Highlights
-
•
Telehealth keeps patients with parkinsonism safe from traveling to in-person care site during the COVID-19 mitigation phase.
-
•
During the COVID-19 crisis, a telemedicine program for patients with parkinsonism was boosted in Milan, Italy.
-
•
This two-step model integrates a telenursing forward triage followed by video-consultations by experienced neurologists.
Keywords: Telemedicine, Parkinson disease, Integrated management, COVID-19
Since the first patient diagnosed with COVID-19 in Lombardy, Italy has become the third most affected country (>217.000 cases, >30.000 deaths) in the world, as of May 9th, 2020 [1]. Whereas the initial response strategy to COVID-19 aimed to contain its spread, policy makers are moving from containment (‘Phase One’) to mitigation (‘Phase Two’) by gradually lifting lockdown restrictions. This ‘Phase Two’ (which will probably last for 1 or 2 years) may be more dangerous than ‘Phase One’, because patients with chronic neurological diseases, such as Parkinson's disease (PD) and other forms of parkinsonism, are allowed again to engage in risky travel to in-person care sites. To avoid a second peak in incidence and further increases in death rates, we propose a two-step telehealth model. The first step involves a “forward triage” performed by a readily accessible case manager (namely a PD nurse specialists, PDNS), who can solve many medical problems directly and remotely, alleviating the pressure on the overburdened patient's own regular providers, many of whom were deeply involved in managing the COVID-19 challenges and consequently had little time for attending to the needs of PD patients. For those patients who do require subsequent input by a medical specialist, the second step consists of remote assessment by a neurologist/geriatrician. This strategy would reconcile the need of patients for accessible, high-level medical expertise with the need to protect patients and clinicians from exposure.
The first step, a novel remote telenursing assistance service (named “ParkinsonCare”) is viable in Milan since February 2019, with a rapidly accelerated adoption during the COVID-19 crisis. This remote telenursing assistance was positioned as a new service outside the regular care facilities and was made available free of charge to patients. Specifically, a PDNS acting as personal case manager remotely assists patients using a predefined semi-structured interview and create a dossier, which is available for patients, their own neurologist and other members of the multidisciplinary care team within an online platform. Separate triage protocols are in place for specific common medical issues (e.g., falls, dysphagia), allowing for standardised assessment of the problem plus delivery of tailored advice. From March 12th to May 14th, 2020, this service managed 2021 interactions (telephone calls) between PDNS and 525 patients throughout Italy, of whom 398 patients (76%; 59.1% men, age 73.7 ± 9.7 [range 39–94] years, PD-duration 8.6 ± 6.3 years) required PDNS management. Among these patients, 247 (62%) were fully managed by the PDNS, while 151 (38%) required subsequent referral to a multidisciplinary team, which was performed via 194 video-consultations, sometimes with more than one health professional. Once contact had been established, the PDNS first attempted to get in touch with the patient's own regular neurologist. In case of unavailability, another neurologist experienced in movement disorders was contacted. Only one third (36.4%) of referred patients needed a neurologist (typically for medication adjustments); the remaining patients required physiotherapists (35.8%), psychologists (16%), speech therapists (8%) or occupational (3.8%) therapists. Out of 194 video-consultations (using Zoom® platform), only 18 (9.3%) failed, mostly due to patient/caregiver's inability to deal with the hardware and/or software and concomitant lack of a younger family member; one experienced broadband connection failure. Over two-thirds of patients/caregivers (70%) provided positive feedback, comments were not provided in 28% of cases, and 2% were disappointed by the lack of home-care nursing.
The second step was implemented at the “Carlo Besta” Neurological Institute by initiating regulation-compliant [2] video-consultations (using Microsoft Teams® platform) with experienced neurologists on March 30th, 2020, which were followed by an online release of a password-encrypted medical report (approved by the Ethics Committee and anticipated by signed informed consent). This approach was reimbursed by the Lombardy Regional health system at the same rate of in-person follow-up visits. From March 30th to May 14th, 2020, video-consultations increased steadily to become over two-thirds (71.4%) of the total number of outpatient assessments. Out of the 174 scheduled visits, 54.6% were replaced by video-consultation (59% men, age 68.6 ± 10.8 [range 39–89] years), 23.6% were cancelled (mostly due to lockdown restrictions, COVID-19-related symptoms, or mild/stable PD), and only 21.8% of patients needed in-person visit.
