Abstract
Background
The extent of the COVID-19 pandemic and the resulting response has varied globally. The European and African Hepato-Pancreato-Biliary Association (E-AHPBA), the premier representative body for practicing HPB surgeons in Europe and Africa, conducted this survey to assess the impact of COVID-19 on HPB surgery.
Methods
An online survey was disseminated to all E-AHPBA members to assess the effects of the pandemic on unit capacity, management of HPB cancers, use of COVID-19 screening and other aspects of service delivery.
Results
Overall, 145 (25%) members responded. Most units, particularly in COVID-high countries (>100,000 cases) reported insufficient critical care capacity and reduced HPB operating sessions compared to COVID-low countries. Delayed access to cancer surgery necessitated alternatives including increased neoadjuvant chemotherapy for pancreatic cancer and colorectal liver metastases, and locoregional treatments for hepatocellular carcinoma. Other aspects of service delivery including COVID-19 screening and personal protective equipment varied between units and countries.
Conclusion
This study demonstrates that the COVID-19 pandemic has had a profound adverse impact on the delivery of HPB cancer care across the continents of Europe and Africa. The findings illustrate the need for safe resumption of cancer surgery in a “new” normal world with screening of patients and staff for COVID-19.
Introduction
In December 2019, international awareness emerged of a new coronavirus that had been rapidly spreading through the Chinese city of Wuhan.1 By late February 2020, it became clear that severe outbreaks of SARS-COV-2, as the virus had been named, had resulted in almost 3000 deaths in Italy.2 By March 2020 the virus had spread to many other countries in Europe and much further globally, with over 10,000 new cases per day. On the 11th March 2020, COVID-19, the disease caused by SARS-COV-2, was declared an international pandemic by the World Health Organization, and over 80,000 new cases per day were reported by the end of April.3 As more countries began to see cases of the virus, the capacity of healthcare systems around the world began to struggle not only to cope with patients affected directly by the virus but also simultaneously to care for with those with other life-threatening conditions such as cancer.
Many urgent plans were made at hospital and national levels for the management of the virus. Intensive care units came under intense strain and needed rapid expansion to cope with increasing requirement for ventilation in severe cases. Hospital and national resources were understandably diverted towards treatment of those with the virus, reducing capacity for treatment of other serious pathologies including those that needed urgent cancer surgery. In many regions, elective surgery was cancelled. Within many hepato-pancreato-biliary (HPB) units across the world, changes to established management protocols were necessarily introduced at short notice as temporizing treatment strategies for cancers of the pancreas, liver and biliary tree, all of which normally required urgent surgical treatment.
Surgeons around the world also faced new challenges in terms of protecting themselves whilst treating patients potentially infected with COVID-19. Some centres in Italy with early experience of COVID-19 reported rates of infection of surgeons as high as 30%, causing concern regarding the importance and availability of personal protective equipment (PPE) for healthcare workers during the pandemic.4 There was also alarm at the possible consequences of perioperative COVID-19 infection, as data from Wuhan, China indicated a high mortality rate of 20% in a small cohort of patients who underwent elective surgery and were subsequently found to be COVID positive.5
The varying impact of the virus in different countries and healthcare systems raised great interest amongst surgeons for a cross-sectional look at the way HPB surgery, and in particular HPB cancer surgery, was being delivered in the face of these new challenges. This led the European and African Hepato-Pancreato-Biliary Association (E-AHPBA) to propose and devise a survey of the experience of our member HPB surgeons across the region, to allow comparisons of practice and identify opportunities for improvement and collaboration as this pandemic continues.
Methods
Questionnaire design
An online survey comprising 14 branch and stem questions (Supplementary File 1) was designed by members of the E-AHPBA Scientific and Research Committee. The survey was designed to cover demographics of individual units (yearly volume of pancreatic and liver resections and academic status) and capacity challenges (intensive care unit (ICU) expansion, occupancy by COVID-19 positive patients and reduction in operating room capacity). Questions were also asked regarding the provision of non-urgent surgery, the reasons behind cancellation of cancer surgery, staffing issues within their units and any change in management of HPB cancers during the pandemic. In addition, surgeons were asked about pre-operative COVID-19 screening and the availability of various levels of PPE across different clinical environments.
Circulation
The questionnaire was disseminated to all E-AHPBA members during the exponential phase of the outbreak, via email and also broadcast via social media avenues such as Twitter® (San Francisco, California, USA). The survey was open for a three-week period between 10th April 2020 and 30th April 2020. Regular reminders were sent out twice weekly during this period.
