Abstract
Background:
Long-term maintenance of sports participation is important for young men undergoing anterior cruciate ligament (ACL) reconstruction. Identifying biomechanical characteristics in patients who achieve this goal can assist in elaborating rehabilitation programs and in identifying successful recovery, but this has rarely been investigated.
Purpose:
To test the association between maintenance of sports participation at 5 to 10 years after ACL reconstruction and measures of force production and landing biomechanics in men.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 30 men who underwent isolated ACL reconstruction were examined. At 5- to 10-year follow-up, associations were tested between reported outcomes of sports maintenance and objective biomechanical measures. The biomechanical tests included isokinetic knee torque and lower limb kinetics and kinematics during landing tasks. Measurements for each limb were conducted separately, and side-to-side symmetry indices (SI) were calculated. Subgroups included SI greater than +10% (ie, extreme positive), SI lower than –10% (ie, extreme negative), and SI between –10% and +10% (ie, symmetric).
Results:
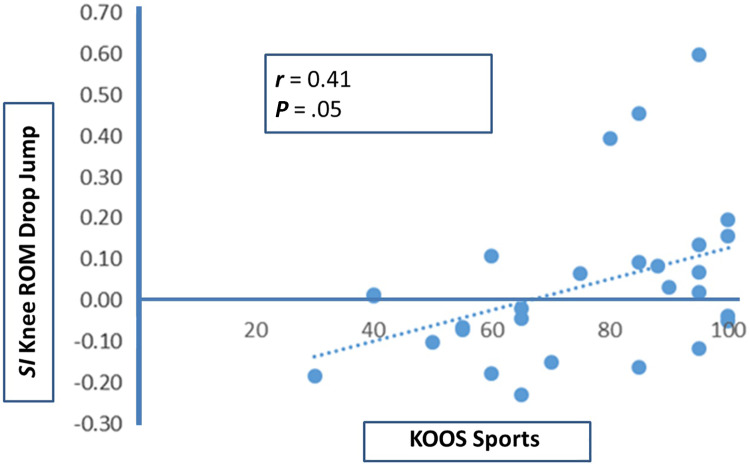
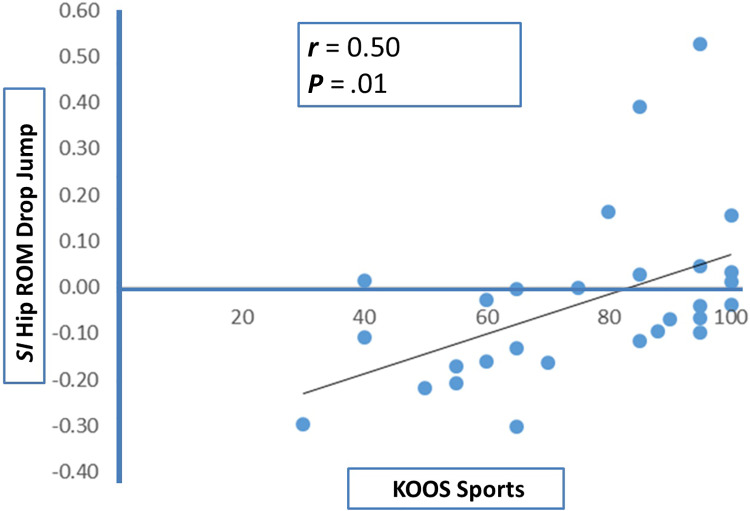
At follow-up, concentric knee torque in the operated limb correlated with Tegner and Marx scores (r = 0.42-0.47; P ≤ .05). Regarding the SI of knee torque, the highest Tegner, Marx, and KOOS (Knee injury and Osteoarthritis Outcome Score) results were associated with symmetry, as opposed to patients with extreme positive or extreme negative SIs (P < .05). As for landing kinematics, Tegner score negatively correlated with knee range of motion (ROM) in the operated limb (r = –0.38; P ≤ .05). With regard to SI, hip and knee ROM correlated with Tegner, IKDC, and KOOS scores (r = 0.41-0.51; P ≤ .05). Specifically, the highest sports participation levels were associated with achieving symmetric hip and knee ROM but also with extreme positive SIs, as opposed to patients with extreme negative SIs (P < .03), indicating substantially higher ROM in the uninjured limb as compared with the operated limb.
Conclusion:
At 5 to 10 years after ACL reconstruction, maintenance of sports participation was associated with symmetric side-to-side concentric knee torque and with producing greater attenuation of hip and knee ROM during the drop jump landing in the operated limb. Therefore, eccentric load programs that can improve attenuation-phase kinematics during landing tasks may be valuable in addition to concentric training and may facilitate enhanced long-term outcomes.
