Abstract
Introduction:
Enhanced visual effects, like animation, have the potential to improve comprehension of probabilistic risk information, particularly for those with lower health literacy. We tested the effect of presentation format on comprehension of colorectal cancer (CRC) screening probabilities to identify optimal risk communication strategies.
Methods:
Participants from a community foodbank and a cancer prevention center were randomized to 1 of 3 CRC screening risk presentations. The presentations used identical content, but varied in format: 1) video with animated pictographs, 2) video with static pictographs, and 3) audiobooklet with static pictographs. Participants completed pre- and post- presentation surveys. The primary outcome was knowledge of probability/risk information regarding CRC screening, calculated as total, verbatim, and gist scores.
Results:
187 participants completed the study and were included in this analysis. Median age was 58 years (Interquartile Range [IQR]: 14 years), most participants were women (63%), and almost half had a high school education or less (46%). Approximately one quarter had inadequate health literacy (S-TOFHLA marginal/inadequate: 28%; Brief Health Literacy Screener low: 18%) and about one half had low numeracy (Subjective Numeracy Scale low: 54%; Graphical Literacy Measure low: 50%). We found no significant differences in total, verbatim, or gist knowledge across presentation formats (all p > 0.05).
Discussion:
Use of an animated pictograph to communicate risk does not appear to augment or impede knowledge of risk information. Regardless of health literacy level, difficulty understanding pictographs presenting numerical information persists. There may be a benefit to teaching or priming individuals on how to interpret numerical information presented in pictographs before communicating risk using visual methods.
Trial Registry:
INTRODUCTION
Understanding and applying probabilities and risk information is an essential part of making informed healthcare decisions.1 An informed decision occurs when the patient has an adequate understanding of the health condition, treatment options, and benefits and harms, and the decision is consistent with the patients’ personal values.1–4 Knowledge, values, attitudes and behavior are integral features of an informed decision; yet, knowledge is one of the most important indicators of informed decision making.4,5 To enhance understanding, when communicating probabilities to patients, evidence supports using natural frequencies and illustrations (e.g., cartoons, bar charts, pictographs).6,7 Moreover, structured, tailored or interactive communication tools can increase patient knowledge.6,7 These strategies are particularly important for those with low health literacy.1
Health literacy is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”8 It is estimated that approximately half (50%) of adults in the United States (US) demonstrate health literacy related challenges and over one-third (36%) demonstrate skills that are consistent with basic or below basic health literacy.9 Skills like retaining and applying specific numerical information, presenting information visually (e.g., graphs), and using technology to access information all contribute to one’s health literacy.10 Numeracy, defined as how comfortable one is with numeric information, is a critical component of health literacy in risk information processing.11 Thus, individuals with low health literacy may have a diminished capacity to understand risk information. In addition, these individuals are often less aware of preventive services, like cancer screening. Combined, these may inhibit their ability to make informed cancer screening decisions.1 Optimal strategies to communicate risk information in the context of cancer screening are needed.
In a review of computer-based visual presentations of risk information by Stellamanns and colleagues,12 static graphical depictions were found to improve comprehension, yet the results were inconsistent across studies. In the case of dynamic depictions, the authors found that additional evaluation is needed among those with limited numeracy and graphical literacy to make a determination about theimpact on risk communication.12 Recommendations exist for presenting risk information to those with low numeracy (e.g., plain language, absolute risk, incremental risk, pictographs, presentation of only critical information, and time interval for risk occurrence).13 However, strategies for optimal risk communication are also lacking. Moreover, Hawley et al.14 found that viewing pictographs resulted in adequate gist and verbatim risk knowledge in those with low numeracy, and the information was considered more trustworthy by those with high or low numeracy. In addition, Tait et al.15 found that regardless of numeracy levels, pictographs significantly increased both gist and verbatim knowledge and were better accepted by patients when compared to text and tables. Therefore, using dynamic depictions like animation in combination with pictographs may be an effective risk communication strategy for those with low health literacy.
Communication tools designed for various health conditions have used pictographs in multiple ways; for example, computer-generated graphics accompanied by text, voice narration, or both;16–18 animated icon arrays;19,20 interactive games;21 risk calculators;22 and the use of personalized, animated avatars.23 While a number of these interventions were successful in reducing decisional conflict,16 increasing risk perception and intentions,23 and eliciting emotional responses to risk messages,21 few studies have measured patient recall, and their results are mixed.18,19,24,25 Additionally, few animated interventions have been developed specifically for low health literacy populations.26–28
With the goal of improving risk communication among low health literacy populations, we developed a decision aid for colorectal cancer (CRC) screening suitable for those with low health literacy in 3 formats: an audiobooklet, a video with static images and a video with animated images. The objectives of this investigation were to: 1) adapt an existing decision aid for 3 strategies for communicating probabilities, 2) test their effectiveness in increasing patient understanding of risk information, and 3) examine the intervention effects by health literacy levels.
METHODS
Study Participants
Participants for this randomized controlled trial were recruited from 2 sites in Houston, Texas: 1) The Cancer Prevention Center at The University of Texas MD Anderson Cancer Center and 2) Bethel’s Heavenly Hands. These settings were selected to recruit those with a broad range of health literacy levels. The Cancer Prevention Center serves approximately 23,000 patients per year and provides cancer screening, cancer risk assessments, and other cancer prevention programs. Patients can make their own appointments or can be referred by physicians. Bethel’s Heavenly Hands is a non-profit organization assisting individuals with food, clothing, shelter, and medical care. Bethel’s Heavenly Hands serves approximately 5,500 people monthly through their food pantry service.
Men and women aged 45–75 years who were English speakers were eligible to participate. Individuals that reported a previous diagnosis of colorectal cancer were excluded. At the Cancer Prevention Center, participants were recruited in November and December, 2012. Trained research assistants approached men and women in the center’s waiting room and invited them to participate in the study. Participants completed the study either immediately or after their appointments at the center. At Bethel’s Heavenly Hands, individuals were invited to participate during weekly food assistance service between December 2012 and January 2013. Participants completed the study immediately or were invited to return the following week if they did not have time to complete it the same day.
The Institutional Review Board at The University of Texas MD Anderson Cancer Center approved the study protocol and consent process.
