Abstract
There has been a rapid global spread of a novel coronavirus, the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which originated in Wuhan China in late 2019. A serious threat of nosocomial spread exists and as such, there is a critical necessity for well-planned and rehearsed processes during the care of the COVID-19 positive and suspected patient to minimize transmission and risk to healthcare providers and other patients. Because of the aerosolization inherent in airway management, the pediatric otolaryngologist and anesthesiologist should be intimately familiar with strategies to mitigate the high-risk periods of viral contamination that are posed to the environment and healthcare personnel during tracheal intubation and extubation procedures. Since both the pediatric otolaryngologist and anesthesiologist are directly involved in emergency airway interventions, both specialties impact the safety of caring for COVID-19 patients and are a part of overall hospital pandemic preparedness. We describe our institutional approach to COVID-19 perioperative pandemic planning at a large quaternary pediatric hospital including operating room management and remote airway management. We outline our processes for the safe and effective care of these patients with emphasis on simulation and pathways necessary to protect healthcare workers and other personnel from exposure while still providing safe, effective, and rapid care.
Keywords: COVID-19, Anesthesia, Otolaryngology, Coronavirus, Airway, Simulation
Glossary of terms
- AGP
aerosol generating procedure
- AIIR
airborne infection isolation room
- ARDS
acute respiratory distress syndrome
- BiPAP
bilevel positive airway pressure
- CDC
Center for Disease Control and Prevention
- COVID-19
disease resulting from SARS-CoV-2 infection
- CPAP
continuous positive airway pressure
- ECMO
extracorporeal membrane oxygenation
- HEPA
high-efficiency particulate air
- HFOV
high frequency oscillatory ventilation
- ICU
intensive care unit
- IR
interventional radiology
- MRI
magnetic resonance imaging
- OR
operating room
- PACU
post anesthesia care unit
- PAPR
personal air purifying respirator
- PPE
personal protective equipment
- PUI
patient under investigation
- SARS-CoV-2
2019 novel coronavirus
1. Introduction
As of June 1, 2020, the rapid global spread of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), originating in Wuhan China, has led to more than 6,000,000 confirmed cases of COVID-19 since its identification in late 2019 [1]. With over 370,000 deaths attributed to the virus, its mortality rate is estimated between 3 and 6% [2]. The majority of COVID-19 related deaths occur in individuals ≥60 years of age [3]. More than 23% have at least one comorbid condition, with hypertension being the most common (12.8%) followed by diabetes mellitus (5.3%) [4].
Pediatric patients are susceptible to SARS-CoV-2 infection, but their infection rate is debated. Initially, China reported that only 2.4% of the confirmed and suspected cases of COVID-19 were in patients ≤19 years of age. However, a subsequent report from a single large city in southern China found that the proportion of pediatric cases increased from 2% to 13% later in the outbreak [5]. Lu et al. using data collected from January 28 through February 26, 2020 from the Wuhan Children's Hospital reported that 12.3% of children, who were either symptomatic or asymptomatic with known contact to persons having confirmed or suspected COVID-19, tested positive for SARS-CoV-2 [6]. Symptom severity does appear to be milder in most pediatric cases as compared to adult cases [5]. In a large study from China, only 5.6% of children infected with SARS-CoV-2 experienced severe disease, as defined by hypoxemia, and 0.6% experienced respiratory or multiorgan failure or acute respiratory distress syndrome (ARDS) [7]. However, the impact of pediatric comorbidities on the severity of COVID-19 disease is still largely unknown.
In a Zhongnan hospital at the Wuhan University, 29% of COVID-19 cases were medical staff and 12.3% of cases were patients who contracted SARS-CoV-2 during hospitalization for other reasons [8]. Therefore, given the serious threat of nosocomial spread, there is a critical necessity for well-planned and rehearsed processes during the care of the SARS-CoV-2 positive and suspected patient to minimize transmission and risk to healthcare providers and other patients. This will require multidisciplinary in situ simulations and ‘walk-throughs,’ and hospital-wide participation to ensure a consistent approach. When emergency airway interventions are performed by pediatric otolaryngologists, the efficiency of each step is critical to best patient outcomes.