Categorization according to COVID prevalence
To allow comparisons between practice in countries with high and low COVID-19 prevalence, the total number of cases in each country as of the 20th April 2020 (the midpoint of the survey) was obtained from the European Centre for Disease Control website.6 An arbitrary cut-off was set at 100,000 cases, and countries that exceeded this total number of cases were labeled “COVID-high” while those below this threshold were labeled “COVID-low”.
Ethics
The NHS Health Research Authority questionnaire (http://www.hra-decisiontools.org.uk/research/; accessed 17th May 2020) was consulted to assess whether this study should be regarded as research. The NHS HRA deemed that this study was not research as the participants were not randomized to different groups, there was no change in treatment or patient care and the findings cannot be regarded as wholly generalizable.7
Statistics
Statistical comparisons between groups with non-parametric data were made using the Mann–Whitney U test via GraphPad (Version 6, 2015; GraphPad Software, San Diego, CA 92108). Significance was accepted at a P value < 0.05.
Results
Demographics
One hundred and forty-five responses (25% of the 569 total E-AHPBA membership) were obtained from surgeons across 32 countries and 130 centres (Supplementary Fig. 1). The responses covered both low and high volume units and the majority of respondents practiced in academic units (Table 1 ). The COVID-low group (<100,000 cases) consisted of 27 countries and 65 responses while the COVID-high group (>100,000 cases) consisted of 5 countries (France, Germany, Italy, Spain, and the United Kingdom) and 80 responses.
Table 1.
Details of participating centres and countries
| Number of respondents (percentages in brackets) | |
|---|---|
| Academic centres | 118 (81) |
| Pancreatic resections per centre per year | |
| 0–20 | 31 (21.4) |
| 21–50 | 46 (31.7) |
| 51–100 | 44 (30.3) |
| >100 | 24 (16.5) |
| Liver resections per centre per year | |
| 0–20 | 16 (11) |
| 21–50 | 34 (23.4) |
| 51–100 | 42 (29) |
| >100 | 53 (36.5) |
| COVID deaths in respective country at time of survey: | |
| <200 | 25 (17.2) |
| 200–5000 | 45 (31) |
| 5001–20000 | 41 (28.3) |
| >20,000 | 34 (23.4) |
| COVID cases in respective country at time of survey: | |
| <10,000 | 27 (18.6) |
| 10,000–100,000 | 38 (26.2) |
| 100,001–150,000 | 46 (31.7) |
| >150,000 | 34 (23.4) |
COVID prevalence at time of response
The total number of cases of COVID in the respective countries of the respondents to this survey varied widely, with <1000 cases nationally for around 3% (n = 5) of respondents to between 10,000 and 100,000 cases nationally for over 26% (n = 38) of respondents. 23% (n = 33) of respondents reported fewer than 1000 deaths in total in each of their countries, while the more severely affected countries (United Kingdom, France, Spain and Italy consisting of a total of 71 respondents or 49%) reported over 18,000 deaths in each country (Table 1).
Operating theatre capacity
Each unit was able to run only two operating theatre sessions per week on average for HPB surgery during the pandemic, with the majority of respondents (n = 91, 63%) reporting running less than half of their usual numbers of operating theatres. COVID-high countries were particularly badly affected, with only 6% (n = 5) of respondents operating within 75–100% of their usual capacity (Table 2 ). Of the COVID-high countries, Germany had the best-preserved operating sessional capacity at around 65% of previous levels, compared to between 30 and 45% of usual capacity across Italy, France, United Kingdom and Spain.
Table 2.
