Abstract
Background
Preliminary evidence suggested that the PPARγ agonist pioglitazone reduces opioid-withdrawal symptoms, possibly by inhibiting increases in proinflammatory cytokines.
Methods
A randomized, placebo-controlled clinical trial was conducted utilizing two different study designs (entirely outpatient, and a combination of inpatient and outpatient) to evaluate the safety and efficacy of pioglitazone as an adjunct medication for people with opioid physical dependence undergoing a buprenorphine taper. Participants were stabilized on buprenorphine/naloxone (sublingual, up to 16/4 mg/day), then randomized to receive oral pioglitazone (up to 45 mg/day) or placebo before, during, and after buprenorphine taper. Outcome measures included the Subjective Opiate Withdrawal Scale (SOWS) and Clinical Opiate Withdrawal Scale, use of rescue medications to alleviate opioid withdrawal symptoms, and opioid-positive urine specimens. Cerebrospinal fluid (CSF) and plasma were collected during the taper in a subset of participants for measurement of proinflammatory cytokines.
Results
The clinical trial was prematurely terminated due to slow enrollment; 40 participants per group were required for adequate statistical power to test study hypotheses. Twenty-four participants enrolled; 17 received at least one dose of study medication (6 pioglitazone, 11 placebo). SOWS scores were higher in the pioglitazone arm than in the placebo arm after adjusting for use of rescue medications; participants in the pioglitazone arm needed more rescue medications than the placebo arm during the post-taper phase. SOWS scores were positively correlated with monocyte chemoattractant protein-1 (MCP-1) in CSF (r = 0.70, p = 0.038) and plasma (r = 0.77, p = 0.015). Participants having higher levels of plasma MCP-1 reported higher SOWS, most notably after the buprenorphine taper ended.
Conclusions
Results from this study provide no evidence that pioglitazone reduces opioid withdrawal symptoms during buprenorphine taper. High correlations between MCP-1 and opioid withdrawal symptoms support a role of proinflammatory processes in opioid withdrawal.
Trial registration
clinicaltrials.gov identifier: NCT01517165
Keywords: Pioglitazone, Buprenorphine, Opioid withdrawal, Cytokines, Opioid dependence
For people with opioid use disorders (OUDs), longer treatment with long-acting opioid agonists such as methadone and buprenorphine is usually more beneficial than a taper (Fiellin et al. 2014). Indeed, taper is not a standalone treatment for OUDs (Gossop 2006), and, for some patients, may never be indicated <https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine>. Nonetheless, some patients want to transition to a medication-free state with appropriate ongoing care, or to maintenance on naltrexone, an opioid agonist. For them, a major unmet medical need is the physical difficulty of withdrawal from opioid agonist treatment, which can present a considerable challenge to maintaining abstinence from opioids. Agonist tapers can be augmented with the alpha-adrenergic drug clonidine, but clonidine in that context primarily reduces the objective signs of opioid withdrawal rather than the more problematic subjective symptoms (Jasinski et al. 1985). Lofexidine has been recently approved by the US FDA for the treatment of opioid withdrawal symptoms.
A new approach to the problem was suggested by preclinical and open-label findings with the FDA-approved diabetes medication pioglitazone (Actos) (Ghavimi et al. 2014). Pioglitazone activates the gamma (γ) subtype of peroxisome proliferator-activated receptors (PPARs), which help regulate sugar metabolism in fat cells (Berger and Moller 2002). PPARγ receptors are also expressed in microglia and neurons in the brain (Kumar et al. 2009) where they can reduce glia-mediated inflammatory responses. This is relevant in opioid physical dependence because glia-derived proinflammatory cytokines, such as interleukin 1β (IL-1β), interleukin 6 (IL-6), and tumor necrosis factor α (TNF-α) are increased with chronic exposure to morphine (Lin et al. 2009). Monocyte chemoattractant protein-1 (MCP-1) has been shown to be associated with development of morphine tolerance (Liu et al. 2017), and MCP-1 mRNA expression has been shown to be reduced in the peripheral blood mononuclear cells of people physically dependent on heroin (Song et al. 2002). Inhibition of these cytokines in rodents has been associated with reduction of opioid-tolerance development, and prevention of opioid withdrawal (Bland et al. 2009; Hutchinson et al. 2007; Hutchinson et al. 2009; Watkins et al. 2009). Pioglitazone is an appealing candidate to use for this purpose because it crosses the blood-brain barrier more easily than other medications in its class and has been shown to activate PPARγ receptors in the brain (Maeda et al. 2007). When we started the clinical trial reported here, we were aware of then unpublished data that pioglitazone (10 or 30 mg/kg) dose-dependently attenuated signs of withdrawal in mice treated sub-chronically with morphine and then given naloxone to precipitate withdrawal (de Guglielmo et al. 2017). We were also aware of a preliminary open-label clinical study in which four outpatients who had been maintained for years on high doses of methadone or buprenorphine, with longtime wishes to taper and multiple unsuccessful attempts to do so, were given pioglitazone (30 mg/day) and were then able to taper from their methadone or buprenorphine with few or no withdrawal symptoms or cravings (Ciccocioppo, unpublished data); the main rationale for our study was to follow up on those findings.
We now report findings from a randomized, placebo-controlled clinical trial, intended to evaluate the safety and efficacy of pioglitazone as an adjunct medication for participants with an OUD undergoing buprenorphine taper. The study was conducted using two different designs: an entirely outpatient study and one that included an 18-day inpatient stay during and after the buprenorphine taper. The clinical trial was prematurely terminated due to slow enrollment, so the number of participants included in this report (6 received pioglitazone, 11 placebo) is far fewer than the 40 participants per group that was required for adequate statistical power to test study hypotheses. The primary clinical endpoints were opioid withdrawal symptom severity, urine opioid drug test results, and use of rescue medications to reduce withdrawal symptoms during and after the taper. Cerebrospinal fluid (CSF) and plasma were collected to determine whether pioglitazone-associated reduction of withdrawal symptoms was mediated by inhibition of increases in proinflammatory cytokines.