The pediatric otolaryngologist and anesthesiologist will encounter the COVID-19 patient in a variety of clinical settings (perioperative/operative, intensive care unit, emergency department, and radiology suite) and situations (emergent airway management, urgent or emergent surgical intervention, diagnostic or interventional radiology, and critical care resuscitation). The pediatric otolaryngologist's and anesthesiologist's role in the COVID-19 patient's care is often occurring within an urgent or emergent context where an increased risk of contamination and therefore threat to public health exists. Because of the aerosolization inherent in airway management, the pediatric otolaryngologist and anesthesiologist should be well-educated in and familiar with strategies to mitigate these high risk periods of viral contamination that are posed to the environment and healthcare personnel during endotracheal intubation and extubation procedures [9]. This places the pediatric otolaryngologist and anesthesiologist in a position to be able to dramatically impact and improve the safety of themselves and those caring for these patients. By assisting other disciplines in the same, these consultants are uniquely equipped to lead hospital pandemic preparedness for the COVID-19 patient. We describe our approach to COVID-19 perioperative pandemic planning at a large quaternary pediatric hospital.
2. Protocols/pathways
COVID-19 pandemic preparations constitute quality improvement efforts and are considered exempt of Institutional Review Board approval. With the spread of the COVID-19 pandemic to the United States, our initial priorities for preparation began in parallel: the Department of Pediatric Otolaryngology began devising and establishing pathways for the difficult airway management of the COVID-19 positive or suspected patient, while the Department of Pediatric Anesthesiology and Pain Medicine established an Anesthesia Covid-19 Task Force. This Task Force divided further into specific teams:
-
1.
Resource Team, tasked with researching and disseminating accurate and up-to-date COVID-19 information.
-
2.
Airway Management Team, in collaboration with otolaryngology, tasked with innovating and protocolizing airway management strategies to minimize aerosolization and environmental contamination.
-
3.
Operating Room (OR) Logistics Team, tasked with delineating workflow changes and navigating interdepartmental processes.
-
4.
Simulation Team, tasked with developing simulations for educating and preparing staff members on new processes.
2.1. Operating Room Management
Priorities in conducting simulation were established. The donning and doffing of personal protective equipment (PPE) was felt to be of the upmost importance in establishing staff safety during high-risk aerosolization procedures. A protocol was adapted from the Centers for Disease Control and Prevention (CDC) and all members of both the anesthesia and otolaryngology teams performed simulation of the protocol. Videos of our protocol were disseminated for further individual review and reinforcement of the technique. The operating room nurses were specifically trained to be our designated donning and doffing observers.
2.1.1. Intraoperative Airway Management
The creation of recommendations, processes, and checklists for management of the COVID-19 positive or suspected patient's airway were guided by the following goals:
-
1.
Optimize patient safety
-
2.
Minimize unnecessary exposure and contamination risk posed to anesthesia colleagues and OR staff
-
3.
Minimize clinical care and process errors by utilizing checklists
-
4.
Conserve personal protective equipment (PPE)
-
5.
Enhance communication among perioperative team members
Specific operating rooms were designated for use in operative cases involving COVID-19 positive patients or patients under investigation (PUI), which includes any untested patient with symptoms, recent travel, or positive contact. These operating rooms are equipped with separate air handling systems. Although not airborne infection isolation rooms (AIIR) with negative pressure ventilation systems, as recommended by the CDC for aerosol generating procedures (AGP), these ORs did have separate high-efficiency particulate air (HEPA) filtration systems and anterooms to facilitate safe donning and doffing [10]. These ORs had all non-essential equipment removed to decrease contamination risks and facilitate effective time-efficient cleaning after caring for suspected or positive COVID-19 patients. Given the minimal equipment left in these ORs after this process, all anticipated medications and supplies (patient age- and size-specific) were placed within steel portable bins and stored immediately outside of the OR for rapid and expeditious use when required. This equipment was brought into the OR at the time of case booking. The Pyxis machine and back-up equipment were housed in the anteroom and the adjacent OR where clean ‘runners’ would be able to retrieve supplies if necessary. Standard and difficult airway equipment were designated for COVID-19 positive or suspected patient's use and kept in the adjacent OR for storage. A standard COVID-19 OR setup was created to facilitate expeditious airway management and minimize environmental contamination [11]. Non-essential team members, including medical students and residents, were excluded from the management of the COVID-19 patient at our institution. The anesthesia team consisted of an attending anesthesiologist and either a fellow or a nurse anesthetist and the otolaryngology team of either two attending surgeons or an attending and a fellow.
