Abstract
Background:
The transition to college is a developmentally sensitive time in which freshmen are at high-risk for engaging in heavy drinking and experiencing changes in weight and body composition. The study tested prospective associations among drinking patterns (weekly drinks, heavy drinking occasions/month) and alcohol calorie intake on weight and waist circumference change over the first year of college.
Methods:
College freshmen (N=103) were randomly selected from a pool of eligible students to participate at the beginning of the academic year. The sample was comprised of 52% males, 46% of individuals identifying as racial or ethnic minority, and 45% students with at-risk drinking as defined by the Alcohol Use Disorders Identification Test- Consumption questions. Students engaging in daily risky drinking (n=2) were excluded. Participants attended three visits during the academic year during which they provided weight and waist circumference measurements and completed assessments about drinking, dietary intake, and physical activity.
Results:
Weight gain (>2.3 kg) occurred in 28% of participants. In linear mixed models, drinking patterns and alcohol calorie intake were not associated with weight or waist circumference changes within individuals, when controlling for demographic and energy balance variables. Drinking patterns and alcohol calorie intake did not account for differences in anthropometric measurements between participants, when controlling for covariates.
Conclusions:
Alcohol use did not explain the anthropometric changes observed in a sample well represented by freshmen engaging in risky drinking (and excluding those with daily risky drinking) during the academic year. Drinking may not contribute to short-term weight gain among freshmen.
Keywords: college students, alcohol use, risky drinking, weight gain, energy intake
Introduction
The transition from high school to college is a developmentally sensitive period that is high-risk for behaviors that can negatively impact health, such as heavy drinking (Brown et al., 2008). According to the developmental risk model of alcohol use presented by Brown et al (2008), early adulthood is a high-risk period for substance use due to active neurodevelopment in brain regions responsible for self-regulatory behaviors, which are not fully mature, combined with expanding access to addictive substances in the environment. The combination of neurodevelopmental and environmental risk factors results in heavy drinking as a prevalent problem on college campuses. Among college freshmen not residing with their parents, 34% endorsed drinking 5+ drinks on one occasion in the last two weeks and 14% endorsed high-intensity consumption of 10+ drinks on one occasion (Patrick and Terry‐McElrath, 2016).
The transition from high school to college is also considered a high-risk period for weight gain and changes in body composition for some students. Approximately 30% of freshmen gain weight during the first year of college, defined as >5 lbs or 2.3kg (Cluskey and Grobe, 2009; Morrow et al., 2006; Wengreen and Moncur, 2009; Zagorsky and Smith, 2011). Weight gain results from an imbalance between energy intake and expenditure. Most studies that examined factors contributing to freshman weight gain and/or increased body fat focused on changes in dietary intake, such as increased caloric intake from snack foods, and decreased energy expenditure from physical activity (Butler et al., 2004; Jung et al., 2008; Levitsky et al., 2004; Vella-Zarb and Elgar, 2009; Wengreen and Moncur, 2009). Studies of diet and physical activity changes have generally reported small to moderate effect sizes on weight and body composition changes.
One factor that has received less attention, but has the potential to create an energy surplus, is heavy episodic drinking. Given that one beer contains approximately 150 calories, college freshmen may consume 750+ calories from beer in a single drinking occasion. In qualitative interviews, freshmen themselves have identified alcohol use as a key factor influencing their weight gain (Nikolaou et al., 2014). Initial evidence from longitudinal studies suggested that risky drinking and increased drinking during freshman year may contribute to weight gain, however most studies had methodological limitations that complicated their study interpretations. For example, in a study of almost 300 freshmen, moderate-risk drinking as defined by the Alcohol Use Disorders Identification Test (AUDIT) was associated with a significant increase in body mass index (BMI) by approximately one point, compared to low-risk drinking students who gained 0.5 BMI points during the academic year (Lloyd-Richardson et al., 2008). However, the AUDIT was administered at the second study assessment point, but not the first, which resulted in post-hoc classifications of students’ drinking patterns. Moreover, energy expenditure was not accounted for in the analytic models. Several additional studies conducted in samples of primarily healthy weight and overweight students found that increased alcohol consumption during the first year of college was associated with weight and BMI increases, particularly among males, with small to moderate effect sizes (Adams and Rini, 2007; Bodenlos et al., 2015; de Vos et al., 2015; Deforche et al., 2015; Economos et al., 2008). However, most studies did not use standard alcohol assessments (Adams and Rini, 2007; Bodenlos et al., 2015; de Vos et al., 2015; Deforche et al., 2015; Economos et al., 2008) and had samples comprised primarily of White females, limiting generalizability (Adams and Rini, 2007; Bodenlos et al., 2015; Economos et al., 2008). Furthermore, the majority of past studies used either self-reported weight (Economos et al., 2008), which is prone to biases in underestimation, or did not account for within-day weight fluctuations in their study designs by taking weight measurements at the same time of day (Adams and Rini, 2007; Bodenlos et al., 2015; de Vos et al., 2015).
In contrast to the aforementioned positive findings, other studies found that alcohol use was not associated with college weight gain (Deliens et al., 2013; Kasparek et al., 2008; Pliner and Saunders, 2008; Pope et al., 2017; Zagorsky and Smith, 2011). For example, in the only study to measure alcohol calorie intake in students, Pope et al (2017) estimated college students’ daily alcohol calorie intake using a food frequency questionnaire and did not find a significant impact on 4-year weight change (Pope et al., 2017). However, 96% of the sample engaged in low-risk drinking, as determined by the AUDIT.
With the current state of the literature, it is unclear whether alcohol use impacts weight gain among college students. Over the past twenty years, discrepant findings have also been reported in the broader literature focused on the general population, with some researchers reporting a positive association between alcohol use and weight gain or obesity (Breslow and Smothers, 2005; Lukasiewicz et al., 2005; Wannamethee et al., 2005), some reporting a negative association alcohol use and weight gain or obesity (Thomson et al., 2012; Tolstrup et al., 2008, 2005), and some reporting null findings (Bobak et al., 2003; Wannamethee et al., 2004). These conflicting findings led to a debate about whether and under what circumstances alcohol use may lead to weight gain or obesity (Bendsen et al., 2013; Sayon-Orea et al., 2011; Suter, 2005; Traversy and Chaput, 2015; Yeomans, 2010a). However, over time some trends have emerged in the broader literature that may inform the college literature. First, the majority of studies in the broader literature have focused on the general population, where alcohol consumption is generally low (Dawson et al., 2015) and detecting effects of heavier drinking patterns may be difficult. Furthermore, many studies assessed low to moderate daily alcohol intake, which may not substantially disrupt energy balance (Bobak et al., 2003; Thomson et al., 2012; Tolstrup et al., 2008; Wang et al., 2010). More recently, researchers have examined the association between heavy episodic drinking (≥4 drinks for females or ≥5 drinks for males; National Institute on Alcohol Abuse and Alcoholism, 2005) and weight gain and/or obesity, with the hypothesis that heavy episodic drinking may lead to excess caloric intake and disrupt energy balance. Researchers have reported consistent findings that heavy episodic drinking may be associated with weight gain and obesity in the general population and among young adults (Chakraborty, 2014; Arif and Rohrer, 2005; Fazzino et al., 2017; Breslow and Smothers, 2005). Finally, research has emerged suggesting there may be differences in the effects of alcohol use on body weight and obesity among those with alcohol use disorder. Daily heavy episodic drinking for a period of years has been found to alter the way in which alcohol is metabolized, which can result in higher energy expenditure and lower body weight despite excess calorie intake from alcohol (Addolorato et al., 2000; de Timary et al., 2012). Overall the pattern regarding alcohol use and obesity-related outcomes in the broader literature is nuanced, but does suggest that non-daily heavy episodic drinking may be associated with excess weight gain and obesity. The same positive association between alcohol use and weight gain may be observed among college students with the use of improved assessment methodology, specifically valid measures of alcohol consumption and measured height and weight.
