SUMMARY
SETTING:
Depression is a prevalent comorbidity of chronic respiratory disease (CRD), and may indicate worse clinical outcomes. The relationship between depression and living with chronic hypoxia due to CRD or residence at altitude has received little attention in resource-poor settings.
OBJECTIVE:
To investigate the association between CRD conditions and depressive symptoms in four settings in Peru.
DESIGN:
We collected data on CRD and depressive symptoms in adults aged ≥35 years. Depressive symptoms were measured according to the Center for Epidemiologic Studies Depression scale. Multivariable ordinal logistic regression was used to assess the adjusted odds of being in a higher category of depressive symptoms as a function of CRD.
RESULTS:
We analyzed data from 2953 participants (mean age 55.3 years, 49% male). The prevalence of major depressive symptoms was 19%, with significant variation according to setting. Participants with at least one CRD (OR 1.34, 95%CI 1.06–1.69) and those living at altitude (OR 1.64, 95%CI 1.10–2.43) had an increased adjusted odds of being in a higher category of depressive symptoms.
CONCLUSION:
We found a high prevalence of depressive symptoms, and a positive association between depressive symptoms with CRD and with living at altitude, both of which cause chronic hypoxia.
Keywords: depressive symptoms, chronic obstructive pulmonary disease, asthma, chronic bronchitis, mental health, chronic hypoxia, altitude
RESUME
CONTEXTE :
La dépression est une comorbidité trés fréquente des maladies respiratoires chroniques (CRD) et peut étre le témoin d’une aggravation clinique. La relation entre la dépression et le fait de vivre avec une maladie respiratoire source d’hypoxie chronique ou d’habiter en haute altitude n’a pas fait l’objet de beaucoup d’attention dans les contextes de faibles ressources.
OBJECTIF :
Etudier l’association entre CRD et symptômes dépressifs dans quatre lieux différents au Pérou.
SCHÉMA :
Nous avons recueilli des données relatives aux CRD et aux symptômes dépressifs chez des adultes âgés de ≥35 ans. Les symptômes dépressifs ont été mesurés selon l’échelle du Center for Epidemiologic Studies et catégorisés en symptômes dépressifs cliniquement significatifs ou majeurs. Une régression logistique multivariée ordinale a permis d’évaluer les risques ajustés d’être dans une catégorie plus élevée de symptômes dépressifs comme une fonction de CRD.
RÉSULTATS :
Nous avons analysé les données de 2953 participants (âge moyen 55,3 ans ; 49% d’hommes). La prévalence d’ensemble des symptômes dépressifs majeurs a été de 19% avec une variation significative en fonction du contexte. Les participants ayant au moins une CRD (OR 1,34 ; IC95% 1,06–1,69) et ceux vivant en haute altitude (OR 1,64 ; IC95% 1,10–2,43) ont eu une augmentation du risque ajusté d’étre dans une catégorie élevée de symptômes dépressifs.
CONCLUSION :
Nous avons découvert une prévalence élevée de symptômes dépressifs au Pérou et une association positive entre symptômes dépressifs et CRD et la vie en altitude, ces deux facteurs étant responsables d’hypoxie chronique.
RESUMEN
MARCO DE REFERENCIA:
La depresión es una comorbilidad frecuente de las enfermedades respiratorias crónicas (CRD) y puede conllevar peores resultados clínicos. La relación entre la depresión y vivir con hipoxia crónica ya sea a través de CRD o residir en la altura ha recibido poca atención en zonas de escasos recursos.
OBJETIVO:
Investigar la asociación entre CRD y síntomas depresivos en cuatro regiones del Perú
DISeÑo:
Recolectamos datos sobre CRD y síntomas depresivos en adultos de edad de ≥35 años. Los síntomas depresivos se midieron de acuerdo a la Escala de Depresión del Centro de Estudios Epidemiológicos. Se utilizó regresión logística ordinal para evaluar las probabilidades ajustadas de estar en una categoría más alta de síntomas depresivos en función a tener una CRD.
RESULTADOS:
Se analizaron datos de 2953 participantes (edad promedio de 55,3 años, 49% varones). La prevalencia de síntomas depresivos mayores fue del 19% con una variacióin significativa de acuerdo a la región. Participantes con al menos una CRD (OR 1,34; IC95% 1,06–1,69) y aquellos que viven en altura (OR 1,64; IC95% 1,10–2,43) tuvieron un aumento en las probabilidades ajustadas de estar en una categoría más alta de síntomas depresivos.
CONCLUSIÓN:
Se encontró una alta prevalencia de síntomas depresivos, y una asociacióin positiva entre los síntomas depresivos con CRD y vivir en la altura, ambos de los cuales causan hipoxia crónica.