Methods
Participants
We recruited participants with opioid dependence (by DSM-IV criteria, because the study was started before DSM-5) who were seeking an opioid agonist taper. Inclusion criteria included the following: 18–65 years of age; evidence of physical dependence on opioids as determined by self-report, urine drug screen and/or physical examination; and seeking an opioid agonist taper. Women had to be either post-menopausal, surgically sterile, or agree to use an IRB-approved form of birth control, e.g., specific hormonal contraceptives or condom plus spermicide. Exclusion criteria included the following: any medical or psychiatric condition that would compromise study participation (including but not limited to diabetes mellitus types I/II, congestive heart failure, cardiovascular or cerebrovascular disease, current diagnosis of any DSM-IV psychotic disorder, physical dependence on alcohol or sedative hypnotics), pregnant or breastfeeding, allergy to pioglitazone, and taking contraindicated medications (e.g., inhibitors and inducers of CYP2C8, certain hormonal contraceptives without the use of an additional method of birth control). Safety monitoring measures and data are reported in the supplementary materials.
Experimental design
Buprenorphine was administered in a naloxone combination product in a 4:1 ratio, as described below. Doses of the combination are expressed in terms of the buprenorphine dose for the remainder of this report.
Initially we conducted the study on an outpatient basis; however, no participants completed the study without using an illicit opioid. This impeded detection of the withdrawal suppressing effects of pioglitazone. Therefore, we revised the study design by shortening the trial and adding an 18-day inpatient stay during and after the end of the buprenorphine taper.
In the original outpatient study design, participants were randomized to receive either pioglitazone or placebo, beginning approximately 1 week after the first dose of buprenorphine and continuing for 12 weeks (2 weeks during buprenorphine maintenance, 4 weeks during a buprenorphine taper, and 6 weeks following the taper). The stabilization dose of buprenorphine was 16 mg/day; during the 4-week taper, the dose was reduced initially by 4 mg, then by 2 mg weekly (i.e., 12, 8, 4, and 2 mg). There was a follow-up visit 1 week after the last daily visit, and a follow-up phone call 3 weeks after that.
The revamped iteration of the study design combined inpatient and outpatient settings. The first 17 days of the study were outpatient: 14 days of buprenorphine stabilization and then the first 3 days of buprenorphine taper. The next 18 days were inpatient: 10 days of continued buprenorphine taper and then 8 more days after the completion of the buprenorphine taper. The participants were then discharged from the inpatient portion of the study and continued outpatient care at our clinic: 10 daily visits, a follow-up visit 1 week after the last daily visit, and a follow-up phone call 3 weeks after that. Participants received a total of 27 days of buprenorphine (14 days during stabilization followed by a 13-day taper). Participants were randomized to receive either pioglitazone or placebo with dosing beginning approximately 1 week after buprenorphine stabilization began and continuing for 5 weeks (3 weeks concurrently with buprenorphine and 2 weeks following the buprenorphine taper). The stabilization dose of buprenorphine was 16 mg, and during the 13-day taper, the dose was reduced to 12 mg on taper day 1, to 8 mg on taper day 4, to 4 mg on taper day 7, and to 2 mg on taper day 10.
In both iterations of the study, participants received weekly individual counseling, including case management, throughout their participation. At the end of the study, all participants were offered assistance with transfer to continued treatment, either medication-free or opioid-agonist treatment.
Data collection
Two opiate withdrawal scales were administered daily throughout the study: the Subjective Opiate Withdrawal Scale (SOWS) and Clinical Opiate Withdrawal Scale (COWS). The SOWS is a list of 16 withdrawal symptoms that participants rate from 0 (not at all) to 4 (extremely) (Handelsman et al. 1987). The COWS has 11 observer-rated items: resting pulse, gastrointestinal upset, sweating, tremor, restlessness, yawning, pupil size, anxiety or irritability, bone or joint aches, gooseflesh skin, and runny nose or tearing (Wesson and Ling 2003). For both scales, the score is the sum of the ratings of the individual items. Withdrawal was assessed daily prior to buprenorphine and pioglitazone dosing.
Drug use was monitored by urine drug screens and self-reports thrice weekly. Urine specimens were collected under observation and tested for morphine, buprenorphine, oxycodone, methadone, cocaine, tetrahydrocannabinol (THC), benzodiazepines, amphetamines, barbiturates, and phencyclidine. Participants were interviewed by trained staff to collect self-reports of drug use.
Participants were offered the option to undergo an additional single collection of blood and CSF. Participants were excluded from CSF collection for the following reasons: bleeding diathesis/coagulopathy; platelet count < 50,000 or INR (international normalized ratio) ≥ 1.5, or on Warfarin (coumadin); evidence of intracerebral mass based on history, neurologic exam, or papilledema on fundoscopic exam; clinically significant lumbar spine disease by history; history of abnormal cranial CT scan or MRI scan, suggesting the possibility of increased intracranial pressure. CSF and blood collection was done once during the buprenorphine taper when the dose was 4 mg/day. Blood and CSF specimens were frozen at −80 °C until the end of the study and then analyzed for the proinflammatory cytokines monocyte chemoattractant protein-1 (MCP-1), interleukin-1 beta (IL-1 beta), IL-6, IL-10, and tumor necrosis factor-alpha (TNF-alpha).
Plasma and CSF samples were analyzed in duplicate with MesoScale V-PLEX Plus (Meso Scale Discovery, MSD) Custom Proinflammatory Panel 1(IL-1β, IL-6, Il-10, TNF-α) and Custom Chemokine Panel 1 (MCP-1). Each 96-well plate had carbon electrodes in the bottom of each well, each pre-coated with one of the 5-anti-cytokine antibodies or the anti-chemokine antibody of interest. No samples had been repeatedly freeze-thawed.