Keywords: ACL reconstruction, drop jump test, single-leg landing test, isokinetic strength test, sports participation
Returning to sport with the establishment of normal knee biomechanics is the primary goal of anterior cruciate ligament (ACL) reconstruction surgery. Following that, maintenance of sports activities throughout the years becomes a second important target, particularly for those who undergo surgery at a relatively young age. This target is related to a multifactorial process involving complex neuromuscular recovery among other factors that evolve over the years.17 One suggested strategy to improve decision making for young athletes throughout early recovery and later during the sports maintenance process is by integrating subjective measures (ie, patient-reported outcome scales) with objective biomechanical measures that assess knee function.7 Until today, however, there has been limited evidence to support clear associations between objective measures of knee function in sports-related tasks and the achievement of returning to sports alongside long-term maintenance of sports activities.6 Further information in this respect can therefore be valuable. In addition, noticeable limitations of study designs related to this subject can be appreciated. These include relying primarily on (1) follow-up assessments of <2 years, which miss the time frame of long-term maintenance of activities, and (2) heterogeneous study populations of mixed graft sources, multiple age groups, or both sexes for a reported outcome.8,15,21
Because knee function after ACL reconstruction is affected by patient age,16,18 duration of follow-up, graft source,32,33,37,41 and sex,2,8,13,19,30,37,40 greater specificity of patient demographics and surgical procedure has been recommended,21 and longer follow-up is required to evaluate function specifically during the maintenance phase after surgery. Furthermore, since ACL reconstruction is particularly justifiable in the young adult age group (ie, 18-35 years),36 5- to 10-year follow-up could represent an optimal time frame for assessing maintenance of sports activities beyond the short-term recovery. The reason is that longer follow-up may subject the outcomes to changes in lifestyle for reasons other than the knee injury or to potential progression of other health-related problems, which may confound the interpretation of sports activity maintenance as it relates to knee recovery.23,29,39
The purpose of the current study was therefore to test the association between maintenance of sports participation at 5 to 10 years after ACL reconstruction and measures of force production and landing mechanics in young men. Based on a meta-analysis that showed altered lower limb kinetics and kinematics at >3 years after ACL reconstruction,10 it was hypothesized that at 5 or more years after surgery, biomechanical abnormalities through the ankle, knee, and hip joints could still be identified and that specific associations between objective biomechanical measures and measures of maintaining sports activities could be determined.
Methods
We identified patients who underwent autologous quadrupled gracilis-semitendinosus ACL reconstruction between 2004 and 2010 at a single arthroscopy unit. The surgery was performed in all patients by using principles similar to the transtibial femoral tunnel drilling technique. Inclusion criteria for this study were (1) male sex, (2) ACL tear that occurred during sport activity only, (3) age of 18 to 35 years at surgery, (4) isolated ACL reconstruction without concomitant knee ligament reconstruction, and (5) follow-up of 5 to 10 years. Exclusion criteria were (1) contralateral ACL tear; (2) revision ACL reconstruction performed during the follow-up period or magnetic resonance imaging–documented ACL graft tear with functional instability awaiting revision; and (3) other significant lower limb injury, surgery, or deformity that could affect lower limb function. In accordance with these criteria, 55 patients were eligible and available for latest clinical follow-up evaluations, and their outcomes and outcome-associated risk factors were published in a separate article.12 Of these 55 patients, 30 volunteered to participate in the current study, which involved further tests in a biomechanical laboratory setup. This study was approved by an institutional review board, and each participant signed informed consent.
To assess maintenance of sports activities, Tegner38 and Marx activity rating scale (Marx)24 scores were used to indicate level of activity, while the International Knee Documentation Committee (IKDC) subjective score3 and the Knee injury and Osteoarthritis Outcome Score (KOOS)35 were used to indicate subjective knee function. Knee laxity was evaluated via side-to-side difference by a KT-1000 arthrometer (MEDmetric Corp) while the knee was in 25° of flexion and under anteriorly directed 30 lb of force. All KT-1000 measurements were performed by a single independent investigator (I.H.) who was not involved in the index surgery. Four objective tests to assess knee biomechanics were performed in a biomechanical laboratory by another independent investigator (Y.W.), who was not involved in the index surgery and was blinded to the KT-1000 measurements and the patient-reported outcome scores. These included (1) isokinetic strength tests of knee flexors and extensors, (2) single-leg landing test, (3) double-leg drop jump test, and (4) single-leg hop test for distance.
An isokinetic dynamometer (Biodex System 3; Biodex Medical Systems Inc) was used to measure knee flexor and extensor maximal torque and work at 180 deg/s. The testing was performed in a seated position, with the hip at 110° of flexion and the knee at 90° of flexion as a comfortable starting position. The participant was secured to the chair by 2 straps across the chest and a single strap at the abdomen and distal thigh of the tested limb to minimize compensations. Knee range of motion (ROM) was set at 90°, with 0° indicating full extension. Before testing, correction for gravity of the tested limb was performed, and several warm-up repetitions were completed. These included 3 submaximal repetitions and 2 maximal repetitions at 180 deg/s. All participants started the test with the healthy, uninjured knee before the operated knee. During the test, the participant was encouraged to perform 5 repetitions in maximal torque of knee flexion and extension at 180 deg/s. The outcome measure of the test was peak flexor and extensor torque (N·m/kg).
For the single-leg landing test and double-leg drop jump test, the following biomechanical model was used for movement analysis: 21 photo-reflective markers were placed at anatomic landmarks on each lower extremity from foot to pelvis level. Location of markers was in accordance with a standard plug-in gait protocol (Vicon Motion Systems Ltd). A knee alignment device was mounted on each knee at the beginning of each examination for the purpose of segment alignment setup at the neutral standing position during a static trial and was then removed before beginning the dynamic tests. In both tests, the participant landed on a force plate (Kistler Group) sampled at 960 Hz. A 6-camera optical stereometric system (Vicon Motion Systems Ltd), sampling at 240 Hz, was used to track lower extremity motions. Data were sampled with the NEXUS 1.7.1 program with a Woltring filter for filling gaps and a Butterworth fourth-order filter with a cutoff frequency of 6 Hz built into the program, and reports were processed with Polygon 3.5.1 software (Vicon Motion Systems Ltd).
The single-leg landing test was performed in accordance with a previous investigation5 as follows. Patients stood on a 21 cm–height step located 6 cm in front of the force plate. Their initial position was both feet on the step facing the force plate. Participants were instructed to place the hands on the waist. They then stepped forward with the test leg and dropped from the step, landing on the force plate on the test leg only. Participants were instructed to stabilize as quickly as possible. After the landing, they remained on the force plate for 3 seconds at the described position. The performance was disqualified and performed again if the opposite leg also touched the ground. Between the performances, the patient rested 30 seconds. This test was performed 3 times for each leg. The following measures were extracted from this test: time to stability (seconds) and peak vertical ground-reaction forces / body weight (N/kg). The beginning of the landing phase was defined as the time that the force platform signal reached 20 N. The moment of stability was defined, in accordance with previous investigators,5 as the time from which the moving mean signal did not exceed 25% of the mean of the standard deviation of the whole series mean. Results are reported per the mean of the 3 trials.