THE BURDEN OF NON-COMMUNICABLE disease (NCD) in low- and middle-income countries (LMICs) continues to increase worldwide.1 Among NCDs, depression is one of the largest contributors to disability, and often co-exists with other medical conditions, causing significantly worse health out- comes.2 Past studies have found that the prevalence of depression among individuals with chronic obstructive pulmonary disease (COPD) ranges from 16% to >40%,3–6 and that COPD is associated with depression, independent of age, socio-economic status (SES), smoking, and comorbidities.7 Depression is similarly common among individuals who suffer from asthma, with prevalence ranging from 18% to 45%.8–10
Depression leads to poor health outcomes in subjects with CRD. Among those with COPD, depression has been associated with worse respiratory quality of life (QoL), worse physical health, an inability to perform activities of daily living, and significantly more COPD exacerbations than those without depression.5,11,12 Furthermore, individuals with COPD have significantly increased odds of suicidal ideation and suicide attempt.13 Individuals with asthma who have depressive symptoms have an increased risk of mortality, hospitalization, and impaired physical and mental health.9,14,15 People with current asthma also have a higher likelihood of suicidal ideation and suicide attempt.16
Residence at altitude has also been linked with increased risk of depression. Data suggest that a region’s mean elevation is significantly correlated with the percentage of people experiencing severe psychological distress and the percentage of people having at least one major episode of depression in the past year.17 Altitude has also been found to be a significant independent risk factor for suicide,18 with data from over 2500 cities showing a significantly higher number of suicide rates in higher altitude cities.19 Taken together, this information suggests that chronic hypoxia, as found in CRD or with living at altitude, may be linked to increased depressive symptoms.
Few studies have investigated the link between depression and chronic respiratory diseases in LMICs. In Peru, NCDs are responsible for >40% of total disability-adjusted life years lost, with major depressive disorders and CRDs greatly contributing to this number.20 We conducted a population-based observational study to investigate the relationship between depressive symptoms and CRD in four distinct settings in Peru with varying degrees of altitude, urbanization, SES, and air pollution exposure. We hypothesized that there would be a high prevalence of depressive symptoms in individuals with CRD in our study population.
METHODS
Study setting
We conducted a population-based study that aimed to determine the prevalence of and risk factors for cardiovascular disease and chronic pulmonary disease in four different settings in Peru, which differed by level of urbanization, altitude, and degree of ambient vs. household pollution: Pampas de San Juan de Miraflores is an urbanized community in Lima, where 60 000 primarily Andean immigrants live at sea level; Tumbes is a semi-urban northern Peruvian city with 20 000 inhabitants living at sea level in a setting with minimal vehicular traffic; Puno is a southern Peruvian city on the shores of Lake Titicaca surrounded by a number of rural villages, with a total population of about 150 000 at 3825 m above sea level; approximately 50% of Puno’s population is rural. Given the difference in urbanization and household air pollution between participants living in urban and rural Puno, Puno was divided into two different sites, urban and rural, for the purposes of our analysis.
Study participants
Individuals were eligible for the study if they were full-time residents of the city, aged ≥35 years, and if they provided informed consent. A community-wide census was conducted at each site, and we selected a random sex- and age-stratified sample of participants in each site (one per household). Study recruitment began in September 2010 and continued until about 1000 individuals in Lima and Tumbes were enrolled. In Puno, we stratified recruitment to include 500 participants each from the urban and rural settings.
Due to low literacy rates, participants provided verbal informed consent after members of the study team had read the informed consent document to them, with the ability to ask questions. Institutional review board approval was obtained from the Universidad Peruana Cayetano Heredia and A B PRISMA, in Lima, Peru, and from the Johns Hopkins Bloomberg School of Public Health in Baltimore, MD, USA.21
Data collection
Study participants responded to questions regarding their demographics, risk factors and cardiac and pulmonary disease symptoms, and their mood, as well as depressive symptoms, using a questionnaire. For those with poor literacy, fieldworkers fluent in Aymara or Quechua asked all questions verbally. Trained technicians documented objective measures, including the weight and height of each participant. Spirometry data were collected before and after the use of 200 μg of inhaled salbutamol using a spacer and the Easy-On-PC spirometer (Zurich, Switzerland) by trained technicians according to joint guidelines provided by the American Thoracic Society and the European Respiratory Society (ATS/ERS).22 A standardized grading system was adapted for quality control. Study participants who had low-quality spirometry results were asked to repeat the test on another day, for a total of three attempts. Overall 95% of tests met ATS/ERS criteria.
Outcome
The main outcome variable for our study was being in a higher category of depressive symptoms, measured according to the Spanish validated version of the Center for Epidemiologic Studies Depression (CES-D) scale, a 20-item scale, with each item scored between 0 and 3 (total possible scores range from 0 to 60).23 Scores of ≥16 are found in subjects with clinically significant depressive symptoms, and scores of ≥23 are found in those with major depressive symptoms.23 We divided the CES-D scale into three categories: scores of 0–15 (no depressive symptoms), 16–22 (clinically significant depressive symptoms), and ≥23 (major depressive symptoms). It should be noted that although the CES-D scale has been validated in Spanish, it has not been validated in either Aymara or Quechua.