Capacity issues and COVID testing during the pandemic
| Number of respondents in each category (percentages in brackets) |
|||
|---|---|---|---|
| COVID-low n = 65 | COVID-high n = 80 | OVERALL n = 145 | |
| Percentage of normal OR activity | |||
| 0–25% | 11 (16.9) | 27 (33.8) | 38 (26.2) |
| 26–50% | 20 (30.8) | 33 (41.3) | 53 (36.6) |
| 51–75% | 8 (12.3) | 12 (15) | 20 (13.8) |
| 76–100% | 20 (30.8) | 5 (6.3) | 25 (17.2) |
| Increase in ICU capacity | |||
| None | 20 (30.8) | 5 (6.25) | 25 (17.2) |
| <50% | 19 (29.2) | 18 (22.5) | 37 (25.5) |
| 50–100% | 12 (18.5) | 22 (27.5) | 34 (23.4) |
| >100% | 14 (21.5) | 35 (43.75) | 49 (33.8) |
| ICU capacity filled with COVID + ve patients | |||
| <24% | 38 (58,5) | 13 (16.3) | 51 (35.2) |
| 25–49% | 5 (7.7) | 14 (17.5) | 19 (13.1) |
| 50–74% | 8 (12.3) | 17 (21.3) | 25 (17.2) |
| >75% | 14 (21.5) | 36 (45) | 50 (34.5) |
| Non-essential surgical procedures | |||
| Stopped | 53 (81.5) | 67 (83.8) | 120 (82.8) |
| Occasional | 8 (12.3) | 11 (13.8) | 19 (13.1) |
| Ongoing | 4 (6.2) | 2 (2.5) | 6 (4.1) |
| Pre-operative COVID testing | |||
| No | 31 (48.4) | 21 (26.6) | 52 (36.4) |
| Nasal swabs | 15 (23.4) | 29 (36.7) | 44 (30.8) |
| CT | 4 (6.3) | 2 (2.5) | 6 (4.2) |
| Nasal swabs + CT | 11 (17.2) | 21 (26.6) | 32 (22.4) |
| Nasal swabs, antibodies + CT | 3 (4.7) | 1 (1.3) | 4 (2.8) |
Non-essential surgery (e.g. elective cholecystectomy) was no longer being carried out in the units of 120 (83%) respondents (Table 2), and only performed in the units of 19 (13%) respondents for recurrent or significant symptoms, such as cholecystitis or pancreatitis.
Laparoscopic surgery during pandemic
In view of concerns that have been mentioned in the literature regarding possible aerosol dissemination of COVID-19 via laparoscopic surgery,8, 9, 10, 11 respondents were specifically asked whether laparoscopic surgery was still being undertaken in their unit. 23% (n = 33) of those who responded reported laparoscopic surgery continuing for both essential and non-essential cases, 58% (n = 82) for essential cases only and 19% (n = 27) reported a halt to laparoscopic surgery in their units during the pandemic.
Pre-operative COVID-19 testing, patient placement and PPE
Little over a third of respondents (36%) stated that pre-operative COVID-19 testing was not routinely carried out in their units; unsurprisingly this was more prevalent in COVID-low countries (Table 2). Deep nasal swabs were the commonest form of testing used, either singly or in combination with pre-operative chest CT.
COVID positive patients detected pre-operatively had their surgery cancelled by 82% (n = 116) of respondents, while 17% (n = 24) continued with surgery with appropriate precautions. Of these 17%, 15% (n = 21) of surgeons reported only proceeding after confirming availability of a post-operative intensive care bed. 88% (n = 121) of respondents reported that patients with COVID positive status were managed in a ward or intensive care environment specifically designated for COVID positive patients. 10% (n = 14) described designated COVID positive areas within wards, while 1.5% (n = 2) reported no segregated placement of COVID positive and negative patients. Unplanned intensive care beds for post-operative complications were readily available where needed in the units of 82 (59%) respondents, and available after some delay in the units of a further 43 (30%) of respondents (30 of whom were from COVID-high countries).
Respirator masks (FFP2 level and above) and eye protection were more regularly available in the operating theatre for COVID positive patients compared to when treating patients with unconfirmed COVID status in the operating theatre (Table 3 ). Only 19% (n = 28) of units had respirator masks and eye protection in wards and clinics when the COVID status of the patient was unknown.
Table 3.