All assays were performed according to the manufacturer’s instructions. The serum and CSF samples were diluted 2-fold in the Proinflammatory Panel 1 and 4-fold in the Chemokine Panel 1. The standard curves for each cytokine and chemokine were generated using the premixed lyophilized standards provided in the kits. Serial 4-fold dilutions of the standards were run to generate a 7-standard concentration set, and the diluent alone was used as a blank. Three levels of multianalyte lyophilized controls were used in all plates and were included in the kit. The plates were washed three times with Wash Buffer (150 μl) prior to sample addition. Fifty microliters of prepared samples, calibrators, or control were added to the wells and the plates sealed and incubated at room temperature with shaking for 2 h. The plates were washed three times with Wash Buffer (150 μl). Detection antibody (25 μl) was added per well, and the plate sealed and incubated at room temperature with shaking for 2 h. At the end of incubation, the plates were washed three times as before. One hundred microliters of the MSD 2X Read Buffer T was added to each well and incubated at room temperature for 10 min, and MSD plates were measured on the MSD Sector Imager 2400 plate reader.
Cytokine concentrations (pg/ml) were determined from the standard curve using a four-parameter logistic fit curve to transform the mean electrochemiluminescence signal (light) intensities into concentrations using the Discovery Workbench software (MSD).
Medications
Pioglitazone was administered once daily in 15 mg capsules. Active capsules (containing 15 mg pioglitazone tablets ground into powder) and identical-looking placebo capsules (containing lactose/cellulose powder) were prepared by the NIH Pharmaceutical Development Section. Participants were given three capsules at the time of dosing; capsules were either all active, a combination of active and placebo, or all placebo, depending on the required dose (e.g., one active capsule and two placebo capsules for a dose of 15 mg, three active capsules for a dose of 45 mg). In both iterations of the study, the pioglitazone dose began at 15 mg for the first 3 days, increased to 30 mg for the next 3 days, and increased to 45 mg daily for the remaining 11 weeks in the first iteration or the remaining 29 days of pioglitazone administration in the second iteration. Pioglitazone is FDA approved for the treatment of diabetes mellitus type 2 (DMT2). For treatment of DMT2, pioglitazone is initiated at 15 or 30 mg/day and may be titrated up 45 mg/day. The titration and dosing in this study were in accordance with the FDA-approved regimen for treating DMT2.
Buprenorphine/naloxone film (Reckitt Benckiser Pharmaceuticals, Inc.) was administered sublingually once daily during visits to the outpatient clinic or during the inpatient stay. Combinations of 8 mg buprenorphine/2 mg naloxone and 2 mg buprenorphine/0.5 mg naloxone film were used to deliver the prescribed doses. Buprenorphine/naloxone doses were not blind to participants or study staff.
Pioglitazone/placebo and buprenorphine were administered by study nursing staff. These medications were not given to take at home except on major holidays and serious weather events.
Rescue medications were administered as needed for symptomatic relief of opioid withdrawal. At each visit, a nurse assessed opioid withdrawal, and if noted by the participant, the study physician discussed the signs and symptoms with the participant and ordered rescue medication(s) as indicated. Symptomatic relief of opioid withdrawal was with ibuprofen, acetaminophen, hydroxyzine, dicyclomine, magnesium hydroxide, and loperamide. There are no known contraindications between these medications for the symptomatic relief of opioid withdrawal and either pioglitazone or buprenorphine. Benzodiazepines were not used. When participants were outpatients, they received a 7-day supply to take at home as needed; when participants were inpatients, study staff administered the medications as needed.
Data analysis
Comparability of treatment arms was checked using Fisher’s exact tests for categorical variables and two-sample t tests for continuous variables. Analysis of the primary outcome measures consisted of comparing withdrawal-symptom scores in the placebo vs. pioglitazone arms throughout the study. Because withdrawal scores were assessed daily, multilevel modeling was used, a repeated-measures approach that would not exclude participants with missing data. The independent variables were treatment arm (pioglitazone or placebo), time, and their interaction, plus use of rescue medications for opioid withdrawal (yes or no) and study iteration (inpatient vs. outpatient). Two models were run for each outcome measure (SOWS and COWS). The first model consisted of treatment arm (pioglitazone—yes or no), taper phase (yes or no), post-taper phase (yes or no), pioglitazone-by-taper interaction, pioglitazone-by-post interaction, use of rescue opioid withdrawal medications (yes or no), and study iteration (inpatient or outpatient). The second model was limited to the taper phase only and consisted of pioglitazone (yes or no), day of taper, pioglitazone-by-day interaction, use of adjunct opioid withdrawal medications (yes or no), and study iteration (inpatient or outpatient).
Secondary outcome measures were the use of rescue medications to alleviate opioid withdrawal symptoms during the study and opioid-negative urines during the post-taper monitoring period. Repeated-measures logistic regression was used to assess group differences in rates of rescue-medication use and of opioid-negative urines during post-taper monitoring. The modeling procedure used for rescue medications was analogous to that used for withdrawal-symptom scores.
Bivariate analyses were used to determine significant correlates of proinflammatory cytokine levels: treatment arm, participant demographics (age, race, sex), substance use (any opiate use and mean daily cigarette consumption in the 5 days prior to sample collection), opioid withdrawal symptoms (maximum SOWS and maximum COWS in the 5 days prior to sample collection). Two-sample t tests were run for categorical variables, and correlation coefficients were calculated for continuous variables.
Results
Participants
Twenty-four participants were enrolled in the study (14 in the initial outpatient iteration, 10 in the revised inpatient iteration), 21 of whom were randomized: 8 in the pioglitazone arm and 13 in the placebo arm. Seventeen received at least one dose of pioglitazone or placebo and were thus considered evaluable (6 in the pioglitazone arm, 11 in the placebo arm); six of them completed the study (2 in the pioglitazone arm, 4 in the placebo arm). A detailed participant disposition is shown in Fig. 1. There were no statistically significant differences between treatment arms on demographic variables, baseline opioid use, and study retention (Table 1).
Fig. 1.
