Abstract
Objective
To examine associations between health insurance coverage, income level and contraceptive use — overall and most/moderately effective method use — among women ages 18–44 at risk of pregnancy, within and across 41 United States jurisdictions in 2017.
Study design
Using data from the 2017 Behavioral Risk Factor Surveillance System, we calculated the proportions of women using any contraceptive method and using a most or moderately effective method for each state/territory and across all jurisdictions, categorized by health insurance coverage and income groups. For both contraceptive use outcomes, we ran simple and multivariable logistic regression models to test for significant differences in outcomes between insured and uninsured individuals.
Results
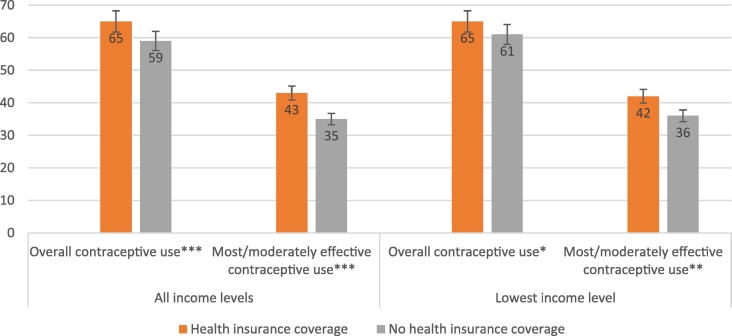
Across jurisdictions, compared to uninsured women, those who had health care coverage had higher levels of contraceptive use (65% versus 59%; p < .001) and most/moderately effective contraceptive use (43% compared to 35%; p < .001); low-income women with coverage also had higher levels of contraceptive use (64% versus 61%; p < .05) and most or moderately effective contraceptive use (42% versus 36%; p < .01) than their uninsured counterparts. Controlling for individual-level demographic characteristics, health insurance coverage was associated with increased odds of most or moderately effective contraceptive use across jurisdictions (adjusted odds ratio = 1.33, p < .01). In 11 states, insured women had significantly higher odds of at least one contraceptive use metric than their uninsured counterparts.
Conclusions
Variation in contraceptive use across the states likely reflects broader demographic, social and structural differences across state and local populations. States' political will and support around contraceptive access likely play a role in individuals' ability to obtain and use contraception.
Implications
Our key finding that insurance coverage is significantly associated with use of most/moderately effective contraceptive methods across the states but not any contraceptive use underscores the importance of health insurance in aiding access to methods that are more costly and often require a visit to a health care provider.
Keywords: Contraceptive use, Behavioral Risk Factor Surveillance System, Method mix, Health insurance coverage, United States
1. Introduction
Across the United States, the use of contraception is ubiquitous among sexually active individuals. As of 2013, 99% of women ages 15–44 who had ever had sex reported using some form of contraception [1], and as of the most recent national data, over 72 million women ages 15–49 (65% of all American women in this age group) were using some form of contraception in 2016 [2]. While these national-level data are helpful in understanding an overall picture of contraceptive use for the country as a whole, varying patterns of use among individuals at the state level could inform state-specific initiatives supporting contraceptive access for individuals seeking to prevent pregnancy. A recent state-level analysis demonstrated that a majority of women of reproductive age in every state use some form of contraception, although method-specific rates of use show wide variability across the states, especially for female sterilization, intrauterine devices (IUDs), oral contraceptives and condoms [3].
Notably, health insurance coverage is a key factor related to contraceptive use that varies widely across states of residence. At the national level, women with health insurance are more likely to use contraception than those who are uninsured. Further, compared to privately insured women, uninsured women are more likely to use less effective, coital methods like condoms and withdrawal [4], [5].
Many changes related to health insurance — especially those that may influence contraceptive use — have occurred since the last, most comprehensive subnational estimates of contraceptive use were available for 2004 [6]. The implementation of the Affordable Care Act (ACA) has expanded individuals' access to health insurance coverage broadly [7], [8], [9], [10]; since 2013, when many of the law's major coverage provisions went into effect, the percentage of uninsured women of reproductive age has declined significantly in nearly every state [10]. The ACA also increased the number of states that expanded their state Medicaid coverage to cover millions more low-income individuals seeking health care. Individuals with health insurance coverage now have access to contraception without cost-sharing, achieved by those with private insurance through the ACA's preventive services requirement (which includes contraception in a list of key preventive services that needs to be covered without cost-sharing) [11] and by those with Medicaid coverage through long-standing federal law [12].
Using the most recently available state-level data on contraceptive use from 2017, we examine the association between health insurance coverage and contraceptive use, taking into account income level, among women ages 18–44 at risk for pregnancy in each of the jurisdictions in the United States with available data.
2. Materials and methods
2.1. Data
This analysis used data from the 2017 Behavioral Risk Factor Surveillance System (BRFSS). Annually, BRFSS provides cross-sectional data on various health-related topics for all 50 US states, the District of Columbia, Guam, Puerto Rico and the US Virgin Islands. Surveys are administered by trained interviewers over the phone throughout the year and are representative of the noninstitutionalized adult population within each state and territory. The median combined response rate for all 2017 BRFSS samples was 45.9%, with the rate ranging from 30.6% in Illinois to 64.1% in Wyoming [13].
