Summary
This prospective observational cohort study is based on the first 500 patients who requested emergency teleconsultation during the initial days of the COVID-19 lockdown in Paris, France between 20 March and 10 April 2020. It is the first study to assess the utility of emergency teleophthalmology with a simple smartphone application or web browser and a webcam to manage emergency eye care in a population with sudden restricted access to ophthalmologists. In this study, every patient who asked for an ophthalmic emergency consultation in a single specialized center in Paris (‘SOS Œil’) first had to undergo a teleconsultation appointment to evaluate the indication for a physical consultation to preserve lockdown. Under medical advice only, a physical appointment was given within a day (if necessary). The aim of the study was to describe the population and diagnoses and evaluate the main judgment criteria, defined as the ‘ability of teleconsultation to properly indicate a physical consultation for fair diagnosis and treatment in eye emergencies’. This organization has permitted physicians and patients to preserve social distancing while avoiding 3 or 4 physical consultations per person. Notably, 27% of teleconsultations were followed by a physical appointment. There was a mean 4.12-day delay between symptom apparition and consultation, and less than 1 day for traumas, superficial corneal foreign body and neuro-ophthalmological emergencies. There was a 96% sensitivity and 95% specificity to properly evaluate the indication of a physical consultation and only 1.0% misdiagnoses that lead to delayed care. Hence, teleconsultation maintained satisfactory healthcare access to patients with severe ophthalmological disorders while preserving social distancing and sanitary precautions. Therefore, teleconsultation may be seriously considered as a way to efficiently regulate ophthalmic emergencies, especially for patients with limited access to a specialist.
Keywords: Teleophthalmology, Emergency ophthalmology, COVID-19, Lockdown, Social distancing
Résumé
Il s’agit d’une étude observationnelle prospective concernant les 500 premiers patients pris en charge pour une téléconsultation d’urgence ophtalmologique lors de la première quinzaine du confinement en France. Il s’agit de la première étude montrant l’utilité de la télé ophtalmologie à l’aide seule d’un smartphone ou d’un navigateur internet équipés d’une webcam pour trier et organiser la prise en charge des urgences ophtalmologiques dans une population soudainement restreinte dans son accès aux soins. Dans cette étude, tout patient réclamant une consultation au centre ophtalmologique (« SOS Œil ») à Paris se voyait proposer un rendez-vous de téléconsultation préalable afin d’évaluer l’indication ou non à une consultation physique et à une rupture du confinement. Sur avis médical, un rendez-vous physique était donné le jour même si nécessaire. L’objectif de l’étude était de décrire la population, les pathologies avec pour critère de jugement principal « la capacité de la téléconsultation à indiquer un rendez-vous physique pour un diagnostic et une prise en charge adéquat ». Cette organisation a permis aux praticiens et aux patients un maintien des mesures de distanciation sociale tout en évitant 3 consultations physiques sur 4. Au total, 27 % des téléconsultations aboutissaient à un rendez-vous physique. Le délai moyen entre l’apparition des symptômes et la téléconsultation était de 4,12 jours, mais moins d’1 jour pour les traumatismes, corps étrangers et troubles neuro-ophtalmologiques. La téléconsultation a montré une sensibilité de 96 % et une spécificité de 95 % à poser une indication correcte de consultation physique avec seulement 1 % d’erreurs diagnostiques conduisant à un retard de prise en charge. De fait, la téléconsultation a permis un maintien satisfaisant de l’accès aux soins ophtalmologiques d’urgence tout en préservant les mesures d’hygiène et de distanciation sociale. La téléconsultation peut être considérée comme un moyen efficace pour réguler l’accès aux services d’urgences ophtalmologiques, et ce particulièrement pour les patients ayant un accès aux soins spécialisés limité.
Mots clés: Téléophtalmologie, Urgences ophtalmologiques, COVID-19, Confinement, Distanciation sociale
Introduction
In the midst of the COVID-19 pandemic, healthcare systems and its providers are endangered. High-volume specialties such as ophthalmology impose important risks for practitioners during physical examination and for patients in waiting rooms, especially for services that experience fluctuating frequencies, such as emergency ophthalmologic departments. There is strong consensus with regard to waiting room social distancing measures and healthcare and patient protective equipment [1]. Teleconsultation (TC) is proposed as a solution to maintain healthcare access and manage the flow in ophthalmology, but its organization remains unclear. Teleophthalmology already has several applications in age-related macular degeneration [2], [3] and diabetic retinopathy [4], [5], [6] requiring fundus cameras and/or optical coherence tomography apparels. Emergency teleophthalmology can utilize remote slit lamp and camera systems [7], [8], [9] or differed tele-expertise with photos for military [10] or remote and poor areas [11].