Definitions
The main exposure variable for this study was having a CRD (defined as asthma, COPD, or chronic bronchitis [CB]). While the pathophysiology and epidemiology of these conditions may be different, these chronic conditions share the same clinical symptoms: shortness of breath, and increased cough and phlegm. Asthma was classified as having two of the three following self-reported conditions: physician diagnosis of asthma, current use of asthma medications, or wheezing in the last 12 months.24,25 COPD was defined in accordance to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines as the presence of airflow limitation shown by a post-bronchodilator forced expiratory volume in 1 s/forced vital capacity ratio of <70%.22 The fixed ratio was chosen for comparability with previous studies.26,27 CB was defined as self-reported phlegm production for at least 3 months a year in 2 successive years.28 We created a wealth index according to assets, household facilities, household income, and occupation.29 Hazardous drinking was defined according to the Alcohol Use Disorders Identification Test (AUDIT) questionnaire, which has been validated in Spanish.30
Biostatistical methods
The primary objective of this analysis was to study the association between being in a higher category of depressive symptoms and having CRD. The prevalence of COPD, asthma, CB, and depressive symptoms was calculated at each of the study sites. An ordinal logistic regression model was used to analyze the relationship between CRD and being in a higher category of depressive symptoms, controlling for age, sex, being obese, schooling years, SES (wealth index based on household income, assets, and household facilities), and indicator variables for study site. To estimate the association between being in a higher category of depressive symptoms and living at high altitude, we calculated the linear combination of parameters of the two sites at high altitude (urban and rural Puno) vs. sea level (Tumbes and Lima). A negative Brant test suggested that the assumption of proportionality of odds was reasonable (P = 0.65). Analyses were performed using STATA, v 12 (Stata-Corp, College Station, TX, USA) and R software (R Computing, Vienna, Austria; www.r-project.org).
RESULTS