The drop jump test was performed in accordance with previous investigations25,31 as follows. Patients stood on a 21 cm–height step located 6 cm in front of the force plate. Their initial position was both feet on the step facing the force plate. Participants were instructed to place the hands on the waist. The patient dropped off the box, landed with each foot onto a separate force platform, and immediately executed a maximal effort vertical jump. The eccentric phase of the drop landing was defined as the duration of time that the force platform signal reached 20 N to the lowest vertical height of the line connecting the right and left anterior superior iliac spine markers. The following measures were extracted for each limb during the eccentric phase of the drop jump test: (1) peak support moment,42 computed as the momentary highest summation of sagittal torque of hip extension, knee extension, and ankle plantar flexion (N·m/kg), and (2) ROM in the sagittal plane at the ankle, knee, and hip joints (degrees). ROM was defined as the difference between maximal flexion and maximal extension during the eccentric phase. Total ROM of the lower limb during the eccentric phase of the drop jump was computed as the summation of the ankle, knee, and hip ROMs. Results are reported as the mean of all trials.
The single-leg hop test for distance was performed with takeoff and landing on the same limb as described.28 The distance was measured bilaterally. The longest hop of 3 trials was selected for analysis.
The symmetry index (SI) for all biomechanical measures was calculated in accordance with an accepted formula used to indicate asymmetries between the limbs in different variables of gait34: SI (%) = 2 × (Xn – Xi) / (Xn + Xi) × 100, where Xn indicates the value of variable in the uninjured side and Xi indicates the value of variable in the injured side. Perfect symmetry is achieved when SI equals zero.
Statistical Analysis
The study sample size was in accordance with previous investigations that evaluated hip and knee landing kinetics and kinematics after ACL reconstruction. These referred to sample sizes of 11 to 35 patients.21 Intraclass correlation coefficients (ICCs) were computed to estimate the reliability of the biomechanical measures. Associations between the subjective measures of ongoing sports participation at 5- to 10-year follow-up and the objective measures of muscle strength and landing biomechanics were analyzed by means of Pearson product-moment correlations. In addition, based on the large standard deviations observed in most biomechanical measures among the participants despite symmetric mean values, subgroup analysis was added to assess whether extreme asymmetry in any of the objective biomechanical variables was associated with reported outcome scores of sports participation. For this purpose, 3 subgroups were defined in relation to the SI of the biomechanical variables: (1) patients with an extreme positive SI (ie, SI higher than +10%; the uninjured limb was characterized by a substantially higher value of the biomechanical variable as compared with the operated limb), (2) patients with an extreme negative SI (ie, SI lower than –10%; the operated limb was characterized by a substantially higher value of the biomechanical variable as compared with the uninjured limb), and (3) patients with almost perfect side-to-side symmetry (ie, SI between –10% and +10%). With each sports participation outcome score as a dependent variable, 1-way analyses of variance were applied for each biomechanical variable to compare the means among the 3 subgroups. In case of a significant main effect, a Tukey honest significance test was used for post hoc comparisons among the means. Level of significance was set at .05. SPSS (v 25; IBM) was used for data analysis.
Results
The Tegner activity level before the injury was a mean ± SD of 8.0 ± 1.4 (range, 7-10), supportive of the study sample representing ACL reconstruction in an active population in terms of cutting-pivoting sports. Mean body mass index was within normal range (24.1 ± 2.2). Mean KT-1000 side-to-side difference was 3.1 ± 2.2 mm, and in 26 (87%) cases, the difference was ≤5 mm, which is considered “normal” or “nearly normal.”11 This also supports the generalizability of the studied group in terms of surgical outcome and in accordance with others who evaluated a similar graft source for ACL reconstruction at 7-year follow-up.22
Table 1 presents the patient-reported outcome scores at 5 to 10 years after surgery. Mean activity level scores indicated that patients were maintaining moderately intense sports activities. Among the reported functional outcome scales, the lowest scores were represented by KOOS-Sports and KOOS–Quality of Life, which also displayed the largest variability. Table 2 presents descriptive statistics of all biomechanical measures in the operated limb and contralateral uninjured limb.
Table 1.
Patient Activity Reported Outcomesa
| Reported Outcome | Mean ± SD |
|---|---|
| Tegner score | 6.0 ± 2.3 |
| Marx activity rating scale | 6.4 ± 5.4 |
| IKDC subjective | 83.3 ± 13.2 |
| KOOS subscale | |
| Knee Symptoms | 82.9 ± 11.3 |
| Pain | 87.8 ± 12.7 |
| ADL | 94.5 ± 9.3 |
| Sports | 76.8 ± 20.8 |
| QOL | 62.0 ± 22.2 |
aADL, Activities of Daily Living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; QOL, Quality of Life.
Table 2.