Randomization and Study Procedures
After potential participants were screened for eligibility and consented, research assistants administered a baseline survey. All participants then viewed a 3:51 minute introductory video that introduced colorectal cancer screening and 3 screening tests: fecal occult blood test, flexible sigmoidoscopy, and colonoscopy. Next, participants were randomized using a double-blind procedure to 1 of 3 intervention arms, as indicated in a sealed randomization assignment envelope: 1) audiobooklet with static pictographs; 2) video with static pictographs; or 3) video with animated pictographs (Table 1). We used computer generated, permuted-block randomization per study site with a block size of 3 and an allocation ratio of 1:1. After randomization, participants viewed the corresponding intervention. The audiobooklet ran for 3:54 (7:45 total minutes), the static video ran for 3:20 (7:11 total minutes), and the animated video ran for 3:22 (7:13 total minutes). Research assistants then administered post-surveys. All participants received a $30 gift card for participating. Participants at the Cancer Prevention Center were also compensated for their parking expenses.
Table 1.
Description and comparison of colorectal cancer screening decision aid intervention arms
| Feature | Audiobooklet | Static Video | Animated Video |
|---|---|---|---|
| Description | Booklet with accompanying narration | FIMDM patient decision aid video | FIMDM patient decision aid with animation features |
| Introduction/Overview with Risk Communication | Addresses 3 questions: 1) How many people get colorectal cancer in their lifetime? 2) How many will die from colorectal cancer? 3) How many will be saved by screening? |
Same | Same |
| Voice-over Narration | Yes | Yes | Yes |
| Risk Presentation | Pictographs | Pictographs | Pictographs |
| Animation | None | Minimal (overlay reinforcing information) | Enhanced (animation highlights the randomness of affected individuals) |
| Time (minutes) | |||
| Introduction Time | 3:51 | 3:51 | 3:51 |
| Intervention Time | 3:54 | 3:20 | 3:22 |
| Total Time | 7:45 | 7:11 | 7:13 |
Note: Abbreviation: FIMDIM=Foundation for Informed Medical Decision Making.
Intervention Development
Our initial aim was to develop a decision aid by identifying the essential tasks patients perform in order to understand probabilistic health information and use the information to make informed, quality decisions. To this end, our research team reviewed relevant empirical literature and identified essential probabilistic information a patient needs to understand to interpret the magnitude of risks and benefits. (Appendix Table 1). This probabilistic information included: 1) the relevant group, 2) the denominator, 3) the numerator, 4) the time frame, 5) the incremental benefit, 6) rare events, and 7) uncertainty with risk estimates. Our strategies for intervention design were based on these tasks. To further support our development approach, we referred to existing literature to understand what attributes of screening tests patients consider important while making a decision.15,29–31 Based on these reviews, we identified animated visual cues (e.g., highlighting, flashing, movement) as a strategy to enhance attention to these essential tasks.
To incorporate visual cues into our intervention development, we reviewed an existing CRC screening decision aid (booklet and video) developed by the Foundation for Informed Medical Decision Making and distributed by Health Dialog.32 We studied the probabilities communicated by the aid including incidence and mortality information about colorectal cancer, screening for CRC, and different tests and their advantages and disadvantages. Based on this research, we developed risk communication modules to communicate risk estimates about colorectal cancer and CRC screening. A risk communication expert panel, made up of clinicians and researchers, reviewed these modules and provided feedback based on their clinical perspective and expertise.
We edited the original 30-minute Health Dialog video down to 3:51 minutes to reduce patient burden and adapted it for a low health literacy audience; changing language to 8th grade reading level from 9th-11th grade level by bulleting the text, adding new pictographs, simplifying by removing information on testing options not usually available to low-literacy populations in Houston, TX (e.g., imaging tests), and eliminating patient and physician vignettes. This version of the video was used to enhance understanding of CRC screening introductory concepts among all participants.
Next, we created a prototype of an animated video to communicate the elements of our risk communication modules (i.e. incidence, incremental benefit, and efficacy of detecting cancer per screening test). The video presented information via bulleted text, graph and static images (i.e., pictographs), with voice-over narration. Finally, we developed 2 other versions of this video for comparison: a version with static images, and a print booklet with an audio narration track.
Cognitive Testing of the Animated Prototype
We conducted 3 rounds of in-person cognitive interviews with eligible individuals at increased risk for low numeracy and low health literacy (n=20). We included English-speaking men and women aged 45 to 75 years with no history of colorectal cancer. All participants first watched an introductory video on CRC screening. They then watched and evaluated the animated video prototype in terms of appearance, layout, and color. Their understandability of the graphics, animation, and narration describing probabilistic information was assessed by interviews, which lasted 45–60 minutes. We changed and improved the video iteratively after each iteration. The updated animated prototype was sent to the expert panel for a final review.
Final Products
One of our final products consisted of a short introductory video (3:51 minutes): an on-screen narrator who introduced screening, CRC, and recommendations for regular screening. The narrator briefly described colon anatomy and polyps, with accompanying graphics. Next, the video introduced 3 CRC screening tests: fecal occult blood test (FOBT), sigmoidoscopy, and colonoscopy. Using a combination of narrative, text, and minimal graphics, the video gave a brief description of each test procedure, its advantages, an explanation of test results, and recommended testing frequency. It also informed the patient about what to expect before, during, and after each test, including sedation: colon preparation, potential discomfort or unpleasantness, and time commitments. All participants viewed the introductory video and CRC risk information.
Participants were then randomized into viewing 1 of our 3 other final products with the same basic content, i.e., 1 of our 3 planned interventions: the audiobooklet, the static video, or the animated video (Table 1).
The first intervention, the audiobooklet, consists of ten pages, plus front and back covers, and has exactly the same content, text and graphics as the videos. The audio-track is also the same narrative, with a prompt at the end of each page asking the patient to turn to the next page.
The second intervention, the static video, presents CRC risk information. After recapitulating the introductory video, it puts forth and then addresses 3 questions sequentially: 1) how many people get colorectal cancer in their lifetime? (incidence); 2) how many will die from colorectal cancer? (mortality); and 3) how many will be saved by screening? (mortality benefit). Static images begin with an icon array of 100 images depicting “smiley” faces (Figure 2), which represents a random sample of 100 persons in the US. Differing from the audiobooklet, as the narration advances in the static video, the icon colors change to depict the percentage of people who will get CRC, die from CRC, or be saved via early detection by screening. Images are presented without animation. The icons representing “affected” individuals are presented in a non-random manner (i.e., all in a row). A graph explains that the risk of colorectal cancer increases with age, and the benefit of CRC screening decreases after age 75 years. The video also contains text, which gives information about the recommended age for CRC screening, states that it can detect cancer early and advises the patient to talk to their doctor about CRC screening.
Figure 2. Images of Risk Concepts, Task Descriptions and Multimedia Strategies for Displaying Risk Estimates.
