
| Clinical Symptoms | ||||||
| Date of symptom onset | 1 Apr 20 | 28 Mar 20 | 3 Apr 20 | 26 Mar 20 | 16 Mar 20 | 15 Mar 20 |
| Fever | Y | N | Y | N | N | N |
| Chills | N | N | Y | N | N | N |
| Cough | Y | N | Y | N | N | Y |
| Sputum production | Y | N | N | N | N | Y |
| Shortness of breath | N | N | N | N | N | Y |
| Nasal complaints | N | Y (Rhinorrhea) | N | Y (Rhinorrhea) | N | N |
| Others | N | N | Y (Headache) | N | Y (Headache) | N |
| Olfactory Dysfunction | ||||||
| Onset date of olfactory dysfunction | 4 Apr 20 | 29 Mar 20 | 3 Apr 20 | 26 Mar 20 | 23 Mar 20 | 23 Mar 20 |
| Interval between olfactory dysfunction and symptom onset (day) | 3 | 1 | 0 | 0 | 7 | 8 |
| Butanol Threshold Test (BTT) Score | ||||||
| First BTT score | 1.5 | 0 | 1 | 3.5 | 2 | 2 |
| Date of first BTT | 9 Apr 20 | 7 Apr 20 | 7 Apr 20 | 7 Apr 20 | 6 Apr 20 | 6 Apr 20 |
| Second BTT score | 3 | 1.5 | 3 | 3.5 | 0 | 3 |
| Date of second BTT | 16 Apr 20 | 15 Apr 20 | 15 Apr 20 | 15 Apr 20 | 15 Apr 20 | 15 Apr 20 |
| Smell Identification Test | ||||||
| SIT (score, of 40) | 26 | 16 | 25 | 21 | 16 | 33 |
| SIT (category) | Moderate microsmia | Anosmia | Severe microsmia | Severe microsmia | Anosmia | Mild microsmia |
| Date of SIT | 10 Apr 20 | 7 Apr 20 | 7 Apr 20 | 7 Apr 20 | 6 Apr 20 | 6 Apr 20 |
| Nasoendoscopy | Normal | Normal | Normal | Normal | Normal | Normal |
| Computed tomography scan | ||||||
| Paranasal sinuses (Lund-Mackay score) | 2 | 1 | 2 | 0 | 0 | 0 |
| Olfactory cleft (opacification score)a | ||||||
| Right | 2 | 2 | 0 | 1 | 0 | 0 |
| Left | 2 | 2 | 0 | 1 | 0 | 0 |
| Thorax (COVID-19 related lung changes)b | N | N | Y | N | Y | N |
Abbreviations: BTT, butanol threshold test; COVID-19, coronavirus disease 2019; N, no; SIT, smell identification test; Y, yes.
aOlfactory cleft opacification score: complete opacification = 2; partial opacification = 1; Unopacified = 0.
bParenchymal ground-glass opacification of the lungs.
Radiographic Assessment by Computed Tomography Scans
Computed tomography sinus and thorax was performed for the 6 patients confirmed with OD. No radiological evidence of sinusitis was found, as represented by a LM score of ≤2. Specifically, bilateral olfactory cleft obstructions were documented in 2 (33%) patients only, whereas partial obstruction was found in 1 patient. The remaining 3 patients (50%) had patent olfactory passages (Figure 2). Computed tomography thorax revealed peripheral ground glass opacification (2 patients), linear parenchymal bands (1 patient), consolidative nodules (1 patient), or no abnormalities (2 patients).
Figure 2.

Computed tomography scans of the nasal cavities and sinuses of coronavirus disease 2019 patients with olfactory dysfunction showing olfactory cleft opacification: complete opacification (A), partial opacification (B), and no opacification (C). Sinusitis was absent.
