Abstract
Objectives
To describe the types of contraception used by women attending Title X-funded clinics and a comparable group of low-income reproductive-age women at risk of unintended pregnancy.
Study design
We estimated the percentage of reproductive aged (15–44 years) women using contraception, by method type and level of effectiveness in preventing pregnancy (i.e., most, moderately, and less effective), using Title X Family Planning Annual Report (2006–2016) and National Survey of Family Growth (2006–2015) data. We divided most effective methods into permanent (female and male sterilization) and reversible (long-acting reversible contraceptives [LARCs]) methods.
Results
Among Title X clients during 2006–2016, use of LARCs increased (3–14%); use of moderately effective methods decreased (64–54%); and use of sterilization (~ 2%), less effective methods (21–20%), and no method (8–7%) was unchanged. These same trends in contraceptive use were observed in a comparable group of women nationally during 2006–2015, during which LARC use increased (5–19%, p < .001); moderately effective method use decreased (60–48%, p < .001); and use of sterilization (~5%), less effective methods (19%), and no method (11–10%) was unchanged.
Conclusions
The contraceptive method mix among Title X clients differs from that of low-income women at risk of unintended pregnancy nationally, but general patterns and trends are similar in the two populations. Research is needed to understand whether method use patterns among low-income women reflect their preferences, access, or the conditions of the supply environment.
Implications
This study contributes to our understanding of patterns and trends in contraceptive use among two groups of reproductive-age women — Title X clients and low-income women nationally who are at risk of unintended pregnancy. The findings highlight areas for further research.
Keywords: Contraception, Unintended pregnancy, Title X, Publicly funded family planning, United States
1. Introduction
Improving pregnancy spacing and preventing unintended pregnancy are national health objectives [1]. Contraception, used correctly and consistently, is one strategy for achieving these objectives [2], and the US Food and Drug Administration (FDA) has approved a range of safe, effective methods to satisfy the preferences, medical considerations, and other needs of most women [3]. A full range of FDA-approved methods, however, may not be accessible to all women, especially those at higher risk of unintended pregnancy (e.g., 18–24, cohabiting, poor and low-income, or minority) [4]. Barriers — geographic, economic, administrative, cognitive (awareness and knowledge), and psychosocial (stigma or confidentiality concerns) [5]—may limit access to the most effective contraceptive methods [6], [7], thereby reducing the number of acceptable options and increasing the risk of unintended pregnancy.
Publicly funded family planning clinics play an important role in meeting the contraceptive service needs of US women. In 2014, an estimated 20.2 million US women needed (i.e., were sexually active, fecund, and not pregnant or seeking pregnancy) publicly funded services because of their young age (< 20) or low income. Of this total, 39% received care in a publicly funded clinic, including 19% who received care in a clinic funded by the Title X National Family Planning Program [8]. Title X is the only federal grant program dedicated solely to providing people with comprehensive family planning and related preventive health services, with priority for providing care to individuals from low-income families [9], [10].
Many publicly funded family planning clinics offer their clients a broad range of contraceptive methods. A 2015 survey found that 77% of all publicly funded clinics and 88% of Title X-funded clinics reported offering at least 10 different reversible methods, and 59% of all clinics and 72% of Title X clinics reported meeting the Healthy People 2020 objective of offering on site the full range of FDA-approved reversible contraceptives [11]. The distribution of contraceptive methods provided to or used by women who attend publicly funded family planning clinics remains unstudied, as does how this distribution compares with self-reported contraceptive use by a similar group of women nationally who are at risk of unintended pregnancy.
The purpose of this study is to describe the patterns and trends in contraceptive use among women at risk of unintended pregnancy who attend Title X-funded family planning clinics. We also examine patterns and trends in contraceptive use among a nationally representative sample of US women for comparison, focusing specifically on low-income women at risk of unintended pregnancy who reported receiving contraceptive services in the previous 12 months.
2. Materials and methods
We used multiyear data from the Title X Family Planning Annual Report (FPAR) for 2006–2016 and from the National Survey of Family Growth (NSFG) for 2006–2015.
2.1. Title X Family Planning Annual Report
FPAR is an annual reporting requirement of all Title X grantees that are funded, as part of a competitive award process [12], to provide contraceptive education, counseling, and services; breast and cervical cancer screening; sexually transmitted disease (STD) and HIV testing, referral, and prevention education; and pregnancy diagnosis and counseling [13]. Grantees aggregate for their network of subrecipients and services sites and report on FPAR the following data: client sociodemographic characteristics, contraceptive method used or adopted at exit from the encounter, receipt of related preventive health services, staffing, and revenue [12]. During each year of the study period, the Title X service network included an average of 91 grantees, 1,151 subrecipients, and 4,251 service sites and served 4.7 million clients (92% of whom were female) [14]. A Title X client is defined as an individual who had at least one face-to-face encounter (i.e., visit) within the calendar year during which they received services related to achieving or preventing pregnancy [12].
2.2. National Survey of Family Growth
The NSFG is a nationally representative survey of reproductive-age women and men living in US households. The survey collects information on sexual activity, pregnancy, childbearing, infertility, contraception, and various social and demographic characteristics, including age, race and ethnicity, annual household income and household size, and health insurance status. The survey also asks female respondents whether they received any contraceptive4 or other sexual or reproductive health service5 in the past 12 months. Household income as a percentage of the US Census Bureau poverty threshold is calculated for each respondent using household income and size and state of residence.
During the three cycles of NSFG used in this study (2006–2010, 2011–2013, and 2013–2015), female response rates were 78% (n = 12,279), 73% (n = 5,601), and 71% (n = 5,699), respectively; the age range of females included in the surveys was 15 to 44 years [15]. Detailed information about the NSFG is described elsewhere [16]. This analysis uses de-identified, public use data files.
2.3. Contraceptive prevalence
We examined contraceptive method prevalence by use of any method, use of an individual method, and use of a method according to its level of effectiveness in preventing pregnancy (i.e., most, moderately, and less effective) [17], [18]. All analyses were restricted to women considered at risk for unintended pregnancy.
2.3.1. Contraceptive prevalence based on individual methods
We calculated individual method prevalence using data on the single most effective contraceptive method used by a woman. In the FPAR, the single most effective method for a Title X client was the method already used or newly adopted at the time of her last family planning encounter of the year, as noted in her medical record. We are unable to differentiate between these two scenarios in the FPAR data. For clients using or adopting more than one type of method, FPAR captures the most effective one in terms of pregnancy prevention. Additionally, the FPAR groups “withdrawal” and “other methods” not listed in the FPAR reporting form (e.g., emergency contraception) into a single “withdrawal and other method” category.
In the NSFG data, individual method prevalence is based on the single most effective contraceptive method used by the woman during the month of the interview (CONSTAT1 variable) [19]. To align with emergency contraception reporting in the FPAR, we grouped women who reported using emergency contraception into a comparable “withdrawal and other method” category. For both sources of data, we grouped female barrier methods (female condom, diaphragm, cervical cap, contraceptive sponge, and spermicide) and other hormonal methods (injectable, ring, and patch) into single and separate categories.
2.3.2. Contraceptive prevalence based on method effectiveness
We calculated prevalence for each method effectiveness category by grouping the single most effective method used by each woman into one of five categories based on the method’s effectiveness in preventing pregnancy under typical use conditions [17], [18]. The five method effectiveness categories were most effective permanent (female and male sterilization); most effective reversible (long-acting reversible contraception [LARC]: implant and intrauterine device or system [IUD/IUS]); moderately effective (injectable, vaginal ring, contraceptive patch, pill, cervical cap, and diaphragm); less effective (male condom, female barrier methods, fertility awareness-based methods [FABM], lactational amenorrhea method, and withdrawal or other method); and no method (no method recorded).
2.3.3. Identifying women at risk of unintended pregnancy
We restricted the analysis of contraceptive prevalence to women at risk of unintended pregnancy (“at risk”). In the FPAR data, all female Title X clients were considered at risk if they were not pregnant or seeking pregnancy. We assumed that most, if not all, of at-risk Title X clients were sexually active and not known to be infecund because they had to have had at least one encounter in the reporting year aimed at preventing unintended pregnancy or achieving pregnancy to be included in the FPAR. We further restricted the Title X study population to women 15–44 to align with the NSFG population during 2006–2015. In the NSFG data, women were considered at risk if they had had vaginal sex with a male in the past 3 months and were not pregnant, seeking pregnancy, or infertile for noncontraceptive or unknown reasons.