Personal protective equipment (PPE) availability during the pandemic
| COVID positive, operating theatre | COVID status unknown, operating theatre | COVID positive, wards and clinics | COVID status unknown,>wards and clinics | |
|---|---|---|---|---|
| Respirator masks | 116 (80) | 57 (39.3) | 93 (64.1) | 28 (19.3) |
| Eye protection | 118 (81.4) | 88 (60.7) | 103 (71.0) | 50 (34.5) |
| Double gown | 85 (58.6) | 46 (31.7) | 59 (40.7) | 16 (11.0) |
| Double gloves | 97 (66.9) | 68 (46.9) | 65 (44.8) | 28 (19.3) |
| Surgical mask | 69 (47.6) | 99 (68.3) | 68 (46.9) | 108 (74.5) |
| Single gown/apron | 40 (27.6) | 67 (46.2) | 50 (34.5) | 66 (45.5) |
| Single gloves | 31 (21.4) | 59 (40.7) | 43 (29.7) | 86 (59.3) |
HPB cancer surgery and the management of HPB cancers during the pandemic
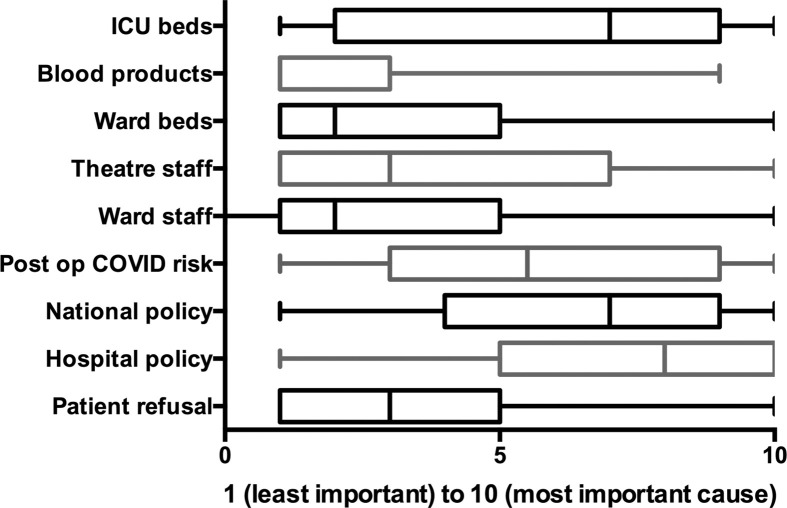
The majority of respondents reported a reduction in surgery for HPB cancers while only 10% (n = 15) of respondents reported cancer surgery proceeding unaffected in the pandemic. The most important reasons listed for cancellation of cancer surgery were lack of intensive care beds, national and hospital directives to stop non-emergency operations, and concern around patients contracting COVID-19 in the post-operative period (rated >5 on a scale of 1 = least important cause to 10 = most important cause, Fig. 1 ). ICU bed availability was a particular issue of concern in COVID-high respondents, with a median score of 8.5 compared to a score of 3 in COVID-low respondents (p < 0.0001).
Figure 1.
Median scores reflecting the grading of causes behind reduction in HPB cancer surgery during the pandemic, 1 = least important cause and 10 = most important cause
Fig. 2 shows the management options utilized by units in COVID-low and COVID-high countries for the commonest HPB cancer types during the pandemic (listed in Supplementary Table 1). Chemotherapy was frequently used for resectable pancreatic cancer during the pandemic, particularly in COVID-high countries (median score of 6 on a scale of 1–10, 1 being the least utilized and 10 being the most utilized option, compared to 3 for COVID-low countries, p = 0.016, Fig. 2a). Radiotherapy was not often used for resectable pancreatic cancer but used occasionally as an addition to chemotherapy in borderline resectable pancreatic cancer (Fig. 2b). Given the relative chemosensitivity of colorectal liver metastases, many respondents in both COVID-low and COVID-high countries ranked chemotherapy as a widely utilized treatment modality in these cases, followed by ablation particularly in COVID-high countries (Fig. 2c).
Figure 2.
Management of resectable pancreatic cancer (a), borderline resectable pancreatic cancer (b), colorectal liver metastases (c), hepatocellular carcinoma (d) and cholangiocarcinoma (e) during the pandemic
Discussion
This is the first European-African wide study of the practice of HPB surgery during the COVID-19 pandemic, covering a wide range of countries and practice volumes and including both academic and non-academic units. In addition we have been fortunate to capture a snapshot of HPB surgical practice in countries with both low and high prevalence of COVID-19 infection and mortality rates to better reflect the differences in the effect of the pandemic across these regions.
