Abstract
Objective
To examine temporal trends in incidence of Rolandic epilepsy (RE), prevalence of comorbidities and antiepileptic drug (AED) prescribing patterns.
Design
Retrospective cohort study.
Setting
The UK.
Patients
Children aged 0–16 years born 1994–2012 were followed from birth until September 2017, transfer to another general practitioner practice or death or practice withdrawal from The Health Improvement Network (THIN), whichever occurred first.
Main outcome measures
Incidence of RE, prevalence of comorbidity and AED prescribing patterns. Read codes for comorbidities and AEDs were adapted from other UK population-based epilepsy studies.
Results
There were 379 children with first RE event recorded between 2000 and 2014 from active THIN practices with available mid-year population counts. Crude annual incidence across all years was 5.31/100 000 (95% CI 4.81 to 5.88). There was no significant time trend in adjusted incidence rate ratios (aIRR) (0.99/year, 95% CI 0.96 to 1.02). Males had higher aIRR (1.48, 95% CI 1.20 to 1.82) as did children aged 6–8 and 9–11 years compared with 4–5 years (aIRR 2.43, 95% CI 1.73 to 3.40; aIRR 2.77, 95% CI 1.97 to 3.90, respectively). There was recorded comorbidity in 12% with 6% with a recorded diagnosis of pervasive developmental disorder. Half of children with RE had a record of being prescribed AEDs.
Conclusions
UK incidence of RE has remained stable with crude incidence of 5/100 000/year. Carers and clinicians need to be aware that comorbidities may exist, particularly pervasive developmental disorders. Carbamazepine is consistently the most commonly prescribed AED for RE in the UK.
Keywords: epidemiology, general paediatrics, neurology, neurodevelopment
What is already known on this topic?
Annual incidence of Rolandic epilepsy (RE) in a Swedish hospital-based study in 1974 was 21/100 000 and 5/100 000 in an Icelandic population-based study in the 1990s.
Attention deficit hyperactivity disorder has been reported in 31% of children with RE, cognitive problems in 22% and behavioural problems including pervasive developmental disorder in 12%.
There is debate whether drug treatment should be given; in the UK, carbamazepine and lamotrigine are recommended first-line, and sulthiame or valproate in other countries.
What this study adds?
The incidence of RE in the UK has remained virtually unchanged since 2000; crude incidence in 2014 was 5/100 000/year and age, gender-adjusted incidence was 3.2/100 000/year.
Population-based data confirmation that comorbidities occur in a proportion of children with RE; 12% were coded with any co-existing disorder and 6% with pervasive developmental disorder.
Half of children with RE were prescribed anti-epileptic drugs with carbamazepine and valproate remaining the most frequently prescribed over the study period.
Introduction
Information on frequency, cause and natural history of Rolandic epilepsy (RE) is necessary to develop optimal treatment strategies. There are few published studies on the incidence of RE.1–4
Several factors influence incidence of epilepsy including socioeconomic status, gender, ethnicity, adaptation of regional or international guidelines in classification and management of epilepsy, availability of experts in epilepsy.5–7 As the presence and distribution of such factors can vary between countries, country-specific data on incidence of RE are most appropriate for resource allocation. Furthermore, country-specific incidence would best inform feasibility of recruitment targets for research studies. There are no contemporary UK studies on incidence of RE.
A retrospective, chart review, hospital-based study of 196 children with RE found high prevalence of comorbid cognitive and behavioural problems. Attention deficit hyperactivity disorder (ADHD) was found in 31%, 22% had specific cognitive problems and 11.7% had behavioural problems including anxiety, depression and pervasive developmental disorder (PDD).8 Other hospital-based studies have reported a higher prevalence of cognitive problems in RE compared with control data.9 10 A case-control study of 89 children with RE found they had higher anxiety and depression scores to controls.11 Hospital-based studies compared with population-based studies are more likely to produce biassed results. There are no population-based studies on comorbidities in RE.