Nasoendoscopy and Biopsy
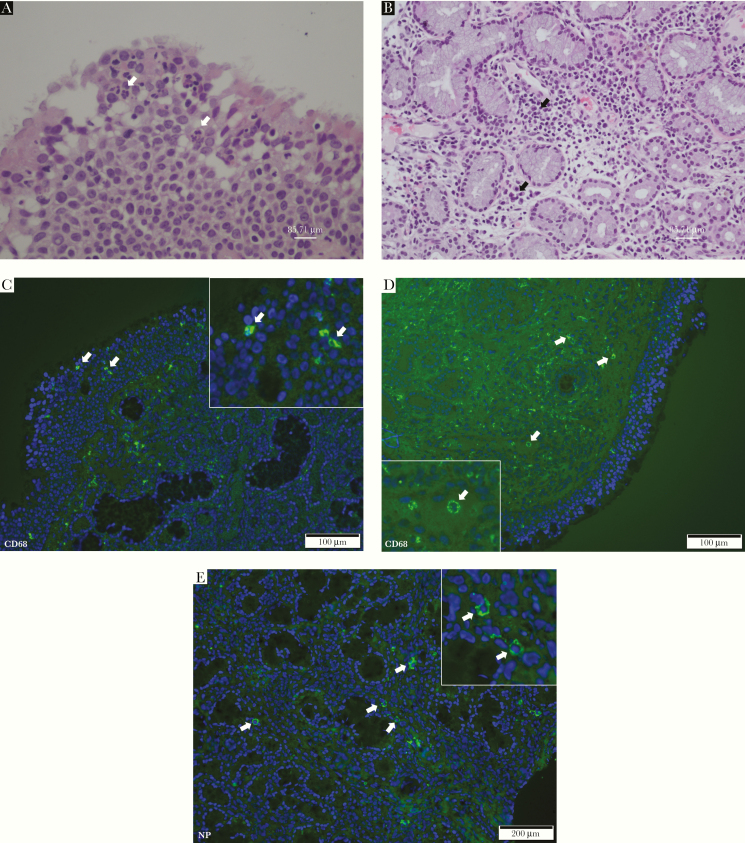
Patients with OD were assessed by nasoendoscopy. No endoscopic evidence of olfactory cleft obstruction, nasal polyps, or active sinusitis was found. Nasal biopsies were performed in 3 patients, 1 specimen of which was positive for SARS-CoV-2 by RT-PCR. The H&E staining of nasal biopsy samples showed minimal inflammatory changes, as represented by minor infiltrations of lymphocytes, plasma cells, and occasional neutrophils in the stroma. In one of the samples, intraepithelial neutrophils were also observed (Figure 3A and B). Immunofluorescence staining for CD68 established the presence of macrophages within the epithelium (Figure 3C) and the stroma (Figure 3D). Scattered cells positive for the SARS-CoV-2 NP protein were found in the stroma (Figure 3E). These cells were confirmed to be macrophages (Figure 3F to I).
Figure 3.
Representative histopathological and immunofluorescence staining results of nasal biopsy tissue sections. (A) Hematoxylin and eosin-stained section showed few intraepithelial neutrophils (white arrows). (B) Small numbers of lymphocytes, plasma cells, and occasional neutrophils amongst mucous glands in the stroma (black arrows). Immunofluorescence staining of CD68 showing presence of scattered macrophages in the (C) epithelium and (D) stroma (green), the area in the boxes was magnified to demonstrate cytoplasmic staining of CD68 (white arrows). (E) Immunofluorescence staining of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleoprotein (NP) in the nasal mucosa (green) and in magnified image (white arrows). Localization of SARS-CoV-2 NP in CD68+ macrophages by double immunofluorescence staining of CD68 (F, green) and SARS-CoV-2 NP (G, red, using mouse anti-SARS-CoV-2 NP and Texas-Red-conjugated Donkey antimouse secondary antibody), cell nuclei counterstained by 4’,6-diamidino-2-phenylindole (DAPI) in blue (H) and merged image (I).
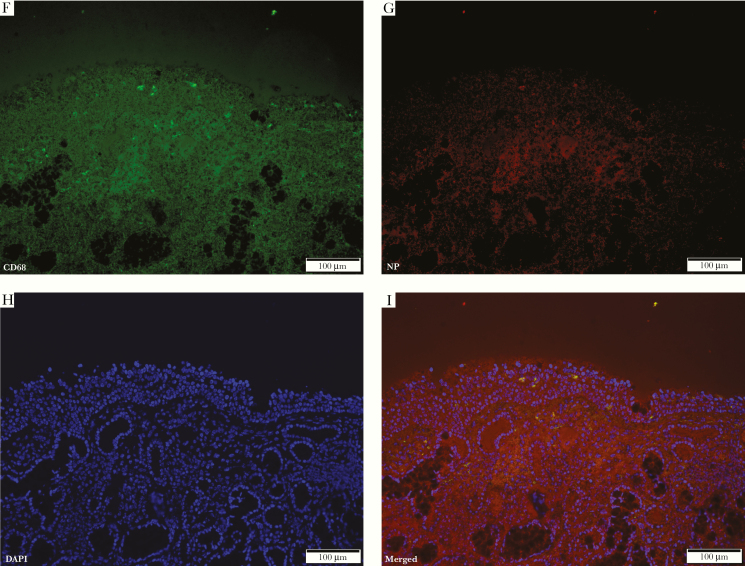
Follow-Up Evaluation by Butanol Threshold Test Assessment
For the 6 patients with OD, follow-up BTT assessments were arranged between 7 and 9 days after the initial examination when all other symptoms of COVID-19 had already subsided (Figure 4). Four patients had measurable and significant improvements in their BTT scores in the second assessment (P = .005). One patient had static olfactory function. Another patient’s BTT score deteriorated further at follow-up. Her nasopharyngeal swab SARS-CoV-2 RT-PCR was already negative at this stage. This shows that OD can persist even after virologic clearance in a subset of patients.