Along with the core survey, comprised of a fixed set of standardized questions asked uniformly across jurisdictions, BRFSS also allows states and territories to administer optional modules approved by the Centers for Disease Control and Prevention (CDC). One such optional module, the Preconception Health/Family Planning module, includes questions about reproductive health indicators. This analysis drew on data from the Preconception Health/Family Planning module to examine contraceptive use and risk of pregnancy. As such, our analysis is limited to 42 of the 43 jurisdictions that administered the module.⁎ The 43rd jurisdiction, US Virgin Islands, included the Preconception Health/Family Planning module in the 2017 BRFSS, but we did not include these data in the analysis because the sample size was too small to allow for reliable estimates. Module data for all jurisdictions are publicly available, except for Illinois and Kentucky. In these two states, data collection timelines for the Preconception Health/Family Planning module differed from the other jurisdictions; we therefore obtained data for these two states through a special request to the state survey administrators. More detailed information on BRFSS methodology, data collection, sampling design and procedures is available elsewhere [14], [15], [16].
The full BRFSS sample across the focus states included 63,803 women† aged 18–49. We limited our analytic sample to women aged 18–44 who were at risk for pregnancy. Women were defined as at risk for pregnancy if they reported being sexually active with one or more male partners the last time they had sex, had not had a hysterectomy, and were not pregnant or postpartum. Individuals who indicated “same sex partner” as a reason for not doing anything to prevent pregnancy at last sex were considered at risk of pregnancy given the possibility of them having had a male partner in close proximity to their last sex and evidence indicating that people who identify as a sexual minority are at higher risk for unintended pregnancy [17], [18], [19], [20], [21], [22].
2.2. Analysis
Our two key outcomes of interest were contraceptive use at last sex and use of most or moderately effective contraceptive methods at last sex. On the BRFSS questionnaire, respondents who report having been sexually active in the past year and indicate that they did something to prevent pregnancy the last time they had sex are asked to report the contraceptive method they used. Most and moderately effective contraceptive methods in this analysis were loosely categorized based on the CDC tiers of effectiveness model [23] and generally require women's contact with the health care system to obtain. This category includes the following methods: female sterilization,‡ IUDs, implants, pills, the patch, the ring and injectables. Given the focus of our analysis on understanding associations between health insurance coverage and contraceptive use, our key independent variables included health insurance coverage and income levels (because people with lower income have less ability to pay for care out of pocket in the absence of health insurance coverage).§ Household income was collected as a categorical variable in the BRFSS. The 12% of female respondents aged 18–44 at risk of pregnancy who did not report household income were excluded from the analysis.⁎⁎ The final analytic sample included 27,818 women aged 18–44 who were at risk for pregnancy with reported incomes. We calculated income levels by dividing the median of the reported household income band by the sum of adults and children reported to be living in the household at the time of interview [24].†† The overall distribution of income levels was stratified into three groups: low, medium and high income, an approach adopted by other researchers using BRFSS income data [25]. Individual health insurance coverage was assessed by asking respondents if they had any kind of health insurance, including prepaid plans such as HMOs and government plans such as Medicaid, or coverage through the Indian Health Service at the time of interview.
All analyses were conducted using Stata version 15.1. Because of BRFSS's multistage, probability-based complex sample design, we applied sampling weights that yield estimates representative of resident women aged 18–49 within each state or territory. In addition, we used design variables for the sampling stratum and cluster to obtain correct standard errors for all estimates. For each jurisdiction, we calculated the overall proportion of women using any contraceptive method by health insurance coverage and income groups. We did the same for most and moderately effective contraceptive method use. For both contraceptive use outcomes, simple logistic regression models testing significance of differences in contraceptive use between insured and uninsured individuals, overall and low income, were run for jurisdictions with income data available for at least 50 individuals per jurisdiction. For jurisdictions with less than 50 individuals who fell into either contraceptive use outcome according to their income and insurance characteristics, we suppressed model results in the tables given the instability of calculations using such small numbers. For the two simple logistic regression models testing significance of difference in each of our two contraceptive use outcomes between insured and uninsured individuals, overall and low income, across jurisdictions, women in all jurisdictions were included in these models.
Next, we constructed two multivariable logistic regression models for each jurisdiction, examining the association between the key independent variable of health insurance coverage at the time of interview and our outcomes of interest: (1) any contraceptive use and (2) most or moderately effective contraceptive method use. Both models control for income, age, race/ethnicity, education level, marital status and, given their association, the interaction between income and insurance coverage.
3. Results
Across the 42 US jurisdictions included in our analysis, most women aged 18–44 at risk of pregnancy used a contraceptive method at last intercourse (64%), ranging from 55% in Kentucky to 72% in Maine (Table 1). Across jurisdictions, women at risk of pregnancy who had health care coverage had higher levels of contraceptive use than their uninsured counterparts (65% versus 59%; p < .001). This pattern held in 18 of the 25 states where reliable estimates were obtained for both insured and uninsured women. The largest gaps in contraceptive use between insured and uninsured women (14–24 percentage points) occurred in Florida, Idaho, Missouri and Ohio. Among low-income women in particular, the population that stands to benefit most from health insurance coverage, those with coverage also had higher rates of overall contraceptive use than did those without health insurance coverage across the jurisdictions (64% versus 61%; p < .05).
Table 1.