Recommendations for anesthesia induction and endotracheal intubation were next developed, with particular attention to mitigating contamination risk, by building upon the Anesthesia Patient Safety Foundation Recommendations for Airway Management in a Patient with Suspected Coronavirus (2019-nCoV) Infection (APSF). Simulations of anesthetic induction and endotracheal intubation scenarios, emphasizing verbalization of tasks and closed loop communication among anesthesia providers, provided the groundwork for formalizing airway recommendations. This departmental approach to standard airway management in the COVID-19 positive or suspected patient was a rapid sequence induction with video laryngoscopy, which is consistent with recommendations that were published by other clinicians [12].
Modifications to the standard airway recommendations were also developed for clinical scenarios for pediatric otolaryngology patients that would lack intravenous (IV) access and require inhalation induction (e.g. emergent removal of airway foreign body) and for pediatric patients with a suspected or known difficult airway (See Appendix A: Airway Management Checklist for Potential Difficult Airway). Additionally, dedicated streamlined bronchoscopy trays containing various sizes of rigid telescopes, Parson's laryngoscopes, and suctions were created for use with the COVID-19 positive or suspected patient to avoid the need to decontaminate the larger emergency airway cart with each intervention.
Recommendations for emergence and tracheal extubation management proved more challenging with regard to protocolization. Significant innovation has been required to develop methods to minimize aerosolization and contamination during tracheal extubation. Our anesthesia department chose not to protocolize each tracheal extubation, but instead developed various strategies to be utilized at the attending anesthesiologist's discretion during the emergence process which included disposable plastic tenting over the patient, a negative pressure suction hood, reusable plexiglass patient head and torso cover, and deep tracheal extubation when feasible. However, the recovery phase of an extubated patient was protocolized to occur in the OR rather than in the post anesthesia care unit (PACU). The anesthesia and surgical team remained with the patient for 20 min following tracheal extubation, allowing for proper air-handling to occur, following which the PACU nurse entered the OR to provide recovery care along-side the anesthesiologist until the patient was deemed by both to be ready for discharge to the ward. At that time, the PACU nurse and the transport team returned the patient to the ward. If the patient required intensive care, the anesthesiologist returned the patient directly to the ICU.
2.1.2. Perioperative Simulation
After solidification of intraoperative anesthetic management of the COVID-19 positive or suspected patient, we turned our attention to the perioperative workflow that would need to occur during the operative intervention of these patients. A scripted perioperative simulation was developed for the management of an urgent surgical case. The participants included general pediatric surgeons, otolaryngologists, anesthesiologists, perioperative nursing leaders, OR nurse educators, OR charge nurses, PACU nurses, and perioperative technicians. The simulation started from the case booking and identification of the patient's positive or suspected COVID-19 status. The most important point of the workflow involved a mandatory huddle within 10 min following the case booking with discussion of the following elements of the case between the anesthesiologist, surgeon, and OR Charge nurse:
-
•
Determine potential for difficult airway (request pediatric otolaryngology presence and initiate COVID-19 Potential Difficult Airway Protocol).
-
•
Designate trained PPE Donning/Doffing observer.
-
•
Confirm contact person for consent (phone consent expected prior to patient transport to minimize contamination).
-
•
Discuss anticipated transportation route (all patients to enter OR directly).
-
•Surgical medications anticipated.
-
○Anesthesia administered (eg. antibiotics, steroids, osmotic diuretics, anti-epileptic agents)
-
○Nursing administered (eg. local anesthetic agents, irrigation solutions)
-
○
-
•
Preoperative laboratory status.
-
•
Blood product needs and availability.
-
•
Special surgical equipment.
-
•
Anticipated patient disposition following surgery.