Figure 4.
Serial progression of butanol threshold test scores in patients with olfactory dysfunction.
Systematic Review
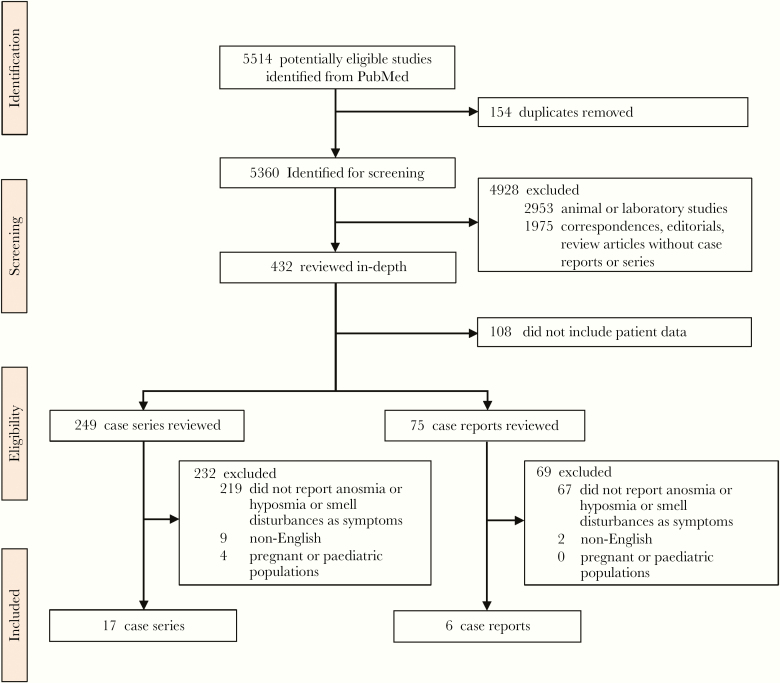
The PRISMA flow diagram is shown in Figure 5. A total of 5514 records from PubMed were screened. We identified 17 cohort studies and 6 case reports from the following: China (1 study), France (4 studies), Germany (1 study), Greece (1 study), Iran (3 studies), Italy (5 studies), Republic of Korea (1 study), Spain (3 studies), United Kingdom (1 study), United States (2 studies), and multinational (1 study) [4–9, 17–33]. The sample sizes of the cohort studies ranged from 4 to 4707 patients. Self-reporting through questionnaires or clinical consultations were the most commonly adopted method for the assessment of olfaction. Only 1 study performed SIT on patients [21]. The reported prevalence of olfactory symptoms ranged from 5% to 98%. There was no difference in prevalence of anosmia based on sex. Clinical recovery of olfaction was documented in 5 reports (4 case cohorts and 1 case report), which showed that majority of patients recovered within 14 days from onset of olfactory disturbances. Details of individual reports are listed in Tables 3 and 4.
Figure 5.
Study selection.
Table 3.