To maintain healthcare access during the COVID-19 lockdown in France, TC has been facilitated by the French government. New patient care has been allowed, and TCs are fully reimbursed by social security. The COVID-19 pandemic increased TC by 800% in France; it represented 10% of the consultations during lockdown.
Our study aimed to assess the efficiency and security of TC with only a laptop computer or smartphone to manage the flow of ophthalmic emergencies, in a specialized emergency ophthalmology office in Paris. The main judgment criterion was defined as the ability of TC to properly indicate a physical consultation (PC) for fair diagnosis and treatment in eye emergencies.
Method
This prospective observational cohort study was conducted on the first 500 patients who received a TC at ‘SOS Œil’, a primary and secondary ophthalmic emergency office in Paris, France. Inclusion lasted from 20 March to 10 April 2020. TC was performed using Doctolib® (Levallois, France), the leading booking platform in France. Patients could access the consultation on a mobile application, tablet or their web browser. The ophthalmologist used his or her laptop computer with remote access to Area® (Soletys, France) ophthalmologic software.
TC was led by five ophthalmologists (1 per day) from 09:00 to 20:00 h 7 days a week; a second ophthalmologist was present for a PC. After TC triage, the ophthalmologist relayed to his or her colleagues’ emergencies that required a physical appointment. The ophthalmologists are experienced residents who are familiar with managing ophthalmic emergencies.
TC followed a standardized protocol:
-
•
displayed on the center website (https://centreophta.com/), the patient had to read the general conditions explaining that TC was for emergency cases only. The purpose of TC was expressed as ‘evaluating the indication to break lockdown’;
-
•
after approving the conditions, the patients could log onto Doctolib®, a TC solution. In case of technical difficulties, a hotline with a secretary was available to help the patient. In case of failure, the ophthalmologist made a direct phone call to evaluate the need for a PC and oriented the patient to the appropriate practitioner or center;
-
•
during TC, the main purpose for the ophthalmologist was to evaluate the indication for a PC. If he or she felt limited with regard to the diagnosis, a PC was given for the same day or the day after (according to the symptoms). There were no guidelines for providing patients with appointments. It was only based on the physician's experience.
During TC, the ophthalmologist followed a standardized protocol: reason for the consultation, when the symptoms began, suspicion of COVID-19 infection and ophthalmologic past medical history — including uveitis, herpes, ocular hypertension or glaucoma, refractive surgery, high myopia, contact lenses wear and unilateral blindness. Screenshots using the patient's webcam could be captured by the practitioner and the patient could use their webcam or scanner to send document(s) estimated to be useful for the consultation.
At the end of the consultation, the ophthalmologist had two options:
-
•
if the TC permitted a certain diagnosis, the ophthalmologist sent a prescription and explained to the patient the normal evolution of the pathology. If the evolution differed, the patient had a direct phone number or email access to the center. At this point, the patients were classified into the chronic follow-up or medical simple anterior segment disorder group;
-
•
if the TC did not permit a clear diagnosis, an appointment was made with the patient at the center or the patient was referred to the nearest colleague if they lived too far away. A diagnostic hypothesis was made by the practitioner and his or her estimation despite the lack of clinical information in TC: visual acuity, intraocular pressure, slit-lamp examination, optical coherence tomography or need for treatment. At this point, the patients were classified into one of three other pathology groups: moderately severe anterior segment disorder (superficial foreign body, herpes virus (HSV) or varicella zoster (VZV) suspicion, episcleritis, preseptal cellulitis, facial paralysis), severe anterior segment disorder (uveitis and corneal abscess suspicion) or vitreoretinal disorder (posterior vitreous detachment, retinal tear or detachment, exudative age macular disease). Patients with a neuro-ophthalmological disorder were directly referred to the nearest tertiary care center. Patients with interrupted post-operative follow-up were free to come for an eye examination. In the case of PC refusal, the practitioner explained the high risk of severe eye damages, and he or she treated the condition in the most appropriate manner depending on his or her hypothesized diagnosis. In this case, the patients were systematically contacted 5 to 7 days after the TC.