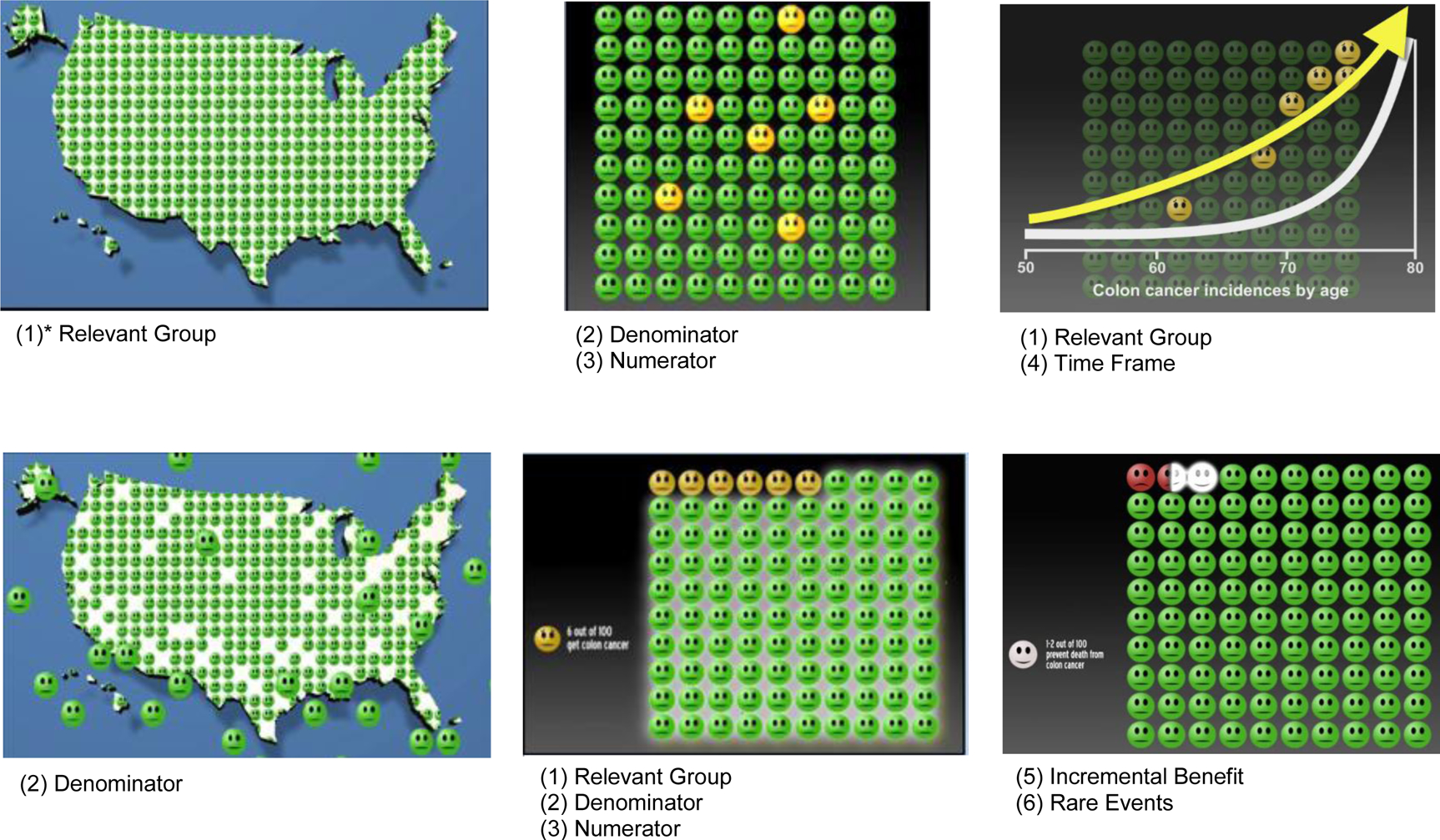
Images of the Risk Concepts, Task Descriptions and Multimedia Strategies for Displaying Risk Estimatesdescribed in Appendix 1.
*Note: These numbers refer to the tasks described in Appendix Table 1.
The third intervention, the animated video, has the same basic content and narration as the static video, with the addition of enhanced computer-generated animation: highlighting, flashing, and movement for emphasis. For example, the animation highlights the randomness of who is selected from the population and who is affected by the disease: the 6 yellow icons out of 100 representing “affected” individuals appear randomly among the other green icons and keep changing to different icons until the graphic finally settles on “highlighting” the top left 6 icons as “affected,” similar to the static video. For all presented questions, the particular group of icons discussed to answer those questions will flash and sometimes move forward for emphasis when the narrator talks about them. The video contains the same text as the static video, plus an animated version of the graph.
Study Measures
Baseline Measures
Participants completed a 3-item CRC screening indicator questionnaire and a 7-item CRC baseline knowledge questionnaire (Table 2).
Table 2.
Sociodemographic and baseline characteristics of the participants.
| Total | Audiobooklet | Static Video | Animated Video | |
|---|---|---|---|---|
| Sociodemographic Characteristics (N=187) | n (%) | n (%) | n (%) | n (%) |
| Age | ||||
| 45–59 years | 110 (58.8) | 34 (54.8) | 36 (58.1) | 40 (63.5) |
| 60–75 years | 77 (41.2) | 28 (45.2) | 26 (41.9) | 23 (36.5) |
| Gender (female) | 118 (63.1) | 40 (64.5) | 35 (56.5) | 43 (68.3) |
| Race/Ethnicity | ||||
| African American/Black | 131 (70.1) | 39 (62.9) | 45 (72.6) | 47 (74.6) |
| White | 38 (20.3) | 17 (27.4) | 11 (17.7) | 10 (15.9) |
| Hispanic/Latino | 7 (3.7) | 1 (1.6) | 4 (6.5) | 2 (3.2) |
| Other/Mixed | 11 (5.9) | 5 (8.1) | 2 (3.2) | 4 (6.2) |
| Education (n=185) | ||||
| Less than High School | 36 (19.5) | 11 (18.3) | 15 (24.2) | 10 (15.9) |
| High School Graduate | 49 (26.5) | 11 (18.3) | 16 (25.8) | 22 (34.9) |
| Some College | 68 (36.8) | 24 (40.0) | 23 (37.1) | 21 (33.3) |
| College Degree or More | 32 (17.3) | 14 (23.3) | 8 (12.9) | 10 (15.9) |
| Study site | ||||
| BHH | 122 (65.2) | 40 (64.5) | 41 (66.1) | 41 (65.1) |
| CPC | 65 (34.8) | 22 (35.5) | 21 (33.9) | 22 (34.9) |
| Health Literacy Measures* | ||||
| S-TOFHLA (marginal/inadequate) | 53 (28.3) | 11 (17.7) | 20 (32.3) | 22 (34.9) |
| BHLS: Brief Health Literacy Screener (low) | 34 (18.4) | 9 (14.8) | 17 (27.4) | 8 (12.9) |
| SNS: Subjective Numeracy Scale (low) | 100 (53.8) | 36 (58.1) | 34 (54.8) | 30 (48.4) |
| Graphical Literacy Measure (low) | 94 (50.3) | 33 (53.2) | 34 (54.8) | 27 (42.9) |
| CRC Screening Indicator Questions | ||||
| Heard of colon cancer screening?† (yes) | 161 (86.1) | 52 (83.9) | 54 (87.1) | 55 (87.3) |
| Screened for colon cancer?‡ (yes) | 93 (49.7) | 32 (51.6) | 29 (46.8) | 32 (50.8) |
| Plan to screen for colon cancer?§ (yes) | 166 (88.8) | 58 (93.6) | 51 (82.3) | 57 (90.5) |
| Baseline Knowledge | Mean (SD) n=186 | Mean (SD) n=61 | Mean (SD) n=62 | Mean (SD) n=63 |
| 7-item Knowledge of CRC Questionnaire‖ | 65.1 (22.0) | 69.1 (19.4) | 63.8 (21.8) | 62.4 (24.4) |
Note. Abbreviations: SD (standard deviation); BHH (Bethel’s Heavenly Hands); CPC (Cancer Prevention Center); CRC (colorectal cancer); S-TOFHLA (Short Test of Functional Health Literacy in Adults)
Cut-points derived from Housten et al., 201838
Before today, had you ever heard of colon cancer screening?