Percentage of women at risk of pregnancy, aged 18–44, using contraception, by health insurance coverage and household income, BRFSS 2017
| Among all women at risk of pregnancy (%) | Insured (%) |
Uninsured (%) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Low income | Medium income | High income | All | Low income | Medium income | High income | ||
| Kentucky | 55 | 55 | 52 | 57 | 63 | - | - | - | - |
| Delaware | 56 | 56 | 54 | 63 | 48 | 58 | 72 | - | - |
| Arizona | 58 | 60 | 61 | 58 | 64 | 51 | 50 | - | - |
| Hawaii | 59 | 60 | 59 | 63 | 54 | - | - | - | - |
| Ohio | 59 | 61 | 61 | 59 | 62 | 37** | - | - | - |
| Texas | 59 | 60 | 66 | 48 | 63 | 57 | 56 | - | - |
| Illinois | 59 | 61 | 66 | 56 | - | - | - | - | - |
| Nevada | 60 | 60 | 55 | 67 | - | - | - | - | - |
| Idaho | 61 | 65 | 68 | 62 | - | 49 | 47* | - | - |
| Nebraska | 61 | 62 | 62 | 63 | - | 56 | 54 | - | - |
| Mississippi | 62 | 60 | 55 | 65 | - | 66 | - | - | - |
| Missouri | 62 | 65 | 65 | 60 | 77 | 50* | 53 | - | - |
| Wisconsin | 62 | 61 | 66 | 56 | 62 | - | - | - | - |
| Georgia | 62 | 64 | 75 | 58 | 61 | 54 | 57* | - | - |
| Louisiana | 62 | 66 | 63 | 67 | - | - | - | - | - |
| Florida | 63 | 67 | 67 | 68 | 65 | 50** | 55 | 47 | - |
| Connecticut | 63 | 64 | 59 | 64 | 77 | - | - | - | - |
| West Virginia | 63 | 64 | 66 | 61 | - | - | - | - | - |
| Minnesota | 63 | 64 | 57 | 64 | 70 | 52* | 49 | - | - |
| Kansas | 63 | 64 | 67 | 61 | 61 | 61 | 62 | - | - |
| Oklahoma | 63 | 63 | 64 | 58 | - | - | - | - | - |
| Indiana | 64 | 65 | 65 | 64 | 70 | 55 | 63 | - | - |
| Utah | 64 | 64 | 63 | 65 | 67 | 62 | 62 | - | - |
| District of Columbia | 64 | 65 | 60 | 69 | 68 | - | - | - | - |
| Wyoming | 64 | 65 | 69 | 63 | 63 | 60 | - | - | - |
| Alabama | 64 | 66 | 72 | 58 | - | 58 | 58 | - | - |
| Iowa | 65 | 64 | 67 | 61 | 65 | 65 | - | - | - |
| Puerto Rico | 65 | 65 | 65 | 59 | - | - | - | - | - |
| Maryland | 65 | 67 | 66 | 62 | 80 | - | - | - | - |
| Oregon | 66 | 66 | 68 | 62 | 73 | - | - | - | - |
| North Carolina | 66 | 66 | 64 | 68 | 63 | 65 | 67 | - | - |
| New Jersey | 66 | 67 | 69 | 64 | 68 | 63 | 64 | - | - |
| South Carolina | 66 | 67 | 67 | 68 | 67 | 61 | 70 | - | - |
| Virginia | 67 | 67 | 71 | 63 | 68 | 63 | 71 | - | - |
| New York | 67 | 66 | 64 | 66 | 73 | 73 | 71 | - | - |
| Massachusetts | 67 | 67 | 66 | 67 | 69 | - | - | - | - |
| South Dakota | 67 | 66 | 65 | 63 | 78 | 79 | - | - | - |
| California | 68 | 68 | 65 | 70 | 76 | 71 | 71 | - | - |
| New Mexico | 69 | 69 | 70 | 64 | - | 71 | 71 | - | - |
| Alaska | 70 | 70 | 60 | 77 | - | - | - | - | - |
| Pennsylvania | 71 | 71 | 66 | 74 | 75 | - | - | - | - |
| Maine | 72 | 71 | 73 | 68 | - | - | - | - | - |
| Total | 64 | 65 | 65 | 64 | 68 | 59*** | 61* | 55 | 48 |
Notes: Simple logistic regression models testing significance of differences in contraceptive use between insured and uninsured individuals, overall and low income, were run for jurisdictions with income data available for at least 50 individuals per jurisdiction. For jurisdictions with less than 50 individuals who were contraceptive users within certain income and insurance categories, we suppressed model results given the instability of calculations using such small numbers. For the two simple logistic regression models testing significance of difference in contraceptive use between insured and uninsured individuals, overall and low income, across jurisdictions, women in all jurisdictions were included in these models. ***p < .001, **p < .01, *p < .05.
Overall across the 42 jurisdictions with available data, two-fifths (42%) of all women ages 18–44 at risk of pregnancy used one of the most or moderately effective contraceptive methods that require contact with the health system at last intercourse (Table 2). Women at risk of pregnancy who had health insurance coverage used most and moderately effective contraceptive methods at higher levels than did their uninsured counterparts (43% compared to 35%; p < .001). This pattern held in 20 of the 25 states where reliable estimates were obtained for most and moderate contraceptive use for both insured and uninsured women. The largest gaps in most and moderate contraceptive use between insured and uninsured women (13–22 percentage points) occurred in Florida, Indiana, Nebraska and Ohio. Among low-income women in particular, those with coverage also had higher rates of most and moderately effective contraceptive use than did those without health insurance overage across the jurisdictions (42% versus 36%; p < .01).
Table 2.