There has been a long-standing view RE does not need treatment with antiepileptic drugs (AEDs).12 13 However, recent data suggesting positive treatment effects on cognitive and/or behavioural comorbidities14 15 may influence whether to treat RE with AEDs. The potential negative cognitive and/or behavioural effects of AEDs are well recognised, with newer AEDs theoretically having fewer effects.16 In the UK, for children who are given treatment, carbamazepine and lamotrigine are the recommended first-line AEDs. In Germany, Austria and Israel, it is sulthiame and in France it is valproate. The scientific evidence for these recommended AEDs is poor.17 Although there has been a UK survey on current treatment approaches,17 it is unclear whether prescribing patterns of AEDs in RE has changed over time. Given lack of evidence of optimum treatment of RE, well-designed trials, with realistic recruitment targets based on contemporary country-specific incidence estimates, are needed.
The aims of this study were to investigate temporal trends in incidence of RE, prevalence of comorbidities and AED prescribing patterns in the UK.
Methods
We carried out a retrospective cohort study using The Health Improvement Network (THIN), a large UK-wide clinical database that prospectively captures Vision software electronic health record (EHR) data on prescriptions, diagnoses and symptoms in patients presenting to their general practitioner (GP).18 19 THIN has been used to carry out a number of population-based studies.5 18 Ninety eight per cent of the UK population are registered with a GP who provides primary care services, refers patients for secondary care and shares care of patients seen in secondary care. In THIN, prescription data are automatically recorded each time a GP issues a prescription and coded using the UK Prescription Pricing Authority and classified according to the British National Formulary.18 Significant medical events are recorded by GPs and coded using the Read system. Data on contact with secondary care are entered from referrals and discharge letters. Demographic data on age, gender and postcode derived Townsend scores of socioeconomic status are also usually available.18 19
As of January 2016, THIN contained pseudonymised primary care EHR from over 15 million patients, of whom over 3.4 million are currently registered, representing almost 6% of the UK population, and is broadly representative of the UK in age, gender and social deprivation.19 Data are available from 1990 onwards, with summarised medical information detailed prior to that. Childhood epilepsy diagnoses as a whole, rather than specific subtypes, in THIN have been previously validated.5
GP practice turnover is inevitable as some practices merge, or close, or switch to another software. Practices can also decline to continue contributing data to THIN. Within that structure, we had no scope to handle missing data or losses to follow-up. THIN practices are regularly assessed to ensure EHRs are of suitably high quality for research.18 19
Children aged 0–16 years born during 1994–2012 with a RE diagnosis (Read code F25y400) prior to September 2017 were included in the full cohort. Full EHR for all children qualifying for RE were available to the researchers. All participants were registered at (or within 6 months of) birth at one of the more than 550 THIN practices. All children were followed from birth until September 2017, transfer to another practice or death or withdrawal of the practice contributing data to THIN; whichever occurred first. Within the full cohort, we intended to examine a subcohort of children aged between 4 and 16 years in the period 2000–2017 who were epilepsy-free at entry into the subcohort, to estimate the annual incidence of RE. However, there was a substantial increase in withdrawn/merged GP practices from 2015 onwards (online supplemental table 1). We therefore restricted analysis of annual incidence up to December 2014. The age range was chosen to cover the lower age RE usually starts, and upper age at which most would be seizure free.20
archdischild-2019-318212supp001.pdf (553.2KB, pdf)
Codes used for identification of comorbidities and AEDs were adapted from population-based epilepsy studies2 5 21 22 and are provided as online supplemental material (online supplemental tables 2 and 3).
Statistical analysis
We summarised over time number of practices contributing mid-year population counts and returning data satisfying THIN quality criteria. Mid-year population counts were summarised across practices.
For denominators, we examined number of children in every THIN practice irrespective of whether they identified cases of RE (ie, the base population) at the midpoint of each study year, broken down by: (i) age group in years 4–5; 6–8; 9–11; 12–14, 15–16 years; (ii) gender; (iii) GP practice, (iv) quintiles of Townsend scores of socioeconomic deprivation. Townsend scores were not updated since 2011, and 7% of contributing practices did not contribute Townsend data. Also, data provided at the practice level were a mean of individual participants’ quartile Townsend score which lacks interpretability and is much less sensitive to differences between practices. Therefore, we were unable to adjust for socioeconomic status.
Gender and age at onset of RE were summarised descriptively, as was presence of comorbidities. The proportion and 95% CIs of children with a record of any AED prescription after RE diagnosis were summarised over time.