The purpose of the present study was to prospectively test associations among alcohol use patterns and alcohol calorie intake with weight and waist circumference change during the first year of college in a sample of freshmen stratified by sex, race/ethnicity, and at-risk drinking status, and excluding students with a pattern of daily heavy drinking. We hypothesized that greater alcohol involvement, operationalized as mean drinks per week, number of heavy drinking occasions per month, and mean calorie intake from alcoholic beverages, would be 1) associated with greater weight and waist circumference change within individuals and 2) would be associated with higher weight and waist circumference across individuals.
Materials and Methods
The study enrolled a sample of college freshmen who attended three assessment visits at the beginning (September), middle (November), and end (April) of the academic year. A description of recruitment and enrollment is presented first, followed by a description of the measurements.
Recruitment and Screening
At the beginning of the Fall semester, all incoming freshmen at a large Midwestern university were sent a recruitment email inviting them to complete a brief, two-minute screen for study eligibility. The email included a link to a study information page and screening consent form. Students were required to consent to screening and then filled out a contact information form, demographic information, and the Alcohol Use Disorder Identification Test-Consumption (AUDIT-C) questions (Bradley et al., 2003; Bush et al., 1998; Saunders et al., 1993). Screening was open for five days.
Eligibility criteria consisted of 1) age ≥18 and 2) first time incoming freshmen (not transferring from another university). Students were ineligible if they endorsed “daily or almost daily” heavy episodic drinking on the AUDIT-C. Daily heavy episodic drinking alters the way alcohol is metabolized, leading to higher energy expenditure and lower body weight (Addolorato et al., 2000; de Timary et al., 2012) and this would have presented a study confound.
Sampling and Enrollment
A priori power analyses indicated that N=103 participants would be sufficient with 80% power to detect moderate-sized effects on the outcomes when accounting for a 20% attrition rate.
To ensure adequate representation across demographic characteristics, the sample was stratified by sex (male/female) and race/ethnicity (White, non-Hispanic/Racial or Ethnic Minority). The sample was also stratified by AUDIT-C defined at-risk drinking status using cut points normed for college students (5+ for females, 7+ for males) (DeMartini and Carey, 2012) to provide enough variation in drinking behavior to facilitate the assessment of the primary outcomes. The stratification resulted in six categories of participants to fill target (N=103) enrollment slots. Randomly sampled students were invited to participate on a rolling basis over four weeks until all enrollment slots were filled.
The study was approved by the Institution Review Board and all students provided full written informed consent before participating.
Assessment visits
Participants completed a series of three laboratory visits during the academic year during which they provided height, weight, and waist circumference measurements, and completed computer-based assessments of alcohol use, medical and health information, diet and weight control behaviors, and physical activity. Following each visit, participants were asked to complete a series of three, photo-assisted online dietary recalls.
An escalating incentive structure was used for the study visits; participants were compensated $25 for completing the baseline visit, $35 for completing the second visit, and $45 for completing the final visit. Participants were also compensated $15 for each dietary recall they completed.
Measures
Alcohol use:
The computerized Time Line Follow Back (TLFB-C) was used to assess daily alcohol use in standard drinks (Sobell et al., 1996; Sobell and Sobell, 1992) (copyrighted to Sobell & Sobell, 2008). The TLFB-C has good test-retest reliability and evidence of convergent validity with the TLFB administered in-person among college student samples (Miller et al., 2002; Pedersen et al., 2012). TLFB-C data were used to compute mean total weekly drinks and mean heavy drinking episodes per month at each time point. Heavy drinking occasions were defined as 4+ drinks for females, or 5+ for males in one episode, in excess of the low-risk drinking guidelines from the National Institute on Alcohol Use and Alcoholism (National Institute on Alcohol Abuse and Alcoholism, 2005). The heavy drinking occasions variable did not account for consuption within a specific period of time (eg, 2 hours). Our hypothesis was that excess caloric intake from alcoholic beverages would lead to weight gain; given that the caloric contents of alcoholic beverages are stable across rate of consumption, we did not expect that rate of drinking would change the number of excess calories consumed from the same quantity of drinks.
Weight, height, and waist circumference:
Participants were weighed in light clothing using a calibrated digital scale accurate to 0.1 kg (Befour PS5700). Participants were weighed at the same time of day at each assessment point to control for within-day weight fluctuations. Height was measured with a stadiometer. To estimate central adiposity, waist circumference was obtained with two measurements per site within 2 cm using standardized procedures (Lohman and Roche, 1988). All measurements were taken twice and averaged to obtain a final value.
Medical questions:
Participants answered questions about chronic medical conditions, prescription medication taken to treat an illness or injury, prescription medication taken for a chronic medical condition, and current use of tobacco products. Participants were also asked whether they were participating in an organized weight loss program (or had since their last study visit) and how much weight they lost weight as a result of their participation in a program(s).
Physical activity:
The International Physical Activity Questionnaire (IPAQ) Short Form, Self-Administered version was used to assess physical activity from transportation, employment, and recreation, including college sports participation. It has evidence for reliability and validity (Craig et al., 2003), including in college student samples (Dinger et al., 2006; Dishman and Steinhardt, 1988).
Diet:
Dietary intake was assessed using the Automated Self-Administered 24 Hour Diet Recall (ASA24) (Subar et al., 2012), the web-based version of the USDA Multiple Pass Diet Recall, developed and hosted by the National Cancer Institute (Conway et al., 2003; Subar et al., 2012). The diet recall method involves an iterative process through which individuals are asked to report detailed information about all food and beverages consumed in the past 24 hours, including food or drink type, the portion size, all contents of the food/beverage, and the amount they consumed. Web-based 24-hour recalls have shown evidence for reliability and convergent validity when compared to interviewer-administered diet recalls with young adults and objective measurement using doubly-labelled water (Arab et al., 2011; Blanton et al., 2006; Kirkpatrick et al., 2014; Moshfegh et al., 2008; Vereecken et al., 2008).
Diet recalls were used to collect data on overall dietary intake, as well as calorie intake from alcoholic beverages, and alcohol-related eating episodes. Thus, participants were asked to include their alcoholic beverage intake in the diet recall reports and the ASA24 program included a reminder at the end of the program to report any alcohol intake. Diet recalls have evidence for convergent validity in measuring alcohol intake when compared with standard retrospective alcohol intake assessments (Agarwal et al., 2016; Serra-Majem et al., 2002).
