Abstract
Background
The COVID-19 pandemic's impact on stroke care is two-fold — direct impact of the infection and indirect impact on non-COVID-19 diseases. Anecdotal evidence and clinical observation suggest that there is a decrease in the number of patients presenting with stroke during the pandemic. We aim to understand the impact of the COVID-19 pandemic on the utilization of stroke emergency services on a single comprehensive stroke center (CSC).
Methods
We performed a retrospective analysis of a prospectively maintained database and compared all emergency department (ED) encounters, acute stroke admissions (including TIA), and thrombectomy cases admitted in March 2017-2019 to patients admitted in March 2020 at a comprehensive stroke center.
Results
Number of total ED encounters (22%, p=0.005), acute ischemic strokes (40%, p=0.001), and TIAs (60%, p=0.163) decreased between March of 2017–2019 compared to March of 2020. The number of patients undergoing EVT in March 2020 was comparable to March 2017–2019 (p=0.430).
Conclusion
A pandemic-related stay-at-home policy reduces the utilization of stroke emergency services at a CSC. This effect appears to be more prominent for ED encounters, all stroke admissions and TIAs, and less impactful for severe strokes. Given the relatively low prevalence of COVID-19 cases in our region, this decrement is likely related to healthcare seeking behavior rather than capacity saturation.
Keywords: Stroke, Covid, Epidemiology, TIA, thrombectomy
Background
In the four-hour period before and during the final match of the 2016 UEFA European Football Championship, there was a significant decrease in emergency department admissions (OR-0.94, 95% CI-0.91–0.97).1 During the four-hour period after Portugal beat France there was a significant increase in emergency department admissions observed in France but not in Portugal.1 Widespread road closures caused by large marathons have been associated with delays in transfer of acute myocardial infarction (MI) patients, and hence have been attendant with increased 30-day mortality compared to admissions on non-marathon days.2 Furthermore, departure from routine life, voluntary or reactionary, caused by any major human event or natural calamity, leads to a ripple effect affecting access to resources and human behavior, especially healthcare seeking behavior.
Numerous similar observations related to major events have been made across various countries. Barriers to unhindered access to medical care can be either systemic or paroxysmal. Systemic factors include insurance availability, level of education and awareness, economic security, and socio-cultural matters. In contrast, paroxysmal events include immediate changes in patient behavior, temporary policy changes, physical barriers to transportation, and limitations of healthcare capacity (Table 1 ). The greater the departure from normal, the greater the impact.
Table 1.
Impact on healthcare services by major events.
| Category | Disruption Factor | Example | Metrics |
|---|---|---|---|
| Patient behavior | Interest in sports events | Euro 2016 Finals1 | Decrease in ED admissions during final match |
| Baseball/Football contests9 | Decrease in male admissions to ED | ||
| Fear and anxiety related to natural disaster or accident | Great East Japan Earthquake/Tsunami/Nuclear disaster10 | Sustained long term increase in avoidable admissions following earthquake | |
| Policy Changes | Curfew | New Orleans Curfew June 1, 199411 | Drop in pediatric EMS runs |
| Physical Barriers | Roadblock/Traffic | US Marathons2 | 4.4-minute transfer delay of MI patients; Increased mortality |
COVID-19 Pandemic and Emerging Trends
The ongoing global pandemic, caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), started in Wuhan (China) in December 2019 (COVID-19 pandemic).3 The healthcare-related impact of the COVID-19 pandemic is two-fold— direct impact of the COVID-19 infection with resultant complications ( increased inflammatory state, hypercoagulability) and indirect impact of the pandemic on non-COVID-19 diseases (systemic and paroxysmal). Anecdotal evidence, clinical observation, and informal on-line polls suggest that there is a decrease in the number of patients presenting with MI during this time.4 , 5 Similar trends have been informally discussed for stroke admissions across the world.6 Fig. 1 is a schematic of the various entities affected by the pandemic and their interaction which may potentially affect stroke care. We aim to understand the impact of the COVID-19 pandemic on the utilization of stroke emergency services on a CSC.
Fig. 1.
Interaction between various entities during the COVID-19 pandemic.
Methods
Study design
We retrospectively analyzed a prospectively maintained database of all emergency department (ED) encounters and all acute stroke admissions [including transient ischemic attacks (TIA)] in the months of March 2017, 2018, 2019, and 2020.