During the PC, the practitioner evaluated the severity of the diagnosis and considered whether the PC was appropriate. Overestimated diagnoses were considered to be false positives, whereas patients with underestimated diagnoses were false negatives. Patients with a justified PC were considered to be true positives and patients managed in TC only with an expected good evolution were considered to be true negatives. To confirm true negatives evaluation, 10% of patients who were initially only treated with TC were contacted 5 to 7 days after TC to assess whether there was good evolution of their symptoms.
Analysis
Patients’ characteristics were analyzed using XLstat® and Pvalue.io® software. Simple anterior segment disorder group characteristics were compared to moderately severe or severe anterior segment disorder, retinal and neuro-ophthalmological emergencies, using the Kruskal-Wallis test for non-parametric data and Fisher's exact or chi-square test for qualitative analysis. TC sensitivity was defined as the number of PCs requested by the practitioners among the total number of appropriate PCs according to the main judgment criterion. TC specificity was defined as the number of patients managed with only TC among the patients who had no need for PC. The positive predictive value was defined as the number of appropriate PCs among the total number of PCs. The negative predictive value was defined as the number of patients appropriately managed with TC among the patients estimated to only require TC.
Results
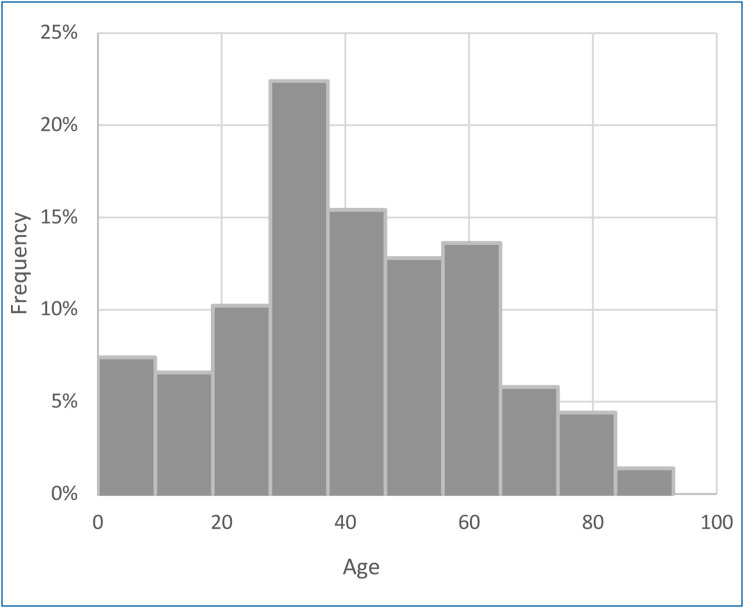
The 500 patients were prospectively included starting 3 days after the lockdown began, between 20 March and 10 April 2020. A mean number of 26.2 ± 5.2 TCs were conducted each day. The population's mean age was 40.7 ± 20.3 (0.6–92) years, with clearly fewer patients over 60 years old (Fig. 1 ). Of all patients, 303 were women (61%) and 197 were men (39%); 434 lived in Paris and its suburbs (87%), whereas 66 (13%) lived in the rest of France. Almost all (486, 97%) were new patients; only 14 (3%) were patients who already had a consultation in the center during the previous year. Nearly all patients (480, 96%) had no suspicion of COVID-19 infection and 20 (4%) were suspected with symptoms or confirmed cases. Fifty-nine (12%) patients asked for the TC based on a general practitioner or pharmacist recommendation, and 441 (88%) had direct access. All but one patient was included for the final evaluation; that patient had an unclear medical history and symptoms, did not attend his or her physical examination and did not respond to email and phone call.
Figure 1.
Teleconsultation patients divided by age.
Past ophthalmologic medical history
Of all patients, 422 (84%) declared no serious past ophthalmologic medical history (PMH), 22 (4%) had a history of uveitis, 16 (3%) had symptoms related to contact lenses, 15 (3%) had high myopia, 11 (2%) had herpes, 6 (1%) had glaucoma, 5 (1%) had had refractive surgery and 3 (1%) had monocular blindness (Table 1 ).
Table 1.