One of our main findings was the variation in capacity for HPB surgery both within and between countries. For example, across the United Kingdom, hospitals with use of local private hospital (and ICU) facilities were able to continue to perform some HPB surgery during the peak of the pandemic unlike hospitals without this option that had to halt or reduce cancer surgery. Differences were also noted between countries within the COVID-high group, with Germany having relatively high operating theatre capacity and intensive care bed availability in contrast to UK and Spain where ICU capacity was a significant cause for cancellation of cancer surgery. Reasons for these differences could not be completely elicited from the survey alone, however may be related to higher baseline intensive care unit capacity in Germany compared to other countries in Western Europe.12 , 13
Our survey showed a significant decrease in the amount of HPB cancer surgery being performed and a resultant unavoidable need to adopt non-operative treatment strategies (where possible) for pancreatic, liver and biliary cancers while the pandemic continues. This is in concordance with a recent publication estimating cancellation of 38% of all cancer surgery across all specialties globally over the peak 12 weeks of the COVID-19 crisis.14 Cancellation of HPB cancer surgery was not only related to resource limitations, but also to concerns of some surgeons and departments to schedule major complex surgery in the context of reduced resources within the hospital, given the reported high mortality rates in post-operative patients developing COVID-19 infection.5 , 15 These issues need to be balanced against the risk of inevitable disease progression in HPB cancers, which have a poor prognosis unless early surgery is performed. Indeed, guidance from the Society of Surgical Oncology (SSO) considers HPB malignancies urgent operations due to the biologically aggressive nature of these cancers.16 The risks of diversion of operable cases towards chemotherapy is not risk-free as chemotherapy-induced immunosuppression may predispose the patient towards severe COVID-19 infection while a lack of response to chemotherapy would inevitably result in progressive disease.17 , 18
Protection of healthcare workers during the pandemic has been a point of much concern globally. Full PPE (respirator masks and eye protection) was not always available in the majority of operating theatres for patients where COVID status was unknown, potentially predisposing healthcare workers to contracting COVID-19 from infected patients. The variation may relate to several factors, including the use of self-isolation periods for patients awaiting non-emergency operations, differences in COVID screening prevalence and in the definitions of risk-prone or aerosol-generating procedures and lack of sufficient PPE supplies. Regardless, the variation in PPE availability within and across countries in our survey highlights the challenges that some units are still facing in meeting the guidance regarding safe working during the COVID-19 pandemic.2 , 9 , 19 , 20 Pre-operative COVID testing, as recommended by national and specialty associations, and carried out by most units in this survey, will also play an important role in ensuring adequate safety of healthcare professionals.21 , 22 Reliable and sensitive testing protocols will additionally facilitate appropriate separation of infected and uninfected patients to minimize iatrogenic spread of the virus, and are likely to prove essential in maintaining safe perioperative care despite ongoing COVID prevalence.
There are doubtless limitations to the extent of data that can be collected in a single snapshot survey, and the conclusions that can be drawn. The response rate of 25% of the E-AHPBA membership, while reasonable for such a survey, means that the results may be affected by sampling bias. In addition, surveys are prone to discrepancies in recall accuracy, and the evolving nature of the pandemic dictates that responses in each unit and country may change with time. Furthermore, some challenges imposed by the pandemic on HPB surgery were too extensive in breadth and depth to be captured, particularly the impact on training. However our focused approach to the survey allowed us to identify the main issues facing the delivery of HPB cancer surgery during the peak of the pandemic and areas for development for the future.
Finally, the parameter used for stratification of COVID-high and COVID-low countries was the total number of cases per country at the time of the survey. We acknowledge that this does not take into account the population of each country, but instead overcomes some of the bias introduced by more comprehensive testing strategies adopted in some countries which may be more likely to detect mild cases. The parameter of cases per 100,000 population therefore would identify higher rates in some (often smaller) countries that may not be representative of an increased burden on health services.
In summary, our survey shows the extent of the impact of the COVID-19 pandemic on the breadth of HPB surgical services across the European and African regions. The worrying drop in the number of HPB cancer operations performed has meant that management of these cancers has perforce had to change, sometimes to less or non-evidence based approaches, while waiting for surgical services to resume. HPB cancer surgery clearly needs to be prioritized, and safe protocols developed for COVID-19 screening, informed consent regarding additional perioperative risks, as well as safeguarding of healthcare workers with appropriate PPE availability, to allow this to continue despite potential further COVID-19 outbreaks in the future.22 The differences in the effect of COVID-19 on HPB cancer surgery between and within COVID-low and COVID-high countries highlights the opportunities for learning and collaboration across all affected countries and allows us to suggest approaches needed to guide the safe re-establishment of HPB cancer surgery during these difficult times.