To aid participants’ recall of their dietary intake, we used a photo-assisted method that has been demonstrated to improve the quality of 24-hour diet recalls with adolescents and adults (Ptomey et al., 2015, 2013). Participants were instructed to use their cell phones to photograph all food and non-alcoholic beverage intake during a 24-hour period. The following day, students completed the ASA24 recall using their photos as a memory aid.
Participants were asked to complete three recalls per assessment period, one on a weekday and two on weekend days to capture differences in eating and drinking habits across the week (Buzzard et al., 1996). Recalls were completed within one week of each in-person study visit. The three recall days were randomly assigned to participants at each time point. Participants received notification via email the night before indicating when to initiate photo days and complete recalls. Participants who provided valid recall data in the form of 2+ recalls, one on a weekday and one on a weekend day (Buzzard et al., 1996) were considered to be compliant with recalls for a given assessment point. Diet recall data were used to compute mean total calorie intake and mean calorie intake from alcoholic beverages.
Disordered eating behavior:
The Eating Pathology Symptoms Inventory (EPSI) was used to measure disordered eating behavior (Forbush et al., 2013). The EPSI conceptualizes eating behavior on a dimensional scale and is appropriate for use in samples with and without eating disorders. The EPSI has shown evidence for excellent discriminant and convergent validity in both female and male college samples (Forbush et al., 2014, 2013). The Binge Eating scale score was considered as a potential covariate in the analytic models.
Data Analysis
Analyses were conducting using Mplus Version 8 (Muthén and Muthén, 1998) A series of linear mixed models were constructed to test the associations among drinking patterns and weight and waist circumference change over time, while accounting for correlations from repeated assessments within participants (Long, 2011). Four linear mixed models were constructed to test whether two drinking behavior variables — mean drinks per week or mean heavy drinking occasions per month — were associated with weight change or waist circumference change as dependent variables. We also tested the relationship between mean alcohol calorie intake derived from the diet recalls and weight and waist circumference change. Full Information Maximum Likelihood estimation (FIML) was used to account for missing data and facilitated the inclusion of all (N=103) participants in all analyses. To disaggregate the between and within subjects effects in our longitudinal models, procedures were followed per the recommendations of Curran and Bauer (2011). Specifically, to test between-subjects differences in drinking, the means of the three drinking variables (weekly drinks, heavy drinking occasions per month, alcohol calorie intake) were computed per individual across study time points, which allowed us to test whether average drinking level was associated with differences in weight and waist circumference across participants over time. To test the effects of within-individual variation in drinking, individuals’ drinking variables at each time point were centered around their drinking variable mean (e.g., an individual’s weekly drinks at each time point were centered around their overall mean weekly drinks across study). By individual-mean centering the drinking variables, we tested whether variation in drinking around an individual’s average drinking level was associated with variation in their weight and waist circumference during the academic year. All linear mixed models included visit number as a measure of time. In parallel with our hypothesis, we included only fixed effects in the models for between subjects effects. For within-subjects effects, a random intercept was included in all models.
Covariates
Dietary intake and physical activity variables were included as covariates in all analytic models due to their direct relationships with energy balance. Mean total calorie intake as determined using the diet recalls was used to account for total energy intake in all models except the alcohol calories model because alcohol calories were included in the calculation of the total calorie intake variable. In the alcohol calorie model, total non-alcohol calorie intake was included instead to account for the effects of non-alcohol related calories on weight and waist circumference outcomes. Weekly average metabolic energy expenditure from walking as determined by the IPAQ was used as a measure of physical activity. We were unable to use the moderate and vigorous physical activity data on the IPAQ because many physical activity estimates were outside a plausible range. Upon examination of the data, many participants appeared to double-report the amount of time they spent in physical activity during the week by reporting equivalent amounts of time spent in both moderate and vigorous activity categories (e.g., 150 minutes of vigorous activity and 150 minutes of moderate activity, both for 4 days per week). This possible double-counting of physical activity resulted in many weekly physical activity estimates that appeared inflated and outside of a valid range. However, the IPAQ daily walking estimates did fall within a plausible range and given that the walking question was separate from the moderate and vigorous physical activity questions in the IPAQ, it seemed reasonable that this question was answered more accurately. Therefore, we used estimated energy expenditure from weekly walking as the best available measure of physical activity.
We examined the following additional variables as potential covariates: sex, race/ethnicity, AUDIT-C defined at-risk drinking at baseline (yes/no), weight class at baseline (underweight or healthy weight/overweight/obese), place of residence (university dorms/fraternity or sorority/off campus), participation in weight loss programs, tobacco use, taking prescription medication for chronic medical conditions, and binge eating. Of the covariates mentioned above, the following had significant relationships with the outcomes and were included in all analytic models: sex and weight class at baseline.
Models using Transformed Variables
The alcohol intake variables that were used as predictor variables in all models were zero-inflated and positively skewed, as is often the case with alcohol data in college samples. However, the use of square-root transformed alcohol variables in the models resulted in the same outcomes (not detailed here) as the models using the original, non-transformed variables. Thus, models with the original variables are reported herein.
Results
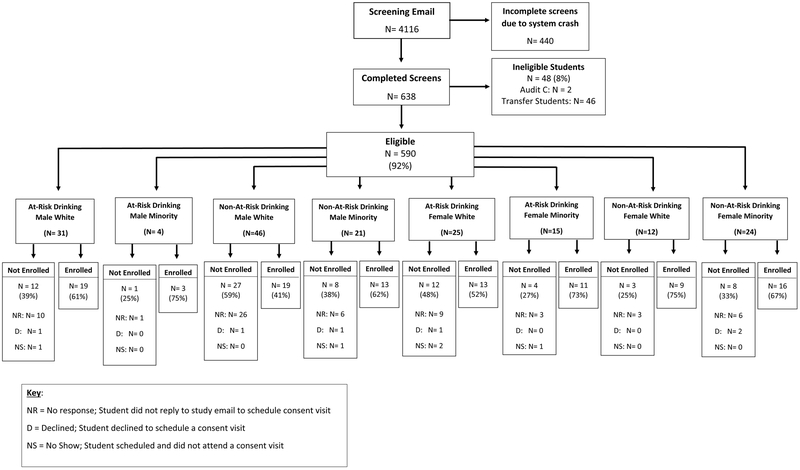
Figure 1 presents the results of screening and enrollment. The recruitment email was sent to all incoming freshmen (N= 4116) and yielded 638 completed screens (16% screening completion rate). An additional 440 responses were incomplete, of which the majority occurred during a technical problem with the host server on the first day. Most students who completed the screen (N=590; 93%) were eligible and the primary reason for ineligibility was transfer student status (non-incoming freshman) (N=46/48; 96%). Of those who completed the screen, 65% were female and 81% were White, non-Hispanic. Of the 178 students invited to participate across six enrollment groups, enrollment rates for most sampling strata were between 60–75% of those contacted, with the exception of the at-risk drinking white female group (enrollment rate = 52%) and the non-at-risk drinking white male group (enrollment rate= 41%). The majority (92%) of individuals who were invited to participate but did not enroll did not respond to our invitation to schedule a study visit. Mean time from screening to enrollment was 19.7 days (SD = 8.3; Range= 5–30).