Population characteristics.
| Total | Male | Female | P | Test | |
|---|---|---|---|---|---|
| Sex | 500 | 303 | 197 | ||
| Age | 40.6 ± 20.3 (0.6–92) | 41.5 ± 20.0 | 39.3 ± 20.8 | 0.25 | Welch |
| Age range | |||||
| < 25 | 105 (21%) | 61 (20%) | 44 (22%) | 0.59 | χ2 |
| 25–45 | 184 (37%) | 107 (35%) | 77 (39%) | – | |
| 45–65 | 151 (30%) | 98 (32%) | 53 (27%) | – | |
| > 65 | 60 (12%) | 37 (12%) | 23 (12%) | – | |
| Location | |||||
| Paris and suburbs | 434 (87%) | 264 (87%) | 170 (86%) | 0.79 | χ2 |
| Rest of France | 66 (13%) | 39 (13%) | 27 (14%) | ||
| Follow-up | |||||
| New patient | 486 (97%) | 295 (97%) | 191 (97%) | 0.79 | χ2 |
| Followed | 14 (2.8%) | 8 (2.6%) | 6 (3%) | ||
| COVID-19 | |||||
| Negative | 480 (96%) | 290 (96%) | 190 (96%) | 0.14 | χ2 |
| Positive | 20 (4%) | 13 (4.3%) | 7 (3.6%) | ||
| Second opinion | |||||
| No | 441 (88%) | 262 (86%) | 179 (91%) | 0.14 | χ2 |
| Yes | 59 (12%) | 41 (14%) | 18 (9.1%) | ||
| Past medical history | |||||
| No | 422 (84%) | 251 (83%) | 171 (87%) | 0.94 | Fisher |
| Uveitis | 22 (4.4%) | 14 (4.6%) | 8 (4.1%) | – | |
| Contact lens | 16 (3.2%) | 11 (3.6%) | 5 (2.5%) | – | |
| High myopia | 15 (3%) | 9 (3%) | 6 (3%) | – | |
| Herpes | 11 (2.2%) | 8 (2.6%) | 3 (1.5%) | – | |
| Glaucoma | 6 (1.2%) | 5 (1.7%) | 1 (0.51%) | – | |
| Refractive surgery | 5 (1%) | 3 (0.99%) | 2 (1%) | – | |
| Monophthalmic | 3 (0.6%) | 2 (0.66%) | 1 (0.51%) | – |
Suspected diagnoses
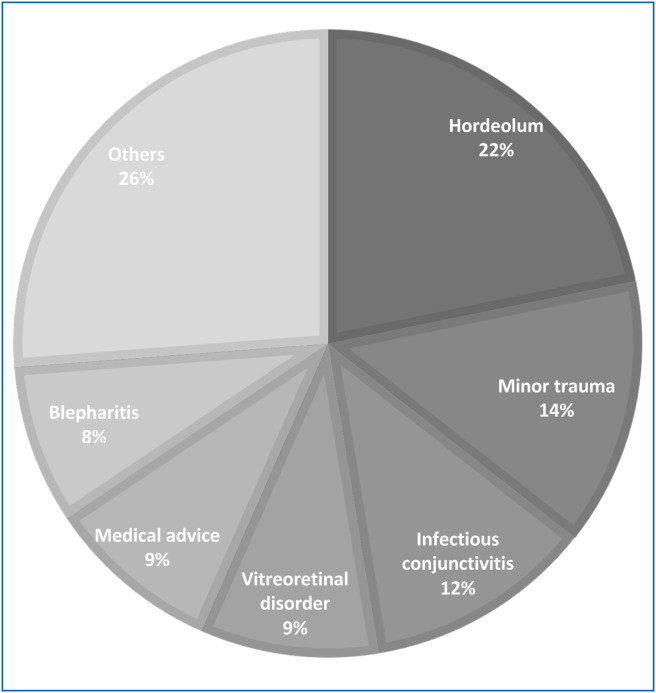
The most common reasons for consultation were simple anterior disorders (321, 64%), among them: hordeolum (109, 21.8%), minor traumas (69, 13.8%), infectious conjunctivitis (59, 11.8%). Table 2 provides additional details. Simple anterior segment disorder was the primary cause of consultation for 321 (64%) patients, followed by vitreoretinal or macular symptoms for 48 (9.6%) and then moderately (34, 6.8%) and severe (38, 7.6%) anterior disorders (Table 2 and Fig. 2 ).
Table 2.