To make the two study populations more comparable, we restricted the NSFG sample to low-income women 15–44 who reported receiving any contraceptive service (birth control method/prescription, check-up, or counseling; sterilization counseling or procedure; or emergency contraception counseling or prescription) in the past year; we also excluded women who were sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income.
2.4. Analytic strategy
The NSFG data include the following 2-year, mutually exclusive survey periods: 2006–2008, 2008–2010, 2011–2013, and 2013–2015. We pooled the FPAR data by year (2006–2007, 2008–2010, 2011–2013, and 2014–2016) to match, to the extent possible, these NSFG survey periods. Contraceptive use data for the same Title X client may appear more than once in the pooled FPAR data if she made at least one visit in more than one of the calendar years in the pooled period. For example, if a Title X client had a family planning encounter in 2006 and 2007, her contraceptive use data would appear twice in the pooled period, but her method in each year might be different. “Study period” refers to 2006–2016 for FPAR and 2006–2015 for NSFG. “Current period” refers to 2014–2016 for FPAR and 2013–2015 for NSFG.
For each time period and data source, we produced descriptive statistics for demographic and socioeconomic characteristics and assessed changes over time in these characteristics by calculating the percentage point change (increase or decrease) between the first and current periods. For NSFG estimates, we performed t tests to compare the differences in each characteristic between the first and current periods. Because the FPAR data are a census of Title X clients and not a sample, we did not produce confidence intervals or perform additional statistical tests for this population. For FPAR-based findings, we highlight and discuss changes (increase or decrease) of at least 5 percentage points between the first and current periods.
We estimated the percentages of at-risk women using contraception by individual method and method effectiveness category, overall (15–44 years) and for three age subgroups (15–19, 20–29, and 30–44 years). Then we assessed changes over time by calculating the percentage-point change in prevalence between the first (2006–07) and current (2014–16) periods for the Title X population. For NSFG-based estimates, we performed t tests to compare the differences between prevalence estimates in the first (2006–2008) and current (2013–2015) periods and presented 95% confidence intervals for overall (15–44 years) estimates by method effectiveness category and for selected individual methods in the figures. To guide the comparison of FPAR- and NSFG-based findings, we highlighted when the FPAR percentage did not fall within the 95% confidence interval of the NSFG estimate. We did not perform statistical testing between the two populations as they represented overlapping groups, and one was a census count while the other was a population-weighted sample. The reader should keep in mind that in the “Results” section our use of terms like “higher” or “lower” to describe differences in contraceptive prevalence between the two populations is not based on statistical comparisons between FPAR-based prevalence values and NSFG-based estimates. We use these terms simply to highlight potential differences between the two populations when the FPAR prevalence value falls above or below the confidence interval for the NSFG-based estimate. As noted earlier, statistical comparisons between these two data sources are not possible. We used SAS 9.4 [20] and SUDAAN 11 [21] and accounted for NSFG’s complex survey design using population weights and design variables.
3. Results
3.1. Study population characteristics
Compared with low-income, at-risk women nationally in 2013–2015, higher percentages of female Title X clients in 2014–2016 had incomes below the poverty level (66% vs. 42%) or were uninsured (49% vs. 19%), and lower percentages were privately insured (16% vs. 49%) or non-Hispanic white (37% vs. 50%) (Table 1). Over the study period (2006–2016), the percentage of the Title X population comprised of teenagers decreased, while the percentages aged 30–39 or Hispanic increased. Additionally, the percentages of women with Medicaid and private insurance increased, while the percentage with no insurance decreased. Among low-income, at-risk women nationally, most (63%) relied on a private physician or health maintenance organization (HMO) for contraceptive care. The characteristics of at-risk women nationally were not significantly different over the study period, except for an increase in the percentage relying on physicians or HMOs for contraceptive care.
Table 1.
Percentage (weighted) distribution of female Title X clients and a comparablea national sample of low-income women at risk of unintended pregnancy,b by selected characteristics: FPAR (2006–2016) and NSFG (2006–2015)
| Family Planning Annual Report |
National Survey of Family Growth |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population (N) or sample (n) size | 2006–07 |
2008–10 |
2011–13 |
2014–16 |
% point change 2006–07 vs. 2014–16 | 2006–08 |
2008–10 |
2011–13 |
2013–15 |
2006–08 vs. 2013–15 % point change and p-value† |
Chi-square test (p-value)‡ | ||||
|
N = 8.2 million |
N = 12.4 million |
N = 11.3 million |
N = 9.2 million |
n = 1,052c |
n = 1,213c |
n = 1,109c |
n = 1,037c |
||||||||
| % | % | % | % | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | ||||
| Age | |||||||||||||||
| 15–19 | 25.6 | 23.6 | 20.0 | 18.5 | –7.1 | 21.3 | (18.5, 24.4) | 22.4 | (20.0, 25.1) | 18.4 | (16.0, 21.1) | 18.4 | (15.5, 21.7) | –2.9 | .15 |
| 20–29 | 52.7 | 53.2 | 53.4 | 51.8 | –0.8 | 53.7 | (49.0, 58.4) | 48.4 | (43.9, 52.9) | 52.0 | (48.1, 55.9) | 52.6 | (47.7, 57.5) | –1.1 | |
| 30–39 | 17.6 | 18.9 | 21.5 | 24.0 | 6.4 | 21.3 | (17.8, 25.3) | 25.3 | (21.4, 29.6) | 23.9 | (19.7, 28.7) | 23.2 | (19.2, 27.8) | 1.9 | |
| 40–44 | 4.1 | 4.4 | 5.1 | 5.7 | 1.5 | 3.7 | (2.3, 5.9) | 3.9 | (2.6, 5.8) | 5.7 | (3.5, 9.1) | 5.8 | (4.0, 8.4) | 2.1 | |
| Race/ethnicity | |||||||||||||||
| Hispanic | 25.3 | 27.9 | 29.1 | 31.6 | 6.4 | 21.2 | (14.1, 30.6) | 23.3 | (18.6, 28.8) | 24.6 | (19.5, 30.5) | 26.3 | (20.9, 32.6) | 5.1 | .88 |
| White, non-Hispanic | 47.8 | 43.7 | 41.0 | 37.0 | –10.8 | 54.3 | (46.0, 62.3) | 55.1 | (49.0, 61.1) | 49.7 | (43.9, 55.6) | 49.8 | (43.9, 55.7) | –4.5 | |
| Black, non-Hispanic | 18.2 | 18.6 | 18.8 | 19.5 | 1.2 | 16.4 | (11.5, 22.9) | 13.6 | (10.0, 18.3) | 18.0 | (14.4, 22.3) | 15.9 | (12.2, 20.5) | –0.5 | |
| Other/multiple, non-Hispanic | 4.9 | 5.2 | 5.6 | 5.7 | 0.9 | 8.1 | (4.4, 14.5) | 7.9 | (5.4, 11.4) | 7.7 | (4.6, 12.7) | 8.0 | (5.5, 11.5) | –0.1§ | |
| Income statusd | |||||||||||||||
| ≤ 100% FPL | 68.2 | 69.9 | 70.1 | 66.3 | –1.9 | 37.0 | (32.4, 41.8) | 35.5 | (31.5, 39.7) | 43.5 | (38.9, 48.2) | 42.1 | (37.7, 46.7) | 5.1 | .59 |
| 101%–150% FPL | 16.7 | 15.3 | 14.1 | 14.0 | –2.7 | 20.6 | (17.5, 24.1) | 20.3 | (17.3, 23.6) | 18.2 | (15.1, 21.8) | 19.0 | (16.1, 22.3) | –1.6 | |
| 151%–200% FPL | 6.2 | 5.4 | 5.3 | 6.0 | –0.2 | 18.7 | (15.8, 22.0) | 18.2 | (14.9, 22.0) | 16.1 | (12.9, 19.9) | 16.1 | (12.6, 20.4) | –2.6 | |
| 201%–250% FPL | 2.5 | 2.4 | 2.2 | 2.8 | 0.3 | 17.5 | (14.1, 21.5) | 18.5 | (15.6, 21.8) | 15.7 | (12.5, 19.6) | 16.5 | (12.8, 21.0) | –1.0 | |
| ≥ 251% FPL | 4.8 | 4.4 | 4.9 | 6.4 | 1.7 | 6.2 | (4.8, 8.0) | 7.4 | (5.5, 9.9) | 6.6 | (4.7, 9.1) | 6.4 | (4.3, 9.5) | 0.2§ | |
| Health insuranced | |||||||||||||||
| Medicaid or other public | 20.7 | 21.1 | 24.3 | 33.8 | 13.1 | 26.8 | (22.7, 31.3) | 30.1 | (25.3, 35.4) | 31.3 | (26.3, 36.8) | 31.8 | (27.3, 36.7) | 5.0 | .56 |
| Private | 8.5 | 8.6 | 9.3 | 15.6 | 7.1 | 49.2 | (43.7, 54.7) | 46.3 | (39.9, 52.8) | 44.6 | (39.2, 50.1) | 48.9 | (44.4, 53.4) | –0.3 | |
| None | 62.7 | 66.0 | 63.8 | 48.6 | –14.0 | 24.0 | (18.9, 29.9) | 23.6 | (19.6, 28.2) | 24.2 | (19.8, 29.2) | 19.3 | (14.9, 24.7) | –4.7 | |
| Source of contraceptive care | |||||||||||||||
| Publicly funded clinic, Title X | 100.0 | 100.0 | 100.0 | 100.0 | — | 21.6 | (17.3, 26.7) | 20.7 | (16.2, 26.0) | 19.1 | (15.5, 23.3) | 16.4 | (13.3, 20.0) | –5.1 | < .01 |
| Publicly funded clinic, non-Title X | — | — | — | — | — | 19.4 | (14.6, 25.2) | 17.2 | (14.0, 21.0) | 10.5 | (8.2, 13.3) | 15.7 | (12.6, 19.3) | –3.6 | |
| Physician/HMO | — | — | — | — | — | 55.7 | (50.6, 60.7) | 58.7 | (52.5, 64.6) | 65.5 | (60.7, 70.0) | 62.6 | (58.8, 66.2) | 6.9* | |
| Othere | — | — | — | — | — | 3.3 | (2.2, 5.0) | 3.3 | (2.0, 5.3) | 5.0 | (3.0, 8.3) | 5.2 | (3.7, 7.3) | 1.9§ | |
Abbreviations: FPAR, Family Planning Annual Report; FPL, federal poverty level; NSFG, National Survey of Family Growth; SE, standard error; HMO, health maintenance organization.