Patient selection
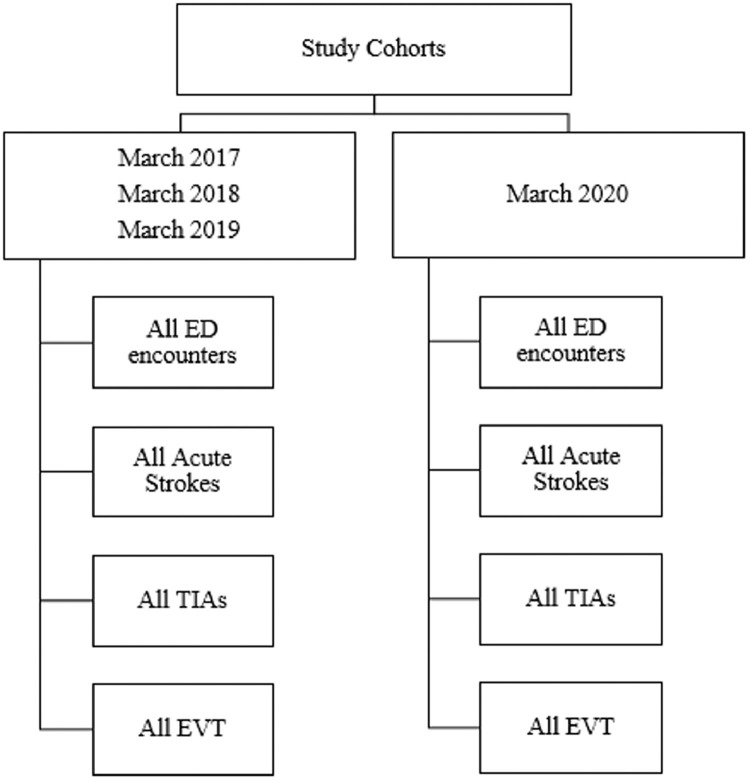
Our center is a tertiary care center in the city of Pittsburgh in Allegheny county and has over 150 critical-care beds. As of March 31, 2020, Allegheny county had a total of 325 cases of SARS-CoV-2 infection, 51 of which required hospitalization, and less than 20 required mechanical ventilation. Furthermore, Allegheny county has 314 adult ICU beds capable of mechanical ventilation.7 The month of March was chosen because the first case of COVID-19 in Pennsylvania was detected on March 6th and work-from-home and other social distancing measures were gradually escalated within the first week of that month. Additionally, no COVID patient were re-directed to other hospital in our hospital network in March 2020. The patients were then divided into the cohorts of March 2017, 2018 and 2019 versus March 2020 encounters (Fig. 2 ).
Fig. 2.
Study design flowchart.
Data collection
Four types of data elements have been reported in this study: ED encounters, acute ischemic stroke admissions, TIAs, patients receiving IV-tPA, and patients receiving endovascular thrombectomy (EVT) with or without IV-tPA. All chart review, neuroimaging, and treatment-related data adjudication were performed by a vascular neurologist.
Ethical considerations
We received institutional board approval for this study.
Statistical analysis
Data were reported as total number of admissions of ED encounters, all ischemic strokes, and thrombectomy admission. Between group comparisons (March 2017-2019 versus March 2020) were made using the one-way ANOVA test with significance level of p<0.05.
Results
Data for the month of March across four years (2017–2020) were analyzed (Table 2 and Fig. 3 )). Number of total ED encounters in March 2017, 2018, and 2019 stood at ranged from 4475, 4597, and 4565, respectively, and decreased to 3552 in March 2020 [p=0.005]. Number of all stroke admissions in the March 2017, 2018, 2019 were 163, 161, and 159, respectively, and decreased to 96 in March 2020 [p=0.001]. Number of all TIA admissions in March 2017, 2018, 2019 were 11, 18, and 16, respectively, and reduced to 6 in March 2020 [p=0.163]. The percentage decrement (comparing mean values of 2017–2019 to 2020) was statistically significant across all ED admission (22%), all stroke admissions (40%), and TIA admissions (60%). Number of patients undergoing EVT remained constant in March 2017 (18 patients), 2018 (22 patients), 2019 (17 patients), and 2020 (16 patients) [p=0.430]. Mean number of strokes receiving IV-tPA (with or without EVT) in March 2017–2019 was 10 and reduced to 7 in March 2020 (30% reduction, p=0.73). None of the patients admitted with acute stroke in March 2020 were suspicious for or tested positive for COVID-19.
Table 2.
Stroke/TIA admissions across March of 2017–2020.
| March 2017 |
March 2018 |
March 2019 |
Mean 2017-19 |
March 2020 |
P value | |
|---|---|---|---|---|---|---|
| All ED admissions | 4475 | 4597 | 4565 | 4546 | 3552 | 0.005 |
| All Acute Stroke Admission | 163 | 161 | 159 | 161 | 96 | 0.001 |
| All Transient Ischemic Attack Admissions | 11 | 18 | 16 | 15 | 6 | 0.163 |
| Strokes undergoing Endovascular Thrombectomy | 18 | 22 | 17 | 19 | 16 | 0.430 |
Fig. 3.
Stroke/TIA admissions across March of 2017–2020.