Suspected diagnoses for teleconsultation patients.
| Diagnosis suspicion | Patients | |
|---|---|---|
| Hordeolum | 109 | 21.8% |
| Minor trauma | 69 | 13.8% |
| Infectious conjunctivitis | 59 | 11.8% |
| Vitreoretinal disorder | 46 | 9.2% |
| Medical advice | 45 | 9.0% |
| Blepharitis | 41 | 8.2% |
| Uveitis | 21 | 4.2% |
| Allergic conjunctivitis | 20 | 4.0% |
| Foreign body | 16 | 3.2% |
| Spontaneous subconjunctival hemorrhage | 15 | 3.0% |
| Corneal abscess | 10 | 2.0% |
| Varicella-zoster | 8 | 1.6% |
| Recurrent corneal erosion | 6 | 1.2% |
| Post-operative follow-up | 6 | 1.2% |
| Major trauma | 5 | 1.0% |
| Diplopia/Transient monocular blindness | 5 | 1.0% |
| Episcleritis | 4 | 0.8% |
| Pre septal cellulitis | 4 | 0.8% |
| Optic neuritis | 3 | 0.6% |
| Macular disorder | 3 | 0.6% |
| Diagnosis missing | 2 | 0.4% |
| Angle-closure | 1 | 0.2% |
| Facial Paralysis | 1 | 0.2% |
| Pterygium | 1 | 0.2% |
Figure 2.
Teleconsultation patients divided by the suspected diagnosis.
Time to consultation
All the patients could access a TC between 09:00 and 20:00 h the same day if needed. The mean time between symptom appearance and consultation was 4.12 ± 9.34 days; it varied from 3.57 ± 8.65 days in the simple anterior segment disorder group to 1.23 ± 1.48 (P < 0.01) days for moderately severe anterior segment disorder and 0.714 ± 0.756 (P < 0.01) days for the neuro-ophthalmological emergencies group (Table 3 ). Not surprisingly, analysis of the simple anterior segment disorder subgroup revealed a significantly lower time to consultation for minor traumas (0.478 ± 1.12 days) compared to hordeolum (4.47 ± 10.1 days) and infectious conjunctivitis (2.14 ± 2.37 days) (P < 0.001) (Table 4 ).
Table 3.
Details for each group of pathologies and analysis.
| Total | Simple anterior segment disorder | Mean anterior segment disorder | Severe anterior segment disorder | Neuro-ophthalmological emergency | Retinal disorder | Post-operative follow-up | Chronic follow-up advice | P | Test | |
|---|---|---|---|---|---|---|---|---|---|---|
| Patients | 500 | 321 (64%) | 34 (6.8%) | 38 (7.6%) | 8 (1.6%) | 48 (9.6%) | 6 (1.2%) | 45 (9%) | < 0.001 | Kruskal-Wallis |
| Time to teleconsultation | 4.12 (± 9.35) | 3.66 (± 8.74) | 1.53 (± 1.89) | 1.79 (± 2.30) | 0.750 (± 0.707) | 4.25 (± 7.51) | 3.83 (± 2.93) | 11.8 (± 17.1) | < 0.001 | Kruskal-Wallis |
| Physical consultation | ||||||||||
| No | 363 (73%) | 302 (94%) | 9 (26%) | 2 (5.3%) | 0 (0%) | 5 (10%) | 3 (50%) | 42 (93%) | < 0.001 | Fisher |
| Yes | 137 (27%) | 19 (5.9%) | 25 (74%) | 36 (95%) | 8 (100%) | 43 (90%) | 3 (50%) | 3 (6.7%) | ||
| Physical consultation refusal | 5 (1%) | 0 (0%) | 1 (2.9%) | 1 (2.6%) | 0 (0%) | 3 (6.2%) | 0 (0%) | 0 (0%) | – | |
| Correct diagnosis | ||||||||||
| Estimated | 467 (94%) | 316 (98%) | 28 (82%) | 27 (73%) | 7 (88%) | 38 (79%) | 6 (100%) | 45 (100%) | < 0.001 | Fisher |
| Confirmed | 120 (24.0%) | 14 (73%) | 28 (82%) | 27 (73%) | 7 (88%) | 38 (79%) | 3 (50%) | 3 (6.7%) | ||
| Diagnosis mistake | 32 (6.4%) | 5 (1.6%) | 6 (18%) | 10 (27%) | 1 (12%) | 10 (21%) | 0 (0%) | 0 (0%) | ||
| No consequences | 27 (5.0%) | 1 (0.4%) | 6 (18%) | 9 (23%) | 1 (12%) | 10 (21%) | – | – | 0.73 | Fisher |
| Care delay | 5 (1%) | 4 (1.2%) | 0 (0%) | 1 (2.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | – | – |
Table 4.