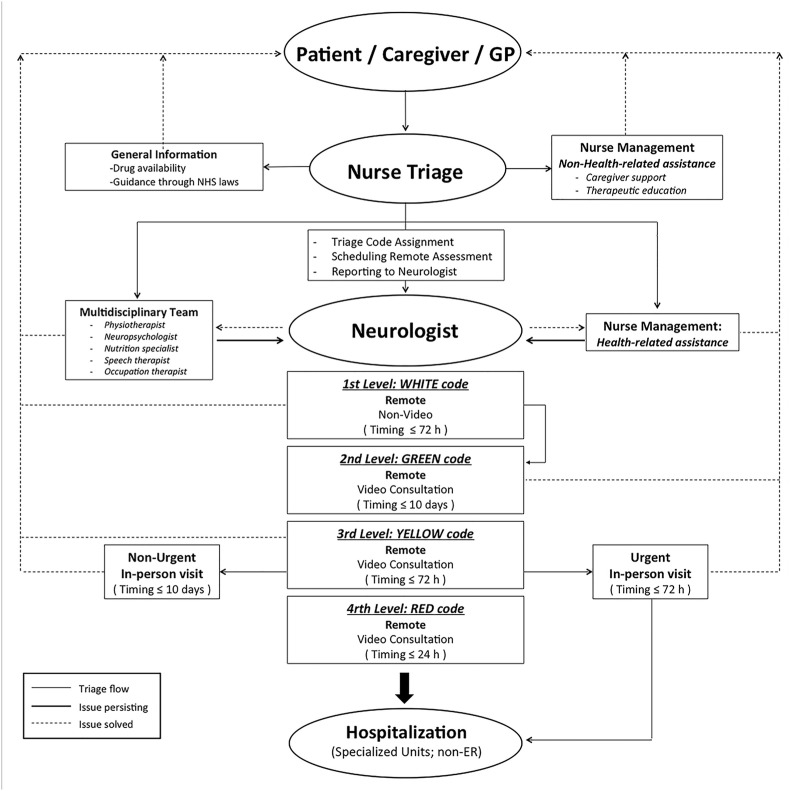
Based on our successful experience during the COVID-19 crisis, we propose a two-pronged model to optimize the management of patients with parkinsonism (Fig. 1 ). Patients contact the PDNS before the formerly scheduled in-person visit or because of an urgent need. The PDNS can directly manage the problem, or refer to the multidisciplinary team, or refer to the neurologist for a medical intervention. Whenever referral to a neurologist is needed, the PDNS assigns a 4-level code triage, where greater urgency would lead to reduced time-to-assessment. Code assignment is based on two gateway questions: (a) does this change increase the risk of morbidity in the short-term (e.g., risk of hip fracture due to falls)? (b) Has functional independence changed? According to the answers to questions ‘a’ and ‘b’, we hypothesize four scenarios: (1) white-code (answer: no/no): non-urgent, solvable via email/telephone; (2) green-code (answer: no/yes): non urgent but needing video-consultation; (3) yellow-code (answer: yes to ‘a’): timely video consultation to solve urgent issues and to decide whether in-person visit is needed; (4) red-code: life-threatening event needing hospitalization. In case of PD-related emergency, a pre-existing multidisciplinary medical team is alerted to plan safe hospitalization in dedicated units (e.g., neurosurgeons for deep brain stimulation battery replacement), by-passing in-person triage at the emergency room and minimizing the risk of infection.
Fig. 1.