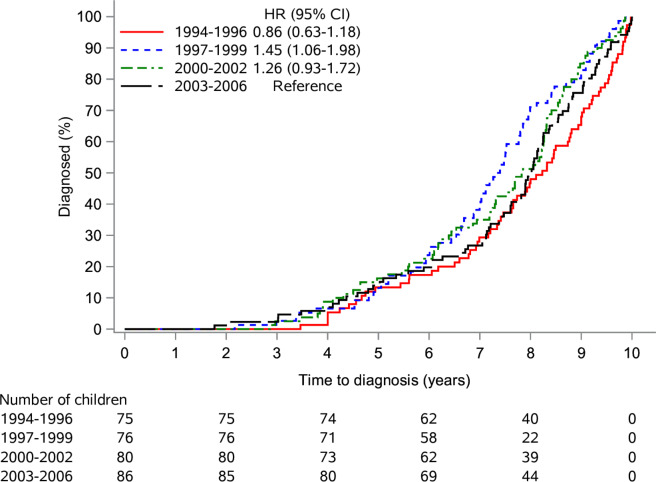
Among the full cohort of children with RE who had at least 10 years of follow-up from birth, the cumulative distribution of time to diagnosis of RE was estimated using Kaplan-Meier (KM) curves. We defined time to diagnosis as time from birth until first occurrence of RE diagnosis in GP records. Cumulative incidence of RE diagnosis by age 5 years and age 8years and 95% CIs were calculated. KM curves were plotted for four birth groups: 1994–1996, 1997–1999, 2000–2002 and 2003–2006. To investigate changes over time in age of diagnosis, HR for each birth group (against the 2003–2006 reference group) and its 95% CIs were estimated from a Cox proportional hazards model. Significance of temporal changes was assessed by log-rank test for trend.
Crude incidence rates per 100 000 were summarised by year and age group. The number of children with a RE Read code was analysed using mixed effects Poisson regression including an offset for mid-year population. The model included potential confounders such as year, gender and age group as fixed effects and practice as a random effect. Year was modelled as categorical (3-year groups) or continuous variable: the continuous version was centred on year 2000 and scaled if necessary. A linear year effect, cubic B-spline and categorical representation were compared using Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) to determine which best modelled the relationship between year and incidence. Adjusted incidence rate and 95% CIs were calculated for each year adjusting for age, gender, year and GP practice. Adjusted incidence rate ratios (aIRR) and 95% CIs for model variables were calculated. As a sensitivity analysis, requirement to extend the model to a negative binomial or zero-inflated Poisson regression was investigated by comparing values of AIC and BIC across models. All hypothesis tests were performed using a two-sided 5% significance level. Analyses were carried out using SAS V.9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Online supplemental table 1 summarises mid-year population counts over time for practices. Withdrawn practices after 2014 were similar sized to those which stayed in THIN, but most withdrawals were in England (online supplemental table 4). Representation of contributing ages of children by year is provided in online supplemental table 5.
There were 516 children with RE identified in the full cohort. Of those, 379 who had a first RE diagnosis recorded between 2000 and 2014 and were from practices with available mid-year population counts were included as our final incidence analyses subcohort sample (online supplemental table 6). From the full cohort, the 317 children with at least 10-year follow-up were used to assess cumulative distribution of time to RE diagnosis (online supplemental table 6 and figure 1).
Figure 1.
Kaplan-Meier plot of time to first Rolandic epilepsy (RE) diagnosis by year of birth for children with a diagnosis of RE and at least 10 years of follow-up from birth.
Table 1 summarises age at diagnosis and gender, overall and by nation of residence for the incidence sample of 379, and for the full cohort of 516 children. Age of RE diagnosis was similar across UK regions (mean age of 9 years).
Table 1.
Age at diagnosis and gender, overall and by nation of residence for the incidence sample of 379, and for the full cohort of 516 children.