Cohort Studies on Olfactory Disturbances in COVID-19 Patients
| Author | Country | Sample Size | Primary Outcome(s) | Methods of Olfactory Assessment | Prevalence of Olfactory Impairment (%) | Female (%) | Proposed Etiology of Olfactory Impairments |
|---|---|---|---|---|---|---|---|
| Beltrán-Corbellini et al [31] | Spain | 79 | Smell and taste disorder | Questionnaire | 25/79 (31%) | 31/79 (39%) | Damage of the olfactory sensory epithelium |
| Bénézit et al [23] | France | 68 | Hyposmia and hypogeusia | Questionnaire | 31/68 (45%) | Not reported | Pathology at the olfactory mucosa |
| Burrer et al [9] | USA | 4707 | COVID-19 in healthcare workers | Consultation | 750/4707 (16%) | Not reported | Nil |
| Giacomelli et al [27] | Italy | 59 | Olfactory and taste disorders | Questionnaire | 14/59 (24%) | 19/59 (32%) | Transneural penetration through the olfactory bulb |
| Heidari et al [33] | Iran | 23 | Anosmia | Consultation | 23/23 (100%) | 15/23 (65%) | Nil |
| Klopfenstein et al [20] | France | 114 | Anosmia | Consultation | 54/114 (47%) | 36/54 (67%) | Nil |
| Lechien et al [7] | Europe (Belgium, France, Italy, Spain) | 417 | Olfactory and gustatory dysfunctions | Questionnaire | 357/417 (86%) | 263/417 (63%) | Viral invasion through ACE2 receptor to olfactory bulb or related regions of CNS |
| Lytras et al [28] | Greece | 40 | Prevalence of COVID-19 in repatriation flights to Greece | Consultation | 2/5 (40%) | Not reported | Nil |
| Mao et al [8] | China | 214 | Neurologic manifestation | Consultation | 11/214 (5%) | 127/214 (59%) | Retrograde neuronal invasion |
| Marzano et al [24] | Italy | 22 | COVID-19 associated skin manifestation | Consultation | 4/22 (18%) | 6/22 (27%) | Nil |
| Moein et al [21] | Iran | 60 | Olfactory dysfunction | UPSIT | 59/60 (98%) | 20/60 (33%) | Damage of the olfactory epithelium |
| Monti et al [26] | Italy | 4 | Clinical characteristics of immunosuppressed patients with chronic arthritis | Consultation | 3/4 (75%) | 4/4 (100%) | Nil |
| Spinato et al [32] | Italy | 202 | Alterations in smell or taste | Questionnaire | 130/202 (64%) | 105/202 (52%) | Nil |
| Toscano et al [29] | Italy | 5 | Guillain-Barré syndrome associated with SARS-CoV-2 | Consultation | 2/5 (40%) | 1/5 (20%) | Nil |
| Wolfel et al [30] | Germany | 9 | Virologic manifestations | Self-reported through consultation | 3/9 (33%) | Not reported | Not suggested |
| Yan et al [4] | USA | 59 | Chemosensory dysfunction | Questionnaire | 40/59 (68%) | 29/59 (49%) | Pathology at the olfactory epithelium |
| Zayet et al [25] | France | 62 | Anosmia and dysgeusia | Consultation | 32/62 (52%) | 38/62 (61%) | Nil |
Abbreviations: CNS, central nervous system; COVID-19, coronavirus disease 2019; SARS-COV-2, severe acute respiratory syndrome coronavirus 2; UPSIT, University of Pennsylvania Smell Identification Test.
Table 4.
Case Reports on Olfactory Disturbances in COVID-19 Patients
| Author | Country | Sex, Age (Years) | Methods of Olfactory Assessment | Radiological Findings | Proposed Etiology of Anosmia |
|---|---|---|---|---|---|
| Eliezer et al [17] | France | F, 40 | Odorant identification | CT and MRI | Olfactory cleft obstruction |
| Galougahi et al [5] | Iran | Not specified | Consultation | MRI of the olfactory bulb | Nil |
| Gane et al [6] | United Kingdom | M, 48 | Consultation | Nil | Conductive loss at the olfactory cleftDirect infection of the olfactory mucosa and destruction of the olfactory sensory neurons |
| Gutiérrez-Ortiz et al [18] | Spain | M, 50 | consultation | Nil | Infection of the olfactory nerve; anti-ganglioside antibodies GD1b IgG |
| Jang et al [19] | Korea | M, 42 | Consultation, visual analog scale | Nil | Nil |
| Ollarves-Carrero et al [22] | Spain | F, 40 | Consultation | Nil | Infection of the olfactory nerve |
Abbreviations: COVID-19, coronavirus disease 2019; CT, computed tomography; F, female; IgG, immunoglobulin G; M, male; MRI, magnetic resonance imaging.