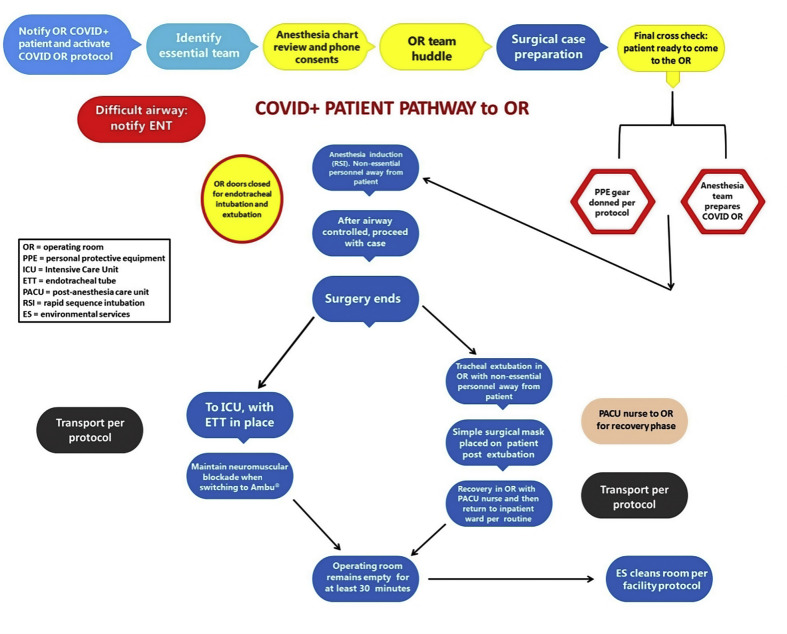
The anesthesia, surgical, and nursing teams then proceeded with the simulated case, incorporating the COVID-19 measures each team had already prepared. During the course of the in-situ simulation, questions in management of the COVID-19 patient and environment were raised at the time of the simulation and addressed with input from the various stakeholders. As a result of this initial perioperative simulation, a perioperative COVID-19 protocol was developed, and an overarching perioperative workflow established (Fig. 1 ). The perioperative simulation was then re-created with the nursing and surgical leaders for each surgical subspecialty.
Fig. 1.
Pathway for care of COVID-19 patient and transport to the operating room.
2.2. Remote Airway Management
Emergent Airway Management: To date, the need for invasive or emergency airway interventions in SARS-CoV-2 infected patients has remained low as it has been reported that only 0.6% of pediatric patients with SARS-CoV-2 infection experience respiratory or multi-organ failure [7]. Yet, it is common for children to present to the emergency department (ED) and ICU with respiratory distress, whether related to viral infections or other etiologies. In such scenarios, the etiology of respiratory failure may remain under investigation as SARS-CoV-2 testing is pending. Respiratory support for children with respiratory insufficiency or failure may include nebulized aerosol treatments and non-invasive ventilatory support such as high-flow nasal cannula, continuous positive airway pressure (CPAP), non-invasive ventilation including bilevel positive airway pressure (BiPAP), as well as endotracheal intubation and positive pressure ventilation.
In our institution, the pediatric anesthesiology and/or otolaryngology departments (depending on clinical situation) serve as back-up for emergency airway management for the ED and ICUs. During the COVID-19 pandemic, given that there are now added precautions that need to be taken prior to managing an airway, it was important that the ED, ICUs, otolaryngology, and anesthesiology departments align their goals and expectations, but also appreciate the different challenges each unit presents in comparison to the controlled environment of the operating room. For example, in the operating room, the goal of airway management was to decrease environmental contamination so that the rest of the anesthetic care and surgical intervention could proceed under relatively clean conditions. While the patient is in the ED or ICU, multiple interventions may be performed prior to endotracheal intubation, such as aerosol treatments or respiratory assistance with non-invasive ventilation, which are all considered AGPs. From the ED or ICU perspective, everything about the patient encounter is high risk for the health care worker.
We aimed to augment the existing airway management strategies and protocols with high-value infection control related addenda. In order to create a universal guideline that would be useful in environments as different as the OR, ED, and ICUs we focused on two core principles:
-
1.
Minimizing contamination risk.
-
2.
Defining the pathways for escalating the expertise for airway management.
Toward the first goal for a universal guideline-minimizing contamination risk-the following points were added to each department's COVID-19 intubation protocols:
-
•
Donning and doffing areas will be clearly marked.
-
•
Intubation team will wear head coverings, such as the bouffant (common to the OR, but not routinely used in the ICU and ED).
-
•
Intubation team will double glove.
-
•
Non-essential staff members will leave the room during intubation.
-
•
Individual roles will be clearly delineated prior to beginning airway management.
-
•
Trainees will not be allowed to be the primary person managing the airway.
-
•
Viral filters will be used after intubation and during transport.
