Summary
Sleep health has multiple dimensions including duration, regularity, timing, and quality [1, 2, 3, 4]. The Coronavirus 2019 (COVID-19) outbreak led to Stay-at-Home orders and Social Distancing Requirements in countries throughout the world to limit the spread of COVID-19. We investigated sleep behaviors prior to and during Stay-at-Home orders in 139 university students (aged 22.2 ± 1.7 years old [±SD]) while respectively taking the same classes in-person and remotely. During Stay-at-Home, nightly time in bed devoted to sleep (TIB, a proxy for sleep duration with regard to public health recommendations [5]) increased by ∼30 min during weekdays and by ∼24 mins on weekends and regularity of sleep timing improved by ∼12 min. Sleep timing became later by ∼50 min during weekdays and ∼25 min on weekends, and thus the difference between weekend and weekday sleep timing decreased — hence reducing the amount of social jetlag [6,7]. Further, we find individual differences in the change of TIB devoted to sleep such that students with shorter TIB at baseline before the first COVID-19 cases emerged locally had larger increases in weekday and weekend TIB during Stay-at-Home. The percentage of participants that reported 7 h or more sleep per night, the minimum recommended sleep duration for adults to maintain health [5] — including immune health — increased from 84% to 92% for weekdays during Stay-at-Home versus baseline. Understanding the factors underlying such changes in sleep health behaviors could help inform public health recommendations with the goal of improving sleep health during and following the Stay-at-Home orders of the COVID-19 pandemic.
Wright et al. follow the sleeping habits of college students before and during the Covid-19 lockdown, finding that the timing of sleep changed, reducing social jetlag. In addition, the regularity of sleep increased, as did total sleep duration, suggesting life during the pandemic may suggest ways to improve sleep health.
Main Text
The COVID-19 pandemic has led to unprecedented changes in human behavior worldwide. We conducted an observational study to investigate changes in multiple dimensions of sleep health behaviors during the COVID-19 pandemic by comparing baseline sleep log data collected from January 29 to February 4, 2020 (before the COVID-19 outbreak spread across North America), to sleep log data collected in the same university students from April 22 to April 29, 2020, when the Stay-at-Home/Safer-at Home order was in effect. We used daily sleep logs to assess bedtimes and waketimes across each study week. Classes at the University of Colorado Boulder officially switched from in-person teaching to remote learning on March 16, 2020. Thirteen participants subsequently moved out of the local Mountain Time Zone (7 moved one time zone west, 5 moved one time zone east, and one moved two time zones east). Because students continued remote learning with classes scheduled according to Mountain Time, the sleep logs for all participants were analyzed according to Mountain Time. Institutional review board approval was obtained.
Outcomes included daily, weekday, and weekend TIB devoted to sleep, bedtimes, waketimes, and sleep midpoints — middle of the reported sleep opportunity — and regularity of sleep timing. Regularity was quantified by the standard deviations of bedtimes, sleep midpoint times and waketimes of each individual with lower scores indicating more regular sleep schedules. We also computed social jetlag — the difference between sleep midpoint on weekends versus weekdays [6] — and the percentage of individuals reporting ≥ 7 h sleep per night.