Biomechanical Measuresa
| Measure | ACLR Limb | Contralateral Limb | Symmetry Index, %b |
|---|---|---|---|
| Knee isokinetic peak torque, N·m/kg | |||
| Extension | 1.73 ± 0.4 | 1.85 ± 0.4 | 6.8 ± 21.5 |
| Flexion | 0.88 ± 0.2 | 0.90 ± 0.2 | 2.4 ± 18.8 |
| Single-legged landing | |||
| Time to stability, s | 1.25 ± 0.1 | 1.25 ± 0.1 | 0.3 ± 6.3 |
| Peak GRF/BW, N/kg | 39.3 ± 8.4 | 40.1 ± 9.8 | 1.7 ± 11.5 |
| Drop jump | |||
| Peak support moment/BW, N·m/kg | 4.75 ± 1.5 | 4.69 ± 1.6 | –1.6 ± 22.7 |
| Torque at peak support moment, N·m/kg | |||
| Hip | 1.78 ± 0.52 | 1.45 ± 0.61 | –16.9 ± 47.1 |
| Knee | 1.59 ± 0.80 | 1.67 ± 0.83 | 5.1 ± 42.3 |
| Ankle | 1.38 ± 0.55 | 1.57 ± 0.71 | 5.9 ± 24.5 |
| Sagittal ROM, deg | |||
| Hip | 31.3 ± 14.5 | 30.7 ± 13.7 | –3.3 ± 18.0 |
| Knee | 47.5 ± 13.3 | 49.1 ± 13.7 | 3.6 ± 19.4 |
| Ankle | 39.2 ± 18.6 | 41.9 ± 16.7 | 9.1 ± 42.8 |
| Total (hip + knee + ankle) | 118.0 ± 32.4 | 121.7 ± 35.5 | 2.6 ± 24.7 |
| Single-leg hop for distance, m | 1.79 ± 0.3 | 1.84 ± 0.2 | 1.6 ± 6.9 |
aValues are presented as mean ± SD. ACLR, anterior cruciate ligament reconstruction; BW, body weight; GRF, ground-reaction force; ROM, range of motion.
bPositive symmetry index indicates a higher value of the measured variable in the contralateral uninjured limb, and negative symmetry index indicates a higher value of the measured variable in the operated limb. In all measures, except hip torque component of the overall peak support moment (defined as hip torque at peak support moment) during the drop jump landing, mean side-to-side symmetry indices were within ±10%, but large SDs suggested high variability among participants in almost all biomechanical measures tested.
Tables 3 and 4 present bivariate correlation coefficients between Tegner, Marx, IKDC, and KOOS scores and each biomechanical measure. At follow-up, Tegner and Marx activity level scores were positively correlated with concentric knee flexor and extensor peak torque and with hip torque at peak support moment in the operated limb during the drop jump landing. Tegner scores were also positively correlated with single-leg peak ground-reaction force and negatively correlated with knee and total sagittal ROM in the operated limb during the drop jump landing. In relation to SIs, hip sagittal ROM SI during the drop jump landing positively correlated with the Tegner score and with IKDC, KOOS-Sports, and KOOS–Quality of Life scores at follow-up, while knee sagittal ROM SI during the drop jump landing positively correlated with the latter 3 measures of sports maintenance. Preinjury Tegner scores significantly correlated with most unilateral biomechanical measures tested in the operated limb.
Table 3.
Bivariate Correlation Coefficients: Contralateral Limb, Operated Limb, and Symmetry Index for the Tegner, Marx, and IKDC Scoresa
| Tegner Preinjury | Tegner Follow-up | Marx Follow-up | IKDC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | CL | ACLR | SI | CL | ACLR | SI | CL | ACLR | SI | CL | ACLR | SI |
| Peak knee torque at 180 deg/s | ||||||||||||
| Extensor | 0.44b | 0.54b | –0.15 | 0.33 | 0.46c | –0.21 | 0.44c | 0.47b | –0.09 | –0.06 | 0.15 | –0.29 |
| Flexor | 0.52b | 0.53b | 0.03 | 0.31 | 0.42c | –0.13 | 0.29 | 0.42c | –0.15 | –0.03 | 0.14 | –0.21 |
| Single-legged landing | ||||||||||||
| Time to stability | 0.05 | 0.11 | 0.05 | 0.13 | –0.12 | –0.31 | 0.17 | –0.12 | –0.37c | 0.17 | 0.05 | –0.18 |
| Peak GRF/BW | 0.35 | 0.26 | 0.23 | 0.33 | 0.45c | –0.17 | 0.14 | 0.31 | –0.17 | 0.13 | 0.05 | 0.18 |
| Drop jump | ||||||||||||
| Peak support moment/BW | 0.63b | 0.57b | 0.14 | 0.37 | 0.38 | –0.03 | 0.34 | 0.37 | –0.06 | –0.20 | –0.11 | –0.24 |
| Torque at peak support moment | ||||||||||||
| Hip | 0.34 | 0.32 | –0.05 | 0.46c | 0.47c | –0.09 | 0.47c | 0.51c | –0.09 | 0.10 | –0.03 | –0.13 |
| Knee | 0.64b | 0.54b | –0.08 | 0.17 | 0.25 | 0.14 | 0.14 | 0.20 | 0.15 | –0.17 | –0.02 | 0.34 |
| Ankle | 0.37 | 0.44c | 0.07 | 0.19 | 0.20 | –0.01 | 0.15 | 0.22 | 0.07 | –0.41c | –0.23 | 0.29 |
| Sagittal ROM | ||||||||||||
| Hip | –0.26 | –0.41c | 0.34 | 0.06 | –0.12 | 0.43c | 0.11 | –0.01 | 0.27 | 0.40c | 0.23 | 0.51c |
| Knee | –0.33 | –0.56b | 0.39c | –0.17 | –0.38c | 0.33 | –0.09 | –0.25 | 0.23 | 0.38c | 0.06 | 0.46c |
| Ankle | –0.24 | –0.45c | 0.25 | –0.05 | –0.32 | 0.27 | 0.07 | –0.25 | 0.24 | –0.05 | –0.26 | 0.24 |
| Totald | –0.35 | –0.64b | 0.33 | –0.06 | –0.38c | 0.33 | 0.05 | –0.24 | 0.28 | 0.28 | –0.01 | 0.37 |
| Single-leg hop test for distance | 0.50b | 0.65b | 0.31 | 0.29 | 0.33 | –0.06 | 0.20 | 0.31 | 0.02 | –0.09 | 0.07 | 0.34 |
aACLR, anterior cruciate ligament reconstruction; BW, body weight; CL, contralateral (uninjured); GRF, ground-reaction force; IKDC, International Knee Documentation Committee; ROM, range of motion; SI, symmetry index.
bP ≤ .01.
cP ≤ .05.
dHip + knee + ankle.