Figure 1.
Screening and Recruitment
Figure 2 depicts attendance rates at each study visit. Retention at Visit 3 was 78%. Five participants withdrew from the study and two were unable to continue their participation because they moved to a different university. Compliance with diet recalls was 76% at baseline (78 provided valid data/103 who completed the baseline visit), 66% at Visit 2 (61 provided valid data/92 who completed the Visit 2) and 70% at Visit 3 (56 provided valid data/80).
Figure 2.
Retention by Study Time Point
Sample Characteristics
Participant characteristics at baseline are presented in Table 1. Stratified sampling resulted in a sample comprised of 52% males, 46% of individuals identifying as Racial or Ethnic Minority, and 45% AUDIT-C defined at-risk drinking.
Table 1.
Participant Characteristics (N=103)
| M(SD) or N(%) | |
|---|---|
| Age | 18.2(0.6) |
| Sex (% male) | 54(52) |
| Race/ethnicity | |
| White, non-Hispanic | 58(56) |
| African American | 6(6) |
| Asian/Asian American | 14(14) |
| Native American | 2(1) |
| Hispanic American | 15(15) |
| Multiracial | 8(8) |
| BMI baseline | 24.9 (4.4) |
| Weight class at baseline | |
| Underweight | 1(1) |
| Healthy weight | 64(62) |
| Overweight | 25(24) |
| Obese | 13(13) |
| AUDIT-C score baseline | 4.0(3.2) |
Note. M=mean; SD=standard deviation; BMI= body mass index; AUDIT-C = Alcohol Use Disorder Identification Test- Consumption questions
Participants who did not complete Visit 3 did not significantly differ from those who completed Visit 3 with regard to baseline at-risk drinking status (χ2(1) =0.34, p = 0.56), sex (χ2(1) =0.04, p = 0.83), Minority race or ethnicity (χ2(1) =1.02, p = 0.31), or baseline BMI (t(39) = −0.03, p= .97).
At Visit 3, 28% of participants who attended the visit (22/80) gained >2.3 kg. Among those who gained weight, mean gain was 4.6 kg (SD= 1.8; Range= 2.3 – 8.3). Mean waist circumference change among those who gained weight was 6.0 cm (SD = 2.6; Range= 1.9 – 12.8). Weight gain occurred across those of healthy weight (N=11/51; 22%), overweight (N=7/19; 37%), and obese weight classes (N=4/10; 40%).
Across participants, mean weekly drinks during the study was 6.5 (SD= 8.5; Range= 0–41.6) and mean heavy drinking occasions per month was 3.2 (SD= 3.7; Range 0–17). Mean daily calorie intake from alcoholic beverages was 57.1 (SD= 142.7; Range = 0– 779.9). Alcohol intake was reported in 16% of completed diet recalls across 22 participants, 17 of whom were in the AUDIT-C at-risk drinking group at baseline and five who were not in the at-risk drinking group. Zero participants reported alcohol-related eating episodes in the diet recalls.
Descriptive statistics for the variables used in analyses are presented in Table 2 and a correlation matrix is presented in Table 3.
Table 2.
Descriptive Statistics of Measured Variables used in Analyses
| Variable | Mean | Standard Deviation |
|---|---|---|
| Weekly drinks | 6.55 | 8.53 |
| Heavy drinking episodes per month | 3.16 | 3.66 |
| Alcohol calorie intake | 57.08 | 142.45 |
| Total caloric intake | 2100.93 | 641.21 |
| Total non-alcohol caloric intake | 2043.86 | 609.33 |
| Weekly energy expenditure from walking | 892.44 | 929.60 |
| Weight (kg) | 72.16 | 15.35 |
| Waist circumference (cm) | 78.35 | 11.34 |
Table 3.
Correlation Matrix of Measured Variables
| Weekly drinks |
Alcohol calories |
Monthly heavy drinking |
Energy expenditure from walking |
Non- alcohol total calorie intake |
Waist circ. |
Weight | Sex | Overwt. | Obese | |
|---|---|---|---|---|---|---|---|---|---|---|
| Weekly drinks | 1.00 | |||||||||
| Alcohol calories | 0.109 | 1.00 | ||||||||
| Monthly heavy drinking | 0.941 | 0.161 | 1.00 | |||||||
| Energy expenditure from walking | 0.011 | 0.045 | 0.069 | 1.00 | ||||||
| Non-alcohol total calorie intake | −0.197 | 0.114 | −0.231 | 0.090 | 1.00 | |||||
| Waist circ. | 0.101 | 0.049 | 0.033 | −0.048 | 0.084 | 1.00 | ||||
| Weight | 0.185 | 0.076 | 0.118 | −0.069 | 0.125 | 0.936 | 1.00 | |||
| Sex | −0.240 | −0.050 | −0.104 | 0.097 | −0.409 | −0.350 | −0.486 | 1.00 | ||
| Overweight | 0.149 | −0.151 | 0.143 | 0.041 | −0.031 | 0.180 | 0.139 | −0.041 | 1.00 | |
| Obese | −0.006 | 0.066 | −0.025 | 0.003 | −0.001 | 0.765 | 0.703 | −0.069 | −0.215 | 1.00 |
Linear mixed models
Within-subjects effects without covariates:
In the linear mixed models, weekly drinks, heavy drinking occasions per month, and caloric intake from alcoholic beverages as measured within-individuals were not significantly associated with individuals’ weight or waist circumference changes during the academic year (all alcohol variables for weight outcome: beta values = −0.001 to 0.000, p values = .116 to .996; all alcohol variables for waist circumference outcome: beta values = −0.002 to 0.005, p values = 0.835 to 0.996).
Within-subjects effects with covariates:
Weekly drinks and heavy drinking occasions per month as measured within-individuals were not significantly associated with individuals’ weight or waist circumference changes during the academic year when accounting for total caloric intake, energy expenditure from walking, sex, and baseline weight class (all p values = .495 to .870; Table 4). Beta values indicated that students’ alcohol use did not significantly vary from their typical drinking patterns during the year (all beta values = −0.07 to 0.01; Table 4). Mean alcohol calorie intake as measured within-individuals was significantly associated with individuals’ weight change when accounting for total non-alcohol caloric intake, energy expenditure from walking, sex, and baseline weight class; however the magnitude of the effect size indicated the effects were not meaningful (b = −0.002, p= .035; Table 4). Mean alcohol calorie intake was not significantly associated with individuals’ waist circumference change during the year (Table 4).
Table 4.