| All | England | Scotland | Northern Ireland | Wales | |
| Full cohort | |||||
| Number | 516 | 365 | 83 | 22 | 46 |
| Gender | |||||
| Male | 325 (63%) | 222 (61%) | 61 (73%) | * | 27 (59%) |
| Female | 191 (37%) | 143 (39%) | 22 (27%) | * | 19 (41%) |
| Age at onset (years) | |||||
| Mean (SD) | 8.6 (2.7) | 8.5 (2.7) | 8.4 (2.8) | 9.7 (2.8) | 9.3 (3.2) |
| Min, Max | 2, 18 | 2, 16 | 3, 14 | 3, 15 | 4, 18 |
| Incidence sample | |||||
| Number | 379 | 304 | 38 | 11 | 26 |
| Gender | |||||
| Male | 232 (61%) | 180 (59%) | 28 (74%) | * | 15 (58%) |
| Female | 147 (39%) | 124 (41%) | 10 (26%) | * | 11 (42%) |
| Age at onset (years) | |||||
| Mean (SD) | 9.0 (2.5) | 8.9 (2.4) | 9.1 (2.7) | 10.3 (2.4) | 9.6 (2.9) |
| Min, Max | 4, 16 | 4, 16 | 5, 14 | 7, 15 | 5, 16 |
Data are n, n (%), mean (SD) or min, max, where n is the number of children with Rolandic epilepsy (overall, and by nation).
*Not presented due to disclosure of small numbers.
Figure 1 illustrates time to RE diagnosis by year of birth, with no significant evolution in time to diagnosis (p=0.51). The proportion of children with RE diagnosed by 5 years was 14.2% (95% CI 10.2% to 18.5%) and by 8 years was 55% (95% CI 49.5% to 60.4%).
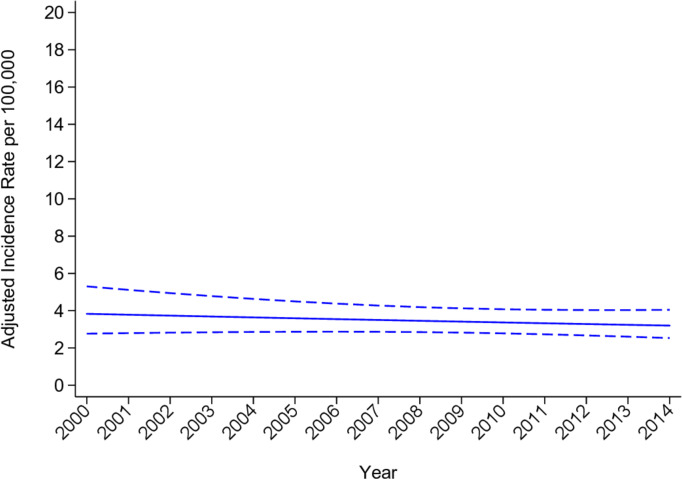
Crude incidence rate over the study period was 5.31/100 000/year (95% CI 4.81 to 5.88). Crude incidence rate by age group and year are provided in table 2A. In the Poisson regression model, a linear representation of year was clearly most appropriate, with lowest BIC (linear 4515; spline 4523; categorical 4540). Age-adjusted and gender-adjusted incidence in 2014 was 3.20/100 000/ year (95% CI 2.53 to 4.05). table 2B summarises aIRRs. Males showed significantly greater incidence (aIRR 1.48, 95% CI 1.20 to 1.82) as did children aged 6–8 and 9–11 years compared with aged 4–5 years reference group (6–8: aIRR 2.43 (95% CI 1.73 to 3.40); 9–11: aIRR 2.77 (95% CI 1.97 to 3.90)). There was no significant time trend in aIRR (p=0.38); Figure 2 illustrates point estimate and 95% CI for adjusted incidence rate by year. Sensitivity analysis confirmed suitability of the Poisson regression model (AIC 4451; BIC 4515) compared with negative binomial (AIC 4450; BIC 4523) and zero-inflated Poisson (AIC 4454; BIC 4583).
Table 2.
Crude incidence rate of children with Rolandic epilepsy per 100,000 with 95% confidence intervals by age group and year, and adjusted incidence rate ratios (aIRR) with 95% confidence intervals.