Table 4.
Bivariate Correlation Coefficients: Contralateral Limb, Operated Limb, and Symmetry Index for the KOOS Subscalesa
| Knee Symptoms | Pain | ADL | Sports | QOL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | CL | ACLR | SI | CL | ACLR | SI | CL | ACLR | SI | CL | ACLR | SI | CL | ACLR | SI |
| Peak knee torque at 180 deg/s | |||||||||||||||
| Extensor | –0.07 | 0.09 | –0.20 | –0.15 | –0.11 | –0.07 | –0.05 | 0.02 | –0.11 | 0.02 | 0.22 | –0.27 | 0.10 | 0.27 | –0.24 |
| Flexor | –0.12 | 0.03 | –0.18 | –0.21 | 0.00 | –0.29 | –0.15 | –0.09 | –0.07 | 0.02 | 0.20 | –0.21 | 0.05 | 0.28 | –0.30 |
| Single-legged landing | |||||||||||||||
| Time to stability | 0.13 | 0.07 | –0.07 | 0.09 | 0.02 | –0.11 | 0.23 | 0.21 | –0.05 | 0.19 | 0.13 | –0.10 | –0.03 | –0.12 | –0.13 |
| Peak GRF/BW | –0.10 | –0.10 | –0.02 | 0.07 | –0.06 | 0.23 | 0.06 | –0.06 | 0.21 | –0.01 | –0.04 | 0.02 | 0.04 | 0.03 | 0.07 |
| Drop jump | |||||||||||||||
| Peak support moment/BW | –0.26 | –0.19 | –0.24 | –0.30 | –0.23 | –0.08 | –0.18 | –0.02 | –0.26 | –0.18 | –0.08 | –0.25 | 0.01 | 0.00 | –0.01 |
| Torque at peak support moment | |||||||||||||||
| Hip | –0.11 | –0.25 | –0.06 | 0.00 | –0.15 | –0.11 | –0.19 | –0.26 | 0.02 | 0.04 | 0.00 | –0.03 | 0.26 | 0.02 | –0.29 |
| Knee | –0.25 | –0.10 | 0.35 | –0.25 | –0.10 | 0.31 | –0.01 | 0.19 | 0.38 | –0.11 | –0.05 | 0.15 | –0.05 | 0.00 | 0.14 |
| Ankle | –0.21 | –0.12 | 0.14 | –0.45b | –0.32 | 0.13 | –0.25 | –0.08 | 0.22 | –0.36 | –0.14 | 0.33 | –0.22 | –0.03 | 0.29 |
| Sagittal ROM | |||||||||||||||
| Hip | 0.43b | 0.35 | 0.24 | 0.33 | 0.27 | 0.21 | 0.08 | 0.01 | 0.15 | 0.48c | 0.33 | 0.50c | 0.36 | 0.21 | 0.48c |
| Knee | 0.35 | 0.19 | 0.18 | 0.35 | 0.14 | 0.28 | 0.05 | –0.10 | 0.22 | 0.48b | 0.19 | 0.41b | 0.44b | 0.13 | 0.46b |
| Ankle | 0.20 | –0.01 | 0.15 | –0.05 | –0.25 | 0.16 | –0.03 | –0.08 | 0.06 | 0.11 | –0.22 | 0.29 | 0.04 | –0.26 | 0.29 |
| Totald | 0.41b | 0.23 | 0.19 | 0.24 | 0.05 | 0.21 | 0.10 | –0.08 | 0.12 | 0.43b | 0.10 | 0.40b | 0.40b | 0.01 | 0.43b |
| Single-legged hop test for distance | –0.13 | –0.07 | 0.09 | –0.23 | –0.01 | 0.33 | –0.07 | 0.13 | 0.40b | 0.01 | 0.14 | 0.28 | 0.02 | 0.15 | 0.23 |
aACLR, anterior cruciate ligament reconstruction; ADL, Activities of Daily Living; BW, body weight; CL, contralateral (uninjured); GRF, ground-reaction force; KOOS, Knee injury and Osteoarthritis Outcome Score; QOL, Quality of Life; ROM, range of motion; SI, symmetry index.
bP ≤ .05.
cP ≤ .01.
dHip + knee + ankle.
Table 5 presents subgroup comparisons of the 3 SI categories of biomechanical measures that showed significant associations with ongoing sports participation scores. These included knee isokinetic muscle torque and hip and knee ROM during the drop jump landing. For isokinetic extensor and flexor knee torque, patients who reported the highest ongoing sports participation belonged to the midrange subgroup of SI. These patients had close-to-perfect symmetry of extensor and flexor knee torque values. For hip and knee ROM during the drop jump landing, patients who reported the highest ongoing sports participation belonged to the symmetric SI subgroup but also to the extreme positive SI subgroup (SI > +10%), which refers to patients with substantially higher hip and knee ROM in the uninjured limb as compared with the operated limb during the drop jump landing.
Table 5.