Have you ever been screened for colon cancer?
In the future, do you plan to get screened for colon cancer?
7-item CRC Knowledge Questionnaire: 1) Does your risk of colon cancer increase with age?; 2) Does smoking affect your chance of getting colon cancer?; 3) Does eating foods high in fiber reduce the risk of colon cancer?; 4) If one of your parents gets colon cancer, does it increase your chance of getting colon cancer?; 5) Are white people more likely to get colon cancer than Blacks of African-Americans?; 6) Can a person have colon cancer without having pain or other symptoms?; 7) Is there a test that can find colon cancer early?
Primary Outcomes: Total, Verbatim, and Gist CRC Screening Knowledge
Participants’ knowledge of colorectal cancer risks and benefits were measured on the post-intervention survey. Verbatim knowledge, or the ability to correctly identify specific probabilities, was evaluated by 5 questions pertaining to numbers and risk estimates referred to within the interventions.33 Gist knowledge was measured by 6 questions eliciting responses based on the participants’ overall understanding of the key messages in the interventions.33 Total knowledge was measured by combining the verbatim and gist knowledge questions, and adding 3 additional questions that were quantitative in nature, but without specific numeric information (14 total questions). Scores were assigned for each question; for analyses, the percentage of questions answered correctly was calculated to be used as the main outcome.
Health Literacy Measures
We used objective and subjective measures of health literacy to capture the multiple facets that make-up health literacy. We measured: health literacy, numeracy, and graphical literacy since they were most relevant to the developed interventions.
The Short Test of Functional Health Literacy in Adults (S-TOFHLA) is a health literacy measure made up of 36 items to be completed in 7 minutes. Scores range on a continuous scale from 0–36, based on the scoring system developed by Baker et al.34 Participants were classified into 3 levels based on their scores: “inadequate” (0–16), “marginal” (17–22) and “adequate” (23–36) health literacy. The “inadequate” and “marginal” categories were combined into 1 category, and were compared to “adequate” health literacy category in this analysis (inadequate/marginal vs. adequate).
The Brief Health Literacy Screener (BHLS) assess participants’ health literacy using 3 items with Likert-type response options ranging 1–5.35,36 Higher scores indicate higher health literacy. Scores on the 3 questions were summed to give an overall health literacy score ranging from 3–15. Participants with scores ≤9 were classified as “low” scores and >9 were “high” scores.37
Numeracy was measured using the 8-item Subjective Numeracy Scale (SNS) that asked participants to indicate their level of comfort with performing certain simple mathematical operations.11 Participants could choose a number ranging from 1–6 to indicate their comfort with numbers. The average of their responses to all 8 items was calculated to give their total subjective numeracy score (range 1–6). Participants with scores ≤4 were classified as “low” scores and >4 were “high” scores.38
The Graphical Literacy Measure (GLM)39 was used to assess participants’ understanding of visual depictions of information. The GLM asked participants to interpret graphical images using a 13-item questionnaire. Each correct answer received a score of 1, and each incorrect answer, a score of 0. The summed score for total graphical literacy was a continuous variable with possible scores ranging from 0–13. Participants with scores ≤6 were classified as “low” scores and >6 were “high” scores.38
Program Evaluation
To ensure the interventions materials were perceived as credible by the participants, we measured the perceived credibility using the following 5 questions adapted from Han et al.30: 1) How accurate does the information seem to you?; 2) How much do you trust the information presented in this program?; 3) How believable is the information presented in this program?; 4) How trustworthy is the information that was presented in this program; and 5) How reliable is the information that was presented in this program? Each question used a response format ranging from “Not at all” (0) to “Completely” (10). The credibility scale was summed to yield a range from 0 (lowest credibility) to 50 (highest credibility).
Hypothesis
We hypothesized that participants who viewed the video with animated pictographs, compared to participants who viewed the video with static pictographs or audiobooklet, would have higher total, verbatim, and gist knowledge scores. Secondarily, we hypothesized that the differences in knowledge scores between the 3 intervention arms would be greater for patients with lower health literacy than for patients with higher health literacy.
Statistical Analysis
Participants in the different intervention arms were compared for demographic differences at baseline. We evaluated the primary hypothesis using a regression model with an indicator of static versus animated group (the audiobook group was excluded from this analysis). Additional analyses with all three randomized groups were conducted (animated versus audiobook; static versus audiobook). Covariates were included in the model in a subsequent analysis. We used robust standard errors to protect against residual heterogeneity. For our secondary outcome, we modeled the primary outcome using indicator variable of treatments (animated versus static), the health literacy score, and their interaction.
RESULTS
All models met the assumptions for linear regression. Residual plots and histograms showed no patterns indicating lack of normality, linearity or homoscedasticity.