| A: Crude incidence rate of children with Rolandic epilepsy per 100 000 with 95% CIs by age group and year | |||||
| Year | Age in years | ||||
| 4–5 | 6–8 | 9–11 | 12–14 | 15–16 | |
| 2000–2002 | 2.5 (1.1 to 6.1) | 4.9 (2.6 to 9.1) | |||
| 2003–2005 | 4.6 (2.6 to 8.1) | 7.6 (5.3 to 10.8) | 9.9 (6.8 to 14.4) | ||
| 2006–2008 | 3.1 (1.6 to 6.0) | 6.9 (4.8 to 9.8) | 8.4 (6.1 to 11.4) | 3.2 (1.7 to 5.9) | |
| 2009–2011 | 3.1 (1.7 to 5.7) | 9.8 (7.3 to 13.0) | 8.3 (6.1 to 11.3) | 3.3 (2.1 to 5.4) | 1.5 (0.6 to 3.9) |
| 2012–2014 | 1.9 (0.9 to 3.9) | 6.1 (4.3 to 8.6) | 6.9 (4.9 to 9.8) | 2.7 (1.6 to 4.7) | 0.6 (0.2 to 2.4) |
| B. Adjusted incidence rate ratios (aIRR) and 95% CI | ||
| aIRR (95% CI) | P value | |
| Year | 0.99 (0.96 to 1.02) | 0.380 |
| Age group (years) | ||
| 4–5 | Ref | <0.0001 |
| 6–8 | 2.43 (1.73 to 3.40) | |
| 9–11 | 2.77 (1.97 to 3.90) | |
| 12–14 | 1.06 (0.69 to 1.64) | |
| 15–16 | 0.34 (0.14 to 0.80) | |
| Sex | ||
| Female | Ref | 0.0002 |
| Male | 1.48 (1.20 to 1.82) | |
Estimates are from a Poisson model including fixed effects of year, gender and age group, and a random practice effect and an offset term for mid-year population estimates.
Figure 2.
Adjusted incidence rate per 100 000 and 95% CI of year for Rolandic epilepsy in children over years 2000–2014.
Table 3 provides data on comorbidities. Among the 379 incidence RE children, 12% had a record of any co-existing disorder and 6% had a pervasive developmental disorder. Half of children with RE were recorded as being prescribed AEDs; there was a higher proportion among those aged 6–11 years with prescriptions in more recent years (online supplemental figure 1). The most frequent AEDs were carbamazepine (34%), sodium valproate (16%), lamotrigine (7%) and levetiracetam (5%). Over the study period, carbamazepine and valproate remained most frequently prescribed.
Table 3.
Record of a co-existing disorder in children with Rolandic epilepsy in the incidence sample (n=379)
| N (%) | |
| Any co-existing disorder | 46 (12%) |
| Behavioural/emotional/social functioning/mental health | <10* |
| Developmental (unspecified) | 31 (8%) |
| Motor function/hyperkinetic/tic | 13 (3%) |
| Pervasive developmental | 21 (6%) |
| School problems | 11 (3%) |
| Speech and language | <10 (-%) |
*Not presented due to disclosure of small numbers.
Discussion
The main findings of this population-based study are1: incidence of RE in the UK remained virtually unchanged over the study period with a crude rate in 2014 of 5/100 000/year (similar to the 1990s Icelandic studies) and a higher incidence among males and greatest incidence in children aged 6–11 years2; confirmation of the presence of comorbidities in RE, with a higher proportion of pervasive developmental disorders than reported in the general population3; ‘older’ type medications, in particular carbamazepine, are consistently preferred prescribed AEDs.
While there are studies that have examined temporal trend of childhood epilepsy as a whole (and show a decreasing incidence),5 23 we are not aware of any other studies that have examined temporal trends of other specific benign childhood epilepsy syndromes. Our contemporary incidence rate of RE in the UK and factors that influence rate are similar to those reported in an Icelandic population-based study in 1998 that identified 38 children3 but lower than the 21/100 000/year in a hospital-based Swedish study in 1975.1 All three have similar sociodemographic composition and ready access to paediatricians with expertise in epilepsy so difference in country-specific rates are likely to related to study design. With a crude incidence rate of 5.31/100 000/year, applied to the 10 217 388 UK population of children aged 4–16 years (https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland), we estimate 542 new RE cases annually in the UK. This is higher than the 340 new RE cases estimated in 2012 by the UK-wide Epilepsy12 audit,1 24 but lower than the 751 estimated by a 2014 cross-sectional survey of UK paediatricians with clinical responsibility for epilepsy.17 Discrepancy between our estimate and these two other UK studies may be related to differences in the study designs, low rate of syndromic diagnoses by reporting clinicians in Epilepsy12 audit, or multiple counts of patients who had shared care between a paediatrician and a tertiary paediatric neurologist in the cross-section survey. There is no financial incentive for UK GP practices to be more exacting in coding for epilepsy syndrome/type and it is possible that we missed RE cases recorded under another non-specific epilepsy code. However, equally there is no reason to believe that GPs would systematically not be more specific in coding having received confirmation of a specific epilepsy syndrome from hospital specialists. Given identification of copy number variants at Xp22.31 as a risk factor for RE, we hypothesise higher incidence in males may be related to an X linked recessive genetic pre-disposition.4
RE was often previously referred to as benign RE as the seizures were often age-limited and were easily controlled. Our results provide further evidence that RE is more than seizures.14 25–27 Consideration should be given to monitoring carefully for co-existing cognitive and/or behavioural problems particularly pervasive developmental disorders. Concerns that such comorbidities may not be well recorded in practices would suggest that our results are underestimates and true additional burden is more substantial.