Analysis of time to consultation for the simple anterior segment disorder subgroup.
| Diagnosis | Mean (SD) | Median [IQR] | Min | Max | n | P | Test |
|---|---|---|---|---|---|---|---|
| Minor trauma | 0.478 (1.12) | 0 [0–1.00] | 0 | 7 | 69 | < 0.001 | Kruskal-Wallis |
| Hordeolum | 4.47 (10.1) | 2.00 [1.00–4.00] | 0 | 90 | 109 | – | – |
| Infectious conjunctivitis | 2.14 (2.37) | 2.00 [0–3.00] | 0 | 10 | 59 | – | – |
| Blepharitis | 10.3 (15.6) | 5.00 [3.00–10.0] | 0 | 90 | 41 | – | – |
| Allergic conjunctivitis | 4.05 (4.35) | 3.50 [2.75–4.00] | 0 | 21 | 20 | – | – |
| Others | 1.17 (1.70) | 1.00 [0–1.00] | 0 | 7 | 23 | – | – |
SD: standard deviation; IQR: interquartile range.
PCs
There were a total of 137 (27%) PCs. The practitioners estimated a consultation was required for 120 (23.0%) patients. Five (1.0%) patients declined despite the ophthalmologist's recommendation, whereas 22 (4.4%) patients called for a PC the week following TC: 19 (3.8%) had symptom evolution that differed from the specialist expectations and 3 (0.06%) did not feel comfortable with TC (Table 3).
TC predictability
Among the 137 PC, 120 were appropriate. For 17 patients, the severity of the diagnosis was overestimated. What was initially considered to be a corneal abscess, uveitis or suspected corneal foreign body were, upon physical examination, only traumatic keratitis or conjunctivitis.
Of the 363 patients initially managed only via TC, 5 retrospectively required a PC (details in the following paragraph). At this point, TC evaluation had a 96% sensitivity and 95% specificity. TC evaluation had a 87.6% positive predictive value and a 98.6% negative predictive value.
Misdiagnoses leading to a delayed consultation (TC sensitivity)
The severity of the diagnosis for 5 (1%) patients (whom we are aware of) was underestimated. These patients suffered from care delay caused by TC:
-
•
two patients were suspected to have a traumatic keratitis had a corneal foreign body; both were diagnosed 3 days later via a PC in our center after calling back;
-
•
one COVID-19-positive patient with suspected viral conjunctivitis had uveitis; the patient was diagnosed 7 days later in our center after calling back;
-
•
one patient with a corneal abscess initially refused a PC and was finally diagnosed with corneal abscess by her or his ophthalmologist;
-
•
one patient with suspicion of chronic corneal abscess on a blind eye finally had a neovascular glaucoma diagnosed by her or his ophthalmologist 2 days later.
TC limitation justifications
Among the 101 patients with available data to evaluate TC limitations, practitioners justified the consultation because the patient needed: a slit lamp examination (49%), eye fundus (25%), access to treatment (4%), optical coherence tomography (3%), visual acuity and intraocular pressure (1% each). Twenty-three per cent of the PCs were justified by a non-coherent medical history that limited the clinical orientation.
Discussion
Teleophthalmology already has multiple applications, but the use of a single mobile device in emergency has only been evaluated in war zones [10] or poor and inaccessible areas [11].
This observational monocentric study is the first to provide data on the viability of emergency teleophthalmology in a developed country during the COVID-19 lockdown. This organization permitted ophthalmologists to evaluate and select patients and organize PCs during the entire day while maintaining strict social distancing precautions. This flow regulation permitted the ophthalmologists to see 1 patient every 15 minutes in TC and 1 patient every 30 minutes at the center, as well as the ability to maintain post-emergency follow-up and secondary ophthalmologic care addressed by colleagues. The number of patients never exceeded 2 in a single waiting room. A special entrance, corridor and examination box were dedicated to COVID-19 patients to avoid nosocomial contamination.