Activity Outcome Scores Among SI Subgroups of Knee Torque and Drop Jump Kinematics Showing Significant Interrelationshipsa
| Biomechanical Measure: Activity-Reported Outcome Measure | SI Subgroup, Mean ± SD | Post Hoc Comparisons | P Value | ||
|---|---|---|---|---|---|
| (1) SI < –10% | (2) SI ± 10% | (3) SI > +10% | |||
| Quadriceps peak torque/BW | |||||
| Marx: latest follow-up | 1.5 ± 1.9 | 9.0 ± 4.9 | 5.3 ± 5.3 | 1 < 2 | .025 |
| KOOS–Knee Symptoms | 76.8 ± 9.6 | 89.1 ± 9.6 | 78.5 ± 10.8 | 1, 3 < 2 | .024 |
| Hamstrings peak torque/BW | |||||
| Tegner: latest follow-up | 6.0 ± 2.1 | 7.0 ± 2.2 | 4.7 ± 1.8 | 3 < 2 | .041 |
| Marx: latest follow-up | 6.7 ± 6.0 | 8.64 ± 5.3 | 3.1 ± 3.3 | 3 < 2 | .037 |
| DJ hip sagittal ROM | |||||
| IKDC subjective | 73.3 ± 10.5 | 85.5 ± 12.6 | 94.8 ± 5.1 | 1 < 2, 3 | .006 |
| KOOS–Knee Symptoms | 75.8 ± 7.8 | 84.5 ± 11.9 | 88.3 ± 10.0 | 1 < 2, 3 | .073 |
| KOOS-Sports | 57.5 ± 15.5 | 84.5 ± 18.1 | 90.0 ± 9.1 | 1 < 2, 3 | .001 |
| KOOS-QOL | 41.5 ± 14.9 | 70.6 ± 18.4 | 72.0 ± 16.6 | 1 < 2, 3 | .001 |
| DJ knee sagittal ROM: KOOS-QOL | 43.1 ± 17.5 | 63.1 ± 22.9 | 72.4 ± 12.4 | 1 < 3 | .027 |
aThe SI subgroup with the highest activity outcome score for each biomechanical measure is indicated in bold. BW, body weight; DJ, drop jump; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; Marx, Marx activity rating scale; QOL, Quality of Life; ROM, range of motion; SI, symmetry index.
Figures 1 and 2 show, on an individual basis, the correlations between knee and hip side-to-side SIs of ROM during the drop jump landing and maintenance of sports participation as represented by the KOOS-Sports score. Patients with higher scores (KOOS-Sports ≥80) were characterized by positive SIs as opposed to patients with lower scores (KOOS-Sports <80), who were characterized by negative SIs. This means greater attenuation of hip and knee ROM in the operated limb relative to the uninjured limb in more active patients.
Figure 1.
Correlations between knee side-to-side SIs of ROM during the drop jump landing and maintenance of sports participation as represented by KOOS-Sports score. KOOS, Knee injury and Osteoarthritis Outcome Score; ROM, range of motion; SI, symmetry index.
Figure 2.
Correlations between hip side-to-side SIs of ROM during the drop jump landing and maintenance of sports participation as represented by the KOOS-Sports score. KOOS, Knee injury and Osteoarthritis Outcome Score; ROM, range of motion; SI, symmetry index.
The ICCs for the reliability of the biomechanical measures were fair for the time to stability (ICC = 0.66 and 0.77 for the injured and uninjured limb, respectively) and high for all other variables (ICC = 0.86-0.99).
Discussion
The present study was designed to test correlations between objective biomechanical measures of force production and landing biomechanics and maintenance of sports participation at 5 to 10 years after ACL reconstruction. The most pronounced biomechanical characteristics observed in patients who reported higher maintenance of sports participation included (1) symmetric concentric knee extensor and flexor torque, (2) symmetric hip and knee ROM during the drop jump landing, and (3) positive side-to-side SIs of hip and knee ROM, indicating higher ROM in the uninjured limb during the drop jump landing. Inferior maintenance of sports participation was observed in patients with inverse side-to-side relationships of hip and knee ROM, where higher sagittal motion appeared in the operated limb as compared with the uninjured limb. In other words, patients who reported higher activity scores not only reestablished symmetric side-to-side concentric knee extensor and flexor torque but also showed improved hip and knee sagittal plane motion attenuation immediately following ground contact, which was accompanied by higher ground-reaction forces and higher moments in the operated limb.
Previous investigators have indicated the value of identifying asymmetries in hip and knee kinematics during the early phases of the rehabilitation process after ACL reconstruction.25,31 The current study shows that these asymmetries remain valuable to distinguish between an optimal and suboptimal functional recovery and thus potentially guide decision-making junctions long after surgery. These results are also consistent with those of previous investigators who emphasized that the best functional outcome scores were observed in patients who achieved symmetric knee ROM during the rehabilitation phase after ACL reconstruction.4 The SIs of isokinetic knee extensor and flexor torque have also been considered fundamental to guide decision making during the first and second years after surgery.1,9,14 The current results support the value of this measure during the maintenance phase at ≥5 years after surgery. In this regard, although studies by previous investigators have suggested nearly full recovery of knee muscle strength to deficits of within 10% relative to the uninjured side at ≥5 years after surgery,20,26 a finding supported by the current study in terms of group means, this did not undermine the value of measuring concentric force production around the knee during such a relatively long follow-up. The reason is that large interindividual variabilities in the ability to produce powerful knee extension and flexion torque characterized this population. Thus, close-to-perfect side-to-side symmetry of concentric knee flexor and extensor torque was still associated with maintenance of higher activity levels, as opposed to patients with side-to-side SIs either higher than +10% or lower than –10%. Altogether, it could be summarized that to maintain higher activity levels at the maintenance phase after ACL reconstruction, patients would benefit from re-establishment of concentric knee force production, which is important during jumping or changing directions, in addition to optimizing eccentric muscle torque around the knee and hip, which is important to re-establish stable and effective landing.