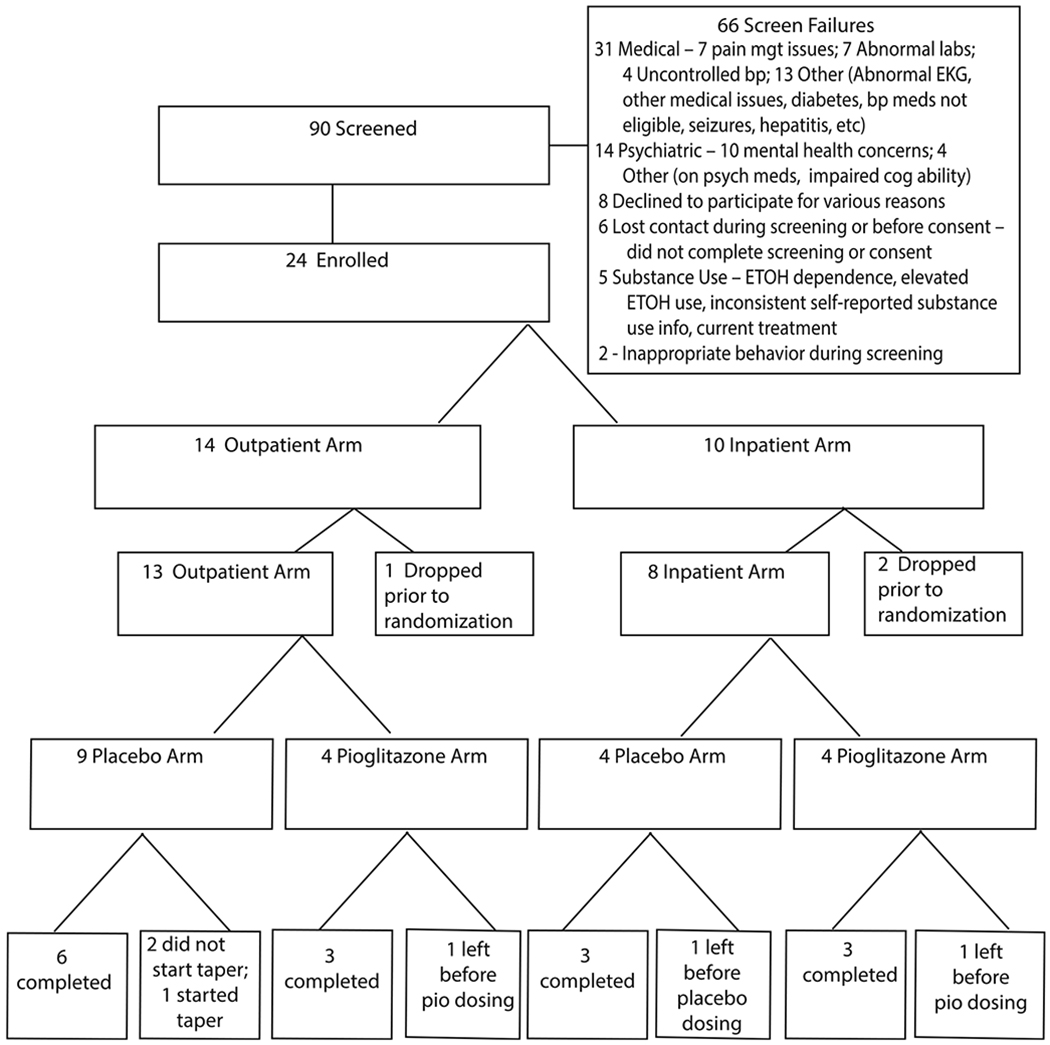
CONSORT diagram showing participant disposition for the outpatient and inpatient versions of the study
Table 1.
Characteristics of enrolled participants1
| Participant characteristics | Total enrolled (N = 24) | Pioglitazone (N = 8) | Placebo (N = 13) |
|---|---|---|---|
| Demographics | |||
| Age (mean ± SD) | 39.91 ± 8.22 | 38.43 ± 9.20 | 39.54 ± 7.74 |
| African American | 54.2% (13/24) | 37.5% (3/8) | 61.5% (8/13) |
| Female | 25.0% (6/24) | 37.5% (3/8) | 23.1% (3/13) |
| Years education (mean ± SD) | 13.04 ± 1.63 | 14.00 ± 2.20 | 12.69 ± 1.11 |
| Unemployed | 77.3% (17/22) | 85.7% (6/7) | 84.6% (11/13) |
| Baseline opioid use | |||
| Used heroin > 2 days past 30 days | 62.5% (15/24) | 75.0% (6/8) | 53.9% (7/13) |
| Years of heroin use (mean ± SD) | 9.88 ± 8.53 | 8.88 ± 8.17 | 11.46 ± 9.24 |
| Study retention | |||
| Completed study | 25.0% (6/24) | 25% (2/8) | 30.8% (4/13) |
| Evaluable | 70.8% (17/24) | 75% (6/8) | 84.6% (11/13) |
Pioglitazone and opioid withdrawal, rescue medications, and opioid use
The analyses of clinical endpoints for this study (withdrawal symptoms, use of rescue medications, and opioid-positive urine specimens) were limited to participants who received at least one dose of study medication (N = 17, 6 pioglitazone, 11 placebo) and to data that were collected during the pioglitazone/placebo administration period. Because of the differing study durations of the two iterations of the study (outpatient only, inpatient/outpatient), we elected to analyze data from the same time frame for both iterations: 1 week before, during, and 2 weeks after the buprenorphine taper. As noted above, we also included study iteration as a covariate in all models.
Opiate withdrawal—SOWS and COWS
Figures 2 and 3 show individual participants’ SOWS scores over time, along with urine opioid results and adjunct medication use. The time points in the figure represent the portion of the study during which participants were receiving pioglitazone; participants are receiving buprenorphine on days < 0. Each panel in Fig. 2 is a participant who received pioglitazone (n = 6), each panel in Fig. 3 is a participant who received placebo (n = 9). Two participants in the placebo group were omitted from Fig. 3: one due to dropping out prior to the taper phase, and another due to early dropout and few data points. These participants were only omitted from the figure in order to best utilize the space in the figure; their data were included in all analyses. There is an upward trend in SOWS scores over time that is visually apparent among the majority of participants in the pioglitazone group, but in the minority of participants in the placebo group.
Fig. 2.