— Not applicable.
* < .05;
† Based on t test comparing estimates for first and current period.
‡ Based on chi-square test for difference by survey period.
§ Cell sizes are too small for significance testing.
Note: The size of the Title X age subgroups may not sum to the total because of rounding.
We restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
In the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
The weighted NSFG samples for females 15–44 years are 2006–08 (N = 9,143,000), 2008–10 (N = 10,520,000), 2011–13 (N = 10,345,000), 2013–15 (N = 10,425,000).
FPAR income and health insurance distributions include all Title X clients (female and male).
Other sources of contraceptive care include an employer or company clinic, hospital or urgent care, or “some other place.”
3.2. Contraceptive prevalence: any vs. no method
About the same percentages (90%) of at-risk Title X clients during 2014–2016 and women nationally during 2013–2015 were using any contraception, while a lower percentage of Title X clients (7%) than women nationally (10%) used no method (Table 2). Missing contraceptive use data for Title X clients may account for some of the difference in nonuse between the two groups. Finally, in both groups, there were no substantial changes in the use of any or no methods overall or by age subgroup over time.
Table 2.
Trends in contraceptive prevalence among female Title X clients and a comparablea national sample of low-income women at risk of unintended pregnancy,b by method use (any or no method) and method effectiveness category (most, moderately, or less effective), age group, and year: FPAR (2006–2016) and NSFG (2006–2015)
| Family Planning Annual Report |
National Survey of Family Growth |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006–07 |
2008–10 |
2011–13 |
2014–16 |
2006–07 vs. 2014–16 % point change | 2006–08 |
2008–10 |
2011–13 |
2013–15 |
2006–08 vs. 2013–15 % point change | |||||
| Population (N) or Sample (n) |
N = 8.2 million |
N = 12.4 million |
N = 11.3 million |
N = 9.2 million |
n = 1,052c |
n = 1,213c |
n = 1,109c |
n = 1.037c |
||||||
| % | % | % | % | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |||
| Any method | ||||||||||||||
| 15–44 | 88.9 | 88.1 | 91.5 | 90.1 | 1.1 | 89.3 | (86.5, 91.6) | 89.2 | (86.2, 91.6) | 89.5 | (86.7, 91.8) | 90.2 | (87.1, 92.6) | 0.9 |
| 15–19 | 89.1 | 88.3 | 91.9 | 90.4 | 1.3 | 84.1 | (77.3, 89.1) | 83.2 | (76.0, 88.5) | 86.9 | (80.3, 91.5) | 89.2 | (82.3, 93.6) | 5.2 |
| 20–29 | 89.5 | 88.7 | 92.1 | 91.2 | 1.6 | 91.4 | (87.8, 94.0 | 91.4 | (88.0, 93.9) | 90.6 | (87.5, 93.0) | 93.3 | (90.5, 95.3) | 1.9 |
| 30–44 | 87.2 | 86.5 | 90.1 | 87.9 | 0.7 | 89.3 | (81.8, 93.9) | 90.1 | (84.8, 93.7) | 89.4 | (84.0, 93.2) | 85.3 | (78.0, 90.4) | –4.0 |
| Most effective permanentd | ||||||||||||||
| 15–44 | 1.8 | 1.8 | 1.8 | 2.1 | 0.3 | 5.2 | (3.7, 7.3) | 7.8 | (5.7, 10.6) | 6.5 | (4.2, 10.0) | 5.1 | (3.5, 7.5) | –0.1 |
| 15–19 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | — | 0.0 | — | 0.0 | — | 0.0 | — | 0.0 |
| 20–29 | 0.8 | 0.8 | 0.7 | 0.6 | –0.2 | 4.1 | (2.5, 6.8) | 5.8 | (3.5, 9.4) | 4.1 | (2.4, 6.8) | 2.5 | (1.2, 4.9) | –1.7 |
| 30–44 | 6.2 | 5.8 | 5.5 | 5.9 | –0.3 | 12.0 | (7.1, 19.7) | 17.0 | (11.4, 24.5) | 14.9 | (8.4, 24.9) | 13.1 | (8.1, 20.5) | 1.1 |
| Most effective reversibled | ||||||||||||||
| 15–44 | 3.0 | 5.8 | 9.3 | 14.1 | 11.1 | 5.3 | (3.8, 7.4) | 13.0 | (10.1, 16.7) | 16.4 | (12.9, 20.5) | 18.7 | (15.0, 23.0) | 13.4⁎⁎⁎ |
| 15–19 | 0.7 | 2.4 | 5.3 | 11.2 | 10.4 | 2.2 | (0.7, 6.1) | 5.1 | (2.1, 11.6) | 3.9 | (1.1, 12.3) | 11.4 | (6.0, 20.5) | 9.2⁎ |
| 20–29 | 3.2 | 6.2 | 9.7 | 14.7 | 11.5 | 6.6 | (4.4, 9.8) | 14.9 | (11.1, 19.6) | 17.9 | (14.1, 22.6) | 21.8 | (17.1, 27.3) | 15.1⁎⁎⁎ |
| 30–44 | 5.5 | 8.4 | 11.6 | 15.0 | 9.6 | 5.1 | (2.7, 9.5) | 16.0 | (10.8, 23.1) | 21.4 | (13.8, 31.6) | 17.7 | (12.9, 23.8) | 12.5⁎⁎⁎ |
| Moderately effectivee | ||||||||||||||
| 15–44 | 63.6 | 60.5 | 58.8 | 54.2 | –9.4 | 60.1 | (56.0, 64.1) | 54.5 | (49.9, 58.9) | 51.3 | (47.3, 55.2) | 47.8 | (43.2, 52.5) | –12.3⁎⁎⁎ |
| 15–19 | 67.1 | 66.3 | 66.8 | 62.8 | –4.2 | 60.2 | (52.9, 67.1) | 63.6 | (55.6, 70.9) | 62.9 | (53.2, 71.6) | 61.4 | (51.7, 70.4) | 1.2 |
| 20–29 | 66.2 | 62.8 | 61.0 | 56.2 | –10.0 | 62.9 | (57.1, 68.3) | 55.3 | (48.7, 61.7) | 54.5 | (49.4, 59.6) | 48.9 | (43.4, 54.4) | –14.0⁎⁎⁎ |
| 30–44 | 53.3 | 49.4 | 48.2 | 45.4 | –7.9 | 54.2 | (46.3, 61.8) | 46.1 | (38.8, 53.6) | 38.4 | (31.1, 46.4) | 37.3 | (29.2, 46.1) | –16.9⁎⁎ |
| Less effectivef | ||||||||||||||
| 15–44 | 20.5 | 20.0 | 21.6 | 19.6 | –0.9 | 18.6 | (15.7, 22.0) | 13.9 | (11.8, 16.4) | 15.4 | (12.5, 18.8) | 18.6 | (15.4, 22.2) | 0.0 |
| 15–19 | 21.3 | 19.6 | 19.8 | 16.4 | –4.9 | 21.7 | (15.6, 29.3) | 14.6 | (10.1, 20.6) | 20.2 | (12.8, 30.4) | 16.4 | (10.6, 24.4) | –5.3 |
| 20–29 | 19.4 | 18.9 | 20.7 | 19.7 | 0.3 | 17.7 | (14.0, 22.2) | 15.4 | (12.4, 18.9) | 14.1 | (9.8, 19.7) | 20.2 | (16.4, 24.6) | 2.4 |
| 30–44 | 22.2 | 22.9 | 24.8 | 21.6 | –0.6 | 18.0 | (12.4, 25.3) | 11.0 | (7.9, 15.2) | 14.8 | (9.5, 22.3) | 17.2 | (12.1, 23.9) | –0.8 |