Percentage of women at risk of pregnancy, aged 18–44, using most or moderately effective contraception, by health insurance coverage and household income, BRFSS 2017
| Among all women at risk of pregnancy (%) | Insured (%) |
Uninsured (%) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Low income | Medium income | High income | All | Low income | Medium income | High income | ||
| District of Columbia | 28 | 29 | 22 | 33 | 32 | - | - | - | - |
| Illinois | 34 | 36 | 37 | 38 | - | - | - | - | - |
| Texas | 34 | 34 | 37 | 27 | 34 | 35 | 35 | - | - |
| New York | 37 | 38 | 37 | 38 | 42 | 33 | 32 | - | - |
| Arizona | 38 | 40 | 40 | 38 | 40 | 30 | 29* | - | - |
| Delaware | 38 | 37 | 34 | 43 | 32 | 46 | 54 | - | - |
| Georgia | 38 | 40 | 45 | 39 | 35 | 32 | 37 | - | - |
| Louisiana | 38 | 40 | 39 | 40 | - | - | - | - | - |
| New Jersey | 39 | 40 | 40 | 40 | 40 | 33 | 37 | - | - |
| Kentucky | 39 | 40 | 37 | 41 | 49 | - | - | - | - |
| Florida | 40 | 45 | 44 | 46 | 44 | 23*** | 24* | 22 | - |
| Ohio | 40 | 41 | 44 | 40 | 40 | 27 | - | - | - |
| Connecticut | 40 | 41 | 36 | 41 | 55 | - | - | - | - |
| Hawaii | 41 | 42 | 41 | 45 | 32 | - | - | - | - |
| Maryland | 41 | 43 | 42 | 39 | 54 | - | - | - | - |
| South Carolina | 42 | 43 | 39 | 46 | 54 | 32 | 37 | - | - |
| Nebraska | 42 | 44 | 44 | 44 | - | 31 | 32 | - | - |
| Missouri | 42 | 43 | 39 | 44 | 53 | 37 | 40 | - | - |
| Mississippi | 42 | 42 | 40 | 44 | - | 41 | - | - | - |
| California | 42 | 42 | 39 | 46 | 49 | 45 | 44 | - | - |
| Virginia | 43 | 44 | 48 | 42 | 43 | 35 | 41 | - | - |
| Idaho | 43 | 46 | 48 | 42 | - | 33 | 32 | - | - |
| Kansas | 44 | 44 | 50 | 39 | 41 | 38 | 41* | - | - |
| Indiana | 44 | 46 | 44 | 46 | 55 | 31** | 36 | - | - |
| Minnesota | 44 | 45 | 39 | 44 | 52 | 36 | 31 | - | - |
| Wisconsin | 45 | 44 | 46 | 41 | 50 | - | - | - | - |
| Alaska | 45 | 46 | 48 | 44 | - | - | - | - | - |
| Nevada | 45 | 46 | 45 | 46 | - | - | - | - | - |
| Utah | 45 | 46 | 44 | 48 | 48 | 40 | 38 | - | - |
| Alabama | 46 | 46 | 48 | 43 | - | 43 | 45 | - | - |
| South Dakota | 46 | 45 | 46 | 39 | 58 | 53 | - | - | - |
| Oregon | 47 | 47 | 51 | 40 | 52 | - | - | - | - |
| North Carolina | 48 | 48 | 53 | 47 | 34 | 45 | 46 | - | - |
| Pennsylvania | 49 | 49 | 44 | 54 | 53 | - | - | - | - |
| Oklahoma | 49 | 52 | 55 | 46 | - | - | - | - | - |
| Iowa | 49 | 49 | 49 | 49 | 48 | 47 | - | - | - |
| West Virginia | 49 | 49 | 50 | 51 | - | - | - | - | - |
| Puerto Rico | 49 | 49 | 51 | 26 | - | - | - | - | - |
| Massachusetts | 50 | 51 | 55 | 52 | 46 | - | - | - | - |
| Wyoming | 50 | 51 | 52 | 49 | 52 | 47 | - | - | - |
| New Mexico | 51 | 51 | 54 | 45 | - | 52 | 53 | - | - |
| Maine | 57 | 57 | 59 | 55 | - | - | - | - | - |
| Total | 42 | 43 | 42 | 43 | 44 | 35*** | 36** | 31 | 28 |
Notes: Most or moderately effective contraception includes female sterilization, LARC or hormonal contraception. Simple logistic regression models testing significance of differences in most or moderately effective contraceptive use between insured and uninsured individuals, overall and low income, were run for jurisdictions with income data available for at least 50 individuals per jurisdiction. For jurisdictions with less than 50 individuals who were most or moderately effective contraceptive method users within certain income and insurance categories, we suppressed model results given the instability of calculations using such small numbers. For the two simple logistic regression models testing significance of difference in most or moderately effective contraceptive use between insured and uninsured individuals, overall and low income, across jurisdictions, women in all jurisdictions were included in these models. ***p < .001, **p < .01, *p < .05.
In bivariate analyses, by both contraceptive use metrics across US jurisdictions, insurance is significantly associated with higher levels of contraceptive use, especially among low-income individuals at risk of pregnancy (Fig. 1).
Fig. 1.
Differences in contraceptive use, overall and most/moderately effective method use, among women ages 18-44 at risk of pregnancy across 42 US jurisdictions, by health insurance coverage and income level, BRFSS 2017.
Controlling for several individual-level demographic characteristics potentially associated with contraceptive use, we found no significant association between health insurance coverage and use of any method of contraception among women ages 18–44 at risk of pregnancy across US jurisdictions (Table 3). In contrast, we did find a significant association between health insurance coverage and use of most and moderately effective contraceptive methods among women ages 18–44 at risk of pregnancy across US jurisdictions [adjusted odds ratio (AOR) = 1.33]. In 11 states (Alabama, Arizona, Florida, Georgia, Hawaii, Idaho, Kansas, Louisiana, Nebraska, Ohio and Oklahoma), insured women ages 18–44 at risk of pregnancy had significantly higher odds of either any contraceptive method use or specific use of most or moderately effective forms of contraception than their uninsured counterparts.