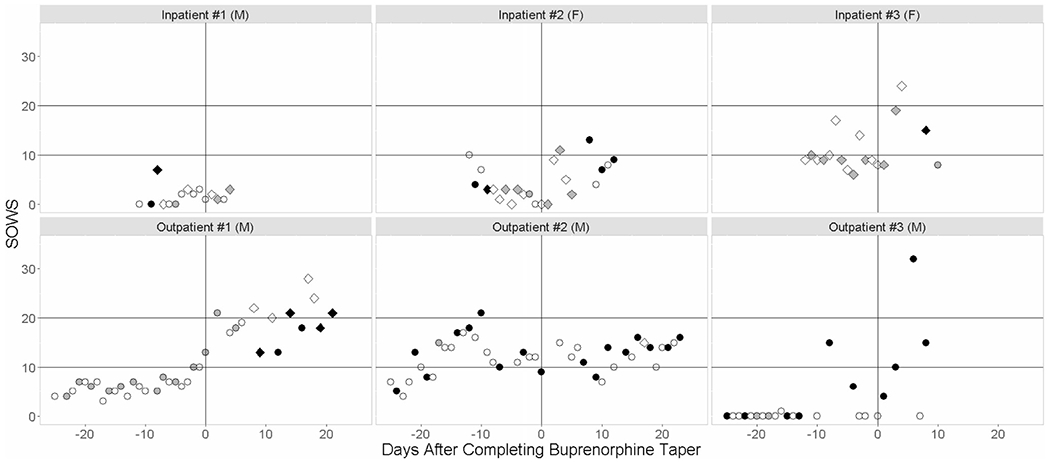
Time trends in SOWS scores with rescue-medication use and urine opioid results for participants receiving pioglitazone (3 inpatients, 3 outpatients). The time points in the figure represent the portion of the study during which participants were receiving pioglitazone. The duration of the buprenorphine taper was 28 days for participants enrolled in the initial outpatient study design, and 13 days for participants enrolled in the subsequent inpatient study design. The color of the marker indicates opioid positivity (positive = black, negative = gray, not tested = white) while marker shape indicates use of adjunct medications (diamond = yes, circle = no). Participant sex (F = female, M = male) is indicated in parentheses
Fig. 3.
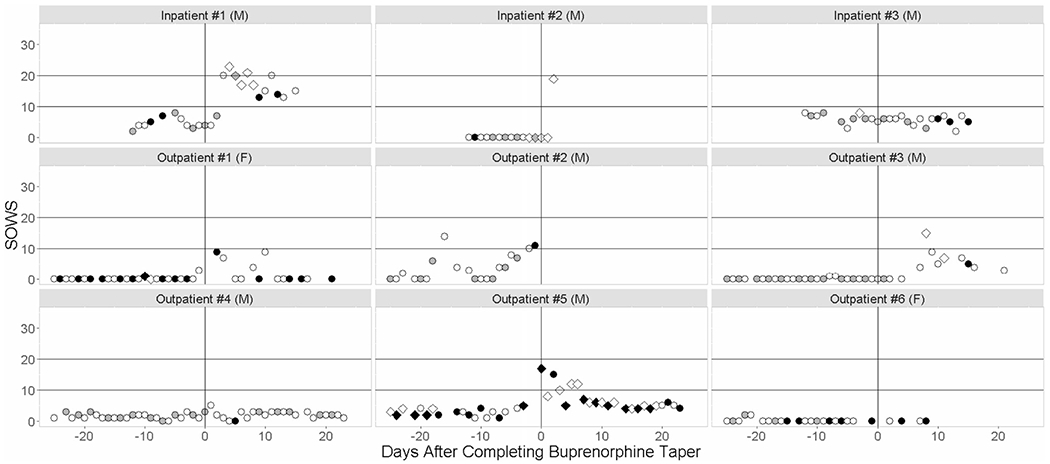
Time trends in SOWS scores with rescue-medication use and urine opioid results for participants receiving placebo (3 inpatients, 6 outpatients). The time points in the figure represent the portion of the study during which participants were receiving pioglitazone placebo. The duration of the buprenorphine taper was 28 days for participants enrolled in the initial outpatient study design, and 13 days for participants enrolled in the subsequent inpatient study design. The color of the marker indicates opioid positivity (positive = black, negative = gray, not tested = white) while marker shape indicates use of adjunct medications (diamond = yes, circle = no). Participant sex (F = female, M = male) is indicated in parentheses
For SOWS, there was no main effect of pioglitazone, whether the time frame was the whole study (F1,624 = 0.14, p = 0.71) or the taper phase only (F1,273 = 1.18, p = 0.28). There were significant effects of time and significant pioglitazone-by-time interactions: in the model for the whole study, these were the effect of taper (F1,624 = 8.87, p = 0.003), post-taper (F1,624 = 5.38, p = 0.021), pioglitazone-by-taper (F1,624 = 13.66, p = 0.0002), and pioglitazone-by-post-taper (F1,624 = 45.46, p < 0.0001); in the model for taper phase only, these were the effect of taper day (F1,273 = 4.86, p = 0.028) and pioglitazone-by-day (F1,273 = 4.27, p = 0.04). The regression coefficients for the interaction terms provide the magnitude of the difference in SOWS scores for the medication groups, after adjusting for rescue-medication use and study iteration. The SOWS score for the pioglitazone group was 2.99 ± 0.81 points higher during the taper phase and 6.19 ± 0.92 points higher during the post-taper phase. The difference in slopes during the taper phase was an increase of 0.088 ± 0.043 points per day.
For COWS, there was again no main effect of pioglitazone for the whole study (F1,645 = 0, p > 0.99) or for the taper phase only (F1,274 = 0.16, p = 0.69). In the model for the whole study, there was a significant effect of post-taper phase (F1,645 = 24.02, p < 0.0001), but no significant effect of taper phase or any significant pioglitazone-by-phase interactions. The regression coefficient for post-taper phase was 1.10 ± 0.23, indicating that the COWS score was higher in the post-taper phase than before the taper began, after adjusting for rescue-medication use and study iteration. In the model for the taper phase alone, the main effect of taper day was statistically significant (F1,274 = 8.05, p = 0.0049), but there was no significant pioglitazone-by-day interaction. The regression coefficient for taper day was −0.031 ± 0.018, indicating that COWS decreased daily during the taper phase, after adjusting for rescue-medication use and study iteration.
