Highlights
-
•
Only 3% of patients referred for CT for other reasons than a suspicion of COVID-19 pneumonia are diagnosed with the condition.
-
•
Asymptomatic patients with incidentally discovered COVID-19 pneumonia have predominantly mild or moderate lung involvement.
Keywords: COVID-19 pneumonia, Multidetector, Computed tomography, Incidental findings
Abbreviations: CRP, C-reactive protein; CT, computed tomography; COVID-19, Coronavirus disease 2019; GGO, ground glass opacities; RT-PCR, reverse-transcriptase polymerase chain reaction; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2
Abstract
Purpose
The purpose of this study was to determine the prevalence and imaging characteristics of incidentally diagnosed COVID-19 pneumonia on computed tomography (CT).
Materials and methods
This retrospective study was conducted between March 20th and March 31st, 2020 at Cochin hospital, Paris France. Thoracic CT examinations of all patients referred for another reason than a suspicion of SARS-CoV-2 infection were reviewed. CT images were analyzed by a chest radiologist to confirm the presence of findings consistent with COVID-19 pneumonia and quantify disease extent. Clinical and biological data (C-reactive protein serum level [CRP] and white blood cell count) of patients with CT findings suggestive for COVID-19 pneumonia were retrieved from the electronic medical chart.
Results
During the study period, among 205 diagnostic CT examinations, six examinations (6/205, 3%) in 6 different patients (4 men, 2 women; median age, 57 years) revealed images highly suggestive of COVID-19 pneumonia. The final diagnosis was confirmed by RT-PCR. Three inpatients were suspected of extra thoracic infection whereas three outpatients were either fully asymptomatic or presented with fatigue only. All had increased CRP serum level and lymphopenia. Disease extent on CT was mild to moderate in 5/6 patients (83%) and severe in 1/6 patient (17%).
Conclusion
Cumulative incidence of fortuitous diagnosis if COVID-19 pneumonia did not exceed 3% during the highest pandemic phase and was predominantly associated with limited lung involvement.
1. Introduction
The coronavirus disease (COVID)-19 pandemic led to a rapidly increasing number of patients with respiratory symptoms referred for computed tomography (CT) for a suspicion of coronavirus disease 2019 (COVID-19) pneumonia. In order to limit the risk of contamination of other patients, the radiology department of our institution decided to dedicate one CT unit for all suspicions of SARS-CoV-2 infection whereas two other CT units located in another building continued to evaluate other patients. While a severe course of SARS-CoV-2 occurs in about 4% of infected individuals who present a severe pneumonia, many patients may present with non-specific symptoms such as fever, asthenia or diarrhea, and some individuals may remain totally asymptomatic [1]. CT can reveal lung parenchyma abnormalities such as ground glass opacities (GGO) in asymptomatic patients with SARS-CoV-2 infection [2]. In a series of 24 asymptomatic patients, two-thirds had mild extension of the disease with involvement of a single lobe and only GGO on CT [3].
We hypothesized that in a high epidemic context, CT could reveal signs of infection in patients referred for CT for other reasons than a suspicion of SARS-CoV-2 infection. Several studies have reported CT findings during the early course of infection. Most of the time lung abnormalities consisted of bilateral GGO at the early stage of the disease, and band consolidations at a later stage, consistent with organizing pneumonia [1], [4], [5], [6], [7].
The purpose of this study was to determine the prevalence and imaging characteristics of incidentally diagnosed COVID-19 pneumonia on chest CT.
2. Materials and methods
2.1. Study design
This retrospective study was conducted at Cochin Hospital, Paris, France, between March 20th and March 31st, 2020. We analyzed thoracic images of all diagnostic CT examinations which have been performed on the two CT units of our institution not dedicated to the evaluation of patients with suspected or confirmed COVID-19 pneumonia.
We included all in- and outpatients who presented images highly suggestive of COVID-19 pneumonia on their chest CT, and were later confirmed of having asymptomatic COVID-19 pneumonia by reverse transcription polymerase chain reaction (RT-PCR) positivity. The requirement for informed patient consent was waived by the ethics committee of our institution (AAA-2020-08028).
2.2. CT image acquisition
All CT examinations were performed with the patient in the supine position, using two different 64-slice CT units: SOMATOM® Edge (Siemens Healthineers) or Revolution HD® (GE Healthcare).