Table 3.
Adjusted odds ratios and confidence intervals representing associations between health insurance coverage and contraceptive method use, any and most/moderately effective method use, among women at risk of pregnancy, aged 18–44 years old, by jurisdiction,a BRFSS 2017
| Use of any contraceptive method |
Use of most and moderately effective contraceptive methodb |
|||
|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | |
| Alabama | 2.27 | (1.11, 4.63) | 1.34 | (0.66, 2.73) |
| Alaska | 0.95 | (0.22, 4.07) | 1.25 | (0.26, 6.00) |
| Arizona | 1.63 | (0.97, 2.75) | 2.00 | (1.15, 3.48) |
| California | 0.57 | (0.30, 1.08) | 0.70 | (0.40, 1.23) |
| Connecticut | 1.28 | (0.48, 3.42) | 1.90 | (0.69, 5.26) |
| Delaware | 0.52 | (0.18, 1.53) | 0.46 | (0.16, 1.32) |
| District of Columbia | 2.44 | (0.39, 15.29) | 2.25 | (0.18, 28.39) |
| Florida | 2.14 | (1.08, 4.24) | 2.75 | (1.31, 5.77) |
| Georgia | 2.81 | (1.22, 6.45) | 2.33 | (1.03, 5.29) |
| Hawaii | 3.73 | (1.27, 10.91) | 5.89 | (1.48, 23.35) |
| Idaho | 2.88 | (1.22, 6.80) | 1.90 | (0.80, 4.46) |
| Illinois | 2.48 | (0.78, 7.88) | 4.33 | (0.92, 20.38) |
| Indiana | 0.97 | (0.52, 1.80) | 1.24 | (0.72, 2.15) |
| Iowa | 1.75 | (0.69, 4.45) | 1.87 | (0.77, 4.55) |
| Kansas | 1.30 | (0.86, 1.96) | 1.49 | (1.01, 2.19) |
| Kentucky | 0.76 | (0.17, 3.39) | 2.11 | (0.56, 7.94) |
| Louisiana | 2.88 | (1.21, 6.88) | 2.02 | (0.77, 5.26) |
| Maine | 1.23 | (0.32, 4.67) | 2.16 | (0.57, 8.12) |
| Maryland | 0.89 | (0.26, 3.07) | 1.43 | (0.44, 4.64) |
| Massachusetts | 0.60 | (0.09, 3.82) | 0.86 | (0.15, 4.86) |
| Minnesota | 1.17 | (0.53, 2.60) | 1.01 | (0.49, 2.11) |
| Mississippi | 0.55 | (0.20, 1.46) | 0.89 | (0.33, 2.41) |
| Missouri | 1.68 | (0.79, 3.57) | 1.08 | (0.52, 2.24) |
| Nebraska | 2.03 | (0.91, 4.53) | 2.26 | (1.01, 5.04) |
| Nevada | 1.12 | (0.34, 3.64) | 2.65 | (0.86, 8.20) |
| New Jersey | 0.97 | (0.40, 2.37) | 1.00 | (0.43, 2.33) |
| New Mexico | 1.18 | (0.49, 2.81) | 1.18 | (0.54, 2.58) |
| New York | 0.77 | (0.36, 1.65) | 1.60 | (0.80, 3.20) |
| North Carolina | 0.99 | (0.38, 2.61) | 1.17 | (0.48, 2.81) |
| Ohio | 4.88 | (1.53, 15.56) | 2.52 | (0.81, 7.81) |
| Oklahoma | 1.12 | (0.41, 3.01) | 2.66 | (1.03, 6.86) |
| Oregon | 2.28 | (0.84, 6.19) | 1.03 | (0.42, 2.55) |
| Pennsylvania | 0.89 | (0.27, 2.92) | 1.95 | (0.48, 8.02) |
| Puerto Rico | 0.83 | (0.41, 1.66) | 1.05 | (0.56, 1.99) |
| South Carolina | 0.40 | (0.10, 1.58) | 0.93 | (0.29, 2.98) |
| South Dakota | 1.48 | (0.76, 2.91) | 1.09 | (0.57, 2.07) |
| Texas | 0.64 | (0.37, 1.08) | 0.86 | (0.50, 1.47) |
| Utah | 1.21 | (0.52, 2.80) | 1.45 | (0.68, 3.10) |
| Virginia | 1.10 | (0.40, 3.04) | 0.67 | (0.22, 2.06) |
| West Virginia | 0.75 | (0.20, 2.81) | 0.78 | (0.29, 2.12) |
| Wisconsin | 0.78 | (0.25, 2.42) | 1.51 | (0.53, 4.31) |
| Wyoming | 1.25 | (0.22, 6.95) | 2.31 | (0.24, 22.15) |
| Total | 1.19 | (0.99, 1.44) | 1.33 | (1.11, 1.59) |
Each model tests the relationship between the dependent variables of contraceptive use, any and most/moderately effective method use, and the key independent variable of health insurance coverage within jurisdications and across jurisdictions. Models control for income, insurance*income interaction, age, race/ethnicity, education level and relationship status. Adjusted odds ratios in bold represent tests producing significant differences in the outcome.
Most and moderately effective methods include female sterilization, IUDs, implants, pills, patch, ring and injectables.