Use of rescue medications for opioid withdrawal
Of the six participants in the pioglitazone arm, 50% needed rescue medications during the buprenorphine taper and 83.3% needed them after the taper. In the placebo arm, 60% (6/10) of participants needed rescue medications during the buprenorphine taper, and 50% (4/8) needed them after the taper. At this by-person summary level, there were no statistically significant differences between treatment arms within either study phase.
In the repeated-measures model for the whole study, the main effects of pioglitazone (F1,667 = 1.60, p = 0.21) and taper phase were not statistically significant (F1,667 = 1.73, p = 0.19) but there was a significant main effect of post-taper phase (F1,667 = 13.57, p = 0.0002) as well as significant interactions for pioglitazone-by-taper (F1,667 = 4.52, p = 0.034) and pioglitazone-by-post taper (F1,667 = 4.55, p = 0.033). The regression coefficients for both the main effect of post-taper phase (2.06 ± 0.56) and for the pioglitazone-by-post interaction (2.82 ± 1.32) were significantly greater than zero, indicating that rescue-medication use was greater in the post-taper phase than in the pre-taper phase (as would be expected), and that this increase was greater in the pioglitazone arm than in the placebo arm.
In the repeated-measures model limited to the taper phase, there were no significant effects of pioglitazone, taper day, or pioglitazone-by-day interaction.
Opioid use—urine toxicology
The mean percentage of opioid-positive urines during the post-taper period was 57.50 ± 41.68 for the pioglitazone arm and 58.85 ± 37.50 for the placebo arm. Repeated-measures logistic regression was used to test the hypothesis of treatment differences in opioid-positive urine specimens during the post-taper period. This analysis was limited to 14 participants for whom urine data were available during this phase (6 in the pioglitazone arm, 8 in the placebo arm). The model consisted only of a single independent variable, treatment arm. There was no statistically significant effect of treatment arm (F1,64 = 0.01, p = 0.91), indicating that the arms did not differ in opioid use following the buprenorphine taper.
Pioglitazone and markers of inflammation
Concentrations of the proinflammatory cytokines MCP-1, IL-1 beta, IL-6, IL-10, and TNF-alpha were measured once in CSF and plasma in nine participants: four in the pioglitazone arm and five in the placebo arm. Three biomarkers (IL-1 beta in both CSF and plasma, and TNF-alpha in CSF) were below the detection limit in more than half the samples and were excluded from treatment comparisons.
Plasma levels of IL-10 were higher in the pioglitazone arm than in the placebo arm (t7 = −2.58, p = 0.037); plasma levels of TNF-alpha also tended to be higher in the pioglitazone arm (t7 = −2.22, p = 0.062) (Table 2).
Table 2.
Levels of proinflammatory cytokines in CSF and plasma by treatment arm
| Cytokine | Pioglitazone (N = 4) 2/4 (50%) women |
Placebo (N = 5) 0/5 (0%) women |
||
|---|---|---|---|---|
| Mean ± SDa | Individual valuesb | Mean ± SDa | Individual valuesb | |
| CSF | ||||
| MCP-1 | 384.0 ± 40.5 | 346, 356, 401, 433 | 344.8 ± 62.2 | 287, 313, 324, 352, 448 |
| IL-1 beta | All <0.14 | All <0.14 | ||
| IL-6 | 1.20 ± 0.44 | 0.84, 0.97, 1.17, 1.82 | 2.11 ± 1.82 | 0.52, 0.97, 1.84, 1.84, 2.05, 5.18 |
| IL-10 | 0.16 ± 0.03 | 0.12, 0.15, 0.16, 0.2 | 0.18 ± 0.03 | 0.13, 0.18, 0.19, two 0.2 |
| TNF-alpha | Two <0.09, 0.14, 0.17 | Three <0.09, 0.1, 0.2 | ||
| Plasma | ||||
| MCP-1 | 195.0 ± 53.6 | 118, 199, 229, 234 | 165.4 ± 29.0 | 125, 156, 167, 174, 205 |
| IL-1 beta | Three < 0.14, 0.22 | Four < 0.14, 0.14 | ||
| IL-6 | 0.83 ± 0.42 | 0.31, 0.73, 0.96, 1.31 | 0.95 ± 0.74 | 0.31, 0.64, 0.67, 0.89, 2.22 |
| IL-10c | 0.68 ± 0.16 | 0.51, 0.63, 0.71, 0.88 | 0.45 ± 0.12 | 0.26, 0.45, 0.46, 0.48, 0.59 |
| TNF-alphad | 3.13 ± 1.06 | 2.19, 2.75, 2.92, 4.64 | 1.92 ± 0.55 | 1.45, 1.57, 1.81, 1.95, 2.84 |
Summary statistics were not calculated when 50% or more of samples were below the detection limit
Individual participant values are shown in ascending order
Higher in the pioglitazone arm than in the placebo arm (t7 = −2.58, p = 0.037)
Higher in the pioglitazone arm than in the placebo arm (t7 = −2.22, p = 0.062)
There were several large and statistically significant correlations between cytokines and withdrawal scores, without respect to medication group assignment. SOWS was positively correlated with MCP-1 levels in both CSF (r = 0.70, p = 0.038) and plasma (r = 0.77, p = 0.015), and COWS was positively correlated with plasma levels of TNF alpha (r = 0.68, p = 0.044). Cytokine levels were not related to opioid use, cigarette consumption, race, or sex.
Discussion
Results from this small randomized clinical trial provide, at best, no evidence that pioglitazone prevents opioid-withdrawal symptoms during a taper from buprenorphine. This study was hindered by poor enrollment, premature termination and a very small sample size, which makes analysis of data and interpretation of results problematic. Only six participants received at least one dose of pioglitazone and could be included in the analyses of primary outcomes, which was far fewer than planned sample size of 40 evaluable participants per group. Despite these limitations, findings from this study warrant publication. First, it offers compelling evidence that promising results from a small, open-label case series that found pioglitazone to be an effective add-on treatment for patients undergoing taper from agonist maintenance therapy are not reproducible. Second, this study is one of very few published studies of the effects of pioglitazone on opioid withdrawal in humans; most investigations of pioglitazone as a potential treatment in substance use disorders have focused on other drugs of abuse such as nicotine (Jones et al. 2017), alcohol (Blednov et al. 2015), or cocaine (Schmitz et al. 2017) or been performed in rodents (Stopponi et al. 2011, 2013, Miller et al. 2018). Third, these findings add to the growing body of work that neuroinflammatory processes contribute to opioid tolerance, dependence, and withdrawal.