Of note, drop jump landing kinematics in this study were reported through sagittal plane motions at the hip, knee, and ankle, although motion in this plane is interrelated with coronal and transverse plane motions.25,31 Transverse plane kinematics involve smaller ROM and asymmetries and thus are harder to quantify as compared with sagittal plane kinematics.25 Furthermore, accuracy of measuring coronal plane kinematics has been previously questioned.27 Therefore, the focus in this study was on sagittal plane kinematics, which is consistent with previous investigations.15
Among the biomechanical measures tested, all showed side-to-side SI means of within ±10%, except hip torque at peak support moment, which showed substantial asymmetry, with 17% higher values at the operated side. This may imply that patients compensate for suboptimal knee function by generating higher torque at the hip region of the involved side to dissipate the external loads during the drop jump landing. The clinical significance of the hip role during this task was substantiated by the correlations between hip torque levels at peak support moment during the drop jump landing and Tegner and Marx scores at follow-up (see Table 3). It is also important to note that the clinical benefit of achieving symmetry in this study should be viewed in light of the fact that the contralateral limb in this group represented a healthy uninjured limb, with normal values of strength and kinematics. Symmetry by itself may not be a desired goal in cases where the contralateral limb is poorly functioning for whatever reason.
Preinjury Tegner activity level was associated with several biomechanical characteristics at 5 to 10 years after the operation. These variables accounted for 17% to 42% of the variance of the Tegner preinjury scores despite the prolonged follow-up period. Five variables were associated with preinjury activity for the operated and uninjured limbs: isokinetic knee flexor and extensor torque, peak drop jump support moment, knee torque during peak drop jump support moment, and single-leg hop distance. These results may well exemplify a general association between preinjury activity level and higher ability for force production, even in the long run. This also provides a biomechanical explanation for the association observed previously12 between preinjury and long-term follow-up Tegner levels after ACL reconstruction, beyond the mere “wish” of any athlete to maintain activity levels throughout the years after an injury. Furthermore, in the operated limb, a lower preinjury Tegner score was associated with lower sagittal ROMs during force absorption in all 3 lower extremity joints. Since knee sagittal ROM during force attenuation was significantly related to Tegner score during follow-up as well, together these results point again to a potential benefit of inclusion of an eccentric strengthening of the lower musculature through a limited ROM in the adaptation process, particularly with respect to the knee muscles. This perspective is in accordance with recent meta-analyses that showed reductions in knee extension moments in ACL-reconstructed knees during single- and double-leg landing tasks,15,21 a finding that supports addressing such deficits after surgery.
The significant relationships between Tegner activity level scores and long-term movement characteristics signify the relevancy of motion variables in the evaluation of the adaptation process. Most strength measures of the operated limb as well as knee ROM correlated with preinjury and follow-up activity outcome measures. However, at follow-up, peak support moment and hip and ankle ROM during drop jump and single-leg hop distance did not reach significance. Yet, hip torque during drop jump landing significantly correlated with Tegner score at follow-up. The differences between the preinjury and follow-up associations of activity level with movement variables can be, at least in part, attributed to the span of the follow-up period. That is, at 5 or more years after the operation, maintenance of activities is subjected to multiple factors that determine whether athletes remain active and at which level. For example, factors that can affect Tegner level at follow-up besides biomechanical constraints per se may include changes in lifestyle for reasons other than the knee injury, accumulation of other health-related problems, and other intervening factors.23,29,39 With longer follow-up after surgery, it likely becomes even more challenging to isolate specific common biomechanical measures that correlate with maintenance of active lifestyle. This supports the rationale to limit this type of a study, which focuses on biomechanical aspects of sport-related elements of movement, to 5 to 10 years of follow-up, as opposed to studies that focus on the development of specific long-term knee morbidity (eg, arthritis), where longer follow-up after ACL reconstruction is desired.
Limitations of this study include the retrospective design and the use of the uninjured leg as a reference for measuring neuromuscular deficits in the injured leg. This is nevertheless in accordance with a recent study showing that neuromuscular functions—which include peak torque of knee extensor and flexor contractions measured on a Biodex dynamometer, knee joint proprioception, 1-leg standing balance test, and the single-leg hop test for distance—were not impaired in the uninjured leg at >6 months after an ACL injury, despite the reduction in physical activity following an injury.43 These results support the presumption that the contralateral limb can serve as adequate reference to examine recovery of the injured leg’s neuromuscular function during the rehabilitation process after an injury. In addition, the relatively limited follow-up rate of 55% resulted from the nature of this study, which was based on voluntary participation and required from the participants a thorough time-consuming biomechanical evaluation in a biomechanical laboratory. In these circumstances, 25 of the 55 patients, who were all young men from the working class, were unwilling to volunteer for personal reasons unrelated to the surgery. Despite this limitation, the study sample size was in accordance with previous investigations that reported hip and knee kinetics and kinematics after ACL reconstruction and referred to sample sizes of between 11 and 35 patients.21
Conclusion
At 5 to 10 years after ACL reconstruction, maintenance of sports participation is associated with symmetric side-to-side concentric knee torque and with producing greater attenuation of hip and knee ROM during drop jump landing in the operated limb. Therefore, eccentric load programs that can improve attenuation-phase kinematics during landing tasks may be valuable in addition to traditional concentric training and may facilitate enhanced long-term outcomes.
Footnotes
Final revision submitted March 26, 2020; accepted April 9, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Helsinki Committee at the Meir General Hospital, Kfar Saba, Israel (0215-13-MMC).