Participant characteristics
We analyzed data from 2953 participants who had completed questionnaires, including the CES-D scale, and who had spirometry data available for the diagnosis of COPD. The average age of the study participants was 55.3 years ± 12.4 standard deviation (SD); 51% were female. The prevalence of daily smoking was 3.3% and average body mass index (BMI) was 27.8 kg/m2 ± SD 4.6. There were no differences in age (P = 0.62), sex (P = 0.41), daily smoking (P = 0.53), biomass fuel use (P = 0.73), and reported history of pulmonary tuberculosis (P = 0.30) or asthma (P = 0.28) between participants with and those without complete data.
Prevalence of depressive symptoms
We plotted the distribution of CES-D scores and found that they were highest in rural Puno and lowest in Tumbes (Figure 1). The overall prevalence of having clinically significant depressive symptoms and major depressive symptoms were respectively 19.3% and 16.7%, with important variations by age and site (Figure 2). Specifically, CES-D scores increased with age, and there was a similar prevalence of clinically significant and major depressive symptoms at each site (Figure 2). The prevalence of major depressive symptoms was highest in rural Puno, followed by urban Puno, Lima, and was lowest in Tumbes (Table 1). Participants with high CES-D scores were more likely to be women, were older in age, had a lower wealth index and lower education level, were less likely to drink heavily or smoke daily, less likely to be overweight, and were more likely to live in rural Puno. When we compared prevalence rates across settings by altitude according to degree of urbanization, we found that rural Puno had higher ratios of major depressive symptoms than Tumbes (30.8% vs. 5.7%, P < 0.001). There was a trend toward higher rates of major depressive symptoms in urban Puno compared to Lima (20.9% vs. 17.7%, P = 0.22); however, this difference was not significant.
Figure 1.
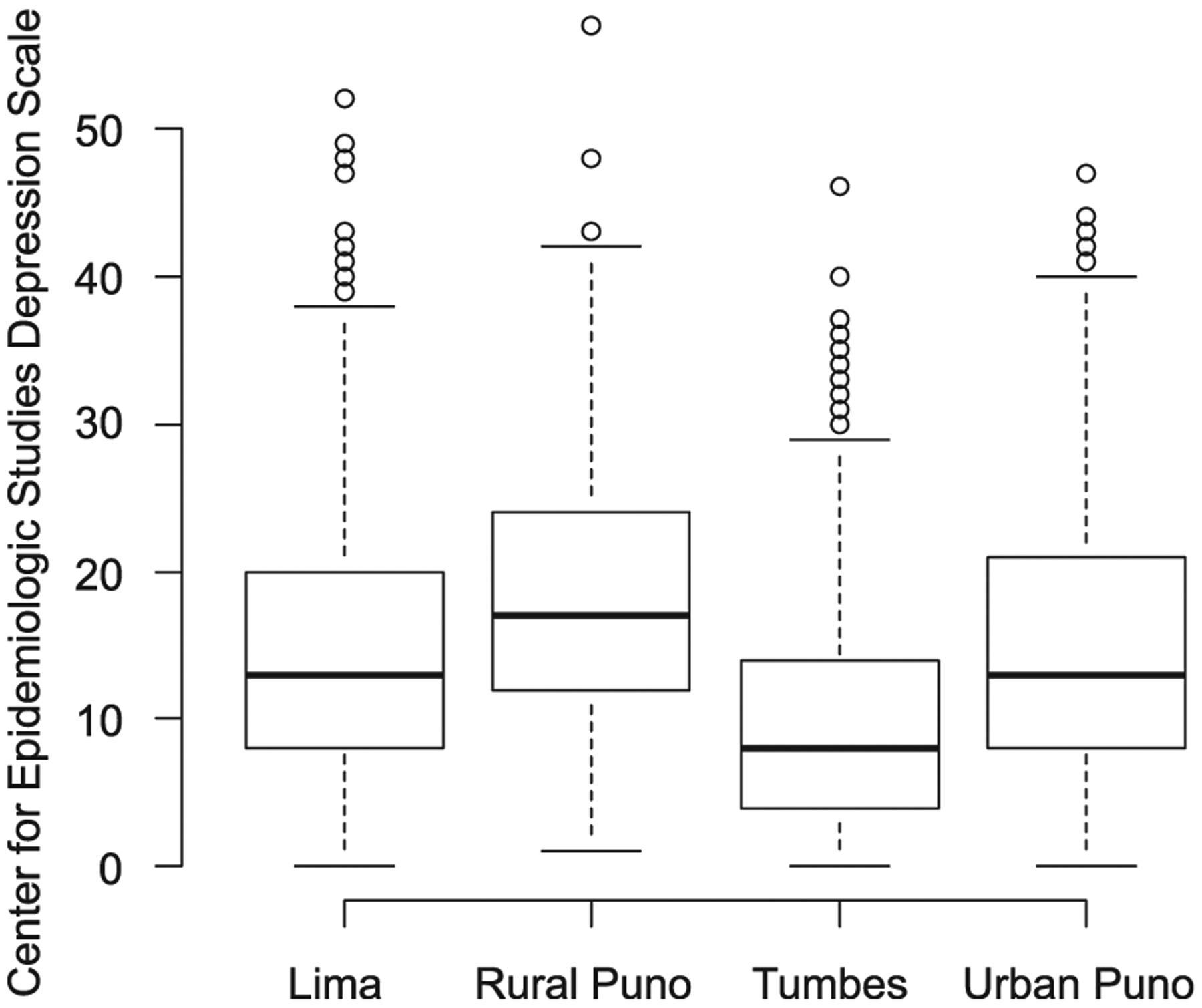
Boxplots of the Center for Epidemiology Depression Scale Score by site.
Figure 2.
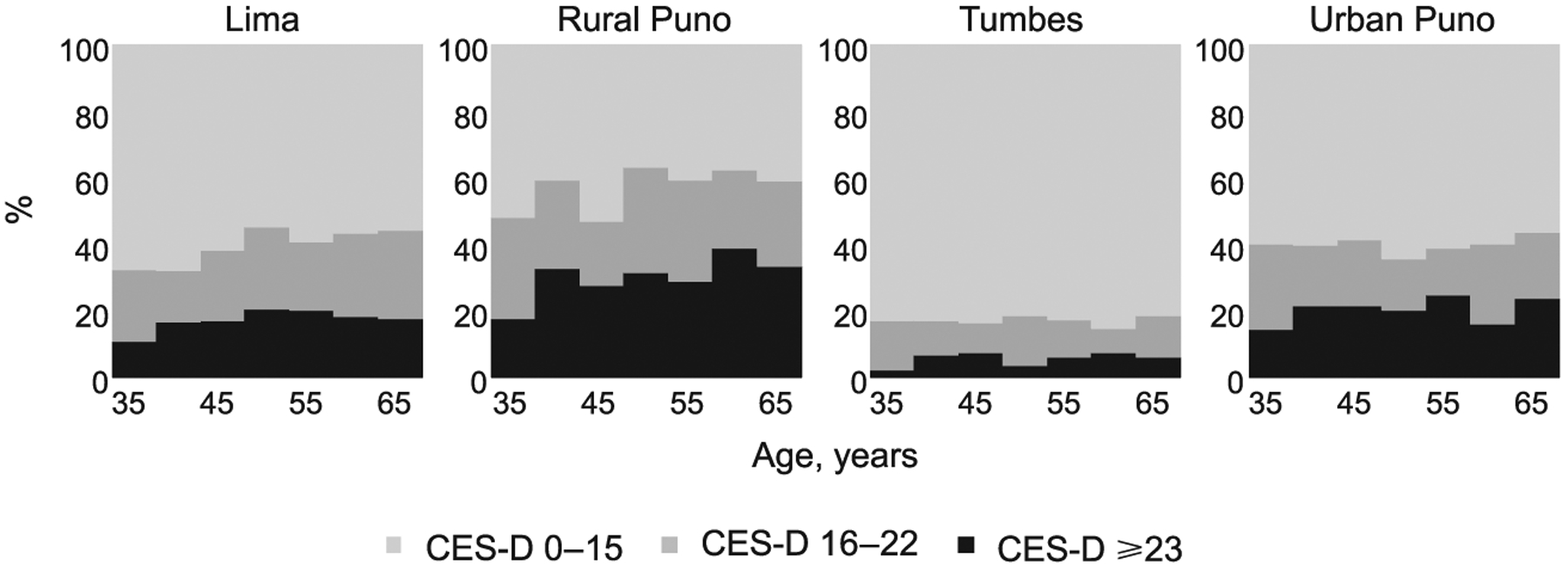
Lasagna (i.e., stacked barplot) plots of categories of depressive symptoms by age and site. CES-D = Center for Epidemiologic Studies Depression.
Table 1.