Demographic Characteristics
One hundred and eighty-seven participants completed the post-intervention survey and were included in these analyses. Participant characteristics are described in Table 2. A majority of the participants were female (63.1%), African-American/Black (70.1%) and between ages 45–59 years (58.8%). Approximately half (46.0%) of participants had a high school education or less. Few participants (13.9%) had never heard of CRC screening; however, half (49.7%) of participants had previously completed CRC screening and almost 90% said that they had plans to be screened in the future. Participants had moderate knowledge of CRC screening (mean score: 65.1% correct answers on baseline knowledge questionnaire).
Effect of Intervention Format on CRC Screening Knowledge
The intervention format (i.e., audiobooklet, static video, animated video) did not have a significant effect on the total, verbatim, or gist knowledge scores (Table 3). Participants in all 3 intervention arms had, on average, high gist knowledge (>70% correct answers), and moderately high total and verbatim knowledge (>50%). Analysis with all 3 randomized arms did not show any significant result in the comparison between audiobooklet vs. static video (mean [standard deviation]; audiobooklet: 66.8 [16.4] vs. static video: 62.0 [20.4]; p=0.15) or audiobooklet vs. animated video (audiobooklet: 66.8 [16.4] vs. animated video 65.0 [18.6]; p=0.56).
Table 3.
Knowledge scores between the 3 intervention groups (unadjusted).
| Intervention Group | P-values | |||||
|---|---|---|---|---|---|---|
| Total (n=187) | Audiobooklet (n=62) | Static Video (n=62) | Animated Video (n=63) | Audiobooklet vs. Static Video | Audiobooklet vs. Animated Video | |
| Knowledge Measures | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Total Score* | 64.6 (18.5) | 66.8 (16.4) | 62.0 (20.4) | 65.0 (18.6) | 0.15 | 0.56 |
| Verbatim Score† | 56.6 (22.7) | 58.3 (21.4) | 55.0 (23.7) | 56.6 (23.2) | 0.43 | 0.67 |
| Gist Score‡ | 75.2 (20.6) | 78.2 (16.7) | 71.2 (23.4) | 76.2 (20.7) | 0.06 | 0.55 |
Note. Abbreviations: SD (standard deviation).
Total Score: percent correct out of the total 14-items measuring knowledge.
Verbatim Score: percent correct out of 8-items pertaining to specific numbers and risk estimates referred to within the interventions.
Gist Score: percent correct out of 6-items pertaining to overall understanding of the key messages within the interventions.
Health Literacy Scores
A quarter of participants had inadequate health literacy (S-TOFHLA marginal/inadequate: 28.3%; BHLS low: 18.4%) and over half had limited numeracy (SNS low: 53.0%; GLM low: 50.3%). Mean scores for various health literacy and numeracy measures did not significantly differ by intervention arm when examining total and verbatim knowledge scores (Table 4). However, mean gist scores were significantly different for those who had adequate health literacy based on S-TOFHLA scores (audiobooklet mean: 81.4; static video mean: 74.2; animated video mean: 85.8; p=0.01). Additionally, there was no statistically significant interaction between health literacy and the 3 randomized study arms.
Table 4.
Comparison between health literacy levels and intervention group on knowledge scores.
| Audiobooklet | Static Video | Animated Video | P-values | ||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| Total Score | |||||||
| S-TOFHLA adequate | 51 | 69.8 (14.5) | 42 | 65.7 (19.1) | 41 | 71.6 (15.4) | .24 |
| S-TOFHLA inadequate/marginal | 11 | 53.3 (18.2) | 20 | 54.3 (21.2) | 22 | 52.6 (18.0) | .96 |
| BHLS high | 52 | 65.9 (16.4) | 45 | 64.0 (19.5) | 54 | 65.2 (18.7) | .87 |
| BHLS low/inadequate | 9 | 69.8 (16.7) | 17 | 56.7 (22.2) | 8 | 62.5 (19.8) | .31 |
| SNS high | 26 | 71.4 (17.7) | 28 | 64.8 (23.8) | 32 | 72.5 (15.0) | .25 |
| SNS low/inadequate | 36 | 63.5 (14.7) | 34 | 59.7 (17.0) | 30 | 56.0 (18.0) | .19 |
| Graph high | 29 | 77.1 (11.8) | 28 | 74.2 (13.5) | 36 | 72.8 (15.3) | .46 |
| Graph low/inadequate | 33 | 57.8 (14.4) | 34 | 51.9 (19.6) | 27 | 54.5 (17.5) | .38 |
| Verbatim Score | |||||||
| S-TOFHLA adequate | 51 | 61.0 (19.8) | 42 | 59.2 (21.8) | 41 | 61.0 (21.7) | .90 |
| S-TOFHLA inadequate/marginal | 11 | 45.5 (24.5) | 20 | 46.3 (25.7) | 22 | 48.3 (24.2) | .94 |
| BHLS high | 52 | 56.5 (20.9) | 45 | 56.1 (24.4) | 54 | 56.7 (24.1) | .99 |
| BHLS low | 9 | 65.3 (22.3) | 17 | 52.2 (22.2) | 8 | 54.7 (18.8) | .34 |
| SNS high | 26 | 62.5 (22.6) | 28 | 58.5 (25.0) | 32 | 65.6 (19.1) | .47 |
| SNS low | 36 | 55.2 (20.1) | 34 | 52.2 (22.5) | 30 | 45.8 (22.8) | .22 |
| Graph high | 29 | 69.4 (19.1) | 28 | 68.3 (18.5) | 36 | 63.9 (20.0) | .47 |
| Graph low | 33 | 48.5 (18.4) | 34 | 44.1 (22.0) | 27 | 46.8 (23.9) | .70 |
| Gist Score | |||||||
| S-TOFHLA adequate | 51 | 81.4 (14.8) | 42 | 74.2 (22.8) | 41 | 85.8 (13.7) | .01 |
| S-TOFHLA inadequate/marginal | 11 | 63.6 (18.0) | 20 | 65.0 (24.1) | 22 | 58.3 (19.8) | .57 |
| BHLS high | 52 | 78.5 (17.3) | 45 | 74.4 (22.4) | 54 | 76.5 (20.6) | .61 |
| BHLS low | 9 | 75.9 (14.7) | 17 | 62.8 (24.7) | 8 | 72.9 (23.5) | .31 |
| SNS high | 26 | 83.3 (18.3) | 28 | 73.2 (27.7) | 32 | 81.8 (16.6) | .17 |
| SNS low | 36 | 74.5 (14.6) | 34 | 69.6 (19.5) | 30 | 69.4 (22.8) | .45 |
| Graph high | 29 | 87.4 (13.1) | 28 | 82.1 (17.5) | 36 | 84.7 (16.6) | .47 |
| Graph low | 33 | 70.2 (15.5) | 34 | 62.3 (24.0) | 27 | 64.8 (20.3) | .27 |
Note. Abbreviations: SD (standard deviation). Means are percent correct on the total, verbatim, and gist knowledge questions.