| No method | ||||||||||||||
| 15–44 | 8.1 | 6.9 | 6.2 | 6.8 | –1.3 | 10.7 | (8.4, 13.5) | 10.8 | (8.4, 13.8) | 10.5 | (8.2, 13.3) | 9.8 | (7.4, 12.9) | –0.9 |
| 15–19 | 8.1 | 7.1 | 5.9 | 6.8 | –1.3 | 15.9 | (10.9, 22.7) | 16.8 | (11.5, 24.0) | 13.1 | (8.5, 19.7) | 10.8 | (6.4, 17.7) | –5.2 |
| 20–29 | 7.8 | 6.5 | 5.7 | 6.1 | –1.6 | 8.6 | (6.0, 12.2) | 8.6 | (6.1, 12.0) | 9.4 | (7.0, 12.5) | 6.7 | (4.7, 9.5) | –1.9 |
| 30–44 | 8.9 | 7.8 | 7.2 | 8.0 | –0.9 | 10.7 | (6.1, 18.2) | 9.9 | (6.3, 15.2) | 10.6 | (6.8, 16.0) | 14.7 | (9.6, 22.0) | 4.0 |
| Missing | ||||||||||||||
| 15–44 | 3.0 | 5.0 | 2.3 | 3.1 | 0.1 | — | — | — | — | — | ||||
| 15–19 | 2.8 | 4.7 | 2.1 | 2.8 | 0.0 | — | — | — | — | — | ||||
| 20–29 | 2.7 | 4.8 | 2.2 | 2.7 | 0.0 | — | — | — | — | — | ||||
| 30–44 | 3.9 | 5.8 | 2.7 | 4.1 | 0.2 | — | — | — | — | — | ||||
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth; CI, confidence interval.
Note: The size of the Title X age subgroups may not sum to the total because of rounding.
— Not applicable.
< .001;
< .01;
< .05.
We restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
In the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
The weighted NSFG samples for females 15–44 years are 2006–08 (N = 9,143,000), 2008–10 (N = 10,520,000), 2011–13 (N = 10,345,000), 2013–15 (N = 10,425,000).
Most effective permanent methods include female and male (vasectomy) sterilization. Most effective reversible methods/LARCs include implants and IUDs.
Moderately effective methods include hormonal methods (injectables, vaginal ring, contraceptive patch, and pills) and cervical caps or diaphragms.
Less effective methods include male condoms, female barrier methods (female condom, sponge, and spermicide), fertility awareness-based methods (FABMs), lactational amenorrhea method (FPAR only), and withdrawal or “other” methods. EC is grouped with less effective methods in both the FPAR and NSFG data.
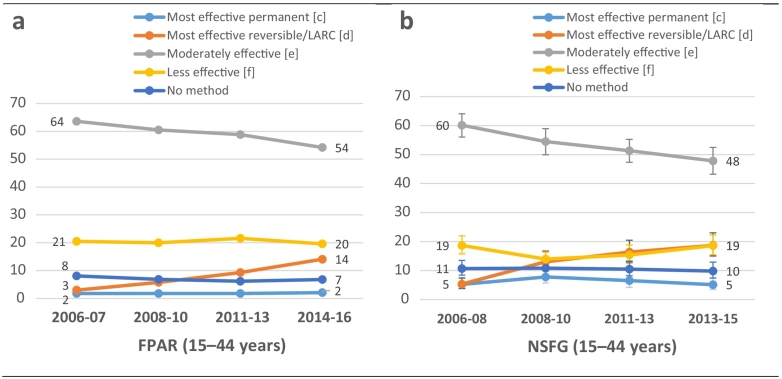
3.3. Contraceptive prevalence by method effectiveness
During 2014–2016, 2% of Title X clients overall (15–44 years) were using a most effective permanent method (i.e., sterilization) compared with 5% among women nationally in 2013–2015 (Table 2 and Fig. 1); sterilization use in either group did not change substantially between the first and current periods. The percentage of at-risk women using most effective reversible methods was lower among Title X clients than women nationally (14% vs. 19%), and in both groups use of these methods increased over time. Moderately effective methods were the most common type of methods used by both groups, but prevalence of these methods was higher among Title X clients than women nationally (54% vs. 48%). In addition, both groups experienced a decrease in the use of moderately effective methods over time. The percentages of women using less effective methods were similar for Title X clients (20%) and women nationally (19%), and in both groups prevalence between the first and current periods saw almost no change. Finally, although prevalence by method effectiveness category varied according to age subgroups — for example, most effective method use was lower in teenagers than older women — over the study period, trends for women overall (15–44 years) were generally consistent with those found within age subgroups.
Fig. 1.
Trends in the percentage of female Title X clients (a) and a comparablea national sample (b) of low-income women at risk of unintended pregnancyb who use a most effective permanent,c most effective reversible/LARC,d moderately effective,e less effective,f or no method of contraception, by year: FPAR (2006–2016)g and NSFG (2006–2015)h
NOTE:
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth; LARC, long-acting reversible contraceptive.
aWe restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
bIn the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
cMost effective permanent methods include female and male (vasectomy) sterilization.
dMost effective reversible/LARC methods include implants and IUDs.
eModerately effective methods include hormonal methods (injectables, vaginal ring, contraceptive patch, and pills) and cervical caps or diaphragms.
fLess effective methods include male condoms, female barrier methods (female condom, sponge, and spermicide), fertility awareness-based methods (FABMs), lactational amenorrhea method (FPAR only), and withdrawal or “other” methods. Emergency contraception (EC) is grouped with “less effective” methods in both the FPAR and NSFG data.
gThe FPAR populations for each period are as follows: 2006–07 (8,185,457), 2008–10 (12,390,516), 2011–13 (11,327,058), 2014–16 (9,245,609).
hNSFG samples for at-risk females aged 15–44 years are as follows: 2006–08 (unweighted = 1,052; weighted = 9,143,000), 2008–10 (unweighted = 1,213; weighted = 10,520,000), 2011–13 (unweighted = 1,109; weighted = 10,345,000), 2013–15 (unweighted = 1,037; weighted = 10,425,000).