The type of CT acquisition (thoracic or abdominal CT) and use of contrast depended on the reason for CT referral. However, all patients had an available thoracic CT acquisition with 1-mm slice reconstruction thickness and standard protocol [8], either performed at first or following the identification of abnormalities of the lung bases on abdominal CT. All reconstructed images were stored in our picture archiving and communication systems (PACS) (Carestream Version 12.1.6.0117).
2.3. Image analysis
All chest CT images were reviewed by a board-certified radiologist (M.-P. R.) with 20 years of experience in thoracic imaging. CT features highly suggestive of COVID-19 pneumonia included peripheral ground glass opacities admixed with areas of consolidation, crazy paving pattern or band consolidation, as described in previous studies [4], [9]. Focal consolidation, centrilobular nodules and mucoid impactions were considered as signs of bacterial infection. The extent of CT abnormalities was visually quantified, and considered as mild, when affecting less than 10% of the lung, moderate when involving up to 25% of the lung and severe when affecting more than 50% of the lung.
2.4. Clinical and biological data
We analyzed the frequency and type of symptoms as well as the reason for CT referral. The oxygen saturation measurement was not available at the time of CT because the patients had no respiratory symptoms. The body mass index (BMI) of each patient was calculated. Regarding biological data, we analyzed white blood cell count, platelet count and C-reactive protein (CRP) serum levels.
3. Results
Between March 20th and March 31st, 205 diagnostic CT examinations have been performed for routine indications at our Radiology Department, mainly for oncologic indications or suspicions of acute illness. Of these, six CT examinations (6/205, 3%) performed in six different patients, showed images highly suggestive of COVID-19 pneumonia. There were 4 men and 2 women with a median age of 57 years (IQR: 51, 78; range: 0–86 years). CT examinations were read first by the attending radiologist and then analyzed by the expert chest radiologist for confirmation. All patients were tested for SARS-CoV-2 infection following CT and had a positive RT-PCR result. The clinical characteristics of the 6 patients are summarized in Table 1 . Three of them were inpatients, referred for CT because they had fever and were suspected of having extra thoracic infection. They had abdominal and pelvic CT examination but the presence of opacities in the lung bases had led to perform additional chest CT. Noteworthy, one of these febrile patients had been tested by RT-PCR with a first negative result, 5 days before CT.
Table 1.
Clinical and imaging features.
| Patient # | Age (years) | Sex | Clinical symptoms | Lymphocyte count (× 109/L) | CRP (mg/L) | Indication for referral to CT | CT protocol | CT features | Lung extent on CT | Origin and number of days of hospitalization | Medical history |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 49 | M | Fever | 0.82 | 29 | Suspicion of cholangitis | Contrast-enhanced CT of the thorax, abdomen and pelvis | Diffuse bilateral GGO with consolidations and right pleural effusion | Severe (> 50%) | Inpatient 5 days |
Metastatic cholangiocarcinoma |
| 2 | 85 | M | Fatigue | 0.6 | 91 | Suspicion of neoplasia | Contrast-enhanced CT the thorax, abdomen and pelvis | Bilateral GGO with few areas of consolidation in both lower lobes | Mild (< 10%) |
Outpatient | Repeated falls and weight loss |
| 3 | 86 | F | Asymptomatic | 0.8 | 40 | Preoperative assessment of a lung nodule | Unenhanced chest CT | Patchy peripheral GGO with crazy paving in both lower lobes | Moderate (10 to 25%) |
Outpatient | Chronic obstructive pulmonary disease Spiculated lung nodule |
| 4 | 58 | M | Asymptomatic | 1.3 | 35 | Routine oncologic follow-up | Contrast enhanced CT of the thorax, abdomen and pelvis, followed by an additional thoracic CT | Discrete areas of GGO in both lower lobes with unique image of atoll sign | Mild (< 10%) |
Outpatient | Renal cell carcinoma surgically treated two years ago |
| 5 | 30 | F | Fever | 1.2 | 46 | Puerperal endometritis | Contrast-enhanced CT of the abdomen and pelvis, followed by an additional thoracic CT | Bilateral focal GGO and consolidations with linear consolidations in the left lower lobe | Mild (< 10%) |
Inpatient 4 days |
Vaginal delivery 3 days ago |
| 6 | 55 | M | Fever | 1 | 32 | Suspicion of postoperative abscess | Contrast-enhanced CT of the abdomen and pelvis followed by an additional thoracic CT | Subpleural GGO in the left lower lobe | Mild (< 10%) |
Inpatient 60 days |
Radical prostatectomy for prostate cancer 2 month ago |
Note. CT: computed tomography; GGO i: ground glass opacities; CRP: C-reactive protein; M: male; F: female.
