Summary
In modern societies, human rest–activity rhythms and sleep result from the tensions and dynamics between the conflicting poles of external social time (e.g., work hours and leisure activities) and an individual’s internal biological time. A mismatch between the two has been suggested to induce ‘social jetlag’ [1] and ‘social sleep restriction’, that is, shifts in sleep timing and differences in sleep duration between work days and free days. Social jetlag [2,3] and sleep restrictions [4] have repeatedly been associated with negative consequences on health, mental wellbeing, and performance. In a large-scale quasi-experimental design, we investigated the effects of the phase with the most rigorous COVID-19 restrictions on the relationship between social and biological rhythms as well as sleep during a six-week period (mid-March until end of April 2020) in three European societies (Austria, Germany, Switzerland). We found that, on one hand, the restrictions reduced the mismatch between external (social) and internal (biological) sleep–wake timing, as indexed by significant reductions in social jetlag and social sleep restriction, with a concomitant increase in sleep duration. Sleep quality on the other hand was slightly reduced. The improved individual sleep–wake timing can presumably be attributed to an increased flexibility of social schedules, for instance due to more work being accomplished from home. However, this unprecedented situation also led to a significant increase in self-perceived burden, which was attendant to the decrease in sleep quality. These adverse effects may be alleviated by exposure to natural daylight as well as physical exercise.
Blume et al. study the effects of the COVID-19 lockdown on the mismatch between social and biological sleep–wake timing as well as sleep. Increased flexibility of social schedules reduced the mismatch while sleep quality was reduced, possibly due to increased burden. These adverse effects may be alleviated by daylight exposure and exercise.
Main Text
Austria entered the strictest form of the COVID-19 ‘lockdown’ on 13 March 2020, Switzerland on 16 March, and in Germany the most rigorous regulations took effect on 23 March (in some federal states even earlier). This meant that all schools and shops, except for stores selling basic supplies (e.g., food shops, drug stores, and pharmacies), were closed. Contact bans were introduced, and freedom to travel was restricted by borders being closed and public transportation being reduced to a minimum. Moreover, public life came to a standstill and a large proportion of employees started working from home. In a one-time online survey addressing people in Switzerland, Germany, and Austria, we studied the effects of the lockdown on social jetlag, social sleep restriction, sleep quality, and sleep duration between 23 March and 26 April 2020. A total of 435 valid datasets were obtained during this period (327 women, four diverse; median age group 26–35 years). The majority of respondents had a rather high socioeconomic status and high educational level (Supplemental Information, published with this article online). The survey included (i) questions to assess volunteers’ sleep quality and social sleep restriction (i.e., difference in sleep duration between work days and free days), and (ii) an ultra-short version of the Munich Chronotype Questionnaire [5] to assess social jetlag (i.e., the difference in mid-sleep between work days and free days). Additionally, we assessed (iii) life satisfaction and (iv) collected detailed background information (see Supplemental Information). Importantly, questionnaires i–iii were answered twice in a row, once retrospectively referring to the time before the lockdown and once referring to the time since participants noticed the restrictions.
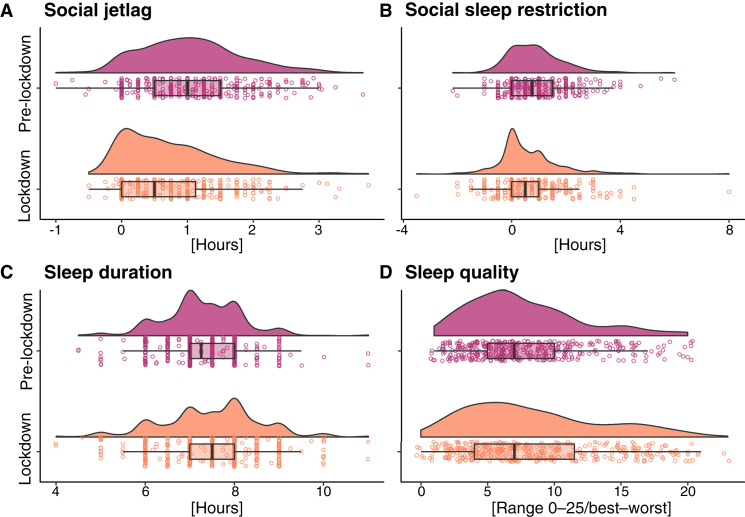
We preregistered our hypotheses and statistical analyses prior to human data inspection [6]. Advanced non-parametric analyses (see Supplemental Information) revealed that the COVID-19 lockdown reduced the mismatch between external (social) and internal (biological) sleep–wake timing, which was probably due to the responders’ increased flexibility of social schedules (i.e., external time). In particular, during the six-week period, median social jetlag was reduced by 13 minutes (inter-quartile range [IQR] = –31–17 min; Figure 1 A) and median social sleep restriction by 25 minutes (IQR = –51–5 min; Figure 1B). The improved alignment was also associated with a median increase in sleep duration by about 13 minutes (IQR = –25–51 min; Figure 1C). The reduction in social jetlag was driven by a delay in mid-sleep on work days during the lockdown. One factor that was consistently associated with the ameliorated alignment was an increase in the proportion of work accomplished from home, which in turn was linked to an increased flexibility of working hours. Additionally, a reduction in working hours but not leisure time activities during the lockdown was associated with the ‘improved’ alignment. In line with previous findings, particularly later chronotypes seemed to benefit from the lockdown in terms of a reduced discrepancy between social and biological sleep–wake timing [1,7].