A paradoxical effect of pioglitazone was observed: SOWS scores were higher in the pioglitazone arm than in the placebo arm during both the taper and withdrawal phases of the study, and the need for rescue medications after the taper was also higher in the pioglitazone arm than in the placebo arm. We acknowledge that the small sample size could have led to an erroneous finding that might not have been apparent had the study recruited the desired number of participants. Multiple studies have demonstrated that pioglitazone attenuates opioid withdrawal symptoms in rodents (de Guglielmo et al. 2017; Ghavimi et al. 2014, 2015); however, negative findings for pioglitazone are not without precedent in the literature. Despite the small size of our study, we can confidently conclude that we did not replicate the dramatically good results of the open-label case series that preceded it (Ciccocioppo, unpublished data).
Since we designed this clinical trial in 2011, one unexpected negative result for the use of pioglitazone has been documented in the preclinical literature. Javadi et al. (2013), using a procedure in which pioglitazone (at doses ranging from 2.5 to 20 mg/kg) was co-administered daily with morphine, found that this co-administration exacerbated, rather than reduced, naloxone-precipitated withdrawal in mice. This exacerbation was prevented by inhibition of nitric oxide synthase (NOS), leading the authors to conclude pioglitazone was activating the nitric oxide/guanylyl cyclase/cyclic guanosine monophosphate (NO/GC/cGMP) pathway. In addition, a laboratory study in humans showed that 45 mg pioglitazone did not change the subjective effects of oxycodone in nondependent opioid users (Jones et al. 2016). The authors suggested that the pioglitazone dose given, though sufficient to treat diabetes, may not be sufficient to suppress glial release of proinflammatory cytokines, and their sample of nondependent opioid users may not have been responsive to pioglitazone due to a floor effect as opioid-dependent users may have higher tonic levels of glial activity for pioglitazone to suppress. Our findings support the first of those explanations: a 45 mg/day dose of pioglitazone was not sufficient to reduce levels of proinflammatory cytokines in either CSF or plasma in our opioid-dependent sample. Another possible explanation for our negative findings is that the effects of pioglitazone for attenuating opioid withdrawal, while well-documented in rodents, may not generalize to humans. Species-specific differences in the actions of PPARγ agonists may account for the results observed in our study.
Our study found that levels of proinflammatory cytokines were correlated with withdrawal-symptom severity, and adds to the accumulating body of work that neuroinflammatory processes contribute to opioid tolerance, dependence, and withdrawal. This may reflect more general mechanisms because the correlation between MCP-1 levels and withdrawal-symptom severity is consistent with a prior report of elevated MCP-1 levels in the CSF of alcohol-dependent patients undergoing withdrawal (Umhau et al. 2014).
The main strength of our study, in each of its iterations, was its randomized, placebo-controlled design. Additionally, we were able to assess and demonstrate the safety of pioglitazone and buprenorphine co-administration (see supplementary data). The adverse events reported by participants in our study were mild, and safety-monitoring measures were within normal range. Because alleviation of withdrawal symptoms in patients with OUDs undergoing agonist taper is a novel use of pioglitazone, there are no other clinical data demonstrating the safety of these medications given in combination.
Our study’s primary limitation was its small sample size. Due to slow enrollment, the study’s Data and Safety Monitoring Board (DSMB) conducted a futility analysis, which showed that that the effect sizes observed to date were substantially smaller than the anticipated effect size on which the required sample size of 80 completers was based, and that the required sample sizes for adequate (80%) power for these smaller effect sizes were quite large, exceeding 300 participants per treatment arm. Based on these findings, we terminated the study. An additional limitation was that the primary outcome was originally treatment response (defined as abstinence from opioids and not requiring rescue withdrawal medication). The low rates of abstinence from opioids observed during the study’s initial outpatient design made this outcome infeasible. Participants’ continued use of opioids during the outpatient portion of the study lessened the validity of the withdrawal measures taken during this phase of the study.
Because of these limitations, and because we did not test pioglitazone doses higher than 45 mg/day, we cannot state categorically that pioglitazone is ineffective as an aid to opioid taper. However, we can conclude that pioglitazone at 45 mg/day did not perform as expected based on results from preclinical and clinical studies.
Supplementary Material
Acknowledgments
Funding This study was supported by the Intramural Research Program of the National Institute on Drug Abuse, National Institutes of Health, and the Swedish Research Council.