Program Evaluation
The intervention materials were rated as highly credible study the participants, with mean score above 47 out of a possible 50 maximum score. No credibility mean score differences between intervention arms were observed.
DISCUSSION
Few investigations have compared enhanced visual effects for communication of risk information using a cancer screening patient decision aid among those with limited health literacy and numeracy. Total, verbatim, and gist scores were not significantly different across intervention arms (audiobooklet, static, and animated). Moreover, knowledge scores did not differ significantly across intervention arms when stratified by health literacy and numeracy levels. Of minor note, we observed that participants with adequate health literacy according to S-TOFHLA scores had significantly different gist knowledge scores when stratified by intervention arm; however, this was not observed when examining health literacy using BHLS or numeracy using SNS and GLM. Overall, gist knowledge scores were high for all intervention arms. This suggests that our presentation strategies were successful in communicating key risk information to all participants. Thus, these findings suggest that the use of animation in patient decision aids had similar effects on cancer screening risk comprehension as a well-designed static decision aid.
We prioritized recruiting those from minority and potentially vulnerable populations, namely racial/ethnic minorities and those with low health literacy. Among study participants, more than 70% reported their race/ethnicity as Black/African American and most participants were women. In addition, over 50% had low numeracy and about 20% had low health literacy. Enrolling participants from potentially vulnerable populations provides unique insight into the effects of risk communication strategies among a population often motivated to engage in shared decision making yet may have limited true opportunities to actually engage in the decision-making process.40 The decision aids used in this study were developed using strategies for a low health literacy audience, including: using plain language; conveying risk information using absolute risk and incremental risk; providing only relevant information about options; and, using simple pictographs both with and without enhanced animation features.13,41 Our results suggest that use of a well-designed static decision aid may be not more beneficial when compared to a more resource intensive animated video. These findings can help inform risk communication strategies to be used to support decision making among potentially vulnerable populations and in low resource settings.
Our findings regarding the effects of animation in risk communication have been supported by other studies. In a review by Stellamanns and colleagues, static visual aids were found to be effective in increasing understanding; however, they cite a need for further research to evaluate the effectiveness of dynamic formats in risk communication.12 Our investigation builds upon this work as it is one of the first to examine the use of animation when compared to static depictions of risk in a cancer screening patient decision aid. While use of animation may enhance message relevance, use of well-designed static materials may be as beneficial and may also enhance decision aid feasibility in various contexts.18 Enhanced animation techniques may be distracting to viewers; thus, using animation to enhance risk communication may obscure the overall risk messaging.42,43 In contrast, our investigation found that enhanced animation did not augment or impede total, verbatim, or gist knowledge scores. Hence, this unique contribution highlights that animated decision aids may not be differentially impactful in communicating risk information when compared to a well-designed static decision aid. Therefore, researchers may consider their purpose and priorities to decide if the resources associated with developing, maintaining, and implementing decision aid interventions with animation is warranted.
Variations in the presentation of risk information can influence understanding, perceived risks and benefits, and the trustworthiness of the information being conveyed.13–15,18,44 Likewise, the context of the medical decision to be made can also influence how risk is perceived and applied.13 For example, in the context of a preventive screening decision, like CRC screening, healthy individuals are learning about the frequencies of the benefits and harms associated with screening. In contrast, when a diagnosed patient is making a treatment decision for an aggressive disease, the emotional and probabilistic tasks required of the decision are much higher and may necessitate multiple risk communication strategies to support the decision making process.13 For those with limited health literacy, employing pictographs to convey risk accompanied by a plain language description that is easy to process may support the multiple risk communication strategies a complex, high stakes decision demands and may be as beneficial as enhanced animation.13,18 In addition, teaching or priming those with limited health literacy on how to interpret numerical information presented in pictographs may further provide decision support when making complex decisions.40
Limitations
This study recruited participants from a cancer prevention center and community services center located in a large US metropolitan city. The racial/ethnic make-up of our participants did not represent all populations and the ability to communicate in English was an inclusion criterion. Participants recruited from different settings may have had different exposure to health information. Thus, future research that includes participants from various racial/ethnic groups as well as those who prefer to communicate in languages other than English and recruited from various settings may enrich and build upon these findings. Our study was cross-sectional and therefore the long-term follow-up for knowledge retention was lacking. Health literacy and numeracy measures provided valuable insight into patient abilities; however, they are limited in how they measure all factors associated with health literacy and numeracy.38 Additionally, the animation strategies used in the decision aids did not represent all possible uses of animation, e.g., the depiction of time; therefore, future studies investigating the different types and uses of animation may yield insight into the impact of various features on total, verbatim, and gist knowledge scores
CONCLUSION
This study suggests that animation offers no advantage over well-designed static materials in improving knowledge and recall of numerical risk among those with low health literacy. Future work should pursue longitudinal follow-up to assess if these knowledge gains are sustained over time. Use of static visual aids to communicate risk may be as effective as animation and more feasible to implement in a variety of settings. Available resources, such as access to technology and funding, may guide developers’ choice for the use of animation in decision aids.
Figure 1.