4. Discussion
Several national studies have demonstrated that health insurance is key to increasing access to health care and decreasing delays in desired services [26], [27], [28]. Additional evidence indicates that health insurance coverage plays a key role in influencing variation in unintended pregnancy rates across states; in 2006 analyses of state-level data, increased rates of unintended pregnancy were associated with higher proportions of uninsured women, while decreased rates of unintended pregnancy were associated with higher proportions of women receiving Medicaid coverage in states [29]. Our study contributes to the literature by using state-specific data to demonstrate that health insurance coverage may be a key factor influencing contraceptive use, especially among low-income women at risk of pregnancy using methods that require connecting to the health care system, like long-acting reversible contraception (LARC) methods and shorter-acting hormonal methods such as the pill, patch, injectables and ring.
Our key finding that insurance coverage is significantly associated with use of most and moderately effective contraceptive methods across the states but not any contraceptive use underscores the importance of health insurance coverage in aiding access to methods that are more costly and often require a visit to a health care provider. Insurance coverage may facilitate users to shift between methods, especially from less expensive (and less effective) ones like condoms and withdrawal, more than driving a shift from nonusers to users of contraception.
Medicaid expansion programs represent one example of state initiatives that may significantly improve access to and use of contraceptive use generally, and the more effective methods available only through health care providers specifically, by increasing eligibility levels for health insurance and, thus, numbers of individuals with coverage. The ACA's Medicaid expansions — which offer full-benefit Medicaid coverage to people with incomes up to 138% of the federal poverty level in states that have taken up this option — have led to increases in both health insurance coverage and access to health care services for state residents, particularly among low-income and other vulnerable populations. [10], [30]
In addition, many states, starting in the 1990s, have expanded Medicaid in a more targeted way by offering coverage only for family planning and related services to individuals who are ineligible for full-benefit Medicaid coverage, usually for individuals below a specific income level (an “income-based Medicaid family planning expansion”). Contraceptive use among women broadly [31] and in abortion care settings [32] is higher among those who live in states with income-based Medicaid family planning expansion programs as compared to use among those who do not. Further, a number of state program evaluations have also found increases in overall contraceptive use and the use of most/moderately effective contraception as well as improved continuity of contraceptive use between the time prior to and following states' establishment of a family planning expansion program [33].
Progress demonstrated by these and other initiatives to increase and improve health insurance coverage for reproductive-aged individuals may stall or slide backwards given recent federal efforts to undermine the ACA and Medicaid [34]. The number of US residents who were uninsured increased in 2018, for the first time since the ACA was enacted [35]. An ongoing lawsuit, Texas v. U.S., could overturn the ACA entirely, resulting in millions more people losing coverage and eliminating important protections such as the federal contraceptive coverage guarantee [36]. In addition, the current administration has worked to undermine the contraceptive coverage guarantee directly by establishing broad exemptions for employers with religious or moral objections to contraception; those exemptions have been blocked by federal courts thus far, but if allowed to go into effect, some privately insured people could lose coverage for some or all contraceptive methods [37].
One potential strategy to mitigate inequitable access to contraception among uninsured and underinsured individuals is to provide broad access to contraceptive services through Title X, the federally funded family planning program expressly created to support the provision of contraceptive and broader sexual and reproductive health-related services to low-income and young people [38]. However, our findings indicate that the presence of this program in every state is not enough to realize the goal of securing full contraceptive access regardless of insurance coverage or ability to pay. In fact, Title X grant money is designed to supplement, not replace, insurance, and Title X clinics rely on Medicaid and private insurance for 50% of their program revenue [39]. Given recent changes to regulations guiding the Title X program that undermine the original intent behind its creation [40], it is likely that other strategies — specifically at the state level — may continue to be needed to reduce gaps in contraceptive use based on health insurance coverage.
Our findings are subject to several limitations, many of which are inherent to the study design of the BRFSS. Response rates to surveys administered over the phone are typically lower than in-person ones [41], [42], and these low response rates may be associated with underrepresentation of several demographic groups, especially some of those that we focus on in our models (racial/ethnic minorities and young people) [43]. Household income level, in particular, had high item nonresponse; this variable was missing for 12% of the analytic sample. Some individuals enrolled in a Medicaid family planning expansion program but who are otherwise uninsured may have been represented within the uninsured category of health insurance coverage in BRFSS. As a result, our finding of an association between health insurance coverage and contraceptive use may be an underestimate, especially in states with large proportions of the population covered through these family planning expansion programs, like California. In addition to the self-report nature of contraceptive use in BRFSS possibly being subject to response bias, assessment of this measure in the BRFSS allows for only one method used at a single point in time (last sex) to be recorded by the interviewer, despite growing evidence indicating that many individuals employ more complex contraceptive strategies than using just one method at each coital act [44], [45]. The wording of the BRFSS contraceptive use item also points respondents who report being sexually active in the past year only to the last time that they had sex; no time frame was provided to limit respondents as to how far back in time the last act of intercourse may have occurred (e.g., within the last 3 months or last year).
Variation in contraceptive use across the states, especially in use by health insurance status and income level, likely reflects broader demographic, social and structural differences across state and local populations. For example, the extent to which individuals may plan or want a pregnancy, and subsequent contraceptive use to achieve these pregnancy goals, varies widely across the states [46]. In addition, particularly in today's climate in which federal support for family planning services is in question, states' political will and support around contraceptive access likely play a key role in individuals' ability to obtain and use contraception. Further research is needed to broaden understanding as to how factors at each of these levels may enable or hinder individuals in their desires and ability to access and use their preferred contraceptive method.