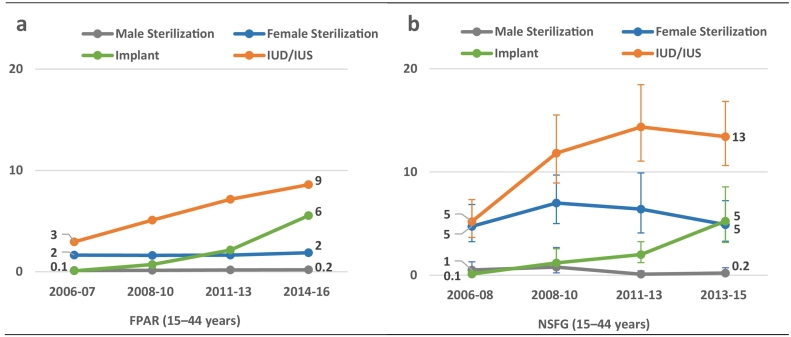
3.4. Contraceptive prevalence by individual method
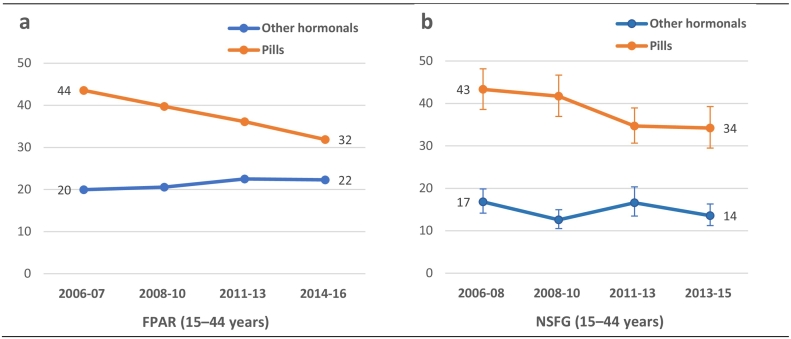
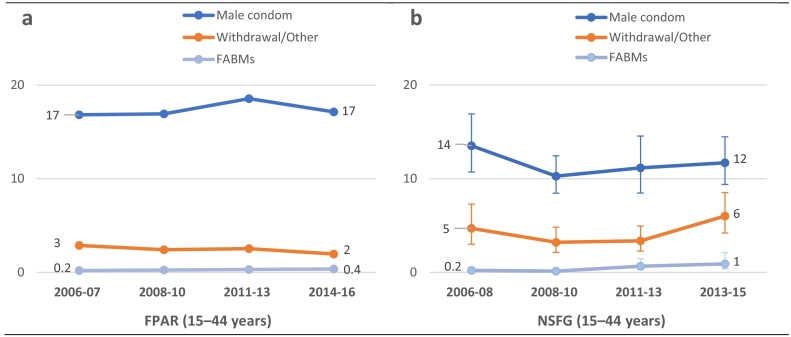
For use of individual methods, the differences between the Title X population and the comparable national population were more pronounced (Table 3). Female sterilization was lower among Title X clients (2%) than women nationally (5%), but male sterilization was similar (0.2% in both groups); male or female sterilization prevalence did not change between the first and current periods (Table 3 and Fig. 2). IUD use was lower among Title X clients (9%) than women nationally (13%) and increased in both groups over time. Prevalence of implants was similar in both groups (~ 5%) and showed a similar increase from 0.1% in the first period. Similar percentages of women in Title X (32%) and nationally (34%) used pills, which decreased over time in both groups (Table 3 and Fig. 3). Among Title X clients, the use of other hormonal methods (e.g., injectable, ring, patch) was higher than among women nationally (22% vs. 14%); over time, the prevalence of other hormonal methods in either group did not change. Compared with women nationally, Title X client male condom use was higher (17% vs. 12%) and use of withdrawal (2% vs. 6%) or no method (7% vs. 10%) was lower. In both populations, use of FABMs was low (between 0.4% and 1%) and did not change over time (Table 3 and Fig. 4). As with prevalence in method effectiveness categories, use of individual methods varied by age subgroups, but trends for at-risk women overall (15–44 years) were generally consistent with trends observed within age subgroups.
Table 3.
Trends in contraceptive prevalence among female Title X clients and a comparablea national sample of low-income women at risk of unintended pregnancy,b by age group, method use (any or no method), individual method type, and year: FPAR (2006–2016) and NSFG (2006–2015)
| Method by Age Group | Family Planning Annual Report |
National Survey of Family Growth |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006–07 |
2008–10 |
2011–13 |
2014–16 |
2006–07 vs. 2014–16 % point change |
2006–08 |
2008–10 |
2011–13 |
2013–15 |
2006–08 vs. 2013–15 % point change |
|||||
| % | % | % | % | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |||||||
|
15–44 |
N = 8.2 million |
N = 12.4 million |
N = 11.3 million |
N = 9.2 million |
n = 1,052c |
n = 1,213c |
n = 1,109c |
n = 1.037c |
||||||
| Any method | 88.9 | 88.1 | 91.5 | 90.1 | 1.1 | 89.3 | (86.5, 91.6) | 89.2 | (86.2, 91.6) | 89.5 | (86.7, 91.8) | 90.2 | (87.1, 92.6) | 0.9 |
| Male sterilization | 0.1 | 0.1 | 0.2 | 0.2 | 0.1 | 0.5 | (0.2, 1.3) | 0.8 | (0.2, 2.7) | 0.1 | (0.0†, 0.4) | 0.2 | (0.1, 0.7) | –0.3 |
| Female sterilization | 1.6 | 1.6 | 1.6 | 1.9 | 0.2 | 4.7 | (3.2, 6.8) | 7.0 | (5.0, 9.7) | 6.4 | (4.1, 9.9) | 4.9 | (3.3, 7.2) | 0.2 |
| Implant | 0.1 | 0.7 | 2.2 | 5.5 | 5.5 | 0.1 | (0.0†, 0.4) | 1.2 | (0.6, 2.6) | 2.0 | (1.2, 3.2) | 5.2 | (3.2, 8.6) | 5.1⁎⁎⁎ |
| IUD/IUS | 2.9 | 5.1 | 7.1 | 8.6 | 5.6 | 5.2 | (3.7, 7.3) | 11.8 | (8.9, 15.5) | 14.4 | (11.1, 18.5) | 13.4 | (10.6, 16.8) | 8.2⁎⁎⁎ |
| Other hormonald | 20.0 | 20.6 | 22.5 | 22.3 | 2.3 | 16.8 | (14.2, 19.9) | 12.6 | (10.5, 15.0) | 16.6 | (13.5, 20.3) | 13.6 | (11.2, 16.3) | –3.2 |
| Pills | 43.6 | 39.8 | 36.1 | 31.9 | –11.7 | 43.3 | (38.6, 48.2) | 41.7 | (36.9, 46.7) | 34.7 | (30.7, 38.9) | 34.2 | (29.5, 39.3) | –9.1⁎ |
| Male condom | 16.8 | 16.9 | 18.6 | 17.1 | 0.3 | 13.5 | (10.7, 16.9) | 10.3 | (8.4, 12.4) | 11.1 | (8.5, 14.5) | 11.7 | (9.4, 14.5) | –1.8 |
| Female barriere | 0.7 | 0.6 | 0.4 | 0.2 | –0.5 | 0.2 | (0.1, 0.7) | 0.5 | (0.1, 1.7) | 0.2 | (0.1, 0.9) | 0.0† | (0.0†, 0.3) | –0.2 |
| Withdrawal or otherf | 2.9 | 2.4 | 2.5 | 2.0 | –0.9 | 4.7 | (3.0, 7.3) | 3.2 | (2.1, 4.8) | 3.4 | (2.3, 4.9) | 6.0 | (4.2, 8.5) | 1.3 |
| FABMg | 0.2 | 0.3 | 0.3 | 0.4 | 0.2 | 0.2 | (0.1, 0.5) | 0.1 | (0.0†, 0.4) | 0.7 | (0.3, 1.5) | 0.9 | (0.4, 2.1) | 0.7 |
| No method | 8.1 | 6.9 | 6.2 | 6.8 | –1.3 | 10.7 | (8.4, 13.5) | 10.8 | (8.4, 13.8) | 10.5 | (8.2, 13.3) | 9.8 | (7.4, 12.9) | –0.9 |
| Missing | 3.0 | 5.0 | 2.3 | 3.1 | 0.1 | — | — | — | — | — | ||||
|
15–19 |
N = 2.1 million |
N = 2.9 million |
N = 2.3 million |
N = 1.7 million |
n = 242 |
n = 260 |
n = 204 |
n = 199 |
||||||
| Any method | 89.1 | 88.3 | 91.9 | 90.4 | 1.3 | 84.1 | (77.3, 89.1) | 83.2 | (76.0, 88.5) | 86.9 | (80.3, 91.5) | 89.2 | (82.3, 93.6) | 5.2 |
| Male sterilization | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | — | 0.0 | — | 0.0 | — | 0.0 | — | — |
| Female sterilization | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | — | 0.0 | — | 0.0 | — | 0.0 | — | — |
| Implant | 0.1 | 0.9 | 2.8 | 7.6 | 7.6 | 0.1 | (0.0†, 1.0) | 0.2 | (0.0†, 0.8) | 0.9 | (0.3, 2.9) | 7.5 | (3.0, 17.3) | 7.4⁎ |
| IUD/IUS | 0.7 | 1.6 | 2.4 | 3.5 | 2.9 | 2.0 | (0.7, 6.1) | 4.9 | (2.0, 11.5) | 3.0 | (0.6, 13.0) | 3.9 | (1.6, 9.1) | 1.9 |