Conceptual framework of remote assistance to the patient. Circles represent people involved in the diagnostic-therapeutic flow-chart; rectangles represent actions. Solid lines, triage flow; dashed lines, health-related issues solved; bold lines, health-related issues persisting. The 4-code colours have been chosen according to the assignment of progressive urgency at Italian ER triage. Abbreviations: ER, emergency room; GP, general practitioner.
Before the outbreak, it has been proposed that in-person visits might become the “Option B” for frail patients with chronic diseases, such as PD [3]. Randomized controlled trials on patients with chronic diseases, including PD, suggest that similar health outcomes may be reached using telehealth compared with in-person visits [4,5]. Creating telemedicine programs usually takes time due to challenges in adaptation among end-users (patients and clinicians), logistics, reimbursement, data security and patient privacy. Nonetheless, many countries had already invested in telemedicine prior to the present COVID-19 crisis (e.g., U.S., UK, France, etc.) [3,5]. However, the COVID-19 crisis has certainly catalyzed this ongoing conversion process [6], and many countries worldwide, here exemplified by Italy [2], took giant strides within just a few weeks. This fast and widespread international adoption of telemedicine typically involved the patient's own regular care team, who now deliver their services remotely, instead of using in-clinic assessments. The radically new element that we introduce here consists of a remote consultation service by case managers, who were not originally part of the patient's care team. This solution may be a viable alternative in case specialized nurses of the patients' regular care team cannot be newly appointed to this telehealth service. Similarly, the second step of the process could again involve a new team member (an independent movement disorders expert) if the patient's own medical specialist was inaccessible. By necessity, this strategy can now be field-tested on a wide-scale until the COVID-19 menace is controlled successfully, and we anticipate that many successful elements will probably become part of our new way of working after this crisis had resolved [6]. For example, even in the US but also in various other countries, many PD patients do not have access to a nearby neurologist as part of the regular care team [7], so having access to a remote specialist could offer a possible solution, provided that issues such as reimbursement and liability are resolved. Further research obviously remains needed to fully establish the pros and cons of teleconsultation services, including the novel two-step approach introduced here.
Acknowledgments
We are thankful to Orientina Di Giovanni for collecting information and providing data about the ParkinsonCare service and Daniele Volpe for providing video-access to rehab professionals. At the Fondazione IRCCS Istituto Neurologico Carlo Besta, we thank Antonio Elia, Luigi Romito, Grazia Devigili, Salvatore Bonvegna, Nico Golfrè Andreasi, and Giulia Straccia for video consultations and manuscript revision; Alice Basili for providing data on video-consultations, and Francesca De Giorgi for providing helpful insights on Italian telemedicine regulations. RC is thankful to Esther Cubo for helpful insights on telemedicine.
References
- 1.Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Updated May 7, 2020.
- 2.Gabbrielli F., Bertinato L., De Filippis G., Bonomini M., Cipolla M. April 13, 2020. Istituto Superiore di Sanità. Interim provisions on telemedicine healthcare services during COVID-19 health emergency; p. 29. 2020, ii. Rapporti ISS COVID-19 n. 12/2020. [Google Scholar]
- 3.Duffy S., Lee T.H. In-person health care as option B. N. Engl. J. Med. 2018;378:104–106. doi: 10.1056/NEJMp1710735. [DOI] [PubMed] [Google Scholar]
- 4.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015:CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beck C.A., Beran D.B., Biglan K.M. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology. 2017;89(11):1152‐1161. doi: 10.1212/WNL.0000000000004357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bloem B.R., Dorsey E.R., Okun M.S. The coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurol. Epub. 2020 Apr 24 doi: 10.1001/jamaneurol.2020.1452. [DOI] [PubMed] [Google Scholar]
- 7.Willis A.W., Schootman M., Evanoff B.A., Perlmutter J.S., Racette B.A. Neurologist care in Parkinson disease: a utilization, outcomes, and survival study. Neurology. 2011;77(9):851‐857. doi: 10.1212/WNL.0b013e31822c9123. [DOI] [PMC free article] [PubMed] [Google Scholar]