Linear mixed models for alcohol use and anthropometric outcomes during the first year of college (N=103)
| Beta value | Standard Error |
95% CI | P value | ||
|---|---|---|---|---|---|
| Modela DV: weight (kg) | |||||
| Within: heavy drinking | 0.01 | 0.80 | −0.14, 0.14 | .870 | |
| Between: heavy drinking | 0.17 | 0.27 | −0.36, 0.61 | .536 | |
| Modela DV: weight (kg) | |||||
| Within: weekly drinks | −0.01 | 0.05 | −0.10, 0.08 | .799 | |
| Between: weekly drinks | 0.08 | 0.12 | −0.16, 0.28 | .521 | |
| Modelb DV: weight (kg) | |||||
| Within: alcohol calories | −0.002 | 0.001 | −0.003, 0.000 | .035 | |
| Between: alcohol calories | 0.01 | 0.01 | −0.01, 0.02 | .349 | |
| Modela DV: waist circumference (cm) | |||||
| Within: heavy drinking | −0.07 | 0.11 | −0.27, 0.10 | .495 | |
| Between: heavy drinking | −0.09 | 0.17 | −0.43, 0.19 | .584 | |
| Modela DV: waist circumference (cm) | |||||
| Within: weekly drinks | −0.01 | 0.05 | −0.07, 1.40 | .769 | |
| Between: weekly drinks | −0.02 | 0.08 | −0.17, 0.11 | .835 | |
| Modelb DV: waist circumference (cm) | |||||
| Within: alcohol calories | −0.09 | 0.19 | −0.46, 0.29 | .640 | |
| Between: alcohol calories | 0.004 | 0.003 | −0.002, 0.011 | .209 | |
Note: Within refers to within-subjects effects in the models, interpreted as variation around individual’s typical drinking pattern; between refers to between-subjects effects in the models, interpreted as mean drinking pattern across participants during the study
Covariates included in models: total calorie intake, average metabolic energy expenditure from walking, sex, weight class at baseline
Covariates included in models: total non-alcohol calorie intake, average metabolic energy expenditure from walking, sex, weight class at baseline
Between-subjects effects without covariates:
Results indicated that weekly drinks and heavy drinking occasions per month were significantly associated with weight across participants; greater drinks per week and heavy drinking occasions per month were associated with higher weight (weekly drinks: b= 0.32, p= .007, CI= 0.09, 0.51; heavy drinking occasions: b= 0.07, p= .006, CI= 0.02, 0.13). Alcohol calorie intake was not significantly associated with weight (b= 0.01, p= .568, CI= −0.01, 0.03). None of the alcohol variables were significantly associated with waist circumference (all beta values = 0.006 to 0.109, all p values = 0.179 to 0.573).
Between-subjects effects with covariates:
Results for between-subjects effects indicated that mean weekly drinks, heavy drinking occasions, and mean alcohol calorie intake over the study were not significantly associated with differences in weight or waist circumference across participants, when accounting for total caloric intake, energy expenditure from walking, sex, and baseline weight class (all p values = .193 to .835; Table 4). In all models, sex and weight class at baseline were significantly associated with the outcomes (all p values ≤ .01).
Discussion
The study prospectively examined the relationship between alcohol use patterns and short-term weight and waist circumference change in a sample of college freshmen well-represented across sex, race/ethnicity, and at-risk drinking status, and excluding students with a pattern of daily heavy drinking. Our results suggest that students’ weekly drinks and heavy drinking occasions were not associated with their weight and waist circumference changes during the academic year. Alcohol use on average did not change from the beginning to the end of the academic year, while weight increased in 28% of the sample. Thus, alcohol consumption did not explain the weight and waist circumference changes observed in the study. Also, while we had substantial variability in average weekly drinks and heavy drinking occasions across participants, drinking patterns were not significantly associated with differences in weight and waist circumference across participants. Importantly, we accounted for both demographic and energy balance variables in our models and in the case of between-subjects effects, sex and baseline weight class were more meaningful predictors of differences in anthropometric outcomes than alcohol use.
Overall, our findings are in contrast to prior studies that reported a significant impact of drinking on weight gain in college freshmen. For example, Lloyd-Richardson et al (2008) observed a significant difference in weight gain trajectories across AUDIT scores among freshmen, with moderate-risk drinkers gaining more weight than low-risk drinkers. In our study, AUDIT-C-defined at-risk drinking pattern at baseline was not significantly associated with anthropometric outcomes and heavier drinking as reported in the TLFB-C was not associated with changes in anthropometric measurements during the academic year. Lloyd-Richardson et al (2008) did have a substantially larger sample of >300 students and may have had more statistical power to detect between-subjects effects. However, our study did account for energy expenditure in analytic models, and we identified AUDIT-C drinking patterns a priori instead of post-hoc, which may have also contributed to differences in our findings. Our results also differ from the other studies that reported increases in alcohol use were associated with changes in weight during the first year of college (Adams and Rini, 2007; Bodenlos et al., 2015; de Vos et al., 2015; Deforche et al., 2015; Economos et al., 2008). These studies used alcohol measures that were not standardized and some used a dichotomous variable representing any non-zero increase in alcohol use over the year. In contrast, we used a gold-standard alcohol measure, the TLFB and more comprehensively evaluated change in alcohol use over the academic year using longitudinal modeling, and these factors may have contributed to differences in findings.
One commonality among most prior studies in literature is the assumption that calories consumed from alcoholic beverages are most directly related to energy balance. However, most studies used drinking behavior variables (e.g., drinks per week) as proxy variables of alcohol calorie intake, which has limitations (Kasparek et al., 2008). To our knowledge, our study was the first to also measure caloric intake from alcoholic beverages using 24-hour diet recalls with a college sample that was well-represented by at-risk drinking students (45%). While the findings with the alcohol calorie variable were consistent with the null findings observed using the other drinking variables, alcohol intake was only reported in 16% of the diet recalls, which is in contrast to TLFB-C data that indicated the majority drank alcohol. Our inability to fully capture data on alcohol calorie intake may have prevented us from more precisely testing the relationship between energy intake from alcoholic beverages and anthropometric outcomes. In addition, we received zero alcohol-related eating reports in the diet recalls, which also precluded us from testing potential indirect effects of alcohol use on weight change via alcohol-related eating. It appeared that the web-based diet recall method was not well-suited to measuring alcohol calorie intake and alcohol-related eating episodes among college students and methods are needed to measure intake behaviors in real-time (Fazzino et al., 2018).
Beyond considerations of measurement limitations, the main factor likely contributing to the null findings was that students were able to maintain energy balance, despite excess caloric intake from alcohol. Research suggests that some college students, particularly females, may restrict food calorie intake before drinking in order to compensate for alcohol calorie intake and avoid weight gain (Barry and Piazza-Gardner, 2012; Burke et al., 2010), and some students may have employed this strategy during the current study. Students may have also compensated in healthy ways, either by consuming lower calorie foods the day before or after drinking, and/or through physical activity. It is noteworthy that 28% of the sample did gain weight, but our findings indicate weight gain was likely due to other factors. It may be that compensating for nights of drinking was feasible because for most students drinking was periodic. Other factors present on a daily basis may have been more difficult for some students to compensate for, such as dining at the all-you-can-eat dormitory cafeterias (Leischner et al., 2018; Levitsky and Youn, 2004).