-
•
Inadvertent contamination from fresh oxygen flow through Ambu bags will be minimized by using lowest possible flow.
-
•
Inadvertent contamination from airway equipment will be minimized by ensuring strict attention to processes.
-
•
Videolaryngoscopy will be used as a first-line technique.
-
•
Intubation team will be dismissed immediately after the airway is secured for doffing following airway management.
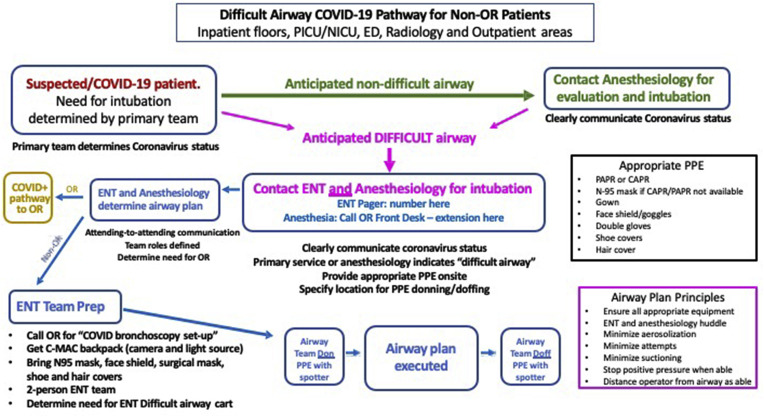
The second aspect for a universal guideline was to offer guidance for when and how to alert the otolaryngology and/or anesthesiology staff for assistance (Fig. 2 ). An emphasis was placed on early communication with these services to afford sufficient time for resource mobilization. The following guidelines were developed as pathways for escalating airway expertise in COVID-19 patients:
-
1.Consider endotracheal intubation by Primary Team if:
-
○Non-invasive ventilation requirements exceed 16/8 cm H2O
-
○FiO2 ≥ 0.5 for more than 4 h
-
○Frequent suctioning is needed
-
○
-
2.Consider consultation with Anesthesiology if:
-
○Significant comorbid conditions exist
-
○Cardiac or pulmonary status is rapidly deteriorating
-
○
-
3.Consider consultation with Otolaryngology if:
-
○Difficult airway by exam or history as per standard difficult airway pathway
-
○
Fig. 2.
Non-perioperative care for the COVID-19 patient with a potentially difficult airway needing activation of Otolaryngology and/or Anesthesia services.
CAPR: controlled air purifying respirator
ED: emergency department
NICU: neonatal intensive care unit
OR: operating room
PAPR: powered air purifying respirator
PICU: pediatric intensive care unit
PPE: personal protective equipment.
When the primary team has determined that the intubation assistance is required, they are to provide the following information:
-
○
Location
-
○
Age and weight of patient
-
○
Urgency
-
○
Suspected difficult airway
-
○
COVID-19 status
Once the anesthesiology team arrives, they assume all airway responsibilities and determine who remains in the room during endotracheal intubation. This represents a transition from our previous practice of allowing advanced trainees in the ED or ICU to manage the airway under the anesthesiologist's guidance. To prepare for this, the anesthesiology department created a special emergency bag containing PPE and cleaning equipment, advanced airway equipment for use outside the operating room suites, and induction medication. This allowed the anesthesiology team to be self-sufficient and work in a manner more consistent with our workflow in the operating room.
Likewise, the otolaryngology team prepared a separate emergency bag containing a C-MAC monitor, camera attachment, and portable battery light source with backup PPE for their use in emergent remote airway management situations involving COVID-19 positive or suspected patients. However, if surgical airway was anticipated and the patient was deemed stable for expedited transport, a path to the OR was preferable over bedside surgical interventions that would expose numerous providers (Fig. 2).
Remote emergency airway management was not simulated, as the ED and ICUs had too many faculty and staff who would need to be involved and trained. Rather, we felt dissemination of the information by our departmental liaisons was appropriate and we instead focused simulation efforts on managing the possible operative and anesthetic interventions that would be required for a difficult airway.
3. Discussion
The literature contains a paucity of information describing the collaboration of the pediatric otolaryngologist and anesthesiologist for pandemic airway preparedness. The COVID-19 pandemic is a public health crisis in which an estimated 19,481 individuals will require endotracheal intubation during peak demand in the United States [13]. In order to mitigate contamination risk, COVID-19 patients should be intubated by the most skilled providers, underscoring the important role of the pediatric otolaryngologist and anesthesiologist.