Our finding that half of children with RE were prescribed AEDs by GPs is similar to the 60% of paediatricians who reported treatment in a recent cross-sectional survey.17 While the survey showed that carbamazepine was the preferred AED at one time-point, our study shows that it has consistently been the preferred AED over time. The lack of prescribing ‘newer’ AEDs (such as lamotrigine and levetiracetam) more often used after failure of ‘older’ AEDs (such as carbamazepine), probably reflects the natural history of seizures that are readily controlled. Given now recognised physical, cognitive and behavioural adverse effects in offspring,28 29 there are now UK-wide guidelines that restrict the use of valproate in females of potential childbearing age.28 At first glance it may seem surprising that valproate was the second most commonly prescribed AED, however these guidelines postdate our study period. Futures studies may see valproate being prescribed much less in girls and an increase in alternatives of which lamotrigine and levetiracetam appear preferred.
Limitations
THIN is representative of the UK population but care outside the GP setting is not fully captured. Studies using routine administrative datasets like THIN provide an opportunity to provide population-based data on research topics, obtain insight on real-life patient management and address clinically relevant questions more quickly and at lower cost than other study types. However, there may be data that are systematically missing and this limitation needs to be borne in mind.
The risk of misdiagnosis of epilepsy is well known.30 We were unable to achieve the ideal of carrying out a direct validation of RE and comorbidities diagnoses and our results need to be considered in this context. However, medical diagnoses in THIN have high validity31–33 and high validity of epilepsy diagnoses, as whole rather than specific subtypes, in THIN has been previously reported. The high validity of diagnosis codes in THIN is likely related to the close relationship between THIN GP practices and hospital services. Although diagnosis of RE (as well as comorbidities) were extracted from GP records, the coded diagnoses are very likely to reflect clinical assessments by GPs as well as hospital specialists. RE has been a well-known epilepsy syndrome for decades with a well-established specific GP Read code. These factors, plus our finding of a stable incidence rate over time which is similar to that previously reported in another Western European country, plus not dissimilar estimated annual new RE cases compared with a national UK epilepsy audit and a UK cross-sectional study of RE17 24 give confidence that RE diagnoses were true cases. THIN coding for other childhood epilepsy syndromes may not be the same as for RE. We postulate representability of THIN as a source of scientific research of specific childhood epilepsy syndromes will be related to how familiar THIN database GPs are with individual syndromes and/or the availability of syndrome-specific Read codes. It can be debated that our observation of prescribing practices would be more accurately reflected as GPs frequently aid in long-term prescription of AEDs. While it is possible that variation in coding over time and/or by GP practice could have impacted on our findings, any impact would probably have been minimal; had there been substantial variation, marked stepped changes would have been (and were not) observed.
Conclusions
The contemporary UK incidence of RE is 5/100 000/year and has remained virtually unchanged between 1997 and 2014; males and children aged 6–11 years have highest incidence. Carers and clinicians need to be aware that comorbidities may exist, particularly pervasive developmental disorders. Carbamazepine is consistently the most commonly prescribed AED for RE in the UK. Designing potential UK clinical trials for RE should take these study findings into consideration. Finally, prospective studies with comprehensive enrolment of all epilepsy cases and detailed review by epileptologists could be useful to confirm our study findings.
Footnotes
Contributors: RFMC conceptualised the study. All authors designed the study. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: The study was funded by the Waterloo Foundation. CJW was supported in this work by NHS Lothian via the Edinburgh Clinical Trials Unit.