The study had several limitations. First, self-report assessments were used to measure drinking, dietary intake, and physical activity. Although each measure has evidence supporting its validity, self-report measures are prone to biases. While objective measures are available for diet and physical activity, self-reported alcohol use via the TLFB is considered a gold standard and a best available measure of alcohol intake; alcohol biosensors are limited in their detection of non-binge drinking occasions (<4 drinks) (Roache et al., 2015). In addition, we were only able to use the data from the IPAQ regarding walking, which limited our ability to fully characterize and account for physical activity. Finally, we had missing data due to 22% participant attrition by Visit 3, and ~70% compliance with the diet recalls across the study (range 66% - 76% by time point). However, there were no significant differences in demographic characteristic or at-risk drinking status between those who completed Visit 3 and those who did not. In addition, we used full information maximum likelihood estimation, a robust missing data estimation technique to address missing data. Using FIML allowed us to conduct analyses on all participants who enrolled in the study and to make full use of all available data.
The study had several strengths, including the use of a random sampling procedure to select study-eligible students to participate, adequate representation across demographic characteristics and at-risk drinking, and prospective assessment of alcohol use and anthropometric outcomes.
Implications and Future Directions
Given the substantial health, social, and economic costs of obesity, it remains important to elucidate the factors that may contribute to early weight gain in college in order to inform prevention efforts (Cawley and Meyerhoefer, 2012; Trogdon et al., 2008; Withrow and Alter, 2011). In particular, it is important to identify characteristics of the ~30% of college freshmen who gain weight to facilitate prevention efforts. Given that all freshmen who reside on campus enter the same campus environment and only one-third gain weight, it may be that individual-level risk factors predispose certain individuals to gain weight. For example, some individuals may be particularly vulnerable to the rewarding effects of highly palatable foods (high in sugar, fat, and/or salt), which may yield overeating and weight gain when dining primarily at all-you-can-eat cafeterias on campus. However, to our knowledge, individual-level factors that contribute to freshman weight gain have not been identified, and more work in this area is needed. Second, some individuals, particularly those highly sensitive to reward, may seek to extend the rewarding experience from a night of drinking by consuming highly palatable foods directly following drinking. More research is needed to determine whether individual-level factors may identify students who regularly engage in drinking and alcohol-related eating. Given that alcohol may temporarily increase eating behavior (Schrieks et al., 2015; Yeomans and Bertenshaw, 2008; Yeomans, 2010b), future research is also needed to determine whether alcohol use may play an indirect role in weight gain via its effects on alcohol-related eating. In addition, an investigation of fat, sugar, and salt intake patterns during alcohol-related eating episodes may further elucidate mechanisms related to weight stability or gain. Finally, future work is needed to test whether there may be longer-term associations between alcohol use and obesity-related outcomes throughout the college years. It is possible that heavy drinking patterns do not impact short-term weight outcomes early in college; however, the effects of drinking on body weight may accumulate over longer time periods. There is evidence to suggest that a pattern of regular heavy episodic drinking in early adulthood may lead to excess weight gain and transition to obesity in 5–6 years later (Fazzino et al., 2017). Future methodologically rigorous research that replicates our approach and extends the assessment of weight-related outcomes beyond the first year of college is needed to determine if there may be a delayed-time course to the effects of alcohol use on weight gain and obesity risk.
The current findings may also be used to inform alcohol prevention efforts. Web-based brief interventions are typically used to address alcohol use among college students and many programs reference the caloric density of alcohol and/or potential effects on weight gain. The current study findings do not support the premise that alcohol use contributes to short-term weight gain among freshmen. However, is true that alcohol has a high caloric density, second only to fat (Yeomans, 2010a), and that alcohol consumption may lead to alcohol-related eating (Nelson et al., 2009). Thus, it is reasonable for interventions to address the possibility that alcohol use may lead to excess calorie intake. Finally, researchers designing web-based interventions may consider referencing the potential longer-term effects of regular, heavy episodic drinking on obesity-related outcomes (Fazzino et al., 2017).
Acknowledgments
The research was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism F32 AA024669–01A1 (PI: Fazzino). The funding source was not involved in the study design, collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Declarations of interest: none.
References
- Adams T, Rini A (2007) Predicting 1-year change in body mass index among college students. J Am Coll Health J ACH 55:361–365. [DOI] [PubMed] [Google Scholar]
- Addolorato G, Capristo E, Marini M, Santini P, Scognamiglio U, Attilia ML, Messineo D, Sasso GF, Gasbarrini G, Ceccanti M (2000) Body composition changes induced by chronic ethanol abuse: evaluation by dual energy x-ray absorptiometry. Am J Gastroenterol 95:2323–2327. [DOI] [PubMed] [Google Scholar]
- Agarwal S, Fulgoni VL, Lieberman HR (2016) Assessing alcohol intake & its dose-dependent effects on liver enzymes by 24-h recall and questionnaire using NHANES 2001–2010 data. Nutr J 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arab L, Tseng C-H, Ang A, Jardack P (2011) Validity of a Multipass, Web-based, 24-Hour Self-Administered Recall for Assessment of Total Energy Intake in Blacks and Whites. Am J Epidemiol kwr224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arif AA, Rohrer JE (2005) Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988–1994. BMC Public Health 5:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry AE, Piazza-Gardner AK (2012) Drunkorexia: Understanding the Co-occurrence of Alcohol Consumption and Eating/Exercise Weight Management Behaviors. J Am Coll Health 60:236–243. [DOI] [PubMed] [Google Scholar]
- Bendsen NT, Christensen R, Bartels EM, Kok FJ, Sierksma A, Raben A, Astrup A (2013) Is beer consumption related to measures of abdominal and general obesity? a systematic review and meta-analysis. Nutr Rev 71:67–87. [DOI] [PubMed] [Google Scholar]
- Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ (2006) The USDA Automated Multiple-Pass Method Accurately Estimates Group Total Energy and Nutrient Intake. J Nutr 136:2594–2599. [DOI] [PubMed] [Google Scholar]
- Bobak M, Skodova Z, Marmot M (2003) Beer and obesity: a cross-sectional study. Eur J Clin Nutr 57:1250–1253. [DOI] [PubMed] [Google Scholar]