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
References
- Berger J, Moller DE (2002) The mechanisms of action of PPARs. Annu Rev Med 53:409–435 [DOI] [PubMed] [Google Scholar]
- Bland ST, Hutchinson MR, Maier SF, Watkins LR, Johnson KW (2009) The glial activation inhibitor AV411 reduces morphine-induced nucleus accumbens dopamine release. Brain Behav Immun 23:492–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blednov YA, Benavidez JM, Black M, Ferguson LB, Schoenhard GL, Goate AM, Edenberg HJ, Wetherill L, Hesselbrock V, Foroud T, Harris RA (2015) Peroxisome proliferator-activated receptors α and γ are linked with alcohol consumption in mice and withdrawal and dependence in humans. Alcoholism: Clinical and Experimental Research 39:136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Guglielmo G, Kallupi M, Scuppa G, Demopulos G, Gaitanaris G, Ciccocioppo R (2017) Pioglitazone attenuates the opioid withdrawal and vulnerability to relapse to heroin seeking in rodents. Psychopharmacology 234:223–234 [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Schottenfeld RS, Cutter CJ, Moore BA, Barry DT, O’Connor PG (2014) Primary care-based buprenorphine taper vs maintenance therapy for prescription opioid dependence: a randomized clinical trial. JAMA Intern Med 174:1947–1954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghavimi H, Hassanzadeh K, Maleki-Dizaji N, Azarfardian A, Ghasami S, Zolali E, Charkhpour M (2014) Pioglitazone prevents morphine antinociception tolerance and withdrawal symptoms in rats. Naunyn Schmiedeberg’s Arch Pharmacol 387:811–821 [DOI] [PubMed] [Google Scholar]
- Ghavimi H, Azarfardian A, Maleki-Dizaji N, Hassanzadeh K, Ghanbarzadeh S, Charkpour M (2015) Acute administration of pioglitazone attenuates morphine withdrawal syndrome in rat: a novel role of pioglitazone. Drug Res (Stuttg) 65:113–118 [DOI] [PubMed] [Google Scholar]
- Gossop M (2006) Medically supervised withdrawal as stand-alone treatment? In: Strain EC, Stitzer ML (eds) The treatment of opioid dependence. The Johns Hopkins University Press, Baltimore, pp 346–362 [Google Scholar]
- Handelsman L, Cochrane KJ, Aronson MJ, Ness R, Rubinstein KJ, Kanof PD (1987) Two new rating scales for opiate withdrawal. Am J Drug Alcohol Abuse 13:293–308 [DOI] [PubMed] [Google Scholar]
- Hutchinson MR, Bland ST, Johnson KW, Rice KC, Maier SF, Watkins LR (2007) Opioid-induced glial activation: mechanisms of activation and implications for opioid analgesia, dependence, and reward. Scientific World Journal 7:98–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson MR, Lewis SS, Coats BD, Skyba DA, Crysdale NY, Berkelhammer DL, Brzeski A, Northcutt A, Vietz CM, Judd CM, Maier SF, Watkins LR, Johnson KW (2009) Reduction of opioid withdrawal and potentiation of acute opioid analgesia by systemic AV411 (ibudilast). Brain Behav Immun 23: 240–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasinski DR, Johnson RE, Kocher TR (1985) Clonidine in morphine withdrawal: differential effects on signs and symptoms. Arch Gen Psychiatry 42:1063–1066 [DOI] [PubMed] [Google Scholar]
- Javadi S, Ejtemaeimehr S, Keyvanfar HR, Moghaddas P, Aminian A, Rajabzadeh A, Mani AR, Dehpour AR (2013) Pioglitazone potentiates development of morphine-dependence in mice: possible role of NO/cGMP pathway. Brain Res 1510:22–37 [DOI] [PubMed] [Google Scholar]
- Jones JD, Sullivan MA, Manubay JM, Mogali S, Metz VE, Ciccocioppo R, Comer SD (2016) The effects of pioglitazone, a PPARgamma receptor agonist, on the abuse liability of oxycodone among nondependent opioid users. Physiol Behav 159:33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Comer SD, Metz VE, Manubay JM, Mogali S, Ciccocioppo R, Martinez S, Mumtaz M, Bisaga A (2017) Pharmacol Biochem Behav 163:90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P, Kaundal RK, More S, Sharma SS (2009) Beneficial effects of pioglitazone on cognitive impairment in MPTP model of Parkinson’s disease. Behav Brain Res 197:398–403 [DOI] [PubMed] [Google Scholar]
- Lin SL, Tsai RY, Tai YH, Cherng CH, Wu CT, Yeh CC, Wong CS (2009) Ultra-low dose naloxone upregulates interleukin-10 expression and suppresses neuroinflammation in morphine-tolerant rat spinal cords. Behav Brain Res 207:30–36 [DOI] [PubMed] [Google Scholar]
- Liu L, Gao XJ, Ren CG, Hu JH, Liu XW, Zhang ZW, Fu ZJ (2017) Monocyte chemoattractant protein-1 contributes to morphine tolerance in rats with cancer-induced bone pain. Exp Ther Med 13:461–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda T, Kiguchi N, Fukazawa Y, Yamamoto A, Ozaki M, Kishioka S (2007) Peroxisome proliferator-activated receptor gamma activation relieves expression of behavioral sensitization to methamphetamine in mice. Neuropsychopharmacology 32:1133–1140 [DOI] [PubMed] [Google Scholar]
- Miller WR, Fox RG, Stutz SJ, Lane SD, Denner L, Cunningham KA, Dineley KT (2018) PPARP agonism attenuates cocaine cue reactivity. Addiction Biology 23(1):55–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz JM, Green CE, Hasan KM, Vincent J, Suchting R, Weaver MF, Moeller FG, Narayana PA, Cunningham KA, Dineley KT, Lane SD (2017) PPAR-gamma agonist pioglitazone modifies craving intensity and brain white matter integrity in patients with primary cocaine use disorder: a double-blind randomized controlled pilot trial. Addiction 112:1861–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song LC, Song C, Zeng J, Xiong ML, Lou N (2002) Reduction in monocyte chemoattractant protein-1 mRNA expression in peripheral blood mononuclear cells of diamorphine addicts. Acta Pharmacol Sin 23:336–338 [PubMed] [Google Scholar]
- Stopponi S, Somaini L, Cippitelli A, Cannella N, Braconi S, Kallupi M, Ruggeri B, Heilig M, Demopulos G, Gaitanaris G, Massi M, Ciccioppo R (2011) Biological Psychiatry 69:642–649. [DOI] [PubMed] [Google Scholar]
- Stopponi S, de Guglielmo G, Somaini L, Cippitelli A, Cannella N, Kallupi M, Ubaldi M, Heilig M, Demopulos G, Gaitanaris G, Ciccocioppo R (2013) Activation of PPARγ by pioglitazone potentiates the effects of naltrexone on alcohol drinking and relapse in msP rats. Alcoholism: Clinical and Experimental Research 37: 1351–1360. [DOI] [PubMed] [Google Scholar]
- Umhau JC, Schandt M, Solomon MG, Yuan P, Nugent A, Zarate CA, Drevets WC, Hall SD, George DT, Heilig M (2014) Cerebrospinal fluid monocyte chemoattractant protein-1 in alcoholics: support for a neuroinflamatory model of chronic alcoholism. Alcohol Clin Exp Res 38:1301–1306 [DOI] [PubMed] [Google Scholar]
- Watkins LR, Hutchinson MR, Rice KC, Maier SF (2009) The “toll” of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia. Trends Pharmacol Sci 30:581–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesson DR, Ling W (2003) The Clinical Opiate Withdrawal Scale (COWS). J Psychoactive Drugs 35:253–259 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