Disclaimer: The funders had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the article for publication.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Epidemiological research using THIN data has ethical approval from the South East Multi-Centre Research Ethics Committee (Protocol Number 03/01/073). Additional study-specific approval was obtained from the THIN scientific review committee. Since additional information was not being sought from patients or carers, neither Multi-Centre Research Ethics Committee nor local Research and Development approval were needed.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party.
References
- 1. Heijbel J, Blom S, Bergfors PG. Benign epilepsy of children with centrotemporal EEG foci. A study of incidence rate in outpatient care. Epilepsia 1975;16:657–64. 10.1111/j.1528-1157.1975.tb04748.x [DOI] [PubMed] [Google Scholar]
- 2. Aaberg KM, Gunnes N, Bakken IJ, et al. Incidence and prevalence of childhood epilepsy: a nationwide cohort study. Pediatrics 2017;139:e20163908 10.1542/peds.2016-3908 [DOI] [PubMed] [Google Scholar]
- 3. Astradsson A, Olafsson E, Ludvigsson P, et al. Rolandic epilepsy: an incidence study in Iceland. Epilepsia 1998;39:884–6. 10.1111/j.1528-1157.1998.tb01185.x [DOI] [PubMed] [Google Scholar]
- 4. Addis L, Sproviero W, Thomas SV, et al. Identification of new risk factors for rolandic epilepsy: CNV at Xp22.31 and alterations at cholinergic synapses. J Med Genet 2018;55:607–16. 10.1136/jmedgenet-2018-105319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meeraus WH, Petersen I, Chin RF, et al. Childhood epilepsy recorded in primary care in the UK. Arch Dis Child 2013;98:195–202. 10.1136/archdischild-2012-302237 [DOI] [PubMed] [Google Scholar]
- 6. Ngugi AK, Kariuki SM, Bottomley C, et al. Incidence of epilepsy: a systematic review and meta-analysis. Neurology 2011;77:1005–12. 10.1212/WNL.0b013e31822cfc90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pickrell WO, Lacey AS, Bodger OG, et al. Epilepsy and deprivation, a data linkage study. Epilepsia 2015;56:585–91. 10.1111/epi.12942 [DOI] [PubMed] [Google Scholar]
- 8. Tovia E, Goldberg-Stern H, Ben Zeev B, et al. The prevalence of atypical presentations and comorbidities of benign childhood epilepsy with centrotemporal spikes. Epilepsia 2011;52:1483–8. 10.1111/j.1528-1167.2011.03136.x [DOI] [PubMed] [Google Scholar]
- 9. Danielsson J, Petermann F. Cognitive deficits in children with benign rolandic epilepsy of childhood or rolandic discharges: a study of children between 4 and 7 years of age with and without seizures compared with healthy controls. Epilepsy Behav 2009;16:646–51. 10.1016/j.yebeh.2009.08.012 [DOI] [PubMed] [Google Scholar]
- 10. Gobbi G, Boni A, Filippini M. The spectrum of idiopathic rolandic epilepsy syndromes and idiopathic occipital epilepsies: from the benign to the disabling. Epilepsia 2006;47:62–6. 10.1111/j.1528-1167.2006.00693.x [DOI] [PubMed] [Google Scholar]
- 11. Liu X, Han Q. Depression and anxiety in children with benign childhood epilepsy with centrotemporal spikes (BCECTS). BMC Pediatr 2016;16:128 10.1186/s12887-016-0670-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ambrosetto G, Tassinari CA. Antiepileptic drug treatment of benign childhood epilepsy with rolandic spikes: is it necessary? Epilepsia 1990;31:802–5. 10.1111/j.1528-1157.1990.tb05522.x [DOI] [PubMed] [Google Scholar]
- 13. Peters JM, Camfield CS, Camfield PR. Population study of benign rolandic epilepsy:: is treatment needed? Neurology 2001;57:537–9. 10.1212/WNL.57.3.537 [DOI] [PubMed] [Google Scholar]
- 14. Tacke M, Gerstl L, Heinen F, et al. Effect of anticonvulsive treatment on neuropsychological performance in children with BECTS. Eur J Paediatr Neurol 2016;20:874–9. 10.1016/j.ejpn.2016.07.015 [DOI] [PubMed] [Google Scholar]
- 15. Xiao F, An D, Lei D, et al. Real-Time effects of centrotemporal spikes on cognition in rolandic epilepsy. Neurology 2016;86:544–51. 10.1212/WNL.0000000000002358 [DOI] [PubMed] [Google Scholar]
- 16. Moavero R, Santarone ME, Galasso C, et al. Cognitive and behavioral effects of new antiepileptic drugs in pediatric epilepsy. Brain Dev 2017;39:464–9. 10.1016/j.braindev.2017.01.006 [DOI] [PubMed] [Google Scholar]
- 17. Mellish LC, Dunkley C, Ferrie CD, et al. Antiepileptic drug treatment of rolandic epilepsy and Panayiotopoulos syndrome: clinical practice survey and clinical trial feasibility. Arch Dis Child 2015;100:62–7. 10.1136/archdischild-2013-304211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. CSD E. Thin data from EPIC—A guide for researchers February 2009.