Discussion
Our study aimed to understand the impact of the COVID-19 pandemic on the utilization of stroke emergency services. We find that compared to the month of March in 2017–2019, we observed a significant decrease in the number of ED encounters (any diagnosis) and all stroke admissions in March 2020, 22% and 40%, respectively. While there was a decline in number of patients with TIA (60%) and number of patients receiving IV-tPA (30%) in March 2020, these declines were not statistically significant. In contrast, we observed comparable patients undergoing EVT in March 2020 when compared to preceding years suggesting that there was no difference in the presentation of severe strokes/large vessel occlusions. Broadly, there are two potential explanations as to why the number of stroke cases presenting to a CSC may decline: decreased utilization of emergency services by patients despite a steady rate of strokes and TIAs and/or an absolute decrease in the incidence of stroke.
Number of patients seeking care
Reduction in stroke patients seeking care at hospitals is governed by numerous factors. The stay-at-home and shelter-in-place recommendations may lead to increased social isolation, fewer potential witnesses for symptom onset and hence a reduction in the likelihood of recognizing mild stroke signs and symptoms. Anxiety and fear of contracting SARS-CoV-2 infection in healthcare environments, along with assumptions that hospitals are overwhelmed with COVID-19 patients, may lead to an increased threshold amongst certain groups of patients to seek advanced care and therefore remain at home.5 , 6 There may also be delays in seeking expert care by which time symptoms may resolve, especially TIAs. Telemedicine may not be available in at-risk communities or among the elderly without computers or cell phones.
Similar experiences have been reported in other parts of the world. A recent report from a hospital in Northern Italy, currently in phase 3 of the epidemic, describes a 90% reduction in stroke cases at their casualty department.6
Altered stroke incidence ?
While unlikely, a reduction in the actual cases of stroke/TIA may potentially explain our findings. For example, altered routine life may lead to decreased work-related stress and potentially increased medication compliance. However, the pandemic itself and associated financial insecurity may equally contribute to increased stress, anxiety and poor sleep. A stay-at-home lifestyle may compound poor dietary habits and lack of exercise. Access to refills of medications may be limited. Importantly, COVID-19 itself is a risk factor for stroke8 with approximately 31% of COVID-19 patients in the ICU having thrombotic complications.9 Additionally, COVID-19 related cytokine storm syndromes increase risk of stroke.10
Limitations
Our study is limited by its retrospective nature and a modest sample size. Lack of precise individual level data is another potential limitation.
Conclusion
The COVID-19 pandemic reduces the utilization of stroke emergency services at a CSC. This effect appears to be more prominent for ED encounters, acute ischemic stroke admissions and transient symptoms (TIA) and less impactful for severe strokes. Given the relatively low prevalence of COVID-19 cases in our geography, this decrement is likely related to healthcare seeking behavior rather than healthcare capacity saturation. Data from additional centers are necessary to validate our findings and to contrast them with centers that have a high burden of COVID-19 patients. Identifying vulnerabilities in our existing stroke systems of care could direct future modifications.
Industry sponsorship
No.
Author contributions
Conception/design: Desai, Jadhav; Acquisition of data: Desai; Analysis/interpretation of data: Desai, Jadhav; Drafting the article: Desai, Jadhav; Critically revising the article: All; Administrative/technical/material support: All; Study supervision: Jadhav.
Declaration of Competing Interest
Dr. Desai has no disclosures. Dr Guyette has no disclosures. Dr Martin-Gill has no disclosures. Dr Jadhav has no disclosures.
References
- 1.Hughes HE, Colón-González FJ, Fouillet A. The influence of a major sporting event upon emergency department attendances; a retrospective cross-national European study. PLOS ONE. 2018;13 doi: 10.1371/journal.pone.0198665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jena AB, Mann NC, Wedlund LN, Olenski A. Delays in emergency care and mortality during major U.S. marathons. N Engl J Med. 2017;376:1441–1450. doi: 10.1056/NEJMsa1614073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus Disease (COVID-19) - events as they happen. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen(accessed May 11, 2020).
- 4.Krumholz HM., M.D. The New York Times; 2020. Where have all the heart attacks gone?https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html published online April 6. [Google Scholar]
- 5.Kennedy K.Cleveland clinic says ER visits for heart attack and stroke patients are down 40% because of COVID-19 fears. https://www.cleveland19.com. https://www.cleveland19.com/2020/04/17/cleveland-clinic-says-er-visits-heart-attack-stroke-patients-are-down-because-covid-fears/ (accessed April 18, 2020).
- 6.Morelli N, Rota E, Terracciano C. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020:1–3. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hospital Preparedness Dashboard Map - Public. https://www.arcgis.com/apps/opsdashboard/index.html#/85054b06472e4208b02285b8557f24cf (accessed April 18, 2020).
- 8.Mao L, Jin H, Wang M. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klok FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehta P, McAuley DF, Brown M. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]