Three dimensions of sleep health behaviors significantly changed during Stay-at-Home (Table S1, in Supplemental Information, published with this article online): (i) TIB devoted to sleep increased on weekdays (Baseline = 7.9 ± 1.0 h, Stay-at-Home = 8.4 ± 1.1 h, p < 0.0001) and weekends (8.4 ± 1.5 h, 8.8 ± 1.2 h, p < 0.05) during Stay-at-Home (Figure 1 panel A) — in fact, TIB increased every day of the week (p < 0.05) except for Saturday (p = 0.29; see Supplemental Information), and more participants reported the recommended 7 h TIB [5] on weekdays during Stay-at-Home (92%) versus baseline (84%) (McNemar’s χ2, p < 0.001). Furthermore, participants with shorter TIB devoted to sleep at baseline, before the COVID-19 outbreak, increased their TIB more during Stay-at-Home (Figure 1B,C; weekday r = 0.51, p < 0.000001; weekend r = 0.70, p < 0.000001); (ii) Regularity of sleep timing, determined by the standard deviations of bedtime (1.2 ± 0.6 h, 1.0 ± 0.6 h, p < 0.05), sleep midpoint (1.0 ± 0.5, 0.8 ± 0.5 h), and waketime (1.2 ± 0.5 h, 1.0 ± 0.5 h, p < 0.05) improved during Stay-at-Home — this is considered a positive change in behavior as prior findings show that irregular sleep schedules are associated with poor health and performance outcomes [3,4]; (iii) Sleep timing in general was later during Stay-at-Home versus baseline (Figure 1A). Specifically, average weekly bedtime (0018h ± 1h12min, 0048h ± 1h36min, p < 0.001) and waketime (0824h ± 1h0min, 0906h ± 1h42min, p < 0.000001) as well as weekday bedtime (p < 0.001), and weekday and weekend waketimes (p < 0.01) were later during Stay-at-Home. Weekend bedtimes were not statistically different (p = 0.17). Furthermore, sleep midpoint was later for weekdays (0406h ± 1h0min, 0454h ± 1h36min, p < 0.000001), weekends (0506h ± 1h18min, 0530h ± 1h42min, p < 0.005), and for all days (p < 0.05) during Stay-at-Home (Figures 1A and S1). Generally, later sleep timing is associated with poor health outcomes [2,7]. Social jetlag was reduced during Stay-at-Home (0.9 ± 1.0h, 0.6 ± 0.9h, p < 0.01); this is considered a positive change as findings from prior research shows that larger social jetlag is associated with poor health outcomes [6,7]. Relationships between sunset and bedtime, and sunrise and waketime (Figure 1A) were similar to that previously observed [8] and, if anything, sleep duration would be expected to be longest in the winter [9]; thus, although we did not measure light exposure, it is unlikely that seasonal changes in sunset and sunrise contributed strongly to the observed changes in sleep.
Figure 1.
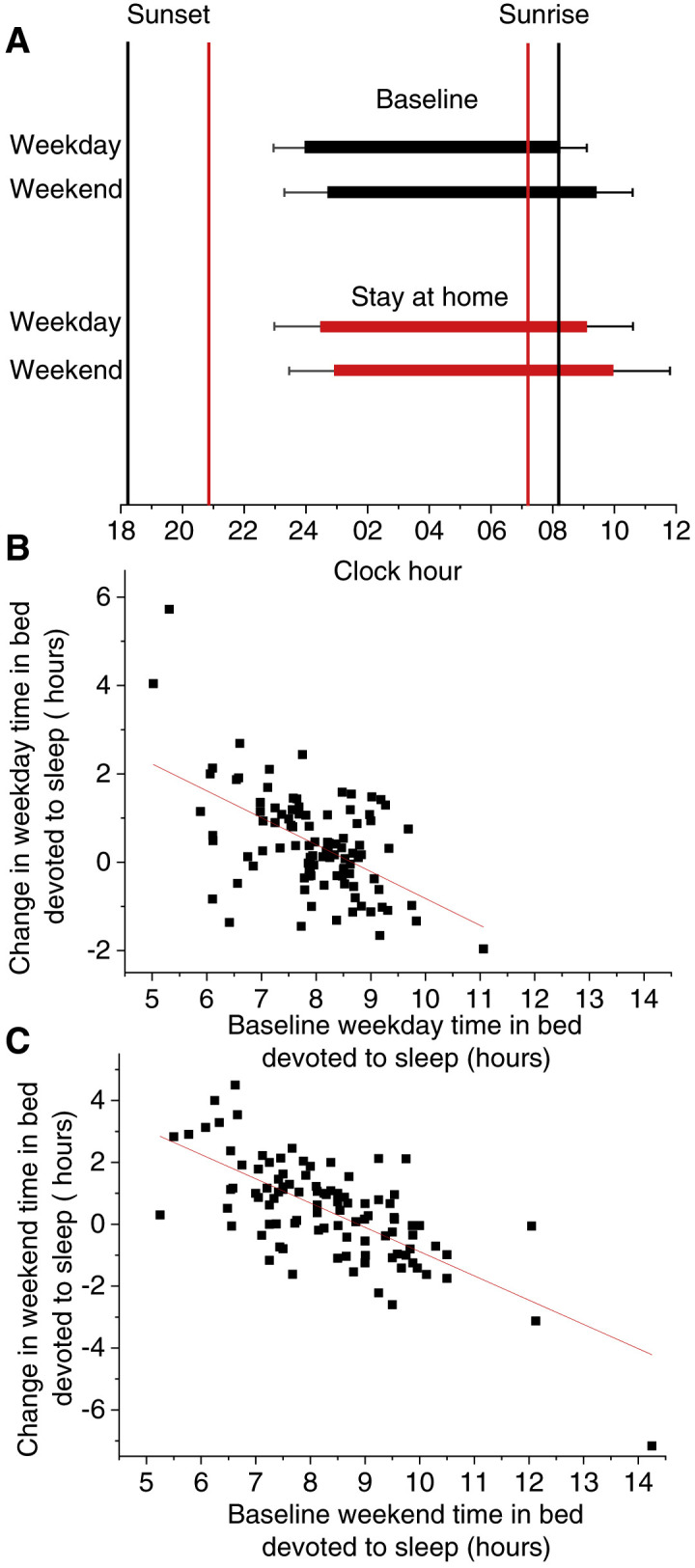
Sleep patterns prior to and during the COVID-19 pandemic and changes in time in bed devoted to sleep.