- 19. Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Jhi 2004;12:171–7. 10.14236/jhi.v12i3.124 [DOI] [PubMed] [Google Scholar]
- 20. Wirrell EC. Benign epilepsy of childhood with centrotemporal spikes. Epilepsia 1998;39:S32–41. 10.1111/j.1528-1157.1998.tb05123.x [DOI] [PubMed] [Google Scholar]
- 21. Aaberg KM, Bakken IJ, Lossius MI, et al. Comorbidity and childhood epilepsy: a nationwide registry study. Pediatrics 2016;138:e20160921 10.1542/peds.2016-0921 [DOI] [PubMed] [Google Scholar]
- 22. Myland M, Buysse B, Tsong W, et al. Seizure frequency, healthcare resource utilisation and mortality in childhood epilepsy: a retrospective cohort study using the thin database. Arch Dis Child 2019;104:1070–6. 10.1136/archdischild-2019-316910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sillanpää M, Lastunen S, Helenius H, et al. Regional differences and secular trends in the incidence of epilepsy in Finland: a nationwide 23-year registry study. Epilepsia 2011;52:1857–67. 10.1111/j.1528-1167.2011.03186.x [DOI] [PubMed] [Google Scholar]
- 24. CD Epilepsy 12 – United Kingdom collaborative clinical audit of health care for children and young people with suspected epileptic seizures (preliminary results). Royal College of Paediatrics and Child Health 2012;97:A98. [Google Scholar]
- 25. Vannest J, Tenney JR, Gelineau-Morel R, et al. Cognitive and behavioral outcomes in benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 2015;45:85–91. 10.1016/j.yebeh.2015.01.041 [DOI] [PubMed] [Google Scholar]
- 26. Giordani B, Caveney AF, Laughrin D, et al. Cognition and behavior in children with benign epilepsy with centrotemporal spikes (BECTS). Epilepsy Res 2006;70:89–94. 10.1016/j.eplepsyres.2006.02.005 [DOI] [PubMed] [Google Scholar]
- 27. Miziara CSMG, de Manreza MLG, Mansur L, et al. Impact of benign childhood epilepsy with centrotemporal spikes (BECTS) on school performance. Seizure 2012;21:87–91. 10.1016/j.seizure.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 28. Bromley R, Weston J, Adab N, et al. Treatment for epilepsy in pregnancy: neurodevelopmental outcomes in the child. Cochrane Database Syst Rev 2014:CD010236 10.1002/14651858.CD010236.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Meador KJ, Baker GA, Browning N, et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol 2013;12:244–52. 10.1016/S1474-4422(12)70323-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Helen Cross J, Cross JH. Pitfalls in the diagnosis and differential diagnosis of epilepsy. Paediatr Child Health 2009;19:199–202. 10.1016/j.paed.2009.02.003 [DOI] [Google Scholar]
- 31. Lo Re V, Haynes K, Forde KA, et al. Validity of the health improvement network (thin) for epidemiologic studies of hepatitis C virus infection. Pharmacoepidemiol Drug Saf 2009;18:807–14. 10.1002/pds.1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Keenan HT, Hall GC, Marshall SW. Early head injury and attention deficit hyperactivity disorder: retrospective cohort study. BMJ 2008;337:a1984 10.1136/bmj.a1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lewis JD, Schinnar R, Bilker WB, et al. Validation studies of the health improvement network (thin) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf 2007;16:393–401. 10.1002/pds.1335 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2019-318212supp001.pdf (553.2KB, pdf)