| Other hormonald | 19.9 | 22.1 | 26.7 | 27.1 | 7.2 | 18.4 | (12.8, 25.7) | 18.3 | (12.8, 25.5) | 11.4 | (7.4, 17.2) | 20.7 | (11.8, 33.7) | 2.3 |
| Pills | 47.2 | 44.1 | 40.0 | 35.7 | –11.4 | 41.8 | (33.9, 50.3) | 45.3 | (38.7, 52.0) | 51.4 | (41.3, 61.5) | 40.8 | (31.3, 50.9) | –1.1 |
| Male condom | 18.2 | 17.2 | 17.4 | 14.6 | –3.6 | 17.0 | (11.2, 25.0) | 8.0 | (5.0, 12.4) | 16.6 | (9.5, 27.6) | 12.6 | (7.3, 20.6) | –4.5 |
| Female barriere | 0.4 | 0.4 | 0.3 | 0.2 | –0.3 | 0.0 | — | 0.0 | — | 0.0 | — | 0.0 | — | — |
| Withdrawal or otherf | 2.6 | 2.0 | 2.1 | 1.4 | –1.2 | 4.7 | (2.4, 9.0) | 6.3 | (3.0, 12.9) | 2.9 | (1.3, 6.4) | 3.8 | (1.7, 8.3) | –0.8 |
| FABMg | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.0 | — | 0.3 | (0.0†, 1.5) | 0.6 | (0.1, 2.7) | 0.0 | — | 0.0 |
| No method | 8.1 | 7.1 | 5.9 | 6.8 | –1.3 | 15.9 | (10.9, 22.7) | 16.8 | (11.5, 24.0) | 13.1 | (8.5, 19.7) | 10.8 | (6.4, 17.7) | –5.2 |
| Missing | 2.8 | 4.7 | 2.1 | 2.8 | 0.0 | — | — | — | — | — | ||||
| 20–29 | N = 4.3 million | N = 6.6 million | N = 6.0 million | N = 4.8 million | n = 546 | n = 616 | n = 604 | n = 541 | ||||||
| Any method | 89.5 | 88.7 | 92.1 | 91.2 | 1.6 | 91.4 | (87.8, 94.0) | 91.4 | (88.0, 93.9) | 90.6 | (87.5, 93.0) | 93.3 | (90.5, 95.3) | 1.9 |
| Male sterilization | 0.1 | 0.1 | 0.1 | 0.1 | 0.0 | 0.1 | (0.0†, 0.9) | 0.2 | (0.1, 0.8) | 0.0 | — | 0.2 | (0.0†, 1.2) | 0.0 |
| Female sterilization | 0.7 | 0.7 | 0.6 | 0.5 | –0.2 | 4.0 | (2.3, 6.8) | 5.6 | (3.3, 9.3) | 4.1 | (2.4, 6.8) | 2.3 | (1.2, 4.4) | –1.7 |
| Implant | 0.1 | 0.7 | 2.3 | 6.1 | 6.0 | 0.2 | (0.0†, 0.8) | 1.8 | (0.6, 4.8) | 3.1 | (1.7, 5.6) | 6.9 | (4.2, 11.0) | 6.7⁎⁎⁎ |
| IUD/IUS | 3.1 | 5.5 | 7.4 | 8.6 | 5.6 | 6.5 | (4.3, 9.6) | 13.1 | (9.5, 17.9) | 14.9 | (11.3, 19.3) | 14.9 | (10.9, 19.9) | 8.4⁎⁎ |
| Other hormonald | 20.8 | 21.2 | 22.6 | 22.0 | 1.2 | 17.7 | (14.3, 21.8) | 11.2 | (8.5, 14.7) | 20.5 | (15.7, 26.3) | 11.5 | (8.9, 14.7) | –6.3⁎⁎ |
| Pills | 45.3 | 41.5 | 38.3 | 34.1 | –11.1 | 45.1 | (38.4, 52.1) | 44.1 | (36.9, 51.5) | 34.0 | (28.8, 39.7) | 37.3 | (31.8, 43.2) | –7.8 |
| Male condom | 15.7 | 15.9 | 17.7 | 17.3 | 1.6 | 13.4 | (9.8, 18.0) | 12.9 | (9.9, 16.7) | 10.1 | (6.6, 15.3) | 12.7 | (9.5, 16.8) | –0.7 |
| Female barriere | 0.6 | 0.5 | 0.3 | 0.2 | –0.4 | 0.1 | (0.0†, 1.0) | 0.0 | (0.0, 0.0) | 0.2 | (0.0†, 1.7) | 0.1 | (0.0†, 0.6) | 0.0 |
| Withdrawal or otherf | 3.0 | 2.4 | 2.5 | 1.9 | –1.0 | 4.1 | (2.5, 6.6) | 2.4 | (1.4, 4.3) | 2.9 | (1.6, 4.9) | 6.1 | (4.0, 9.2) | 2.0 |
| FABMg | 0.2 | 0.2 | 0.3 | 0.3 | 0.1 | 0.1 | (0.0†, 0.8) | 0.0 | (0.0†, 0.3) | 0.8 | (0.3, 2.7) | 1.3 | (0.5, 3.8) | 1.2 |
| No method | 7.8 | 6.5 | 5.7 | 6.1 | –1.6 | 8.6 | (6.0, 12.2) | 8.6 | (6.1, 12.0) | 9.4 | (7.0, 12.5) | 6.7 | (4.7, 9.5) | –1.9 |
| Missing | 2.7 | 4.8 | 2.2 | 2.7 | 0.0 | — | — | — | — | — | ||||
|
30–44 |
N = 1.8 million |
N = 2.9 million |
N = 3.0 million |
N = 2.7 million |
n = 264 |
n = 337 |
n = 301 |
n = 297 |
||||||
| Any method | 87.2 | 86.5 | 90.1 | 87.9 | 0.7 | 89.3 | (81.8, 93.9) | 90.1 | (84.8, 93.7) | 89.4 | (84.0, 93.2) | 85.3 | (78.0, 90.4) | –4.0 |
| Male sterilization | 0.4 | 0.4 | 0.5 | 0.5 | 0.1 | 1.7 | (0.6, 4.8) | 2.3 | (0.5, 9.2) | 0.3 | (0.1, 1.4) | 0.4 | (0.1, 2.0) | –1.3 |
| Female sterilization | 5.8 | 5.4 | 5.0 | 5.4 | –0.4 | 10.3 | (5.7, 18.1) | 14.7 | (9.5, 22.0) | 14.5 | (8.1, 24.6) | 12.7 | (7.9, 19.9) | 2.4 |
| Implant | 0.1 | 0.5 | 1.3 | 3.3 | 3.2 | 0.0 | — | 1.0 | (0.3, 3.1) | 0.8 | (0.3, 2.4) | 0.8 | (0.2, 3.4) | 0.8 |
| IUD/IUS | 5.4 | 7.8 | 10.2 | 11.7 | 6.3 | 5.1 | (2.7, 9.5) | 15.0 | (10.0, 21.9) | 20.6 | (13.0, 30.9) | 16.9 | (12.2, 22.8) | 11.7⁎⁎⁎ |
| Other hormonald | 18.0 | 17.8 | 19.1 | 19.8 | 1.8 | 13.5 | (8.8, 20.2) | 10.4 | (7.0, 15.3) | 13.0 | (8.7, 19.2) | 12.9 | (9.2, 17.6) | –0.7 |
| Pills | 35.1 | 31.5 | 28.9 | 25.5 | –9.6 | 40.7 | (32.6, 49.2) | 35.1 | (27.9, 43.1) | 25.4 | (19.3, 32.7) | 24.4 | (17.5, 33.0) | –16.2⁎⁎ |
| Male condom | 17.9 | 19.0 | 21.0 | 18.5 | 0.5 | 10.9 | (6.8, 16.9) | 7.7 | (5.0, 11.5) | 9.5 | (5.1, 17.2) | 9.3 | (5.6, 15.2) | –1.5 |
| Female barriere | 1.1 | 0.8 | 0.5 | 0.3 | –0.8 | 0.6 | (0.1, 3.0) | 1.6 | (0.4, 5.5) | 0.3 | (0.0†, 2.2) | 0.0 | — | –0.6 |
| Withdrawal or otherf | 3.0 | 2.8 | 3.0 | 2.4 | –0.6 | 6.0 | (2.3, 14.6) | 2.1 | (1.0, 4.6) | 4.5 | (2.4, 8.5) | 7.2 | (3.6, 13.9) | 1.2 |
| FABMg | 0.4 | 0.5 | 0.5 | 0.5 | 0.2 | 0.5 | (0.1, 1.7) | 0.2 | (0.0†, 0.8) | 0.4 | (0.1, 1.8) | 0.7 | (0.2, 2.4) | 0.2 |
| No method | 8.9 | 7.8 | 7.2 | 8.0 | –0.9 | 10.7 | (6.1, 18.2) | 9.9 | (6.3, 15.2) | 10.6 | (6.8, 16.0) | 14.7 | (9.6, 22.0) | 4.0 |
| Missing | 3.9 | 5.8 | 2.7 | 4.1 | 0.2 | — | — | — | — | — | ||||
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth; CI, confidence interval; IUD/IUS, Intrauterine device/system; FABM, fertility awareness-based method. NOTE: The size of the Title X age subgroups may not sum to the total because of rounding. — Not applicable.