Acknowledgments
Acknowledgments
The authors gratefully acknowledge Kathryn Kost, Adam Sonfield, and Rebecca Wind for reviewing early versions of this manuscript.
Funding
Support for this study was provided by an anonymous donor.
Conflicts of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Jurisdictions included in our analysis include Alabama, Alaska, Arizona, California, Connecticut, Delaware, District of Columbia, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, Puerto Rico, South Carolina, South Dakota, Texas, Utah, Virginia, West Virginia, Wisconsin and Wyoming. The US Virgin Islands were excluded because of a low number of observations.
All respondents were asked at the time of the interview to identify their sex as male or female in the Demographic section of the core questionnaire, except if they already self-identified their sex in the landline household enumeration. Only individuals self-identifying as female are included in our sample. Of note, sex assigned at birth was asked in 28 jurisdictions that implemented the BRFSS Sexual Orientation and Gender Identity (SOGI) module. In the 22 jurisdictions that implemented both the Preconception Health/Family Planning module and the SOGI module, approximately 1% of individuals who identified as female in the core questionnaire identified as either male to female transgender, gender nonconforming, stated they were unsure or refused to answer whether they considered themselves to be transgender. These individuals are included in our study sample.
Although the CDC categorization of most and moderately effective methods of contraception includes male sterilization (vasectomy), given our analytic focus on methods that may be influenced by a user's own health insurance coverage, we excluded partner use of vasectomy in our calculations of overall contraceptive use and use of most/moderate contraception.
We also ran these analyses including a state-level variable representing Medicaid expansion program status (present/absent) in our models, which we found to have no significant impact on either contraceptive outcome. Given a state's Medicaid expansion program status really being a proxy for expanded insurance coverage among individuals within a state, we chose to present the simpler and more direct association between insurance coverage at the state level and our contraceptive use outcomes.
Analyses were conducted including and excluding respondents with missing income data; differences in contraceptive prevalence estimates and (adjusted) odds ratios were negligible.
The number of children in the household was assumed to be zero and the number of adults in the household was assumed to be one for cases where this information was missing.
References
- 1.Centers for Disease Control and Prevention (CDC). NSFG – listing C – key statistics from the National Survey of Family Growth 2019. https://www.cdc.gov/nchs/nsfg/key_statistics/c.htm accessed September 6, 2019.
- 2.Daniels K, Abma JC. National Center for Health Statistics; Hyattsville, MD: 2018. Current contraceptive status among women aged 15–49: United States, 2015–2017. [Google Scholar]
- 3.Douglas-Hall A, Kost K, Kavanaugh ML. Guttmacher Institute; New York: 2018. State-level estimates of contraceptive use in the United States, 2017. [Google Scholar]
- 4.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States. 2004 Perspect Sex Reprod Health. 2008;40:94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 5.Jones RK, Lindberg LD, Higgins JA. Pull and pray or extra protection? Contraceptive strategies involving withdrawal among US adult women. Contraception. 2014;90:416–421. doi: 10.1016/j.contraception.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Centers for disease control and Prevention; 2004. Behavioral Risk Factor Surveillance System 2004 state questionnaire. [Google Scholar]
- 7.Collins SR, Bhupal HK, Doty MM. Commonwealth Fund; New York: 2019. Health insurance coverage eight years after the ACA: fewer uninsured Americans and shorter coverage gaps, but more underinsured. [Google Scholar]
- 8.Berchick ER, Hood E, Barnett JC. Government Printing Office, Washington, DC; U.S. Census Bureau: 2018. Health insurance coverage in the United States: 2017. U.S. [Google Scholar]
- 9.Cohen RA, Zammitti EP, Martinez ME. Health insurance coverage: early release of estimates from the National Health Interview Survey, 2016. Washington, DC: National Center for Health Statistics. 2017:A1–A31. Available from: https://www.cdc.gov/nchs/nhis/releases.htm. [Google Scholar]
- 10.Gains in insurance coverage for reproductive-age women at a crossroads. Guttmacher Inst 2018. https://www.guttmacher.org/article/2018/12/gains-insurance-coverage-reproductive-age-women-crossroads (accessed May 20, 2019).
- 11.Sobel L, Salganicoff A, Gomez I. Henry J. Kaiser Family Foundation; Washington, DC: 2018. State and federal contraceptive coverage requirements: implications for women and employers. [Google Scholar]
- 12.Office of the Federal Register National Archives and Records Administration as a Special Edition of the Federal Register. Code of federal regulations: title 42 public health. vol. 42 CFR 441.20. 1996.