Our cohort represents a connected, young and healthy population that mostly sought consults for non-visual, alarming disorders. 2016 emergency ophthalmology departments evaluation provide strong clinical demographic data for the three main Parisian departments (CHNO 15-20, Ophtalmopôle Cochin and Rothschild Ophthalmologic foundation) [12]. The population was 52% male and 48% female, which differed from our cohort (39% male and 61% female). The mean age of that study was 45 years, slightly older than our cohort (40.7 years), a finding that correlates with the fact that our service was Internet based. The prevalence of low BaSe SCOrE [13] pathologies (mostly simple anterior disorders and posterior vitreous detachment) seems consistent with Parisian emergency ophthalmologic demographics, with some differences in the ophthalmological conditions between the three main departments and our TC, namely: 25.4 vs. 11.8% for infectious conjunctivitis, 8.3 vs. 3.2% for foreign body, 7.3 vs. 21.8% for hordeolum, 15% vs. 13.8% for minor trauma (punctate keratitis or corneal ulcer) and 6 vs. 9.2% for posterior vitreous detachment. Those differences might have several explanations. It might be easier to show a pre-eminent eyelid problem compared to a non-painful white eye disorder during TC. The prevalence of lower corneal foreign body prevalence could be explained by the triage secretary inviting patients to have a direct PC to definitively determine the projection in the eye. The higher rate of posterior vitreous detachment could be explained by the attention of connected patients working at home on their computer to myodesopsia. The low retinal detachment rate could be explained by early prophylactic argon laser treatment and the non-inclusion of patients directly addressed in the center for vitreoretinal surgery without TC.
We did not find any available data corresponding to patients’ PMH with regard to Parisian ophthalmologic departments. However, the relatively young age of our cohort, the fact the center has existed for less than a year and the high prevalence of new patients could underlie a more limited PMH. We also did not find available data for the average time between symptom appearance and consultation. Neuro-ophthalmological emergencies received care in less than a day, foreign bodies were mostly removed the same day and most corneal abscess and uveitis had access to specialized consultation within 3 days after symptom commencement.
TC allowed the number of PCs to be reduced by 73% and regulated the number of patients in the waiting room. Only 5 (1%) patients declined a PC despite clear prior TC information, practitioner request and orientation to the nearest ophthalmologic emergency departments with a sanitary medical attestation sent to the patient. The patients’ motivations were not wanting to visit medical services during the COVID-19 outbreak and their fear of contamination; one patient underestimated her or his pathology. At this point, TC seems to be useful to confirm to patients the necessity of a PC and reassure them on the sanitary conditions in the emergency center.
TC had a 96% sensitivity, 95% specificity, 87.6% positive predictive value and 98.6 predictive negative value. Those results are consistent with Ribeiro et al. [11], who reported a 81.94% diagnosis specificity and 92.85% sensitivity between smartphone-based and slit lamp emergency diagnoses in the General Hospital of the Federal University of São Paulo. Misdiagnoses were identified in 6.4% of the population but severity was overestimated creating a useless consultation for 5% of patients and a time to consultation delay with loss of chance for 1% of the patients.
To limit patient loss to follow-up, we explained to patients the normal evolution of the pathology and provided them with direct telephone and email access to the center. These factors likely explain most of the 5.9% of physical examinations of minor anterior segment disorders. The patients who were unhappy with TC or who were addressed to colleagues were systematically contacted 5 to 7 days after the TC. Thirty-six (10%) patients from the simple anterior segment disorder group were called the week following the TC. All had good clinical evolution under treatment and did not feel the need to contact us. We expect that this precaution will reduce the number of misdiagnoses and false negatives.
Considering the potentially long time frame of the COVID-19 pandemic, with several new restriction periods and the need to maintain strict social distancing and sanitary precautions during the next few months, smartphone-based teleophthalmology is an easy and efficient solution to maintain healthcare access and limit and regulate access to ophthalmologic emergency centers. Before extending this option to other Parisian emergency centers, patient and pathology demography should be strictly compared to extrapolate the potential effect on daily use of emergency departments. One limitation could be the smaller number of patients seen daily in SOS Œil compared to the three major Parisian ophthalmic emergency departments. Smartphone or web browser solutions should also be compared to telephonic only teleophthalmology solution developed at ‘OphtalmoPôle de Cochin’ (Paris, France), to avoid technological barriers, as well as to the online triage form developed in CHNO 15-20 emergency department.
Aside from difficulties in healthcare access due to the pandemic, ophthalmological TC seems to be applicable to emergency situations only; classical consultation and chronic follow-are more dependent on refraction, tonometry, slit lamp, eye fundus examination and complementary exams. We think that after the COVID-19 pandemic, teleophthalmology in managing eye emergencies could still find applications for remote populations as well as connected populations with benign pathologies seeking instant access to medical expertise. Another interest could be to contribute regulating emergency services consultation flow.
This service requires one secretary and one doctor dedicated to TC and one practitioner for PCs. Depending on the evolution in demand, this organization could be dedicated to major emergency ophthalmology departments only.