< .001;
< .01;
< .05.
Greater than 0.0 and less than .05.
We restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
In the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
The weighted NSFG samples for females 15–44 years are 2006–08 (N = 9,143,000), 2008–10 (N = 10,520,000), 2011–13 (N = 10,345,000), 2013–15 (N = 10,425,000).
Other hormonal methods include injectable contraception, vaginal contraceptive ring, and contraceptive patch.
Female barrier methods include diaphragm, cervical cap, female condom, contraceptive sponge, and spermicide
The “withdrawal or other” category includes EC.
In FPAR, the FABM method category also includes the lactational amenorrhea method.
Fig. 2.
Trends in the percentage of female Title X clients (a) and a comparablea national sample (b) of low-income women at risk of unintended pregnancyb who use female sterilization, male sterilization, implant, or IUD/IUS, by year: FPAR (2006–2016)c and NSFG (2006–2015)d
NOTE:
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth; IUD/IUS, intrauterine device/intrauterine system.
aWe restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
bIn the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
cThe FPAR populations for each period are as follows: 2006–07 (8,185,457), 2008–10 (12,390,516), 2011–13 (11,327,058), 2014–16 (9,245,609).
dNSFG samples for at-risk females aged 15–44 years are as follows: 2006–08 (unweighted = 1,052; weighted = 9,143,000), 2008–10 (unweighted = 1,213; weighted = 10,520,000), 2011–13 (unweighted = 1,109; weighted = 10,345,000), 2013–15 (unweighted = 1,037; weighted = 10,425,000).
Fig. 3.
Trends in the percentage of female Title X clients (a) and a comparablea national sample (b) of low-income women at risk of unintended pregnancyb who use pills or other hormonal contraception, by year: FPAR (2006–2016)c and National Survey of Family Growth (2006–2015)d
NOTE:
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth.
aWe restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
bIn the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
cThe FPAR populations for each period are as follows: 2006–07 (8,185,457), 2008–10 (12,390,516), 2011–13 (11,327,058), 2014–16 (9,245,609).
dNSFG samples for at-risk females aged 15–44 years are as follows: 2006–08 (unweighted = 1,052; weighted = 9,143,000), 2008–10 (unweighted = 1,213; weighted = 10,520,000), 2011–13 (unweighted = 1,109; weighted = 10,345,000), 2013–15 (unweighted = 1,037; weighted = 10,425,000).
Fig. 4.
Trends in the percentage of female Title X clients (a) and a comparablea national sample (b) of low-income women at risk of unintended pregnancyb who use the male condom, withdrawal, or FABMs, by year: FPAR (2006–2016)c and NSFG (2006–2015)d
NOTE:
Abbreviations: FPAR, Family Planning Annual Report; NSFG, National Survey of Family Growth; FABMs, fertility awareness-based methods.
aWe restricted the national sample of women at risk of unintended pregnancy to low-income women who reported receipt of any contraceptive services in the previous 12 months and who had not been surgically sterilized 13 or more months before the survey. Low-income, at-risk women were those aged 20–44 years with a household income at or below 250% of the federal poverty level and those aged 15–19 years, regardless of income. Contraceptive services included a birth control (BC) method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception (EC) counseling or prescription.
bIn the NSFG, women at risk of unintended pregnancy included women who were sexually active in the previous 3 months (using contraception or not) and excluded women who were currently pregnant, trying to conceive, or sterile. In the FPAR, women at risk of unintended pregnancy include all Title X clients except those who were pregnant or seeking pregnancy.
cThe FPAR populations for each period are as follows: 2006–07 (8,185,457), 2008–10 (12,390,516), 2011–13 (11,327,058), 2014–16 (9,245,609).
dNSFG samples for at-risk females aged 15–44 years are as follows: 2006–08 (unweighted = 1,052; weighted = 9,143,000), 2008–10 (unweighted = 1,213; weighted = 10,520,000), 2011–13 (unweighted = 1,109; weighted = 10,345,000), 2013–15 (unweighted = 1,037; weighted = 10,425,000).
4. Discussion
Contraceptive use and method choice are important measures of contraceptive access [5] and strong predictors of unintended pregnancy risk [22], [23]. Using multiyear data from Title X (2006–2016) and NSFG (2006–2015), we examined patterns and trends in contraceptive use among reproductive-age women (15–44) attending Title X-funded clinics and a comparable group of low-income women nationally who received contraceptive services in the past year and were at risk of unintended pregnancy. Although the mix of contraceptive methods in the national sample differed from that of the Title X clients, over time in both groups we found an increased use of the most effective reversible methods (i.e., LARCs); decreased use of moderately effective methods; and no change in the use of permanent, less effective, or no method. Although the two populations were similar in terms of receipt of contraceptive care and the upper-income threshold, the Title X population appears to be more racially and ethnically diverse, poorer, and uninsured at higher rates than their national counterparts.
The increase in LARC use observed in the two study populations is consistent with LARC trends found in other analyses using NSFG [24], [25], [26]. In the Kavanaugh and Jerman study [26], however, the increase in LARC use was offset by a decrease in sterilization, while the LARC increase in our study was offset by declines in pill (Title X) or pill and other hormonal methods (national). Our decision to exclude from the NSFG sample women who had been sterilized 13 or more months before the survey meant that sterilization users in the NSFG represented those sterilized in the past year and not the cumulative prevalence.
Ease of access is one plausible reason for the observed differences in the use of other hormonal methods between Title X clients and the national sample. As noted earlier, Title X clinics report higher on-site availability of FDA-approved methods than publicly funded clinics receiving no Title X funding [11]. In addition, a 2010 study found that Title X-funded providers were more likely than private physicians to provide other hormonal methods on-site [27]. Finally, participation of almost all Title X providers in the federal 340B Drug Pricing Program allows them to purchase contraceptive supplies at discounted rates and offer them at low or no cost to their clients [28].
Finally, among at-risk Title X clients and low-income women nationally, contraceptive nonuse was 7% and 10%, respectively. These percentages changed little over the study period. Instead of a shift from less effective or no method to more effective ones, we observed a shift from moderately effective to most effective methods. Simulations by Thomas and Karpilow [29], [30], [31] show potential reductions in unintended pregnancy when at-risk women who are using no method adopt any method, including a less effective one. Emphasis on a single type of method (e.g., LARCs), they assert, overlooks the potential impact that may result when nonusers adopt even a less effective method. Research is needed to understand possible reasons [32] why some at-risk women who receive contraceptive care might not be using contraception.
5. Limitations
This study has some limitations. First and foremost, the contraceptive prevalence measures based on NSFG and FPAR data differ in ways that may affect the observed differences in prevalence that we have reported. The NSFG contraceptive use variable (CONSTAT1) is a self-reported measure of the most effective contraceptive method used in the month of the survey. The FPAR contraceptive use measure, in contrast, is provider-reported data on the most effective method received—either already being used or newly adopted during the Title X encounter. In the FPAR data, we are unable to differentiate between a method already in use or newly adopted during the encounter and lack data on the method, if any, at entry to the encounter. Therefore, the FPAR contraceptive use measure may overstate (1) use of any method for Title X clients who enter the encounter using no method and exit the encounter having received any method and (2) use of more effective methods for Title X clients who enter the encounter using a less effective method and exit the encounter having received a more effective method. In addition, a reversible method that is not inserted or injected during the Title X encounter (e.g., condoms, pills, or patch) may be documented in the client’s medical record as the method received and reported in FPAR, but the client may opt to not use that documented method. The extent to which this occurs and affects the national estimates is unknown.
In terms of the NSFG data, the variable (CONSTAT1) we used to define our contraceptive use outcome captures the most effective method used during the interview month. If a woman relies on a coitus-dependent method, such as withdrawal or condom, but she does not have sex in the interview month, she is coded as a nonuser. This has the effect of overstating method nonuse for female respondents who meet these conditions.
In terms of the FPAR data, information on sexual activity and fecundity status for Title X clients is not collected. As a result, we have excluded only those clients who were pregnant or seeking pregnancy and may have retained some clients who were not at risk of unintended pregnancy in the denominator of our FPAR-based prevalence calculations.