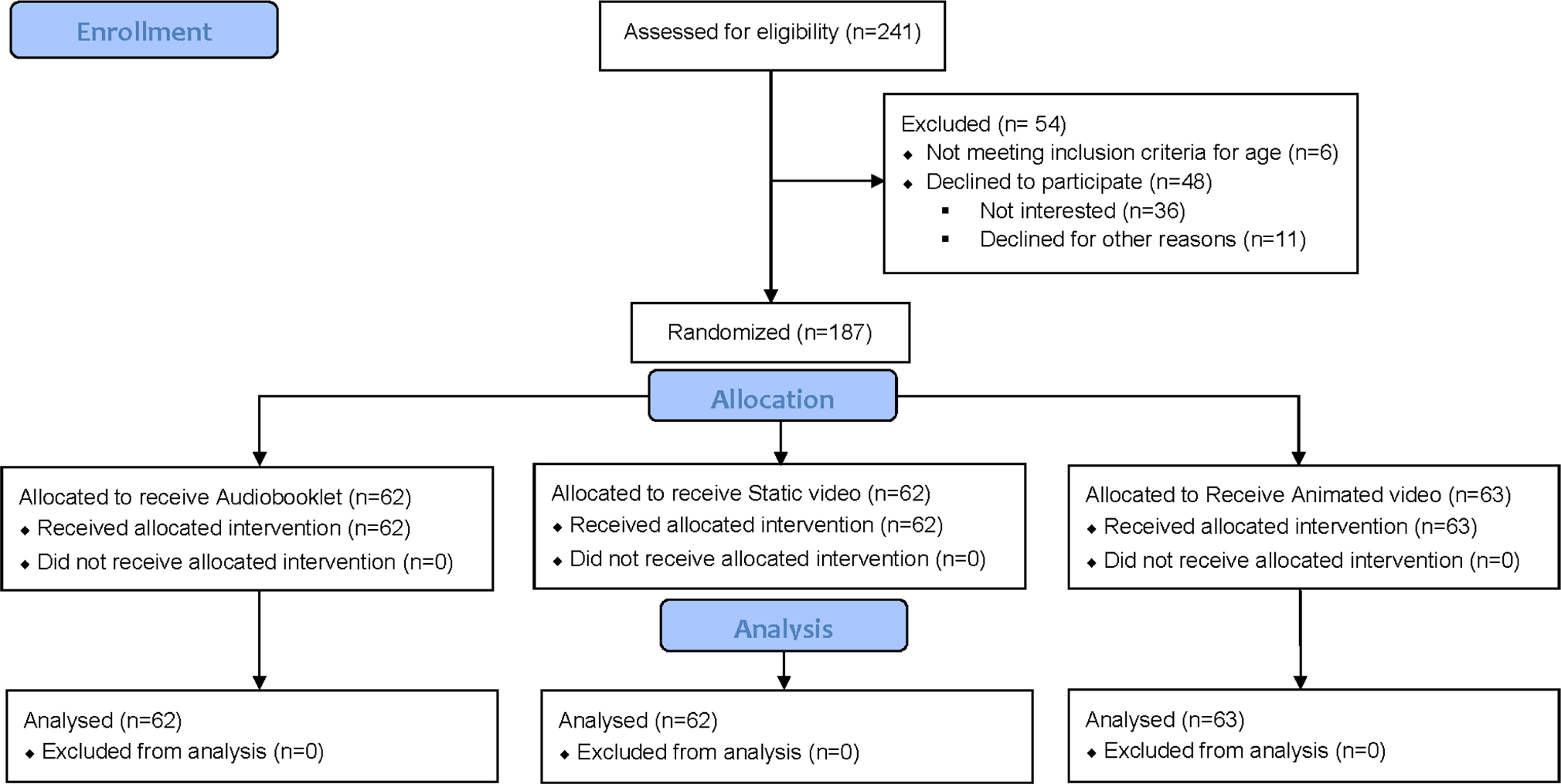
Flowchart of study events (CONSORT diagram)
Acknowledgements:
We would like to acknowledge the contributions of Brian J. Zikmund-Fisher, PhD; Paul K. J. Han, MD, MA, MPH; and Steve Woloshin, MD, MS, who served as expert panel members. We would also like to acknowledge the significant contributions of Suzanne K. Linder, PhD..
This research was supported by the Foundation for Informed Medical Decision Making, [Research Grant 0169-1]; National Cancer Institute at the National Institutes of Health [P30 CA016672 to The University of Texas MD Anderson Cancer Center as a Cancer Center Support Grant and used the Shared Decision Making Core and Clinical Protocol and Data Management; The National Institute on Minority Health and Health Disparities of the National Institutes of Health [K99 MD011485]; and The University of Texas MD Anderson Cancer Center’s Duncan Family Institute for Cancer Prevention and Risk Assessment. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
APPENDICES
Appendix Table 1.
Risk Concepts, Task Descriptions and Multimedia Strategies for Displaying Risk Estimates.
| Risk Concept | Task Description | Multimedia Strategies |
|---|---|---|
| 1. Relevant Group |
|
|
| 2. Denominator |
|
|
| 3. Numerator |
|
|
| 4. Time Frame |
|
|
| 5. Increment-al Benefit |
|
|
| 6. Rare Events |
|
|
| 7. Uncertainty with Risk Estimate* |
|
Note: Understand uncertainty with risk estimate (7) was not included.
Footnotes
Publisher's Disclaimer: This is the prepublication, author-produced version of a manuscript accepted for publication in Medical Decision Making. This version does not include postacceptance editing and formatting. Medical Decision Making is not responsible for the quality of the content or presentation of the author-produced accepted version of the manuscript or of any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (correspondence, corrections, editorials, hyperlinked articles, etc.) should go to http://mdm.sagepub.com/. Those who cite this manuscript should cite the published version as it is the official version of record.
Previous presentation:
International Shared Decision Making Conference, Sydney, Australia, July, 2015.
REFERENCES
- 1.van der Heide I, Uiters E, Jantine Schuit A, Rademakers J, Fransen M. Health literacy and informed decision making regarding colorectal cancer screening: a systematic review. Eur J Public Health. 2015;25(4):575–582. [DOI] [PubMed] [Google Scholar]
- 2.Marteau TM, Dormandy E, Michie S. A measure of informed choice. Health Expect. 2001;4(2):99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michie S, Dormandy E, Marteau TM. The multi-dimensional measure of informed choice: A validation study. Patient Educ Couns. 2002;48(1):87–91. [DOI] [PubMed] [Google Scholar]
- 4.van den Berg M, Timmermans DR, ten Kate LP, van Vugt JM, van der Wal G. Informed decision making in the context of prenatal screening. Patient Educ Couns. 2006;63(1–2):110–117. [DOI] [PubMed] [Google Scholar]
- 5.Davis TC, Dolan NC, Ferreira MR, et al. The role of inadequate health literacy skills in colorectal cancer screening. Cancer Invest. 2001;19(2):193–200. [DOI] [PubMed] [Google Scholar]
- 6.Trevena LJ, Davey HM, Barratt A, Butow P, Caldwell P. A systematic review on communicating with patients about evidence. J Eval Clin Pract. 2006;12(1):13–23. [DOI] [PubMed] [Google Scholar]
- 7.Trevena LJ, Zikmund-Fisher BJ, Edwards A, et al. Presenting quantitative information about decision outcomes: A risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak. 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services. Healthy People 2010 (2nd ed.). Washington, DC: Department of Health and Human Services, National Networks of Libraries of Medicine; 2000. [Google Scholar]
- 9.Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. National Center for Education Statistics. 2006. [Google Scholar]
- 10.Glassman P, National Network Libraries of Medicine. Health Literacy. 2014; Retreived from: http://nnlm.gov/outreach/consumer/hlthlit.html. Accessed May 1, 2019. [Google Scholar]
- 11.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. [DOI] [PubMed] [Google Scholar]
- 12.Stellamanns J, Ruetters D, Dahal K, Schillmoeller Z, Huebner J. Visualizing risks in cancer communication: A systematic review of computer-supported visual aids. Patient Educ Couns. 2017;100(8):1421–1431. [DOI] [PubMed] [Google Scholar]
- 13.Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: Ten steps to better risk communication. J Natl Cancer Inst. 2011;103(19):1436–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawley ST, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns. 2008;73(3):448–455. [DOI] [PubMed] [Google Scholar]
- 15.Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, Fagerlin A. The effect of format on parents’ understanding of the risks and benefits of clinical research: A comparison between text, tables, and graphics. J Health Commun. 2010;15(5):487–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diefenbach MA, Mohamed NE, Butz BP, et al. Acceptability and preliminary feasibility of an internet/CD-ROM-based education and decision program for early-stage prostate cancer patients: Randomized pilot study. J Med Internet Res. 2012;14(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li LC, Adam PM, Townsend AF, et al. Development and usability testing of answer: A web-based methotrexate decision aid for patients with rheumatoid arthritis. Arthritis Rheum. 2011;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tait AR, Voepel-Lewis T, Brennan-Martinez C, McGonegal M, Levine R. Using animated computer-generated text and graphics to depict the risks and benefits of medical treatment. Am J Med. 2012;125(11):1103–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Astley CM, Chew DP, Aylward PE, Molloy DA, De Pasquale CG. A randomised study of three different informational AIDS prior to coronary angiography, measuring patient recall, satisfaction and anxiety. Heart Lung Circ. 2008;17(1):25–32. [DOI] [PubMed] [Google Scholar]