- 13.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta, GA: 2018. The Behavioral Risk Factor Surveillance System 2017 summary data quality report. [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta, GA: 2018. Behavioral Risk Factor Surveillance System. Overview: BRFSS 2017. [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta, GA: 2013. The BRFSS Data User Guide, 2013; pp. 1–10. [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta, GA: 2018. The Behavioral Risk Factor Surveillance System: Complex Sampling Weights and Preparing 2017 BRFSS Module Data for Analysis. [Google Scholar]
- 17.Kann L, O'Malley Olsen E, McManus T, Shanklin SL, Flint KH, Queen B, et al. Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12 — United States and selected sites, 2015. MMWR Surveill Summ 2016;65. [DOI] [PubMed]
- 18.Johns MM, Lowry, Richard, Andrzejewski J, Barrios LC, Demissie Z, McManus T, et al. Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students — 19 states and large urban school districts, 2017. MMWR Morb Mortal Wkly Rep 2019;68. [DOI] [PMC free article] [PubMed]
- 19.Charlton BM, Roberts AL, Rosario M, Katz-Wise SL, Calzo JP, Spiegelman D. Teen pregnancy risk factors among young women of diverse sexual orientations. Pediatrics. 2018;141 doi: 10.1542/peds.2017-2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartnett CS, Lindley LL, Walsemann KM. Congruence across sexual orientation dimensions and risk for unintended pregnancy among adult U.S. women. Womens Health Issues 2017;27:145–151.e2. [DOI] [PubMed]
- 21.Tornello SL, Riskind RG, Sexual Orientation PCJ. Sexual and reproductive health among adolescent young women in the United States. J Adolesc Health. 2014;54:160–168. doi: 10.1016/j.jadohealth.2013.08.018. [DOI] [PubMed] [Google Scholar]
- 22.Blunt-Vinti HD, Thompson EL, Griner SB. Contraceptive use effectiveness and pregnancy prevention information preferences among heterosexual and sexual minority college women. Womens Health Issues. 2018;28:342–349. doi: 10.1016/j.whi.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services. Effectiveness of family planning methods 2011 https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/pdf/Contraceptive_methods_508.pdf (accessed October 31, 2019).
- 24.Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:1241–1247. doi: 10.15585/mmwr.mm6645a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zimmerman FJ, Anderson NW. Trends in health equity in the United States by race/ethnicity, sex, and income, 1993-2017. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.6386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported Insurance coverage, access to care, and health under the affordable care act. J Am Med Assoc JAMA. 2015;314:366–374. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 27.Hoffman C, Health Insurance PJ. Access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–160. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 28.Fox J, Richards C. Vital Signs: Health insurance coverage and health care utilization — United States, 2006–2009 and January–March 2010. MMWR Morb Mortal Wkly Rep 2010;59:1–7. [PubMed]
- 29.Kost K, Finer LB, Singh S. Variation in state unintended pregnancy rates in the United States. Perspect Sex Reprod Health. 2012;44:57–64. doi: 10.1363/4405712. [DOI] [PubMed] [Google Scholar]
- 30.Antonisse L, Garfield R, Rudowitz R, Artiga S. San Francisco, California; Henry J. Kaiser Family Foundation: 2018. The effect of Medicaid expansion under the ACA: updated findings from a literature review. [Google Scholar]
- 31.Kearney MS, Subsidized Contraception LPB. Fertility, and sexual behavior. Rev Econ Stat. 2009;91:137–151. doi: 10.1162/rest.91.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thompson KMJ, Speidel JJ, Saporta V, Waxman NJ, Harper CC. Contraceptive policies affect post-abortion provision of long-acting reversible contraception. Contraception. 2011;83:41–47. doi: 10.1016/j.contraception.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 33.Sonfield A, Benson GR. New York, NY; Guttmacher Institute: 2011. Medicaid family planning expansions: lessons learned and implications for the future. [Google Scholar]
- 34.Center on Budget and Policy Priorities. Sabotage watch: tracking efforts to undermine the ACA 2019. https://www.cbpp.org/sabotage-watch-tracking-efforts-to-undermine-the-aca [accessed September 17, 2019].
- 35.Casselman B, Sanger-Katz M, Smialek J. N Y Times. 2019. Share of Americans with health insurance declined in 2018. [Google Scholar]
- 36.Musumeci M. Kais Fam Found. 2019. Explaining Texas v. U.S.: a guide to the 5th circuit appeal in the case challenging the ACA. [Google Scholar]
- 37.Sonfield A. Despite leaving key questions unanswered. New Contraceptive Coverage Exemptions Will Do Clear Harm. Health Aff Blog. 2017 [Google Scholar]
- 38.Hasstedt K. New York, NY; Guttmacher Institute: 2019. Shoring up reproductive autonomy: Title X’s foundational role. [Google Scholar]
- 39.Fowler C, Gable J, Wang J, Lasater B, Wilson E. Research Triangle Park, NC; RTI International: 2019. Title X family planning annual report: 2018 national summary. [Google Scholar]
- 40.Hasstedt K. What the Trump administration's final regulatory changes mean for Title X | Guttmacher Institute. 2019. https://www.guttmacher.org/article/2019/03/what-trump-administrations-final-regulatory-changes-mean-title-x
- 41.Czajka JL, Beyler A. Mathematica Policy Research; Washington, DC: 2016. Declining response rates in federal surveys: trends and implications (background paper) [Google Scholar]
- 42.Pierannunzi C, Hu SS. Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13 doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schneider KL, Clark MA, Rakowski W, Lapane KL. Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS) J Epidemiol Community Health. 2012;66:290–295. doi: 10.1136/jech.2009.103861. [DOI] [PubMed] [Google Scholar]
- 44.Frohwirth L, Blades N, Moore AM, Wurtz H. The complexity of multiple contraceptive method use and the anxiety that informs it: implications for theory and practice. Arch Sex Behav. 2016;45:2123–2135. doi: 10.1007/s10508-016-0706-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Parr N, Siedlecky S. Use of “dual protection” and other combinations of contraceptive methods in Australia. Aust N Z J Public Health. 2007;31:567–570. doi: 10.1111/j.1753-6405.2007.00145.x. [DOI] [PubMed] [Google Scholar]
- 46.Kost K, Maddow-Zimet I, Kochhar S. New York, NY; Guttmacher Institute: 2018. Pregnancy desires and pregnancy at the state level: estimates for 2014. [Google Scholar]