To the Editor:
The acute respiratory disease, Coronavirus disease 2019 (COVID-19), caused by the novel Coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a worldwide pandemic affecting millions of people.1 , 2 Residents of long-term care (LTC) settings have been severely impacted by the current COVID-19 outbreak.3 Hospitalization rates in COVID-19 positive LTC residents are over 50%, and case fatality rates are over 30%.4 Limitations in effective infection control and prevention and staff members working in multiple facilities have been found to be associated with intra- and interfacility spread. COVID-19 can spread rapidly in LTC facilities, and persons with chronic underlying medical conditions are at greater risk for COVID-19-associated severe disease and death.5 Pharmacists serving LTC facilities perform a number of important activities to improve quality of medication usage, including tracking anti-infective prescribing trends and issuing prescriber recommendations and alerts.6 It is unknown how COVID-19 may be affecting anti-infective prescribing trends in LTC, as well as agents such as hydroxychloroquine sulfate.
Shortly after the first case of COVID-19 was confirmed in the United States, we assembled a cross-functional team of leaders and formed an Outbreak Preparedness and Action Committee, including our Chief Pharmacy Officer. The committee enacted a comprehensive preparedness plan as previously described.7 The infection control measures our pharmacy locations implemented were adapted from the Centers for Disease Control and Prevention. 8 , 9 In February 2020, all consultant pharmacist activities, including medication therapy management, were transitioned to remote engagement and we delivered over 130,000 recommendations to prescribers. We used 1750 contract couriers to deliver medications and took numerous additional infection control steps, including symptom and temperature screenings of employees and contractors and use of appropriate personal protective equipment. We also transitioned to a single-drop-point delivery system and used disposable paper-based delivery containers. In addition, we implemented a 7-day quarantine period for the 450,000 medications returned for credit or destruction. Our pharmacists tracked anti-infective prescription counts weekly at all facilities, as well as those for hydroxychloroquine sulfate.
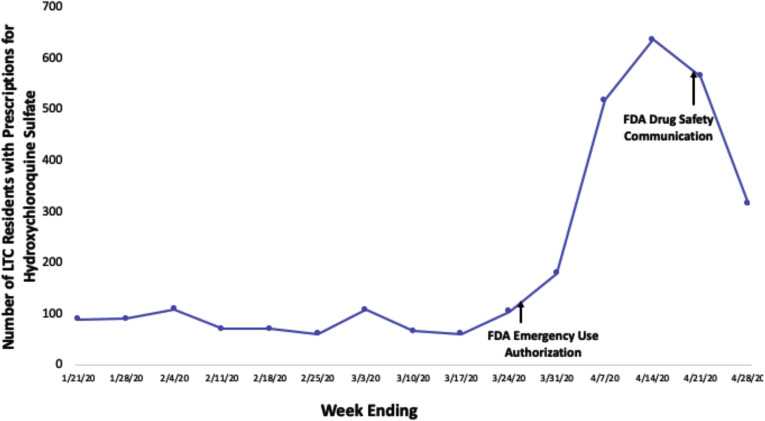
In the 100-day period between January 20, 2020 and April 30, 2020, we provided pharmacy services to 1689 nursing facilities and 488 assisted living facilities. Our pharmacists issued several special prescriber alerts to client facilities, including one on hydroxychloroquine and its potential risk for cardiac arrhythmia, and another on the potential risk associated with nebulized breathing treatments increasing aerosols generated in COVID-19 positive patients. In the 1 month following this alert, dispensing of nebulized medications decreased by 12%. Our pharmacists tracked the number of prescriptions for anti-infective agents during the study period. We observed stable levels of the number of LTC residents receiving prescriptions for antibiotics such as cephalosporins and fluoroquinolones. We observed a typical seasonal pattern in prescriptions for oseltamivir phosphate, but we noted atypical trends in prescriptions for azithromycin and hydroxychloroquine sulfate. The number of LTC residents receiving hydroxychloroquine for rheumatologic conditions in the first 60 days of the pandemic was steady, but increased over 6-fold in the 3-week period following the Food and Drug Administration's emergency use authorization. After April 24, 2020, the date that the Food and Drug Administration issued a drug safety communication on the potential risk of cardiac arrhythmias associated with use of hydroxychloroquine, we saw its use decrease by nearly 50% within 1 week (Figure 1 ).
Fig. 1.
Number of residents in 2177 LTC facilities served by 1 health services organization who received prescriptions for hydroxychloroquine sulfate between January 20 and April 30, 2020.
At least 7700 of the 44,500 LTC facilities in the United States have 1 or more confirmed cases of COVID-19.10 Because COVID-19 has spread rapidly in LTC settings, keeping cases out of homes and mitigating spread when infections occur are important priorities. LTC pharmacy can support best practices in infection control, continue pharmacist consulting using technology to enable remote work, monitor anti-infective prescribing trends, and issue prescriber alerts to provide education and support to LTC facilities during an outbreak. Careful tracking of anti-infectives and other agents, such as hydroxychloroquine, can help prescribers, facilities, and organizations such as Centers for Disease Control and Prevention study prescription trends during a pandemic. A multifaceted, pharmacist-led approach that includes monitoring affected facilities, supporting facility staff and prescribers, monitoring anti-infective prescription trends, and implementing robust infection control measures can enable support of LTC facilities and their residents during a pandemic.
Acknowledgments
The authors wish to express our most sincere gratitude to the caregivers, nurses, and administrative leadership of our country's LTC facilities, who continue to do their very best as they courageously face the COVID-19 pandemic.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zimmerman S., Sloane P.D., Katz P.R. The need to include assisted living in responding to the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21:572–575. doi: 10.1016/j.jamda.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McMichael T.M., Currie D.W., Pogosjans S. Epidemiology of COVID-19 in a long term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMichael T.M., Clark S., Pogosjans S. COVID-19 in a Long-Term Care Facility-King County, Washington, February 27-March 9, 2020. MMWR Morb Moral Wkly Rep. 2020;69:339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thiruchelvam K., Hasan S., Wong P.S. Residential Aged care medication review to improve the quality of medication use: A systematic review. J Am Med Dir Assoc. 2017;18:87.e1–87.e14. doi: 10.1016/j.jamda.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Mills W.R., Sender S., Lichtefeld J. Supporting individuals with intellectual and developmental disability during the first 100 days of the COVID-19 outbreak in the USA. J Intellectual Disabil Res. 2020;64:489–496. doi: 10.1111/jir.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Infection Control Guidance for Healthcare Professionals about Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-nCoV/hcp/infection-control.html Available at:
- 9.Key Strategies to Prepare for COVID-19 in Long-term Care Facilities. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care-strategies.html Available at:
- 10.Yourish K., Lai R., Ivory D. One-third of all US Coronavirus deaths are nursing home residents or workers. The New York Times. 2020 [Google Scholar]