Participant characteristics by CES-D Score
| CES-D score category | ||||
|---|---|---|---|---|
| 0–15 n (%) | 16–22 n (%) | ≥723 n (%) | P value | |
| Sample size | 1890 | 571 | 492 | |
| Demographics | ||||
| Female | 783 (41.5) | 340 (59.5) | 373 (76.0) | <0.001 |
| Age, years, mean ± SD | 54.7 ± 12.3 | 56.0 ± 13.1 | 56.5 ± 12.1 | <0.01 |
| Current daily smoker | 78 (4.1) | 11 (1.9) | 8(1.6) | <0.01 |
| Hazardous drinking | 283 (15.0) | 75 (13.1) | 53 (10.8) | <0.01 |
| Education level | <0.001 | |||
| None to some grade schooling | 757 (40.0) | 291 (51.0) | 275 (56.0) | |
| Completed grade school | 669 (35.4) | 179 (31.4) | 146 (29.7) | |
| Completed high school or higher | 464 (24.6) | 100 (17.5) | 70 (14.2) | |
| BMI, kg/m2 | <0.001 | |||
| Normal (<25) | 486 (25.7) | 182 (31.9) | 165 (33.5) | |
| Overweight (25–29) | 887 (46.9) | 235 (41.4) | 189 (38.4) | |
| Obese (≥730) | 517 (27.4) | 154 (27.0) | 138 (28.0) | |
| Wealth index | <0.001 | |||
| Low | 475 (25.1) | 197 (34.5) | 230 (46.7) | |
| Medium | 669 (35.4) | 200 (35.0) | 149 (30.3) | |
| High | 746 (39.5) | 174 (30.5) | 113 (23.0) | |
| Site | <0.001 | |||
| Lima | 596 (31.5) | 225 (39.4) | 177 (36.0) | |
| Urban Puno | 299 (15.8) | 99 (17.3) | 105 (21.3) | |
| Rural Puno | 214 (11.3) | 136 (23.8) | 156 (31.7) | |
| Tumbes | 781 (41.3) | 111 (19.4) | 54(11.0) | |
| CRD | <0.001 | |||
| Any CRD | 203 (10.7) | 85 (14.9) | 85 (17.3) | |
| Asthma | 32 (1.7) | 11 (1.9) | 20 (4.1) | <0.01 |
| COPD | 102 (5.4) | 37 (6.5) | 38 (7.7) | 0.13 |
| Chronic bronchitis | 88 (4.7) | 47 (8.2) | 40 (8.1) | <0.001 |
CES-D = Center for Epidemiologic Studies Depression; SD = standard deviation; BMI = body mass index; CRD = chronic respiratory disease; COPD = chronic obstructive pulmonary disease.
Association between chronic respiratory disease, high altitude, and depressive symptoms
Overall COPD prevalence was 6.0%, followed by CB at 5.9% and asthma at 2.1%. There was significant variation in CRD by site (Table 2). Among participants with at least one CRD, 22.7% reported having clinically significant depressive symptoms and 22.8% reported having major depressive symptoms vs. 18.8% and 15.8%, respectively, among those who did not have a CRD. We present the results of single variable and multivariable ordinal logistic regression in Table 3. Participants with at least one CRD had higher adjusted odds of being in a higher category of depressive symptoms (odds ratio [OR] 1.34, 95% confidence interval [CI] 1.06–1.69) than those with none. Examined individually, the odds of being in a higher category of depressive symptoms were highest for asthma (OR 1.80), followed by CB (OR 1.31), and COPD (OR 1.29). Participants who lived at high altitude also had an increased adjusted odds of being in a higher category of depressive symptoms (OR 1.64, 95%CI 1.10–2.43).
Table 2.
CRD by setting
| Total n (%) | Lima n (%) | Urban Puno n (%) | Rural Puno n (%) | Tumbes n (%) | |
|---|---|---|---|---|---|
| Asthma | 63 (2.1) | 48 (3.8) | 6(1.2) | 0 | 9 (1.0) |
| COPD | 177 (6.0) | 62 (6.2) | 31 (6.2) | 50 (9.9) | 34 (3.6) |
| Chronic bronchitis | 174 (5.9) | 89 (8.9) | 35 (7.0) | 39 (7.7) | 12 (1.3) |
| Any CRD | 373 (12.6) | 174 (16.4) | 64 (12.7) | 83 (16.4) | 52 (5.5) |
CRD = chronic respiratory disease; COPD = chronic obstructive pulmonary disease.
Table 3.