Conclusion
This study is the first to assess the utility of emergency teleophthalmology with a simple smartphone application or web browser and a webcam to manage emergency eye care in a population with suddenly restrained access to ophthalmologists. This approach permitted us to preserve social distancing and avoid 3 on 4 PCs per patient. Overall, 27% of TCs were followed by a physical appointment. There was a mean 4.12-day delay between symptom appearance and consultation and less than 1 day for traumas, superficial corneal foreign body, and neuro-ophthalmological emergencies. With a 96% sensitivity, 95% specificity and only 1.0% misdiagnoses leading to delayed care, TC permitted satisfying healthcare access to patients with severe ophthalmological disorders while preserving social distancing and sanitary precautions. Therefore, TC may be considered a serious way to help efficiently regulate ophthalmic emergencies, especially for patients with limited access to a specialist.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Li J.-P.O., Shantha J., Wong T.Y., Wong E.Y., Mehta J., Lin H. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127:569–572. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li B., Powell A.-M., Hooper P.L., Sheidow T.G. Prospective evaluation of teleophthalmology in screening and recurrence monitoring of neovascular age-related macular degeneration: a randomized clinical trial. JAMA Ophthalmol. 2015;133:276–282. doi: 10.1001/jamaophthalmol.2014.5014. [DOI] [PubMed] [Google Scholar]
- 3.Ulrich J.N., Poudyal G., Marks S.J., Vrabec T.R., Marks B., Thapa A.B.S. Ocular telemedicine between Nepal and the USA: prevalence of vitreoretinal disease in rural Nepal. Br J Ophthalmol. 2009;93:698–699. doi: 10.1136/bjo.2008.151357. [DOI] [PubMed] [Google Scholar]
- 4.Carroll M., Cullen T., Ferguson S., Hogge N., Horton M., Kokesh J. Innovation in Indian healthcare: using health information technology to achieve health equity for American Indian and Alaska Native populations. Perspect Health Inf Manag. 2011;8:1d. [PMC free article] [PubMed] [Google Scholar]
- 5.Massin P., Chabouis A., Erginay A., Viens-Bitker C., Lecleire-Collet A., Meas T. OPHDIAT: a telemedical network screening system for diabetic retinopathy in the Île-de-France. Diabetes Metab. 2008;34:227–234. doi: 10.1016/j.diabet.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Chasan J.E., Delaune B., Maa A.Y., Lynch M.G. Effect of a teleretinal screening program on eye care use and resources. JAMA Ophthalmol. 2014;132:1045–1051. doi: 10.1001/jamaophthalmol.2014.1051. [DOI] [PubMed] [Google Scholar]
- 7.Blackwell N.A., Kelly G.J., Lenton L.M. Telemedicine ophthalmology consultation in remote Queensland. Med J Aust. 1997;167:583–586. doi: 10.5694/j.1326-5377.1997.tb138904.x. [DOI] [PubMed] [Google Scholar]
- 8.Kumar S., Yogesan K., Hudson B., Tay-Kearney M.-L., Constable I.J. Emergency eye care in rural Australia: role of Internet. Eye (Lond) 2006;20:1342–1344. doi: 10.1038/sj.eye.6702104. [DOI] [PubMed] [Google Scholar]
- 9.Bar-Sela S.M., Glovinsky Y. A feasibility study of an Internet-based telemedicine system for consultation in an ophthalmic emergency room. J Telemed Telecare. 2007;13:119–124. doi: 10.1258/135763307780677640. [DOI] [PubMed] [Google Scholar]
- 10.Mines M.J., Bower K.S., Lappan C.M., Mazzoli R.A., Poropatich R.K. The United States Army Ocular Teleconsultation program 2004 through 2009. Am J Ophthalmol. 2011;152 doi: 10.1016/j.ajo.2011.01.028. [126-132.e2] [DOI] [PubMed] [Google Scholar]
- 11.Ribeiro A.G., Rodrigues R.A.M., Guerreiro A.M., Regatieri C.V.S. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol. 2014;77:214–218. doi: 10.5935/0004-2749.20140055. [DOI] [PubMed] [Google Scholar]
- 12.Bourges P.J.-L. Elsevier Masson; 2018. Urgences en ophtalmologie: rapport SFO 2018. [Google Scholar]
- 13.Bourges J.-L., Boutron I., Monnet D., Brézin A.P. Consensus on Severity for Ocular Emergency: the BAsic SEverity Score for Common OculaR Emergencies [BaSe SCOrE] J Ophthalmol. 2015;2015:576983. doi: 10.1155/2015/576983. [DOI] [PMC free article] [PubMed] [Google Scholar]