Figure 1.
Effects of the ‘lockdown’ on social jetlag, social sleep restriction, sleep duration, and sleep quality.
Social jetlag (i.e., the difference between mid-sleep on free days and work days) is reduced by 13 minutes (A), and social sleep restriction (i.e., the difference in sleep duration between free days and work days) by 25 minutes (B). Sleep duration is increased by 13 minutes (C) while sleep quality (higher values denote decreased sleep quality) is reduced by 0.25 points on a scale from 0–25 (D). Reported differences are interpolated medians of individual differences. Each plot depicts the probability density of the data on top of a boxplot with overlying individual data points. Boxplots: lower and upper hinges correspond to the first and third quartiles (the 25th and 75th percentiles) and the thick vertical line in the box corresponds to the median. The upper (lower) whisker extends from the hinge to the largest (smallest) value no further than 1.5 ∗ inter-quartile range (IQR, or distance between the first and third quartiles).
Beyond this, overall sleep quality slightly decreased during the lockdown by 0.25 points on a scale from 0–25 (higher values indicating decreased sleep quality; IQR = –1.6–2.8; Figure 1D). We observed an increase in subjective burden and a decrease in mental and physical wellbeing, which likely resulted from the exceptional situation due to the pandemic and was associated with decreased sleep quality and sleep duration. The strength of these effects may even have masked a link between reduced social jetlag and positive effects on sleep quality, which has previously been reported [8]. On a more positive note, we were also able to identify factors that limited the decline in sleep quality during the lockdown. These included a reduction in social sleep restriction, that is, the harmonisation of sleep duration across work and free days, as well as a reduction in working hours. Moreover, increases in daylight exposure and exercise may have buffered the negative effects of the lockdown and were associated with less decreased sleep quality and increased sleep duration. Possibly, these factors were able to reduce lockdown-induced stress [9].
In sum, in the three European countries included in this study, the COVID-19 lockdown, during which public life came to a standstill and many people experienced increased flexibility regarding social schedules, led to improved individual sleep–wake timing and overall more sleep. At the same time, however, many people suffered from a decrease in sleep quality in this burdening and exceptional situation. Potential strategies to mitigate the adverse effects of the lockdown on sleep quality may include exposure to natural daylight and exercise.
Footnotes
Supplemental Information contains one figure, one table, and experimental procedures, all of which can be found with this article online at https://doi.org/10.1016/j.cub.2020.06.021.
Supplemental Information
References
- 1.Wittmann M., Dinich J., Merrow M., Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol. Int. 2006;23:497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 2.Wong P.M., Hasler B.P., Kamarck T.W., Muldoon M.F., Manuck S.B. Social jetlag, chronotype, and cardiometabolic risk. J. Clin. Endocrinol. Metab. 2015;100:4612–4620. doi: 10.1210/jc.2015-2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levandovski R., Dantas G., Fernandes L.C., Caumo W., Torres I., Roenneberg T., Hidalgo M.P.L., Allebrandt K.V. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol. Int. 2011;28:771–778. doi: 10.3109/07420528.2011.602445. [DOI] [PubMed] [Google Scholar]
- 4.Depner C.M., Melanson E.L., Eckel R.H., Snell-Bergeon J.K., Perreault L., Bergman B.C., Higgins J.A., Guerin M.K., Stothard E.R., Morton S.J. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr. Biol. 2019;29:957–967.e4. doi: 10.1016/j.cub.2019.01.069. [DOI] [PubMed] [Google Scholar]
- 5.Ghotbi N., Pilz L.K., Winnebeck E.C., Vetter C., Zerbini G., Lenssen D., Frighetto G., Salamanca M., Costa R., Montagnese S., Roenneberg T. The μMCTQ: an ultra-short version of the Munich ChronoType Questionnaire. J. Biol. Rhythms. 2019;35:98–110. doi: 10.1177/0748730419886986. [DOI] [PubMed] [Google Scholar]
- 6.Blume C., Schmidt M., Cajochen C. Sleep and social jetlag during COVID-19. Open Science Framework. 2020 doi: 10.17605/osf.io/mhsw8. [DOI] [Google Scholar]
- 7.Roepke S.E., Duffy J.F. Differential impact of chronotype on weekday and weekend sleep timing and duration. Nat. Sci. Sleep. 2010;2010:213–220. doi: 10.2147/NSS.S12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raman S., Coogan A.N. A cross-sectional study of the associations between chronotype, social jetlag and subjective sleep quality in healthy adults. Clocks Sleep. 2020;2:1–6. doi: 10.3390/clockssleep2010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Quervain D., Aerni A., Amini E., Bentz D., Coynel D., Gerhards C., Fehlmann B., Freytag V., Papassotiropoulos A., Schicktanz N. The Swiss Corona Stress Study. Open Science Framework. 2020 doi: 10.31219/osf.io/jqw6a. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.