- 20.Han PK, Klein WM, Killam B, Lehman T, Massett H, Freedman AN. Representing randomness in the communication of individualized cancer risk estimates: Effects on cancer risk perceptions, worry, and subjective uncertainty about risk. Patient Educ Couns. 2012;86(1):106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ancker JS, Weber EU, Kukafka R. Effects of game-like interactive graphics on risk perceptions and decisions. Med Decis Making. 2011;31(1):130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bissett S, Wood S, Cox R, Scott D, Cassell J. Calculating alcohol risk in a visualization tool for promoting healthy behavior. Patient Educ Couns. 2013;92(2):167–173. [DOI] [PubMed] [Google Scholar]
- 23.Witteman HO, Fuhrel-Forbis A, Wijeysundera HC, et al. Animated randomness, avatars, movement, and personalization in risk graphics. J Med Internet Res. 2014;16(3):e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franklin L Designing interactive decision aids for medical risk communication and exploration of treatment options. University of Maryland, College Park; 2013. Retrieved from: http://www.cs.umd.edu/hcil/trs/2013-20/2013-20.pdf. Accessed May 1, 2019. [Google Scholar]
- 25.Jimbo M, Rana GK, Hawley S, et al. What is lacking in current decision aids on cancer screening? CA Cancer J Clin. 2013;63(3):193–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore JO, Boyer EW, Safren S, et al. Designing interventions to overcome poor numeracy and improve medication adherence in chronic illness, including HIV/AIDS. J Med Toxicol. 2011;7(2):133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang DS, Jani AB, Sesay M, et al. Video-based educational tool improves patient comprehension of common prostate health terminology. Cancer. 2015;121(5):733–740. [DOI] [PubMed] [Google Scholar]
- 28.Miller DP, Spangler JG, Case LD, Goff DC, Singh S, Pignone MP. Effectiveness of a web-based colorectal cancer screening patient decision aid: A randomized controlled trial in a mixed-literacy population. Am J Prev Med. 2011;40(6):608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zikmund-Fisher BJ, Ubel PA, Smith DM, et al. Communicating side effect risks in a tamoxifen prophylaxis decision aid: The debiasing influence of pictographs. Patient Educ Couns. 2008;73(2):209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han PK, Klein WM, Lehman T, Killam B, Massett H, Freedman AN. Communication of uncertainty regarding individualized cancer risk estimates: effects and influential factors. Med Decis Making. 2011;31(2):354–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zikmund-Fisher BJ, Fagerlin A, Roberts TR, Derry HA, Ubel PA. Alternate methods of framing information about medication side effects: Incremental risk versus total risk of occurrence. J Health Commun. 2008;13(2):107–124. [DOI] [PubMed] [Google Scholar]
- 32.Dialog Health. Colon Cancer Screening: Deciding What’s Right for You [booklet and companion DVD] In: Harvard Medical School, reviewer. Boston, MA: Health Dialog Services Corporation; 2016. [Google Scholar]
- 33.Tait AR, Zikmund-Fisher BJ, Fagerlin A, Voepel-Lewis T. Effect of various risk/benefit trade-offs on parents’ understanding of a pediatric research study. Pediatrics. 2010;125(6):e1475–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. [DOI] [PubMed] [Google Scholar]
- 35.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 36.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McNaughton CD, Kripalani S, Cawthon C, Mion LC, Wallston KA, Roumie CL. Association of health literacy with elevated blood pressure: a cohort study of hospitalized patients. Med Care. 2014;52(4):346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Housten AJ, Lowenstein LM, Hoover DS, Leal VB, Kamath GR, Volk RJ. Limitations of the S-TOFHLA in measuring poor numeracy: A cross-sectional study. BMC Public Health. 2018;18(1):405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Galesic M, Garcia-Retamero R. Graph literacy: A cross-cultural comparison. Med Decis Making. 2011;31(3):444–457. [DOI] [PubMed] [Google Scholar]
- 40.Politi MC, Dizon DS, Frosch DL, Kuzemchak MD, Stiggelbout AM. Importance of clarifying patients’ desired role in shared decision making to match their level of engagement with their preferences. BMJ. 2013;347. [DOI] [PubMed] [Google Scholar]
- 41.Zikmund-Fisher BJ, Fagerlin A, Ubel PA. Improving understanding of adjuvant therapy options by using simpler risk graphics. Cancer. 2008;113(12):3382–3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zikmund-Fisher JB, Witteman OH, Fuhrel-Forbis A, Exe LN, Kahn CV, Dickson M. Animated graphics for comparing two risks: A cautionary tale. J Med Internet Res. 2012;14(4):e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mayer RE, Hegarty M, Mayer S, Campbell J. When static media promote active learning: Annotated illustrations versus narrated animations in multimedia instruction. J Exp Psychol Appl. 2005;11(4):256. [DOI] [PubMed] [Google Scholar]
- 44.Schapira MM, Nattinger AB, McAuliffe TL. The Influence of graphic format on breast cancer risk communication. J Health Commun. 2006;11(6):569–582. [DOI] [PubMed] [Google Scholar]