Multivariable ordinal logistic regression of being in a higher category of depressive symptoms
| Single variable | Multivariable | |||
|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Having a chronic respiratory disease | 1.58 (1.28–1.95) | <0.001 | 1.34 (1.06–1.69) | 0.01 |
| Age group, years (reference: 35–44) | ||||
| 45–54 | 1.25 (1.02–1.54) | 0.04 | 1.22 (0.97–1.53) | 0.09 |
| 55–64 | 1.28 (1.03–1.57) | 0.02 | 1.20 (0.95–1.52) | 0.12 |
| ≥65 | 1.33 (1.08–1.65) | <0.01 | 1.12 (0.87–1.44) | 0.38 |
| Sex (reference: male) | 3.02 (2.59–3.52) | <0.001 | 3.25 (2.70–3.90) | <0.001 |
| Being obese (BMI ≥ 35 kg/m2) | 1.01 (0.85–1.19) | 0.88 | 0.93 (0.78–1.13) | 0.49 |
| Daily smoker | 0.42 (0.25–0.70) | 0.001 | 0.91 (0.53–1.56) | 0.74 |
| Education | ||||
| Completed grade school | 0.65 (0.55–0.77) | <0.001 | 0.79 (0.65–0.97) | 0.01 |
| Completed higher school or higher | 0.49 (0.40–0.59) | <0.001 | 0.60 (0.46–0.78) | <0.001 |
| Heavy drinking | 0.76 (0.62–0.95) | 0.02 | 1.33 (1.03–1.73) | 0.03 |
| Wealth index | ||||
| Middle | 2.43 (2.02–2,92) | <0.001 | 1.97 (1.55–2.50) | <0.001 |
| Higher | 1.35 (1.12–1.63) | <0.001 | 1.39 (1.13–1.71) | <0.01 |
| Site | ||||
| Rural Puno | 2.03 (1.65–2.49) | <0.001 | 1.34 (1.05–1.74) | 0.02 |
| Tumbes | 0.31 (0.25–0.38) | <0.001 | 0.24 (0.19–0.31) | <0.001 |
| Urban Puno | 1.06 (0.86–1.31) | 0.59 | 1.23 (0.96–1.56) | 0.11 |
OR = odds ratio; CI = confidence interval; BMI = body mass index.
DISCUSSION
In this multicenter, population-based study in Peru, we found that there was significant variation in the degree of depressive symptoms by setting, with the most depressed individuals living in rural Puno. Participants with CRD were more likely to have depressive symptoms after controlling for factors that could influence CRD or depressive symptoms. Finally, living at high altitude was also associated with depressive symptoms.
To our knowledge, this study is the first to investigate the association between depressive symptoms and CRD in Peru in a population-based study. Our results were similar to those reported in a recent systematic review and meta-analysis demonstrating that COPD increased the risk of developing depression, and that having depression was associated with worse COPD prognosis and outcomes.7 Feelings of depression and anxiety are common in patients with COPD, and are recog-nized as the most common COPD-related comorbidities.31,32 Common mechanisms used to explain this association include the sensation of dyspnea in triggering anxiety, and chemoreceptor hypersensi-tivity to carbon dioxide among individuals with COPD.33,34 Depression and anxiety have also been more commonly found in individuals with asthma than in those without asthma, and having depression and anxiety has been directly associated with worse asthma control.9 Our results may reflect trends in other LMICs.
In our study, we also confirmed that living at high altitude was associated with a higher prevalence of depressive symptoms independent of site differences, as previously described.17 Studies performed in animals have shown that housing female rats at altitude for 1 week can increase depression-like behavior, suggesting that altitude alone can worsen depression status, likely due to chronic hypobaric hypoxia.35 Hypoxia in rats who are housed at altitude causes alteration in frontal lobe metabolites, which is thought to exacerbate depressive behavior.36 Rats exposed to 1–2 weeks of hypobaric hypoxia also have significantly lower serotonin levels, another mechanism thought to be related to increased depressive behavior.37 Young hypothesized that the mechanism of decreased serotonin synthesis associated with hypoxia may contribute to suicide.38
Many studies have shown that individuals with CRD who also have depressive symptoms have worse overall health. There are likely several contributing factors to these poor outcomes, including systemic inflammation (there is some evidence associating tumor necrosis factor-alpha to depression and fatigue),39 psychosocial stressors such as low self-confidence leading to worse disease coping strate-gies,40 and socio-economic factors. Depression may also be a factor for decreased adherence to medical therapies and pulmonary rehabilitation,41 and can make individuals less likely to quit smoking.42 Depression contributes to increased exacerbations, functional limitations in daily activities,12 worsened QoL,11 and increased mortality.5
Given the association between depression and CRD found in our study, the critical issue of mental health needs to be further addressed. Considering how to make these changes in LMICs, however, can be challenging. Some evidence has suggested that pharmacotherapy can be helpful for those with COPD suffering from depression, although randomized controlled trials are lacking. A study of Medicare beneficiaries with COPD found that pharmacotherapy for depression was associated with reduced mortality.6 Pulmonary rehabilitation, which is a highly recommended treatment for COPD, has also been shown to reduce the likelihood of being depressed.43 In LMICs such as Peru, self-help groups focusing on face-to-face interactions may help to create a social support network and allow for psychological benefits.44 Further investigation regarding treatment options is critical, given the worse outcomes for patients with comorbid CRD and depression.
The strengths of this study include its use of a well-characterized, population-based sample in various different settings in Peru, allowing us to look at the effect of altitude on depressive symptoms. We also used validated spirometric measures of lung function to augment our definitions of respiratory disease with objective measures. The depressive symptoms scale was previously validated in Peru, but would also benefit from being validated in Aymara and Quechua. Of note, the limitations of our study include our sample size, which makes sub-analysis challenging when looking at less frequently found risk factors and outcomes, such as days hospitalized due to respiratory disease. We were also reliant on self-reporting for history of previous illness, which may have led to an underestimation, given the poor access to care of many of our study participants. As we did not have migration data for our region, we cannot speculate on the potential effects of migration on depressive symptoms. Finally, we combined all types of CRDs, as they share the same clinical manifestations, which include shortness of breath, and increased cough and phlegm; however, we were limited by sample size to adequately examine the relationship between each of the three conditions and depressive symptoms. Nonetheless, when examined individually, there was a trend for higher odds of being in a higher category of depressive symptoms and each CRD.