Two totally asymptomatic outpatients were referred for CT for oncologic reasons. The last outpatient, an 85-year-old man was referred by the emergency department for suspicion of neoplasia because of recent alteration of the general status and repeated falls. None of the six patients had respiratory symptoms. The BMI of five patients was within the normal range (mean 24, range: 18–25) and one had a BMI of 28.
All six patients had elevated level of C-reactive protein (mean value 45 mg/L, range: 29–91) and lymphopenia (mean value 0.95 × 109/L, range: 0.6 × 109–1.3 × 109/L). Platelet counts were in the range of normal values (mean value 175× 109/L, range 155–230 109/L). CT showed presence of GGO in all patients, typically affecting the lower lobes with a peripheral, posterior and sub pleural distribution (Fig. 1, Fig. 2 ). Four of the six patients had mild involvement, affecting less than 10% of the lung parenchyma. One of them had only unilateral involvement. One patient had a moderate disease extent (10–25%). Only one patient had a severe pneumonia extent (> 50%) with bilateral diffuse ground glass opacities associated with consolidations and a right pleural effusion. This patient secondarily developed respiratory failure, and the disease course had a fatal outcome. The other five patients were either not hospitalized or recovered and were discharged and followed-up through teleconsultation.
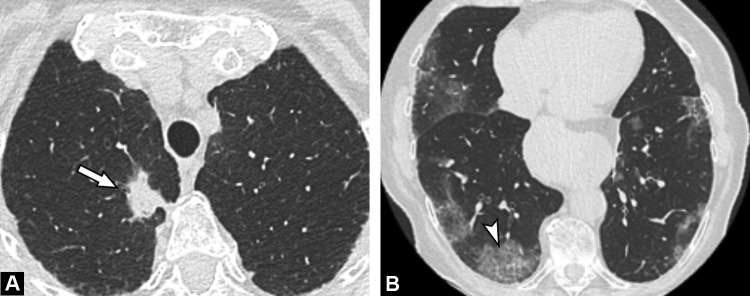
Fig. 1.
A 86-year-old asymptomatic woman with suspicion of lung cancer (Patient # 3). A, CT image of the thorax in the axial plane shows spiculated solid nodule (arrow) in right upper lobe. B, At a different level, sub pleural ground glass opacities are seen bilaterally, with superimposed intralobular thickening resulting in a crazy-paving pattern (arrowhead) in the right lower lobe.
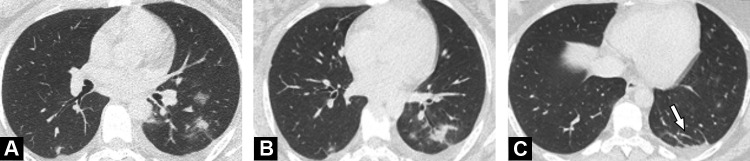
Fig. 2.
A 30-year-old asymptomatic woman treated with antibiotics for post-partum endometritis who has unexplained persistent fever (Patient #5). A, B, Unenhanced CT images in the axial plane show focal ground glass opacities and consolidations. C, At a different level, CT image shows subpleural, curvilinear lines in left lower lobe (arrow).
4. Discussion
In this retrospective evaluation, we found that 3% of the patients referred for CT for other reasons than a suspicion of COVID-19 pneumonia during the high epidemic study period were diagnosed with the condition. Half of them were febrile patients with suspicions of extra thoracic infection whereas the three others were either totally asymptomatic or only presented with fatigue. Even though this proportion is relatively low, it retrospectively justifies our decision to have our technologists provided with personal protective equipment, even when performing CT examinations with non-COVID dedicated CT unitss.
So far, only three studies and two case reports have reported incidental identification of SARS-CoV-2 related pneumonia on chest CT or positron emission tomography/CT [3], [10], [11], [12]. These studies allowed the detection of SARS-CoV-2 infection at early stages, allowing prompt isolation of the patients.