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ageberg W, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med. 2010;38:1334–1342. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34:128–135. [DOI] [PubMed] [Google Scholar]
- 4. Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4:2–12. [PMC free article] [PubMed] [Google Scholar]
- 5. Colby SM, Hintermeister RA, Torry MR, Steadman JR. Lower limb stability with ACL impairment. J Orthop Sports Phys Ther. 1999;29:444–454. [DOI] [PubMed] [Google Scholar]
- 6. Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48:356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dingenen B, Gokeller I. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;47:1487–1500. [DOI] [PubMed] [Google Scholar]
- 8. Engelen-van Melick N, van Cingel RE, Tijssen MP, Nijhuis-van der Sanden MW. Assessment of functional performance after anterior cruciate ligament reconstruction: a systematic review of measurement procedures. Knee Surg Sports Traumatol Arthrosc. 2013;21:869–879. [DOI] [PubMed] [Google Scholar]
- 9. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg HA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hart HF, Culvenor AG, Collins NJ, et al. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2016;50:597–612. [DOI] [PubMed] [Google Scholar]
- 11. Hefti F, Muller W, Jacob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. [DOI] [PubMed] [Google Scholar]
- 12. Hetsroni I, van-Stee M, Marom N, et al. Factors associated with improved function and maintenance of sports activities at five to ten years after autologous hamstring ACL reconstruction in young men. Orthop J Sports Med. 2017;5(4):2325967117700841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res. 2002;402:76–94. [DOI] [PubMed] [Google Scholar]
- 14. Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc. 2017;26:426–433. [DOI] [PubMed] [Google Scholar]
- 15. Johnston PT, McClelland JA, Webster KE. Lower limb biomechanics during single-leg landings following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Med. 2018;48:2103–2126. [DOI] [PubMed] [Google Scholar]
- 16. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaur M, Ribeiro DC, Theis JC, Webster KE, Sole G. Movement patterns of the knee during gait following ACL reconstruction: a systematic review and meta-analysis. Sports Med. 2016;46:1869–1895. [DOI] [PubMed] [Google Scholar]
- 18. Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish National Anterior Cruciate Ligament Register. Arthroscopy. 2014;30:803–810. [DOI] [PubMed] [Google Scholar]
- 19. Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Gender differences exist in neuromuscular control patterns during the pre-contact and early stance phase of an unanticipated side-cut and cross-cut maneuver in 15-18 years old adolescent soccer players. J Electromyogr Kinesiol. 2009;19:e370–e379. [DOI] [PubMed] [Google Scholar]
- 20. Lautamies R, Harilainen A, Kettunen J, Sandelin J, Kujala UM. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2008;16:1009–1016. [DOI] [PubMed] [Google Scholar]
- 21. Lepley AS, Kuenze CM. Hip and knee kinematics and kinetics during landing tasks after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. J Athl Train. 2018;53:144–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35:740–748. [DOI] [PubMed] [Google Scholar]
- 23. Markstrom JL, Tengman E, Hager CK. ACL-reconstructed and ACL-deficient individuals show differentiated trunk, hip, and knee kinematics during vertical hops more than 20 years post-injury. Knee Surg Sports Traumatol Arthrosc. 2018;26:358–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–218. [DOI] [PubMed] [Google Scholar]
- 25. Meyer CAG, Gette P, Mouton C, Seil R, Theisen D. Side-to-side asymmetries in landing mechanics from a drop vertical jump test are not related to asymmetries in knee joint laxity following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moisala AS, Jarvela T, Kannus P, Jarvinen M. Muscle strength evaluations after ACL reconstruction. Int J Sports Med. 2007;28:868–872. [DOI] [PubMed] [Google Scholar]
- 27. Mok KM, Kristianslund E, Krosshaug T. The effect of thigh marker placement on knee valgus angles in vertical drop jumps and sidestep cutting. J Appl Biomech. 2015;31:269–274. [DOI] [PubMed] [Google Scholar]
- 28. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. [DOI] [PubMed] [Google Scholar]
- 29. Ortiz A, Olson S, Libby CL, et al. Landing mechanics between noninjured women and women with anterior cruciate ligament reconstruction during 2 jump tasks. Am J Sports Med. 2008;36:149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nation-wide population based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42:278–284. [DOI] [PubMed] [Google Scholar]
- 33. Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41:249–262. [DOI] [PubMed] [Google Scholar]
- 34. Robinson RO, Herzog W, Nigg BM. Use of force platform variables to quantify the effects of chiropractic manipulation on gait symmetry. J Manipulative Physiol Ther. 1987;10:172–176. [PubMed] [Google Scholar]
- 35. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 36. Shea KG, Carey JL, Richmond J, et al. ; American Academy of Orthopaedic Surgeons. The American Academy of Orthopaedic Surgeons evidence-based guideline on management of anterior cruciate ligament injuries. J Bone Joint Surg Am. 2015;97:672–674. [DOI] [PubMed] [Google Scholar]
- 37. Spindler KP, Huston LJ, Wright RW, et al. ; MOON Group, Dunn WR. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39:348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 39. von Porat A, Henriksson M, Holmstrom E, Thorstensson CA, Mattsson L, Roos EM. Knee kinematics and kinetics during gait, step and hop in males with 16 years old ACL injury compared with matched controls. Knee Surg Sports Traumatol Arthrosc. 2006;14:546–554. [DOI] [PubMed] [Google Scholar]
- 40. Webster KE, McClelland JA, Palazzolo SE, Santamaria LJ, Feller JA. Gender differences in the knee adduction moment after anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2012;46:355–359. [DOI] [PubMed] [Google Scholar]
- 41. Webster KE, Wittwer JE, O’Brien Feller JA. Gait patterns after anterior cruciate ligament reconstruction are related to graft type. Am J Sports Med. 2005;33:247–254. [DOI] [PubMed] [Google Scholar]
- 42. Winter DA. Biomechanical motor patterns in normal walking. J Mot Behav. 1983;15:302–330. [DOI] [PubMed] [Google Scholar]
- 43. Zult T, Gokeler A, van Raay JJ, Brouwer RW, Zijdewind I, Hortobagyi T. An anterior cruciate ligament injury does not affect the neuromuscular function of the non-injured leg except for dynamic balance and voluntary quadriceps activation. Knee Surg Sports Traumatol Arthrosc. 2017;25:172–183. [DOI] [PMC free article] [PubMed] [Google Scholar]