Acknowledgements
The authors would like to express their sincere gratitude to all members of the E-AHPBA who took the time to respond to the survey, and particular thanks to Carrie Hooper for her expert assistance in data collation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.hpb.2020.05.012.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None declared.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Deng X., Yang J., Wang W., Wang X., Zhou J., Chen Z. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin Infect Dis. 2020 May 15 doi: 10.1093/cid/ciaa578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Infection prevention and control and preparedness for COVID-19 in healthcare settings. https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-control-for-the-care-of-patients-with-2019-nCoV-healthcare-settings_update-31-March-2020.pdf [Internet]. [cited 2020 May 12]. Available from:
- 3.World Health Organization . World Health Organization; 2020 May 12. Statement on the COVID-19 situation in Europe.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/statements/statement-on-the-covid-19-situation-in-europe Available from: [Google Scholar]
- 4.Torzilli G., vigano L., Galvanin J., Castoro C., Quagliuolo V., Spinelli A. A snapshot of elective oncological surgery in Italy during the COVID-19 emergency. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004081. https://journals.lww.com/annalsofsurgery/Documents/A%20snapshot%20of%20Elective%20Oncological%20Surgery%20in%20Italy%20during%20COVID-19%20Emergency.pdf [Internet]. (in press). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClin Med. 2020 Apr 5;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Centre for Disease Control COVID-19 global overview. https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html [Internet]. [cited 2020 May 12]. Available from:
- 7.NHS health research authority questionnaire. http://www.hra-decisiontools.org.uk/research [Internet]. [cited 2020 May 17]. Available from:
- 8.Zheng M.H., Boni L., Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020 Mar 26 doi: 10.1097/SLA.0000000000003924. Publish Ahead of Print:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guidance for surgeons working during the pandemic. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/ [Internet]. [cited 2020 May 12]. Available from:
- 10.Tuech J.-J., Gangloff A., Di Fiore F., Michel P., Brigand C., Slim K. Strategy for the practice of digestive and oncological surgery during the Covid-19 epidemic. J Vis Surg. 2020 Mar 31 doi: 10.1016/j.jviscsurg.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chadi S., Guidolin K., Caycedo-Marulanda A., Sharkway A., Spinelli A., Fa Q. Current evidence for minimally invasive surgery during the COVID-19 pandemic and risk mitigation strategies: a narrative review. Ann Surg. 2020 doi: 10.1097/SLA.000000000000401. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wunsch H., Angus D.C., Harrison D.A., Collange O., Fowler R., Hoste E.A.J. Variation in critical care services across north America and western Europe. Crit Care Med. 2008 Oct;36:2787–2793. doi: 10.1097/CCM.0b013e318186aec8. e1–9. [DOI] [PubMed] [Google Scholar]
- 13.Rhodes A., Ferdinande P., Flaatten H., Guidet B., Metnitz P.G., Moreno R.P. The variability of critical care bed numbers in Europe. Intens Care Med Springer-Verlag. 2012 Oct;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 14.CovidSurg Collaborative. Nepogodiev D., Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 May 12 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aminian A., Safari S., Razeghian-Jahromi A., Ghorbani M., Delaney C.P. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020 Mar 26:1. doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Society of Surgical Oncology (SSO) Resource for management options of GI and HPB cancers. https://www.surgonc.org/wp-content/uploads/2020/03/GI-and-HPB-Resource-during-COVID-19-3.23.20.pdf [Internet]. Society for Surgical Oncology. [cited 2020 May 11]. Available from:
- 17.Liang W., Guan W., Chen R., Wang W., Li J., Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020 Mar;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng G., Yin M., Chen X., Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care BioMed Centr. 2020 Apr 28;24:179–183. doi: 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdelrahman T., Ansell J., Brown C., Egan R., Evans T., Ryan Harper E. Systematic review of recommended operating room practice during the COVID-19 pandemic. BJS Open. 2020 May 12:bjs5. doi: 10.1002/bjs5.50304. 50304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jessop Z.M., Dobbs T.D., Ali S.R., Combellack E., Clancy R., Ibrahim N. Personal protective equipment (PPE) for surgeons during COVID-19 pandemic: a systematic review of availability, usage, and rationing. Br J Surg. 2020 May 12 doi: 10.1002/bjs.11750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.European association for endoscopic surgery. https://eaes.eu [Internet]. [cited 2020 May 12]. Available from:
- 22.Søreide K., Hallet J., Matthews J.B., Schnitzbauer A.A., Line P.D., Lai P.B.S. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020 Apr 30;395:949. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.