(A) Sleep times during weekdays and weekends and relationships between bedtimes and waketimes with sunset and sunrise for baseline and Stay-at-Home. (B,C) Relationship between baseline weekday and weekend time in bed devoted to sleep with the change in weekday and weekend time in bed devoted to sleep. Black bars represent reported sleep times for baseline week and red bars reported sleep times for Stay-at-Home week; black lines represent sunset and sunrise for baseline week and red lines represent sunset and sunrise for Stay-at-Home week (A). Error bars are standard deviations. Black squares show individual participant data and red lines are the best linear fit (B,C).
Insufficient sleep duration, irregular and late sleep timing, and social jetlag are common in modern society. These poor sleep health behaviors contribute to and worsen major health problems, including cardiovascular disease, obesity, diabetes, mood disorders, and immune disorders [5]. Our findings provide further evidence that these poor sleep behaviors are modifiable. Additional research using objective measures such as wearable technology validated against polysomnography and markers of circadian phase are needed to better understand our observational data, to determine if our findings apply to the general population, and to identify which factors during Stay-at-Home orders — including public health recommendations and changes in social/work constraints — contribute to changed sleep health behaviors. Further, additional research is needed to assess the impact of experimental manipulation of sleep health behaviors on daytime function, wellbeing and health outcomes.
Footnotes
Supplemental Information contains one figure, one table, and experimental procedures, all of which can be found with this article online at https://doi.org/10.1016/j.cub.2020.06.022.
Supplemental Information
References
- 1.Buysse D.J. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong L., Martinez A.J., Buysse D.J., Harvey A.G. A composite measure of sleep health predicts concurrent mental and physical health outcomes in adolescents prone to eveningness. Sleep Health. 2019;5:166–174. doi: 10.1016/j.sleh.2018.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phillips A.J.K., Clerx W.M., O’Brien C.S., Sano A., Barger L.K., Picard R.W., Lockley S.W., Klerman E.B., Czeisler C.A. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci. Rep. 2017;7:3216. doi: 10.1038/s41598-017-03171-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang T., Mariani S., Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J. Am. Coll. Cardiol. 2020;75:991–999. doi: 10.1016/j.jacc.2019.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watson N.F., Badr M.S., Belenky G., Bliwise D.L., Buxton O.M., Buysse D., Dinges D.F., Gangwisch J., Grandner M.A., Kushida C. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roenneberg T., Allebrandt K.V., Merrow M., Vetter C. Social jetlag and obesity. Curr. Biol. 2012;22:939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 7.Wong P.M., Hasler B.P., Kamarck T.W., Muldoon M.F., Manuck S.B. Social jetlag, chronotype, and cardiometabolic risk. J. Clin. Endocrinol. Metab. 2015;100:4612–4620. doi: 10.1210/jc.2015-2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stothard E.R., McHill A.W., Depner C.M., Birks B.R., Moehlman T.M., Ritchie H.K., Guzzetti J.R., Chinoy E.D., LeBourgeois M.K., Axelsson J. Circadian entrainment to the natural light-dark cycle across seasons and the weekend. Curr. Biol. 2017;27:508–513. doi: 10.1016/j.cub.2016.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de la Iglesia H.O., Fernandez-Duque E., Golombek D.A., Lanza N., Duffy J.F., Czeisler C.A., Valeggia C.R. Access to electric light is associated with shorter sleep duration in a traditionally hunter-gatherer community. J. Biol. Rhythms. 2015;30:342–350. doi: 10.1177/0748730415590702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