In situ simulation is a vital aspect for disaster preparation, as it has been shown to improve clinical skills, teamwork, patient safety, and reliability in high-risk and high-stress environments [14,15]. In our COVID-19 preparations, interdisciplinary cooperation was helpful for identifying problems that each individual department had not previously recognized and addressed. Each simulation and ‘walk-through’ exercise improved communication, workflow, and response times. As a result of these simulations, potential barriers, omissions, and issues were identified. These resulted in modifications to existing protocols which aimed to add infection control-specific principles and facilitate patient care.
Barriers did exist to the development and implementation of these protocols and simulations. With the initial confinement of SARS-Co-V-2 to international locations, the impact the virus would have within our community if spread occurred was difficult to ascertain. Given that the potential pandemic nature of SARS-Co-V-2 was not recognized on a national level early, large-scale preparations for the pandemic were delayed until COVID-19 cases were already present within the community. At that point, a critical time constraint became evident, which demanded that we mobilize resources quickly to develop these pathways. One key factor in being able to do this was that we quickly stopped all elective surgical cases in institutions which provided the necessary time and manpower requirements to develop these strategies.
Given that the initial reports from China indicated low pediatric infection rates, it is possible that the public health impact COVID-19 would have within a pediatric hospital was underestimated. It is possible that as a result, some have questioned the need to adopt changes in pediatric practices related to the pandemic [5]. During a pandemic, there are particular populations that may not manifest symptoms related to the disease but who unwittingly pose as a major public health threat by serving as a vector for spread [16,17]. The asymptomatic carrier state is particularly dangerous with regards to nosocomial spread of infection as healthcare workers may not employ full COVID-19 precautions in caring for the seemingly uninfected patient. AGPs, such as endotracheal intubation and extubation, which under other circumstances appear routine, become high-risk for disease transmission to healthcare providers. Therefore, during a pandemic situation, it is imperative to treat all populations, with the same screening procedures and precautions.
Fortunately, the COVID-19 related case burden in our center has been low to this point, in part because of an aggressive state government that enacted very early school closures and ‘stay-at-home’ orders in conjunction with federal social distancing guidelines. In a 21st century global economy where the air travel is a major facilitator in international disease distribution, the spread of novel pathogens leading to a pandemic of comparable proportion to COVID-19 is not likely to be a singular isolated event [18]. It is imperative, therefore, that going forward pediatric otolaryngology and anesthesiology departments maintain this level of basic collaborative preparation for these situations.
Financial disclosures
None.
Author contributions
Brittany L. Willer, MD: This author wrote the article and was the leader of the Nationwide Children’s Hospital COVID-19 Simulation Team.
Arlyne K. Thung, MD: This author wrote sections of the article and was the leader of the Nationwide Children’s Hospital COVID-19 Airway Management Team.
Marco Corridore, MD: This author wrote sections of the article and was the liaison for the Nationwide Children’s Hospital COVID-19 Airway Management Team to the Emergency Department and the Pediatric Intensive Care Unit.
Ajay J. D’Mello, MD: This author helped develop the Nationwide Children’s Hospital COVID-19 Airway Management Protocol.
Brian S. Schloss, MD: This author wrote sections of the article and was the co-leader of the Nationwide Children’s Hospital COVID-19 Operating Room Logistics Team.
Prashant S. Malhotra, MD: This author helped develop the Nationwide Children’s Hospital Otolaryngology Difficult Airway Covid-19 Pathway.
Patrick C. Walz, MD: This author helped develop the Nationwide Children’s Hospital Otolaryngology Difficult Airway Covid-19 Pathway.
Charles A. Elmaraghy, MD: This author helped develop the Nationwide Children’s Hospital Otolaryngology Difficult Airway Covid-19 Pathway.
Joseph D. Tobias, MD: This author wrote sections of the article and as the Chair of the Department of Anesthesiology and Pain Medicine of Nationwide Children’s Hospital, oversaw the creation of the COVID-19 Task Force.
Kris R. Jatana, MD: This author co-wrote sections of the article.
Vidya T. Raman, MD, MBA: This author wrote sections of the article and created and lead the COVID-19 Task Force of Nationwide Children’s Hospital.