Finally, prevalence measures from both sources rely on the single most effective method used in the month of the survey (NSFG) or at exit from the family planning encounter (FPAR). Data on the single most effective method underestimate the use of less effective methods (e.g., condoms) that women may use concurrently.
6. Conclusion
Ensuring access to a broad range of safe and effective contraceptive methods is a hallmark of high-quality, client-centered family planning care [33] and a requirement of programs that receive Title X funding [13]. In 2016, the National Quality Forum endorsed three contraceptive provision measures, thereby acknowledging the relationship between method choice and use on unintended pregnancy risk and the existence of modifiable factors in the structure, financing, and delivery of contraceptive care. These measures can play an important role in monitoring gaps and driving quality improvements [34], [35].
This study contributes to our understanding of contraceptive use patterns and trends for two groups of low-income women at risk of unintended pregnancy who accessed contraceptive services. Our findings encourage consideration of how analytic strategies, data limitations, patient preferences, and factors of the supply environment might affect the patterns and trends we observe.
Acknowledgments
We acknowledge the editorial support of Sharon Barrell at RTI International.
Footnotes
Declaration of Interests: OPA authors have no financial or personal conflicts of interest to report. RTI authors report that a portion of their salaries, including time for analysis and writing of this manuscript, was supported by the HHS/OPA contract (HHSP23320095651WC/HHSP23337041T) to RTI International.
Funding source: This work was supported under a contract (HHSP23320095651WC/HHSP23337041T) to RTI International from the US Department of Health and Human Services Office of Population Affairs.
Contraceptive services include a birth control method/prescription or checkup, counseling, sterilization counseling or procedure, or emergency contraception counseling or prescription.
Other sexual or reproductive health services include a Pap test or pelvic exam; STD counseling, testing, or treatment; pregnancy testing; prenatal care; postpartum care; and abortion.
Contributor Information
Christina I. Fowler, Email: cfowler@rti.org.
Katherine A. Ahrens, Email: katherine.ahrens@maine.edu.
Emily Decker, Email: edecker@upstream.org.
Julia Gable, Email: jgable@rti.org.
Jiantong Wang, Email: wang@rti.org.
Brittni Frederiksen, Email: BrittniF@kff.org.
Ana Carolina Loyola Briceño, Email: AnaCarolina.LoyolaBriceno@hhs.gov.
Susan B. Moskosky, Email: Susan.Moskosky@hhs.gov.
References
- 1.Office of Disease Prevention and Health Promotion . U.S. Department of Health and Human Services; Washington, DC: 2018. Healthy People 2020: Family Planning Objectives. [Google Scholar]
- 2.Centers for Disease Control and Prevention . U.S. Department of Health and Human Services; Atlanta: 2017. Contraception. [Google Scholar]
- 3.Curtis K.M., Tepper N.K., Jatlaoui T.C. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65:1–103. doi: 10.15585/mmwr.rr6503a1. [DOI] [PubMed] [Google Scholar]
- 4.Finer L.B., Zolna M.R. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bertrand J., Magnani R., Knowles J. The EVALUATION Project, Carolina Population Center; Chapel Hill, NC: 1994. Handbook of indicators for family planning program evaluation; p. 218. [Google Scholar]
- 6.The American College of Obstetricians and Gynecologists (ACOG) (Committee on Practice Bulletins-Gynecology and Long-Acting Reversible Contraception Working Group) Practice Bulletin No. 186: Long-Acting Reversible Contraception: Implants and Intrauterine Devices. Obstet Gynecol. 2017;130:e251–e269. doi: 10.1097/AOG.0000000000002400. [DOI] [PubMed] [Google Scholar]
- 7.The American College of Obstetricians Gynecologists (Committee on Adolescent Health Care and Long-Acting Reversible Contraception Working Group) ACOG Committee Opinion No. 735: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2018;131:e130–e139. doi: 10.1097/AOG.0000000000002632. [DOI] [PubMed] [Google Scholar]
- 8.Frost J.J., Frohwirth L., Zolna M.R. Guttmacher Institute; New York, NY: 2016. Contraceptive needs and services, 2014 update. [Google Scholar]
- 9.Office of Population Affairs . U.S. Department of Health and Human Services; Washington, DC: 2018. About Title X Grants. [Google Scholar]
- 10.Office of Population Affairs . U.S. Department of Health and Human Services; Washington, DC: 2018. Title X Statutes and Regulations. [Google Scholar]
- 11.Zolna M.R., Frost J.J. Guttmacher Institute; New York: 2016. Publicly Funded Family Planning Clinics in 2015: Patterns and trends in service delivery practices and protocols; p. 68. [Google Scholar]
- 12.Office of Population Affairs . OPA; Rockville, MD: 2016. Title X Family Planning Annual Report Forms and Instructions. [Google Scholar]
- 13.Office of Population Affairs . Office of Population Affairs; Rockville, MD: 2014. Program Requirements for Title X Funded Family Planning Projects. [Google Scholar]
- 14.Fowler C.I., Gable J., Wang J., Lasater B. RTI International; Research Triangle Park, NC: 2017. Title X Family Planning Annual Report: 2016 National Summary. [Google Scholar]
- 15.National Center for Health Statistics . CDC; Atlanta, GA: 2017. National Survey of Family Growth: Questionnaires, Datasets, and Related Documentation. [Google Scholar]
- 16.National Center for Health Statistics . CDC; Atlanta, GA: 2016. About the National Survey of Family Growth. [Google Scholar]
- 17.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatcher R.A., Trussell J., Nelson A.L., Cates W., Kowal D., Policar M.S. Ardent Media, Inc; Atlanta, GA: 2011. Contraceptive technology. (20th Revised Edition) [Google Scholar]
- 19.National Center for Health Statistics . NCHS; Hyattsville, MD: 2018. NSFG Current contraceptive status (CONSTAT1) Recode. [Google Scholar]
- 20.SAS Institute . SAS Institute; Cary, NC: 2013. SAS/STAT user's guide (Version 9.4) [Google Scholar]
- 21.Research Triangle Institute . RTI; Research Triangle Park, NC: 2012. SUDAAN Language Manual, Volumes 1 and 2 (Release 11) [Google Scholar]
- 22.Lindberg L., Santelli J., Desai S. Understanding the decline in adolescent fertility in the United States, 2007–2012. J Adolesc Health. 2016;59:577–583. doi: 10.1016/j.jadohealth.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trussell J., Henry N., Hassan F., Prezioso A., Law A., Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87:154–161. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Branum A.M., Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15-44. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 25.Hubacher D., Kavanaugh M. Historical record-setting trends in IUD use in the United States. Contraception. 2018;98:467–470. doi: 10.1016/j.contraception.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 26.Kavanaugh M.L., Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception. 2018;97:14–21. doi: 10.1016/j.contraception.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moskosky S., Zapata L.B., Whiteman M.K. Contraceptive methods available to patients of office-based physicians and Title X clinics: United States, 2009–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1–4. [PubMed] [Google Scholar]
- 28.National Family Planning & Reproductive Health Association . NFPRHA; Washington, DC: 2013. The 340B Drug Discount Program: Benefits and Challenges for Title X. [Google Scholar]
- 29.Karpilow Q.C., Thomas A.T. Reassessing the importance of long-acting contraception. Am J Obstet Gynecol. 2017;216:148. doi: 10.1016/j.ajog.2016.10.012. [e1- e14] [DOI] [PubMed] [Google Scholar]
- 30.Thomas A.T., Karpilow Q.C. The intensive and extensive margins of contraceptive use: comparing the effects of method choice and method initiation. Contraception. 2016;94:160–167. doi: 10.1016/j.contraception.2016.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Thomas A.T., Karpilow Q.C. Long-acting reversible contraception: a silver bullet solution for unintended pregnancy? Am J Public Health. 2018;108:1007–1008. doi: 10.2105/AJPH.2018.304523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mosher W., Jones J., Abma J. Nonuse of contraception among women at risk of unintended pregnancy in the United States. Contraception. 2015;92:170–176. doi: 10.1016/j.contraception.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gavin L., Moskosky S., Carter M. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63:1–54. [PubMed] [Google Scholar]
- 34.Gavin L., Frederiksen B., Robbins C., Pazol K., Moskosky S. New clinical performance measures for contraceptive care: their importance to healthcare quality. Contraception. 2017;96:149–157. doi: 10.1016/j.contraception.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The American College of Obstetricians and Gynecologists . 2018. Contraceptive Care Measures. [Google Scholar]