In conclusion, our study provides evidence of a high prevalence of depressive symptoms in Peru, and identifies both CRD and living at high altitude as potentially important risk factors. While we cannot infer the direction of the association from this study, future interventions aimed to address CRD in LMICs should also screen and treat for depression, which will lead to overall better health outcomes.
Acknowledgements
CRONICAS Cohort Study Group: A Bernabé-Ortiz, J P Casas, G D Smith, S Ebrahim, H H García, R H Gilman, L Huicho, G Málaga, J J Miranda, V M Montori, L Smeeth (cardiovascular disease); W Checkley, G B Diette, R H Gilman, L Huicho, F Leon-Velarde, M Rivera, R A Wise (chronic pulmonary disease); W Checkley, H H García, R H Gilman, J J Miranda, K Sacksteder (training and capacity building).
This project was funded in whole with federal funds from the United States National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD, USA (Contract No. HHSN268200900033C). SEZ was supported by the Department of Medicine Osler Fund for Scholarship of the Johns Hopkins School of Medicine, Baltimore, MD, USA. CHM was further supported by National Institutes of Health Fogarty International Center (5R25TW009340) and the University North Carolina Center for AIDS Research (Chapel Hill, NC, USA). WC was further supported by a Pathway to Independence Award (R00HL096955) from the National Heart, Lung and Blood Institute.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization. Global status report on non- communicable diseases. Geneva, Switzerland: WHO, 2010. http://apps.who.int/iris/bitstream/10665/44579/1/9789240686458_eng.pdf Accessed May 2016. [Google Scholar]
- 2.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370: 851–858. [DOI] [PubMed] [Google Scholar]
- 3.Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest 2008; 134 (Suppl): 43S–56S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-shair K, Dockry R, Mallia-Milanes B, Kolsum U, Singh D, Vestbo J. Depression and its relationship with poor exercise capacity, BODE index and muscle wasting in COPD. Respir Med 2009; 103: 1572–1579. [DOI] [PubMed] [Google Scholar]
- 5.Jennings JH, Digiovine B, Obeid D, Frank C. The association between depressive symptoms and acute exacerbations of COPD. Lung 2009; 187: 128–135. [DOI] [PubMed] [Google Scholar]
- 6.Qian J, Simoni-Wastila L, Rattinger GB, et al. Associations of depression diagnosis and antidepressant treatment with mortality among young and disabled Medicare beneficiaries with COPD. Gen Hosp Psychiatry 2013; 35: 612–618. [DOI] [PubMed] [Google Scholar]
- 7.Atlantis E, Fahey P, Cochrane B, Smith S. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest 2013: 144: 766–777 [DOI] [PubMed] [Google Scholar]
- 8.Mancuso CA, Peterson MG, Charlson ME. Effects of depressive symptoms on health-related quality of life in asthma patients. J Gen Intern Med 2000; 15: 301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eisner MD, Katz PP, Lactao G, Iribarren C. Impact of depressive symptoms on adult asthma outcomes. Ann Allergy Asthma Immunol 2005; 94: 566–574. [DOI] [PubMed] [Google Scholar]
- 10.Nascimento I, Nardi AE, Valenca AM, et al. Psychiatric disorders in asthmatic outpatients. Psychiatry Res 2002; 110: 73–80. [DOI] [PubMed] [Google Scholar]
- 11.Omachi TA, Katz PP, Yelin EH, et al. Depression and health- related quality of life in chronic obstructive pulmonary disease. Am J Med 2009; 122: 778.e9–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng TP, Niti M, Fones C, Yap KB, Tan WC. Comorbid association of depression and COPD: a population-based study. Respir Med 2009; 103: 895–901. [DOI] [PubMed] [Google Scholar]
- 13.Goodwin RD Is COPD associated with suicide behavior? J Psychiatry Res 2011: 45: 1269–1271. [DOI] [PubMed] [Google Scholar]
- 14.Ford ES, Mannino DM, Homa DM, et al. Self-reported asthma and health-related quality of life: findings from the behavioral risk factor surveillance system. Chest 2003; 123: 119–127. [DOI] [PubMed] [Google Scholar]
- 15.Walters P, Schofield P, Howard L, Ashworth M, Tylee A. The relationship between asthma and depression in primary care patients: a historical cohort and nested case control study. PLOS ONE 2011; 6: e20750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goodwin RD, Demmer RT, Galea S, et al. Asthma and suicide behaviors: results from the Third National Health and Nutrition Examination Survey. J Psychiatry Res 2012: 46: 1002–1007. [DOI] [PubMed] [Google Scholar]
- 17.DelMastro K, Hellem T, Kim N, Kondo D, Sung YH, Renshaw PF. Incidence of major depressive episode correlates with elevation of substate region of residence. J Affect Disord 2011; 129: 376–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim N, Mickelson JB, Brenner BE, Haws CA, Yurgelun-Todd DA, Renshaw PF. Altitude, gun ownership, rural areas, and suicide. Am J Psychiatry 2011: 168: 49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brenner B, Cheng D, Clark S, Camargo CA Jr. Positive association between altitude and suicide in 2584 US counties. High Alt Med Biol 2011; 12: 31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute of Health Metrics and Evaluation. Global burden of disease profile: Peru. Seattle, WA, USA: IHME, 2016. http://www.healthdata.org/peru Accessed May 2016. [Google Scholar]