Declaration of competing interest
None.
Acknowledgements
We would like to thank the Nationwide Children's Hospital perioperative nursing staff and nursing leaders, Dr. Marc Michalsky of the General Surgery team, Dr. Mark Hall and Dr. Onsy Ayad of the Pediatric Intensive Care Unit team, and Dr. Berkeley L. Bennett of the Emergency Department team for their participation in our perioperative and hospital-wide simulations. We would especially like to thank our tireless department of anesthesiologists, fellows, and nurse anesthetists who helped make these large-scale COVID-19 preparations a success.
Appendix A. AIRWAY MANAGEMENT CHECKLIST FOR POTENTIAL DIFFICULT AIRWAY
-
•
Designation and confirmation of airway team roles: Pediatric Otolaryngology and Pediatric Anesthesia
-
•
Confirmation of all airway equipment including specialized Pediatric Otolaryngology and Anesthesia Difficult Airway equipment to include flexible bronchoscope, rigid bronchoscope, and emergency tracheostomy access
-
•Anesthesia Plan: have available
-
•Standard airway equipment including endotracheal tubes (ETTs) and Air-Q laryngeal mask airway (LMA)
-
•
-
•Otolaryngology Plan: have available
-
•Parson's laryngoscope with rigid bronchoscopy and tracheostomy set
-
•
-
•
Confirmation of airway plan to include anesthesia induction, initial airway management plan, contingency plans, and when/how pediatric anesthesia to hand-off to pediatric otolaryngology
-
•Confirmation of medications along with saline flushes, syringes needed for case.
-
1.Premedication/Induction medications to be drawn up in patient specific dosing
-
2.Emergency medications
-
3.Additional medications such as muscle relaxation and reversal
-
1.
-
•Final check:
-
1.Reconfirmation of primary airway plan; back up airway plan; extubation plan
-
2.Reconfirmation of roles
-
3.Confirmation surgical/anesthesia consent obtained
-
1.
-
•
Hand hygiene/Donning before patient enters the room
References
- 1.World Health Organization . 2020. Coronavirus Disease (COVID-2019) Situation Reports: Situation Report-133.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ Accessed June 2, 2020. [Google Scholar]
- 2.Baud D., Qi X., Nielsen-Saines K., Musso D., Pomar L., Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30195-X. [published online ahead of print Mar 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC Covid-19 Response Team Severe outcomes among patients with coronavirus disease (COVID-19) MMWR (Morb. Mortal. Wkly. Rep.) 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liuxingbingxue Zazhi. 2020;41(2):145–151. [Google Scholar]
- 5.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): information for pediatric healthcare providers. 2020. cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html Accessed April 8, 2020.
- 6.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J. SARS-CoV-2 Infection in children. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2005073. [published online ahead of print March 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [published online ahead of print March 16. [DOI] [Google Scholar]
- 8.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.1585. [published online ahead of print Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4) doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): interim infection prevention recommendations for patients suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. 2020. cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html Accessed April 8, 2020.
- 11.Dexter F., Parra M.C., Brown J.R., Loftus R.W. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth. Analg. 2020 doi: 10.1213/ANE.0000000000004829. [published online ahead of print Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orser B.A. Recommendations for endotracheal intubation of COVID-19 patients. Anesth. Analg. 2020 doi: 10.1213/ANE.0000000000004803. [published online ahead of print Mar 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray C.J. IHME, University of Washington; Seattle, WA: 2020. Forecasting COVID-19 Impact on Hospital Bed-Days, ICU-Days, Ventilator-Days and Deaths by US State in the Next 4 Months. Institute for Health Metrics and Evaluation (IHME) [DOI] [Google Scholar]
- 14.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can. J. Anaesth. 2020 doi: 10.1007/s12630-020-01620-9. [published online ahead of print Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurup V., Matei V., Ray J. Role of in-situ simulation for training in healthcare: opportunities and challenges. Curr. Opin. Anaesthesiol. 2017;30(6):755–760. doi: 10.1097/ACO.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 16.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.2565. [published online ahead of print Feb 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. [published online ahead of print Mar 4 2020] J. Microbiol. Immunol. Infect.. doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed]
- 18.Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Ichii H., Zacharski M. The association between international and domestic air traffic and the coronavirus (COVID-19) outbreak. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.03.026. [published online ahead of print Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]