Zhang et al. compared CT features between totally asymptomatic and common type symptomatic patients. This excluded severe type defined as breathing rate ≥ 30/min, saturation ≤ 93%, mechanical ventilation shock or other organ failure. In this study, there were no significant differences in individual signs, patterns, zonal predominance or extent of CT abnormalities between common type symptomatic and asymptomatic patients [13]. We found that the majority of our patients had only minor lung involvement, in line with by An et al. [3]. Only one patient presented with more than 50% of lung involvement, but he had a metastatic cholangiocarcinoma with altered performance status, masking the symptoms of pneumonia.
Dane et al. reported COVID-19 pneumonia incidentally found on the lung bases in 23 patients referred for abdominal CT mainly for abdominal pain or diarrhea [12]. However, these researchers did not report the total number of CT examinations performed during the study period, thus it is not possible to evaluate the frequency of these incidental diagnosis [12].
The objective of our study was to obtain a prevalence analysis of COVID-19 pneumonia among patients referred for CT examination for other reasons than a suspicion of SARS-CoV-2 infection in a University Hospital in Paris, France, during the most intense phase of the pandemic. Our estimated cumulative incidence is only 3% (6/205), less than the recently derived estimate of 9% (6/65 patients) from data of department of nuclear medicine in Brescia, Italy between March 16th and March 24th [10]. However, Italy was about two weeks ahead of France regarding the spread of the virus.
In our cohort, a majority of patients had a current or a previous history of cancer. While several studies suggest a particular fragility in oncologic patients [14], our study shows that they can also present with moderate forms or even asymptomatic forms of the disease.
Our study has several limitations. First, it is a retrospective study involving a small number of patients with proven SARS-CoV-2 infection. The probability of selection bias is a concern. As mentioned, our radiology unit was supposed to receive only “non-infected patients”. Moreover, because of the current pandemic, only CT examinations for oncologic follow-up or suspicion of acute conditions were maintained. Our study population, selected on these two criteria, may be not representative of the usual patient population of a public general hospital in Paris, and our study does not allow estimating the true number of asymptomatic patients being infected.
In conclusion, even during the highest phase of the pandemic, incidental discovery of SARS-CoV-2 related pneumonia remained infrequent among patients referred for fever or oncological reasons, with asymptomatic patients having only minor disease extent on CT.
Authors’ contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
Funding
The study received no funding.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inui S., Fujikawa A., Jitsu M., Kunishima N., Watanabe S., Suzuki Y. Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiology Cardiothoracic Imaging. 2020 doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An P., Song P., Wang Y., Liu B. Asymptomatic patients with novel coronavirus disease (COVID-19) Balkan Med J. 2020 doi: 10.4274/balkanmedj.galenos.2020.2020.4.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Intervl Imaging. 2020;101:263–268. doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou Z., Guo D., Li C., Fang Z., Chen L., Yang R. Coronavirus disease 2019: initial chest CT findings. Eur Radiol. 2020 doi: 10.1007/s00330-020-06816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beregi J.P., Greffier J. Low and ultra-low dose radiation in CT: Opportunities and limitations. Diagn Interv Imaging. 2019;100:63–64. doi: 10.1016/j.diii.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 9.On behalf of the European Society of Radiology (ESR), The European Society of Thoracic Imaging (ESTI), Revel M.-P., Parkar A.P., Prosch H., Silva M. COVID-19 patients and the radiology department: advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI) Eur Radiol. 2020 doi: 10.1007/s00330-020-06865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albano D., Bertagna F., Bertolia M., Bosio G., Lucchini S., Motta F. Incidental findings suggestive of Covid-19 in asymptomatic patients undergoing nuclear medicine procedures in a high prevalence region. J Nucl Med. 2020 doi: 10.2967/jnumed.120.246256. [DOI] [PubMed] [Google Scholar]
- 11.Polverari G., Arena V., Ceci F., Pelosi E., Ianniello A., Poli E. 18F-fluorodeoxyglucose uptake in patient with asymptomatic severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019) referred to positron emission tomography/computed tomography for NSCLC restaging. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dane B., Brusca-Augello G., Kim D., Katz D.S. Unexpected findings of coronavirus disease (COVID-19) at the lung bases on abdominopelvic CT. AJR Am J Roentgenol. 2020;24:1–4. doi: 10.2214/AJR.20.23240. [DOI] [PubMed] [Google Scholar]
- 13.Zhang R., Ouyang H., Fu L., Wang S., Han J., Huang K. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. 2020 doi: 10.1007/s00330-020-06854-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desai A., Sachdeva S., Parekh T., Desai R. COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Global Oncology. 2020:557–559. doi: 10.1200/GO.20.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]