- 21.Miranda JJ, Bernabe-Ortiz A, Smeeth L, Gilman RH, Checkley W; CRONICAS Cohort Study Group. Addressing geographical variation in the progression of non-communicable diseases in Peru: the CRONICAS cohort study protocol. BMJ Open 2012; 2: e000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. [DOI] [PubMed] [Google Scholar]
- 23.Ruiz-Grosso P, Loret de Mola C, Vega-Dienstmaier JM, et al. Validation of the Spanish Center for Epidemiological Studies Depression and Zung Self-Rating Depression Scales: a comparative validation study. PLOS ONE 2012; 7: e45413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lodrup Carlsen KC, Haland G, Devulapalli CS, et al. Asthma in every fifth child in Oslo, Norway: a 10-year follow up of a birth cohort study. Allergy 2006; 61: 454–460. [DOI] [PubMed] [Google Scholar]
- 25.Haland G, Carlsen KC, Sandvik L, et al. Reduced lung function at birth and the risk of asthma at 10 years of age. N Engl J Med 2006; 355: 1682–1689. [DOI] [PubMed] [Google Scholar]
- 26.Menezes AM, Perez-Padilla R, Jardim JR, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet 2005; 366: 1875–1881. [DOI] [PubMed] [Google Scholar]
- 27.Jaganath D, Miranda JJ, Gilman RH, et al. Prevalence of chronic obstructive pulmonary disease and variation in risk factors across four geographically diverse resource-limited settings in Peru. Respir Res 2015; 16: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Oca MM, Halbert RJ, Lopez MV, et al. The chronic bronchitis phenotype in subjects with and without COPD: the PLATINO study. Eur Respir J 2012; 40: 28–36. [DOI] [PubMed] [Google Scholar]
- 29.Howe LD, Galobardes B, Matijasevich A, et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol 2012; 41: 871–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alvarado ME, Garmendia ML, Acuna G, Santis R, Arteaga O. [Assessment of the alcohol use disorders identification test (AUDIT) to detect problem drinkers]. Rev Med Chil 2009; 137: 1463–1468. [Spanish] [PubMed] [Google Scholar]
- 31.Hill K, Geist R, Goldstein RS, Lacasse Y. Anxiety and depression in end stage COPD. Eur Respir J 2008: 31: 667–677. [DOI] [PubMed] [Google Scholar]
- 32.Janssen DJ, Spruit MA, Leue C, et al. ; Ciro Network. Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chron Respir Dis 2010: 7: 147–157. [DOI] [PubMed] [Google Scholar]
- 33.Bailey PH The dyspnea-anxiety-dyspnea cycle—COPD patients’ stories of breathlessness: ‘It’s scary when you can’t breathe.’ Qual Health Res 2004: 760–778. [DOI] [PubMed] [Google Scholar]
- 34.Smoller JW, Pollack MH, Otto MW, Rosenbaum JF, Kradin RL. Panic anxiety, dyspnea, and respiratory disease: theoretical and clinical considerations. Am J Respir Crit Car Med 1996: 154: 6–17. [DOI] [PubMed] [Google Scholar]
- 35.Kanekar S, Bogdanova OV, Olson PR, Sung YH, D’Anci KE, Renshaw PF. Hypobaric hypoxia induces depression-like behavior in female Sprague-Dawley rats, but not males. High Alt Med Biol 2015: 16: 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bogdanova O, Abdullah O, Kanekar S, Bogdanov V, Prescot A, Renshaw P. Neurochemical alterations in frontal cortex of the rat after a week of hypobaric hypoxia. Behav Brain Res 2014: 263: 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ray K, Dutta A, Panjwani U, Thakur L, Anand JP, Kumar S. Hypobaric hypoxia modulates brain biogenic amines and disturbs sleep architecture. Neurochem Int 2011: 58: 112–118. [DOI] [PubMed] [Google Scholar]
- 38.Young SN Elevated incidence of suicide in people living at altitude, smokers and patients with chronic obstructive pulmonary disease and asthma: possible role of hypoxia causing decreased serotonin synthesis. J Psychiatry Neurosci 2013; 38: 423–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-shair K, Kolsum U, Dockry R, Morris J, Singh D, Vestbo J. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir Res 2011; 12: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Gen Psychiatry 2010; 25: 1209–1221. [DOI] [PubMed] [Google Scholar]
- 41.Fan VS, Giardino ND, Blough DK, Kaplan RM, Ramsey SD; Nett Research Group. Costs of pulmonary rehabilitation and predictors of adherence in the National Emphysema Treatment Trial. COPD 2008; 5: 105–116. [DOI] [PubMed] [Google Scholar]
- 42.Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA 1990; 264: 1546–1549. [PubMed] [Google Scholar]
- 43.Coventry PA, Bower P, Keyworth C, et al. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLOS ONE 2013; 8: e60532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cafarella PA, Effing TW, Usmani ZA, Frith PA. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology 2012; 17: 627–638. [DOI] [PubMed] [Google Scholar]