- Bodenlos JS, Gengarelly K, Smith R (2015) Gender differences in freshmen weight gain. Eat Behav 19:1–4. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR (2003) Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med 163:821–829. [DOI] [PubMed] [Google Scholar]
- Breslow RA, Smothers BA (2005) Drinking patterns and body mass index in never smokers: National Health Interview Survey, 1997–2001. Am J Epidemiol 161:368–376. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, Murphy S (2008) A Developmental Perspective on Alcohol and Youths 16 to 20 Years of Age. Pediatrics 121:S290–S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke SC, Cremeens J, Vail-Smith K, Woolsey C (2010) Drunkorexia: Calorie Restriction Prior to Alcohol Consumption among College Freshman. J Alcohol Drug Educ 54:17–34. [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 158:1789–1795. [DOI] [PubMed] [Google Scholar]
- Butler SM, Black DR, Blue CL, Gretebeck RJ (2004) Change in diet, physical activity, and body weight in female college freshman. Am J Health Behav 28:24–32. [DOI] [PubMed] [Google Scholar]
- Buzzard IM, Faucett CL, Jeffery RW, McBane L, McGovern P, Baxter JS, Shapiro AC, Blackburn GL, Chlebowski RT, Elashoff RM, Wynder EL (1996) Monitoring dietary change in a low-fat diet intervention study: advantages of using 24-hour dietary recalls vs food records. J Am Diet Assoc 96:574–579. [DOI] [PubMed] [Google Scholar]
- Cawley J, Meyerhoefer C (2012) The medical care costs of obesity: An instrumental variables approach. J Health Econ 31:219–230. [DOI] [PubMed] [Google Scholar]
- Chakraborty S (2014) Analysis of NHANES 1999–2002 data reveals noteworthy association of alcohol consumption with obesity. Ann Gastroenterol Q Publ Hell Soc Gastroenterol 27:250–257. [PMC free article] [PubMed] [Google Scholar]
- Cluskey M, Grobe D (2009) College weight gain and behavior transitions: male and female differences. J Am Diet Assoc 109:325–329. [DOI] [PubMed] [Google Scholar]
- Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ (2003) Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr 77:1171–1178. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bauer DJ (2011) The Disaggregation of Within-Person and Between-Person Effects in Longitudinal Models of Change. Annu Rev Psychol 62:583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Saha TD, Grant BF (2015) Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug Alcohol Depend 148:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Timary P, Cani PD, Duchemin J, Neyrinck AM, Gihousse D, Laterre P-F, Badaoui A, Leclercq S, Delzenne NM, Stärkel P (2012) The Loss of Metabolic Control on Alcohol Drinking in Heavy Drinking Alcohol-Dependent Subjects. PLoS ONE 7:e38682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vos P, Hanck C, Neisingh M, Prak D, Groen H, Faas MM (2015) Weight gain in freshman college students and perceived health. Prev Med Rep 2:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deforche B, Van Dyck D, Deliens T, De Bourdeaudhuij I (2015) Changes in weight, physical activity, sedentary behaviour and dietary intake during the transition to higher education: a prospective study. Int J Behav Nutr Phys Act 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deliens T, Clarys P, Van Hecke L, De Bourdeaudhuij I, Deforche B (2013) Changes in weight and body composition during the first semester at university. A prospective explanatory study. Appetite 65:111–116. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Carey KB (2012) Optimizing the use of the AUDIT for alcohol screening in college students. Psychol Assess 24:954–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinger MK, Behrens TK, Han JL (2006) Validity and Reliability of the International Physical Activity Questionnaire in College Students. Am J Health Educ 37:337–343. [Google Scholar]
- Dishman R, Steinhardt M (1988) Reliability and concurrent validity for a 7-d re-call of physical activity in college students. Med Sci Sports Exerc 20:14–25. [DOI] [PubMed] [Google Scholar]
- Economos CD, Hildebrandt ML, Hyatt RR (2008) College Freshman Stress and Weight Change: Differences by Gender. Am J Health Behav 32:16–25. [DOI] [PubMed] [Google Scholar]
- Fazzino T, Fleming K, Sher K, Sullivan D, Befort C (2017) Heavy Drinking in Young Adulthood Increases Risk of Transitioning to Obesity. Am J Prev Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazzino TL, Martin CK, Forbush K (2018) The Remote Food Photography Method and SmartIntake App for the Assessment of Alcohol Use in Young Adults: Feasibility Study and Comparison to Standard Assessment Methodology. JMIR MHealth UHealth 6:e10460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, Wildes JE, Hunt TK (2014) Gender norms, psychometric properties, and validity for the Eating Pathology Symptoms Inventory. Int J Eat Disord 47:85–91. [DOI] [PubMed] [Google Scholar]
- Forbush KT, Wildes JE, Pollack LO, Dunbar D, Luo J, Patterson K, Petruzzi L, Pollpeter M, Miller H, Stone A, Bright A, Watson D (2013) Development and validation of the Eating Pathology Symptoms Inventory (EPSI). Psychol Assess 25:859–878. [DOI] [PubMed] [Google Scholar]
- Jung ME, Bray SR, Martin Ginis KA (2008) Behavior change and the freshman 15: tracking physical activity and dietary patterns in 1st-year university women. J Am Coll Health J ACH 56:523–530. [DOI] [PubMed] [Google Scholar]
- Kasparek DG, Corwin SJ, Valois RF, Sargent RG, Morris RL (2008) Selected health behaviors that influence college freshman weight change. J Am Coll Health J ACH 56:437–444. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick SI, Subar AF, Douglass D, Zimmerman TP, Thompson FE, Kahle LL, George SM, Dodd KW, Potischman N (2014) Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am J Clin Nutr 100:233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leischner K, McCormack LA, Britt BC, Heiberger G, Kattelmann K (2018) The Healthfulness of Entrées and Students’ Purchases in a University Campus Dining Environment. Healthcare 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitsky DA, Halbmaier CA, Mrdjenovic G (2004) The freshman weight gain: a model for the study of the epidemic of obesity. Int J Obes 28:1435–1442. [DOI] [PubMed] [Google Scholar]
- Levitsky DA, Youn T (2004) The more food young adults are served, the more they overeat. J Nutr 134:2546–2549. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson EE, Lucero ML, Dibello JR, Jacobson AE, Wing RR (2008) The relationship between alcohol use, eating habits and weight change in college freshmen. Eat Behav 9:504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohman TG, Roche AF (1988) Anthropometric Standardization Reference Manual. Champaign, IL, Human Kinetics Pub. [Google Scholar]
- Long J (2011) Longitudinal Data Analysis for the Behavioral Sciences Using R. Thousand Oaks, CA, SAGE Publications, Inc. [Google Scholar]
- Lukasiewicz E, Mennen LI, Bertrais S, Arnault N, Preziosi P, Galan P, Hercberg S (2005) Alcohol intake in relation to body mass index and waist-to-hip ratio: the importance of type of alcoholic beverage. Public Health Nutr 8:315–320. [DOI] [PubMed] [Google Scholar]
- Miller ET, Neal DJ, Roberts LJ, Baer JS, Cressler SO, Metrik J, Marlatt GA (2002) Test-Retest Reliability of Alcohol Measures: Is There a Difference Between Internet-Based Assessment and Traditional Methods? Psychol Addict Behav 16:56–63. [PubMed] [Google Scholar]