DISCUSSION
In this study, we have demonstrated that OD is a characteristic symptom of COVID-19, which is reported by a significant proportion (67%) of patients. We have objectively proved that olfaction is compromised in COVID-19 patients when compared with healthy controls. Remarkably, we found that a subset of COVID-19 patients suffered from profound OD in the absence of typical respiratory and systemic symptoms. Although measurable improvements were documented on follow-up evaluation, OD persisted in a subset of patients even after virologic clearance and hospital discharge.
The etiology of OD in COVID-19 is enigmatic. One case report had proposed that inflammatory obstruction of the olfactory clefts may be a possible cause of anosmia in COVID-19; however, half of the patients with OD in our study had patent olfactory passages. This argues against simple conductive impairment [17]. Alternatively, previous studies have suggested that the inflammatory cytokine milieu in nasal cavity affects olfactory neuronal function in patients with chronic rhinosinusitis [34]. However, only 17% of patients with OD in our study had rhinorrhea or nasal congestion, and minimal inflammatory infiltrates were found in nasal biopsy specimens, suggesting that local inflammation may not be the only contributing factor for OD in COVID-19 infection. Our previous study on SARS-CoV-2 replication in ex vivo human lung tissue also demonstrated that inflammation induced by SARS-CoV-2 is mild and less severe compared with 2003 SARS coronavirus [15].
An alternate hypothesis is direct invasion of the olfactory neurons by SARS-CoV-2. Olfactory dysfunction has been replicated in mice infected with Sendai virus with detectable virus in both olfactory epithelium and bulbs [35]. Similarly, olfactory system infection has also been linked to mouse hepatitis virus and neuroinvasive H5N1 infection in animal models [36, 37]. In vitro, we have recently demonstrated that SARS-CoV-2 is capable of growth in the neural cell line U251 [38]. However, olfactory sensory neurons do not appear to express Angiotensin-converting enzyme 2 (ACE2) and Transmembrane Serine Protease 2 (TMPRSS2) genes [39]. On the other hand, ACE2 and TMPRSS2 genes are found in the supporting cells of the human neuroepithelium, including sustentacular cells, olfactory horizontal basal cells, microvillar cells, and Bowman’s glands, which represent viable targets for SARS-CoV-2 infection [39]. Although our histological analysis of nasal biopsy specimens showed that local inflammation may be minimal or absent, it was notable that SARS-CoV-2 retains the ability to cause infiltrative infection, as demonstrated by CD68+ macrophages carrying viral antigen in the stroma. These macrophages may be able to traffic SARS-CoV-2 to the olfactory neuroepithelium. Such cell-to-cell transfer is well described in human immunodeficiency virus infection where macrophages can secondarily infect lymphocytes. Therefore, transmission of SARS-CoV-2 by CD68+ macrophages to the supporting cells of the olfactory neuroepithelium may disrupt the biochemical and electrophysiological homeostasis of the olfactory receptor neurons, leading to chemosensory dysfunction and impaired neuronal turnover.
In our systematic review, we found that OD was seldom reported in COVID-19 patient cohorts from mainland China. Prevalence of OD in Chinese COVID-19 patients also appeared lower than in Western cohorts of comparable size [8]. Although this might be due to underreporting, we note that intranasal interferon-α is widely prescribed in China for COVID-19 infection in accordance with national treatment guidelines [40]. Intranasal interferon-α treatment is not widely adopted by the rest of the world including Hong Kong. We speculate that early intranasal interferon-α may abrogate local SARS-CoV-2 replication in the olfactory epithelium sufficiently to reduce OD. Prospective interventional trials for the treatment of OD in COVID-19 patients are needed to confirm this important observation.
Olfactory dysfunction and dysgeusia in COVID-19 should not be overlooked because of the associated psychosocial impact on affected patients. Our patients reported distress due to their inability to smell, which affected their appetite and desires for eating. A recent large-scale smartphone-based self-reporting health information study also showed that skipped meals were reported in over 40% of patients who were tested positive for SARS-CoV-2 [41]. Patients might become socially withdrawn because they cannot share culinary experiences with their loved ones. Studies have shown that OD is linked to lower quality of life and depression [42].
There were a few limitations in our study. First, the study sample size was limited by the number of confirmed COVID-19 patients in Hong Kong. However, quantitative olfactory assessments were performed for all participants, which allowed for objective comparison between patient cohorts and controls. Second, imaging and nasoendoscopy were not performed in all patients to limit exposure of patients without OD to invasive assessments. Third, nasal biopsy specimens were obtained from the middle turbinate, which may not contain olfactory neuroepithelium. However, biopsy of the olfactory neuroepithelium at the cribriform plate of the ethmoid bone is not possible in routine bedside endoscopic assessment. Fourth, the control group was not tested for SARS-CoV-2, due to limited number of test kits available, outside of clinical needs. However due to the low prevalence of COVID-19 in Hong Kong, it is unlikely that these healthy volunteers were infected by SARS-CoV-2.