- Morrow ML, Heesch KC, Dinger MK, Hull HR, Kneehans AW, Fields DA (2006) Freshman 15: Fact or Fiction? Obesity 14:1438–1443. [DOI] [PubMed] [Google Scholar]
- Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, Staples RC, Cleveland LE (2008) The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 88:324–332. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (1998) Mplus User’s Guide. Los Angeles, CA, Muthén & Muthén. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (2005) Helping Patients Who Drink Too Much: A Clinician’s Guide Updated Edition. [Google Scholar]
- Nelson MC, Lust K, Story M, Ehlinger E (2009) Alcohol use, eating patterns, and weight behaviors in a university population. Am J Health Behav 33:227–237. [DOI] [PubMed] [Google Scholar]
- Nikolaou CK, Hankey CR, Lean MEJ (2014) Weight changes in young adults: a mixed-methods study. Int J Obes 2005. [DOI] [PubMed] [Google Scholar]
- Patrick Megan E, Terry‐McElrath Yvonne M (2016) High‐intensity drinking by underage young adults in the United States. Addiction 112:82–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Grow J, Duncan S, Neighbors C, Larimer ME (2012) Concurrent validity of an online version of the Timeline Followback assessment. Psychol Addict Behav J Soc Psychol Addict Behav 26:672–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pliner P, Saunders T (2008) Vulnerability to freshman weight gain as a function of dietary restraint and residence. Physiol Behav 93:76–82. [DOI] [PubMed] [Google Scholar]
- Pope L, Hansen D, Harvey J (2017) Examining the Weight Trajectory of College Students. J Nutr Educ Behav 49:137–141.e1. [DOI] [PubMed] [Google Scholar]
- Ptomey LT, Herrmann SD, Lee J, Sullivan DK, Rondon MF, Donnelly JE (2013) Photo-assisted recall increases estimates of energy and macronutrient intake in adults with intellectual and developmental disabilities. J Acad Nutr Diet 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptomey LT, Willis EA, Goetz JR, Lee J, Sullivan DK, Donnelly JE (2015) Digital photography improves estimates of dietary intake in adolescents with intellectual and developmental disabilities. Disabil Health J 8:146–150. [DOI] [PubMed] [Google Scholar]
- Roache JD, Karns TE, Hill-Kapturczak N, Mullen J, Liang Y, Lamb RJ, Dougherty DM (2015) Using Transdermal Alcohol Monitoring to Detect Low-Level Drinking. Alcohol Clin Exp Res 39:1120–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption: II. Addiction 88:791–804. [DOI] [PubMed] [Google Scholar]
- Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M (2011) Alcohol consumption and body weight: a systematic review. Nutr Rev 69:419–431. [DOI] [PubMed] [Google Scholar]
- Schrieks IC, Stafleu A, Griffioen-Roose S, de Graaf C, Witkamp RF, Boerrigter-Rijneveld R, Hendriks HFJ (2015) Moderate alcohol consumption stimulates food intake and food reward of savoury foods. Appetite 89:77–83. [DOI] [PubMed] [Google Scholar]
- Serra-Majem L, Santana-Armas JF, Ribas L, Salmona E, Ramon JM, Colom J, Salleras L (2002) A comparison of five questionnaires to assess alcohol consumption in a Mediterranean population. Public Health Nutr 5:589–594. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M (2008) Alcohol Timeline Followback (TLFB) In: Textbook of Psychiatric Measures , pp 477–479. Washington DC, American Psychiatric Association. [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB (1996) The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend 42:49–54. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline Follow-Back: A Technique for Assessing Self-Reported Alcohol Consumption. Litten Raye Allen Z John P 41–72. [Google Scholar]
- Subar AF, Kirkpatrick SI, Mittl B, Zimmerman TP, Thompson FE, Bingley C, Willis G, Islam NG, Baranowski T, McNutt S, Potischman N (2012) The Automated Self-Administered 24-Hour Dietary Recall (ASA24): A Resource for Researchers, Clinicians and Educators from the National Cancer Institute. J Acad Nutr Diet 112:1134–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter PM (2005) Is alcohol consumption a risk factor for weight gain and obesity? Crit Rev Clin Lab Sci 42:197–227. [DOI] [PubMed] [Google Scholar]
- Thomson CA, Wertheim BC, Hingle M, Wang L, Neuhouser ML, Gong Z, Garcia L, Stefanick ML, Manson JE (2012) Alcohol consumption and body weight change in postmenopausal women: results from the Women’s Health Initiative. Int J Obes 2005 36:1158–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolstrup JS, Halkjaer J, Heitmann BL, Tjønneland AM, Overvad K, Sørensen TIA, Grønbaek MN (2008) Alcohol drinking frequency in relation to subsequent changes in waist circumference. Am J Clin Nutr 87:957–963. [DOI] [PubMed] [Google Scholar]
- Tolstrup JS, Heitmann BL, Tjønneland AM, Overvad OK, Sørensen TIA, Grønbaek MN (2005) The relation between drinking pattern and body mass index and waist and hip circumference. Int J Obes 2005 29:490–497. [DOI] [PubMed] [Google Scholar]
- Traversy G, Chaput J-P (2015) Alcohol Consumption and Obesity: An Update. Curr Obes Rep 4:122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trogdon JG, Finkelstein EA, Hylands T, Dellea PS, Kamal-Bahl SJ (2008) Indirect costs of obesity: a review of the current literature. Obes Rev 9:489–500. [DOI] [PubMed] [Google Scholar]
- Vella-Zarb RA, Elgar FJ (2009) The “freshman 5”: a meta-analysis of weight gain in the freshman year of college. J Am Coll Health J ACH 58:161–166. [DOI] [PubMed] [Google Scholar]
- Vereecken CA, Covents M, Sichert-Hellert W, Alvira JMF, Le Donne C, De Henauw S, De Vriendt T, Phillipp MK, Béghin L, Manios Y, Hallström L, Poortvliet E, Matthys C, Plada M, Nagy E, Moreno LA, HELENA Study Group (2008) Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int J Obes 2005 32 Suppl 5:S26–34. [DOI] [PubMed] [Google Scholar]
- Wang L, Lee I-M, Manson JE, Buring JE, Sesso HD (2010) Alcohol Consumption, Weight Gain, and Risk of Becoming Overweight in Middle-aged and Older Women. Arch Intern Med 170:453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee SG, Field AE, Colditz GA, Rimm EB (2004) Alcohol intake and 8-year weight gain in women: a prospective study. Obes Res 12:1386–1396. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG, Whincup PH (2005) Alcohol and adiposity: effects of quantity and type of drink and time relation with meals. Int J Obes 2005 29:1436–1444. [DOI] [PubMed] [Google Scholar]
- Wengreen HJ, Moncur C (2009) Change in diet, physical activity, and body weight among young-adults during the transition from high school to college. Nutr J 8:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Withrow D, Alter DA (2011) The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev 12:131–141. [DOI] [PubMed] [Google Scholar]
- Yeomans M, Bertenshaw E (2008) Appetite and food intake: A human exprimental perspective In: Appetite and Food Intake: Behavioral and Physiological Considerations (Harris R, Mattes R eds). [Google Scholar]
- Yeomans MR (2010a) Alcohol, appetite and energy balance: Is alcohol intake a risk factor for obesity? Physiol Behav, Beverages and Health 100:82–89. [DOI] [PubMed] [Google Scholar]
- Yeomans MR (2010b) Short term effects of alcohol on appetite in humans. Effects of context and restrained eating. Appetite 55:565–573. [DOI] [PubMed] [Google Scholar]
- Zagorsky JL, Smith PK (2011) The Freshman 15: A Critical Time for Obesity Intervention or Media Myth? Soc Sci Q 92:1389–1407. [Google Scholar]