CONCLUSIONS
In conclusion, this study proves that OD is common in COVID-19 patients using objective functional measurements. We also demonstrated that olfactory cleft obstruction, nasal congestion, and sinusitis were absent in most COVID-19 patients with OD. It is notable that, although overt inflammation may be absent, we have identified CD68+ macrophages carrying SARS-CoV-2 antigen in the stroma of nasal biopsy samples. This raises the possibility that COVID-19-related OD may be caused by infiltrative infection of the sustentacular cells and supporting cells of the olfactory neuroepithelium.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We thank Tracy Chui-Chi Kwok and her nursing team for assistance and logistics coordination.
Author contributions. T. W.-H. C. and S. S. designed the experiments and wrote the manuscript draft. A. J. Z., A. C.-Y. L., and Z. F. performed immunohistochemical analysis of biopsy samples and critically reviewed the manuscript. H.-L. L. performed systematic review together with T. W.-H. C. and S. S. F. K.-C. W. and R. K.-Y. T. performed nasoendoscopies and biopsies from patients. K.-H. C. and S.-M. L. performed reverse-transcriptase polymerase chain reaction analyses. M. Y.-N., S. Y. L., W.-K. K., and S. H.-Y. L. analyzed the computed tomography films. R. S.-L. H. performed histological analysis of nasal biopsy samples. K.-C. L., A. K.-L. W., W.-M. C., P. Y. N., V. C.-C. C., K. K.-W. T., and I. F.-N. H. were involved in patient recruitment, data analysis, and critical review. K.-Y. Y. conceived the study and critically reviewed the manuscript. T. W.-H. C. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. T. W.-H. C., S. S., and K.-Y. Y. were responsible for the decision to submit the manuscript.
Disclaimer. The funding sources did not play a role in the following: study design; collection, analysis, and interpretation of data; writing of the report; and decision to submit the paper for publication.
Financial support. This work was funded by Shaw Foundation Hong Kong; Michael Seak-Kan Tong; Richard Yu and Carol Yu; May Tam Mak Mei Yin; Jessie & George Ho Charitable Foundation; Perfect Shape Medical Limited; Respiratory Viral Research Foundation; Hui Ming, Hui Hoy and Chow Sin Lan Charity Fund Limited; Sanming Project of Medicine in Shenzhen, China (SZSM201911014); High Level-Hospital Program, Health Commission of Guangdong Province, China; Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases and Research Capability on Antimicrobial Resistance for Department of Health of the Hong Kong Special Administrative Region Government; Theme-Based Research Scheme (T11/707/15) of the Research Grants Council; and Hong Kong Special Administrative Region, China.
Potential conflicts of interest. S. S has received speaker’s honoraria from Sanofi-Aventis Hong Kong Limited and Abbott laboratories Limited. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Reference
- 1. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report—132 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200531-covid-19-sitrep-132.pdf?sfvrsn=d9c2eaef_2. Accessed 01 June 2020. [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol 2020. doi: 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Galougahi MK, Ghorbani J, Bakhshayeshkaram M, Naeini AS, Haseli S. Olfactory bulb magnetic resonance imaging in SARS-CoV-2-induced anosmia: the first report. Acad Radiol 2020; 27:P892-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology 2020. doi: 10.4193/Rhin20.114. [DOI] [PubMed] [Google Scholar]
- 7. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020;1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC COVID-19 Response Team. Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:477–81. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Malaty J, Malaty IA. Smell and taste disorders in primary care. Am Fam Physician 2013; 88:852–9. [PubMed] [Google Scholar]
- 11. Cain WS, Gent JF, Goodspeed RB, Leonard G. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope 1988; 98:83–8. [DOI] [PubMed] [Google Scholar]
- 12. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav 1984; 32:489–502. [DOI] [PubMed] [Google Scholar]
- 13. Hopkins C, Browne JP, Slack R, Lund V, Brown P. The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryngol Head Neck Surg 2007; 137:555–61. [DOI] [PubMed] [Google Scholar]
- 14. Chan JF, Zhang AJ, Yuan S, et al. Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID-19) in golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin Infect Dis 2020; ciaa325. doi: 10.1093/cid/ciaa325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chu H, Chan JF, Wang Y, et al. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin Infect Dis 2020; ciaa410. doi: 10.1093/jas/skz227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eliezer M, Hautefort C, Hamel AL, et al. Sudden and complete olfactory loss function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg 2020. doi: 10.1001/jamaoto.2020.0832. [DOI] [PubMed] [Google Scholar]
- 18. Gutierrez-Ortiz C, Mendez A, Rodrigo-Rey S, et al. Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology 2020. doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- 19. Jang Y, Son HJ, Lee S, Lee EJ, Kim TH, Park SY. Olfactory and taste disorder: the first and only sign in a patient with SARS-CoV-2 pneumonia. Infect Control Hosp Epidemiol 2020. doi: 10.1017/ice.2020.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klopfenstein T, Kadiane-Oussou NJ, Toko L, et al. Features of anosmia in COVID-19. Med Mal Infect 2020. doi: 10.1016/j.medmal.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moein ST, Hashemian SMR, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol 2020. doi: 10.1002/alr.22587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ollarves-Carrero MF, Rodriguez-Morales AG, Bonilla-Aldana DK, Rodriguez-Morales AJ. Anosmia in a healthcare worker with COVID-19 in Madrid, Spain. Travel Med Infect Dis 2020:101666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benezit F, Le Turnier P, Declerck C, et al. Utility of hyposmia and hypogeusia for the diagnosis of COVID-19. Lancet Infect Dis 2020. doi: 10.1016/S1473-3099(20)30297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marzano AV, Genovese G, Fabbrocini G, et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol 2020. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zayet S, N’Dri Juliette KO, Royer PY, Toko L, Gendrin V, Klopfenstein T. Coronavirus disease 2019: new things to know! J Med Virol 2020. doi: 10.1002/jmv.25874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Monti S, Balduzzi S, Delvino P, Bellis E, Quadrelli VS, Montecucco C. Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis 2020; 79:667–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giacomelli A, Pezzati L, Conti F, et al. Self -reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis 2020; ciaa330. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lytras T, Dellis G, Flountzi A, et al. High prevalence of SARS-CoV-2 infection in repatriation flights to Greece from three European countries. J Travel Med 2020; 27:taaa054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barre syndrome associated with SARS-CoV-2. N Eng J Med 2020; NEJMc2009191. doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wolfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020; 581:465–9. [DOI] [PubMed] [Google Scholar]
- 31. Beltran-Corbellini A, Chico-Garcia JL, Martinez-Poles J, et al. Acute-onset smell and taste disorders in the context of Covid-19: a pilot multicenter PCR-based case-control study. European J Neuro 2020; 10.1111/ene.14273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 2020; 323:2089‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heidari F, Karimi E, Firouzifar M, et al. Anosmia as a prominent symptom of COVID-19 infection. Rhinology 2020. doi: 10.4193/Rhin20.140. [DOI] [PubMed] [Google Scholar]
- 34. Wu J, Chandra RK, Li P, Hull BP, Turner JH. Olfactory and middle meatal cytokine levels correlate with olfactory function in chronic rhinosinusitis. Laryngoscope 2018; 128:E304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tian J, Pinto JM, Cui X, et al. Sendai virus induces persistent olfactory dysfunction in a murine model of PVOD via effects on apoptosis, cell proliferation, and response to odorants. PLoS One 2016; 11:e0159033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Plourde JR, Pyles JA, Layton RC, Vaughan SE, Tipper JL, Harrod KS. Neurovirulence of H5N1 infection in ferrets is mediated by multifocal replication in distinct permissive neuronal cell regions. PloS One 2012; 7:e46605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Perlman S, Jacobsen G, Afifi A. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology 1989; 170:556–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chu H, Chan JF-W, Yuen TT-T, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe 2020; 1:e14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brann DH, Tsukahara T, Weinreb C, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. bioRxiv 2020. doi: 10.1101/2020.03.25.009084 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. General Office of National Health Committee. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (Trial version 7). 2020. Available at: http://www.gov.cn/zhengce/zhengceku/2020-03/04/5486705/files/ae61004f930d47598711a0d4cbf874a9.pdf. Accessed 01 June 2020.
- 41. Menni C, Valdes AM, Freidin MB, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med 2020. doi: 10.1038/s41591-020-0916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.